Abstract
Background
In 2012, over half of nursing homes were operated by corporate chains. Facilities owned by the largest for-profit chains were reported to have lower quality of care. However, it is unknown how nursing home chain ownerships are related with experiences of care.
Objectives
To study the relationship between nursing home chain characteristics (chain size and profit status) with patients' family member reported ratings on experiences with care.
Data Sources and Study Design
Maryland nursing home care experience reports, the Online Survey, Certification, And Reporting (OSCAR) files, and Area Resource Files are used. Our sample consists of all non-governmental nursing homes in Maryland from 2007 to 2010. Consumer ratings were reported for: overall care; recommendation of the facility; staff performance; care provided; food and meals; physical environment; and autonomy and personal rights. We identified chain characteristics from OSCAR, and estimated multivariate random effect linear models to test the effects of chain ownership on care experience ratings.
Results
Independent nonprofit nursing homes have the highest overall rating score of 8.9, followed by 8.6 for facilities in small nonprofit chains, and 8.5 for independent for-profit facilities. Facilities in small, medium and large for-profit chains have even lower overall ratings of 8.2, 7.9, and 8.0, respectively. We find similar patterns of differences in terms of recommendation rate, and important areas such as staff communication and quality of care.
Conclusions
Evidence suggests that Maryland nursing homes affiliated with large- and medium- for-profit chains had lower ratings of family reported experience with care.
Keywords: nursing home chain, care experience, satisfaction
Introduction
Poor quality of nursing home care has been a long-standing concern,1 with numerous recent studies continuing to report serious quality and safety deficits such as high-stage pressure ulcers for long-stay residents,2,3 high rates of preventable hospital transfers of residents,4-6 and potentially inappropriate medication use.7 Existing literature also suggests that quality-of-care problems are generally more pronounced in for-profit facilities and facilities owned by corporate chains.8-13 Since the 1990s, multi-facility chains have undergone considerable transformations nationally while comprising a sizeable portion of the nursing home market. In 2012, 55 percent of the nation's 15,654 nursing homes facilities were operated by corporate chains.
The current literature on nursing home chain performance, with few exceptions,10,12 compares chain-affiliated facilities to non-chain facilities relying on the dichotomous definition routinely-available in the Online Survey of Certification And Reporting (OSCAR) files and ignores the heterogeneity of chain organizations. Another potential shortcoming of the current literature is that no prior studies have investigated the potential impact on more person-centered measures such as consumer reported experience with care. It has been increasingly recognized that delivering person-centered care is a critical component of high-quality health care.14 In nursing homes specifically, promoting resident-centered care is integral to improved resident quality of life, resident autonomy, and engagement of residents and families in care decisions.15-18 In recognizing the importance of person-centeredness in nursing homes, several states recently initiated resident and/or family member surveys on care experiences and publicly reported facility-level rating scores on state websites.17
This study performed longitudinal analyses on published reports of care experiences in Maryland nursing homes during 2007-2010, and determined the associations of chain characteristics (ownership, chain size, and proprietary status) and family member reported rating scores.
Methods
Data
Data come from three sources including (1) the national OSCAR files that provide nursing home characteristics. We coded nursing home chains in OSCAR to allow monitoring chain ownership types; (2) Maryland nursing home experience with care reports; and (3) Area Resource Files (ARFs) to define county (market) characteristics. All data were obtained annually from 2007 to 2010.
The OSCAR maintained and updated by the Centers for Medicare and Medicaid is generally believed to be reliable for research purposes and widely used for quality evaluations and policy analyses.9-12 The OSCAR data include a binary variable identifying whether a nursing home belongs to a chain and names of the multi-facility chains. We identified chains nationally and their affiliated homes based on reported corporate names. We coded chain ownership through line-by-line inspection of the records in multiple years' data, and addressed inconsistencies by comparing name spelling and inter-temporal relationships in specific nursing homes. In our analyses, we defined chains as those that owned at least two nursing facilities nationally in a given calendar year.
The Maryland Health Care Commission started the annual nursing home satisfaction surveys and public reporting in 2007. Each year, approximately 17,000 surveys were mailed to adult children or spouses of the residents with length-of-stay ≥90 days, with annual response rates ranging from 55 to 60 percent. During each year's survey, roughly two thirds of the respondents visited the nursing home ≥20 times, and 80% visited the nursing home ≥10 times within 6 months before the survey.19-23 Two separate questions were asked every year for (1) overall rating of care on a scale from 1 (worst) to 10 (best); and (2) whether the respondent would recommend the facility to someone he/she knows who need nursing home care (yes/no). In addition, five domains of care were evaluated by respondents, focusing on (3) staff and administration, (4) care provided to residents, (5) food & meals, (6) autonomy & resident rights, and (7) physical aspects of the facility. Each domain contained several questions that rated care experience on a scale of 1 to 4 and the rating of each domain was then calculated as the average of the scores of all questions within the domain. See previous reports for more details.18-22
Sample and variables
We included all Maryland for-profit and nonprofit nursing homes that served long-term residents (n=213), excluding 25 government-owned facilities and 13 hospital-affiliated facilities. The 213 included facilities constituted 820 facility-year observations over the period of 2007-2010.
The dependent variables were overall and domain-specific rating scores for each nursing home in each study year (2007-2010). To define the independent variables, we first categorized identified chains into 3 groups in each year: small chains (with 2-10 facilities), medium chains (11-70 facilities), and large chains (>70 facilities). We then defined 6 dummies as independent variables that categorized nursing homes as (1) independent nonprofit facilities, (2) independent for-profit facilities, (3) nonprofit facilities in small chains, (4) for-profit facilities in small chains, (5) for-profit facilities in medium chains, and (6) for-profit facilities in large chains. There were no nonprofit nursing homes in medium or large chains in Maryland. Numbers of facilities in each chain category in each year are described in Appendix Table 1.
We obtained the following annually defined nursing home covariates which may be associated with consumer ratings according to previous reports:17,19-23 total number of beds, occupancy rate, a case mix index derived from the RUG (resource utilization group) III classification of residents;24 percentage of Medicaid residents, percentage of Medicare residents, percentage of non-Hispanic white residents; staffing levels (hours per resident per day) for registered nurse (RN), licensed practical or vocational nurse (LPN/LVN), and certified nursing assistant; number of deficiency citations received during annual inspection, and if the nursing home is located in a rural area as defined by the rural urban commuting area (RUCA) file.25 County-level covariates included market competition defined based on the Herfindahl–Hirschmann Index, the median household income of residents in the county, and the percentage of older adult population (≥ 65 years) in the county.
Analyses
We performed bivariate analyses on overall and domain-specific care rating scores, other nursing home characteristics, and county covariates, across the 6 ownership groups defined above. We used analyses of variance for continuous variables and chi-square tests for categorical variables in statistical inference. Only annual data of 2010 are used in bivariate analyses.
To test differences in rating scores across ownership groups (independent nonprofit nursing homes as reference), we estimated a set of multivariate linear models, one for each rating, where we controlled for facility random-effects,26 nursing home and county covariates described above, year dummies (2007 omitted), and the within facility clustering of satisfaction scores using the Huber-White robust estimates of standard errors.27 Facility and resident characteristics are adjusted because they influence care ratings independent of ownership. For example, resident case-mix was adjusted for primarily to control for the differences in its impact on the underlying care quality; resident's characteristics, such as cognitive performance are very likely to influence their evaluation of nursing home care. Facility fixed-effects were not estimated because ownership groups were largely time invariant. We obtained adjusted rating scores based on model predictions, and presented adjusted ratings stratified by ownership groups.
Results
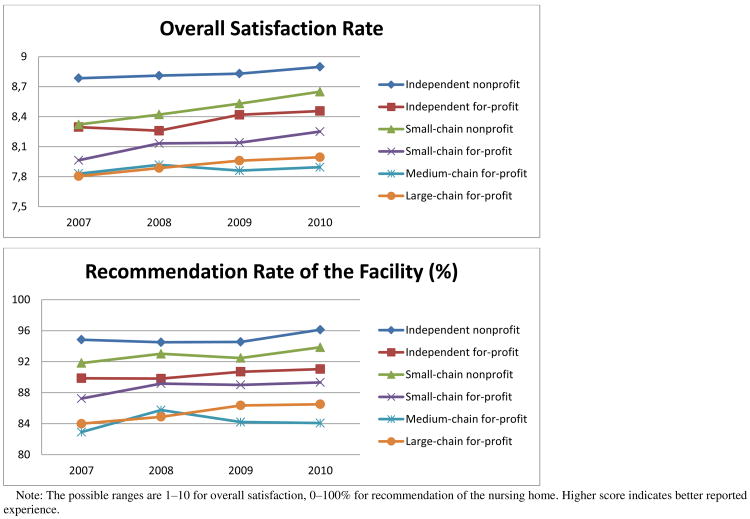
Table 1 presents results of bivariate comparisons across all six ownership groups in 2010, and Figure 1 depicts the overall satisfaction and recommendation rate for these groups of all included Maryland nursing homes in 2007-2010. Compared to independent nonprofit facilities (or small-chain facilities), facilities belonging to chains (or larger chains) generally had more beds, higher percentage of Medicare residents, lower percentage of white residents, lower staffing levels for CNAs, and more deficiency citations; chain-owned facilities and those owned by larger chains also tended to be in urban areas (Table 1).
Table 1. Descriptive statistics of Maryland nursing homes, 2010, by nursing home ownership type.
| Independent, nonprofit |
Independent, for-profit |
Small-chain, nonprofit |
Small-chain, for-profit |
Medium-chain, for-profit |
Large-chain, for-profit |
p-value | |
|---|---|---|---|---|---|---|---|
| Number of Nursing Homes | 46 | 37 | 14 | 20 | 30 | 55 | |
| Nursing home characteristic | |||||||
| Experience with care rating | |||||||
| Overall satisfaction (1-10), mean | 8.90 | 8.46 | 8.65 | 8.25 | 7.89 | 7.99 | < 0.01 |
| Recommendation rate (0-100), % | 96.12 | 91.04 | 93.85 | 89.32 | 84.07 | 86.50 | < 0.01 |
| Staff & administration (1-4), mean | 3.77 | 3.69 | 3.71 | 3.66 | 3.61 | 3.62 | < 0.01 |
| Care provided (1-4), mean | 3.66 | 3.56 | 3.58 | 3.51 | 3.42 | 3.43 | < 0.01 |
| Food & meals (1-4), mean | 3.61 | 3.60 | 3.51 | 3.45 | 3.37 | 3.38 | < 0.01 |
| Autonomy (1-4), mean | 3.71 | 3.50 | 3.66 | 3.47 | 3.42 | 3.43 | < 0.01 |
| Physical aspects (1-4), mean | 3.59 | 3.48 | 3.51 | 3.42 | 3.32 | 3.29 | < 0.01 |
| Total number of beds, mean | 116.33 | 126.19 | 120.29 | 95.90 | 145.13 | 141.95 | 0.05 |
| Occupancy rate, % | 87.01 | 89.35 | 85.88 | 92.45 | 84.79 | 86.74 | 0.17 |
| Case mix index score, mean | 0.82 | 0.85 | 0.85 | 0.84 | 0.87 | 0.88 | < 0.01 |
| Percentage of Medicaid residents, % | 48.32 | 59.52 | 50.82 | 60.86 | 69.66 | 64.85 | < 0.01 |
| Percentage of Medicare residents, % | 11.92 | 14.95 | 15.84 | 16.84 | 16.62 | 19.66 | < 0.01 |
| Percentage of White residents, % | 83.52 | 70.38 | 73.51 | 69.66 | 58.16 | 60.16 | < 0.01 |
| Staff hours per resident per day, mean | |||||||
| Registered nurse | 0.42 | 0.40 | 0.46 | 0.38 | 0.33 | 0.55 | < 0.01 |
| Licensed practical/vocational nurse | 0.95 | 0.85 | 0.80 | 0.92 | 1.05 | 0.97 | 0.05 |
| Certified nursing assistance | 2.44 | 2.29 | 2.37 | 2.03 | 1.97 | 1.67 | < 0.01 |
| Number of deficiencies, mean | 9.49 | 12.13 | 10.46 | 11.71 | 14.04 | 11.70 | 0.13 |
| Rural location, % | 23.91 | 18.92 | 14.29 | 15.00 | 10.00 | 7.27 | 0.26 |
| County characteristic | |||||||
| Market competition, mean | 0.86 | 0.87 | 0.87 | 0.86 | 0.88 | 0.89 | 0.96 |
| Medium household income × $1k, mean | 64.49 | 66.59 | 74.13 | 64.04 | 64.23 | 67.48 | 0.54 |
| Percentage population ≥ 65 yrs, % | 13.40 | 13.33 | 12.95 | 13.76 | 12.54 | 12.76 | 0.56 |
Note: p-values were calculated from analyses of variance for continuous variables, and chi-square test for categorical variables when comparing group differences.
Figure 1.
Overall satisfaction and recommendation rate of all Maryland nursing by chain ownership size and proprietary status during 2007-2010.
Independent nonprofit facilities tended to have the highest scores for both overall ratings and ratings on specific domains of care. Specifically, Figure 1 suggests that both overall satisfaction and recommendation ratings have been increasing over the study years and that the ratings of the independent nonprofit group were higher than other groups. Chain-owned facilities tended to have lower scores than independent facilities, and nonprofit facilities generally performed better than for-profit ones, confirming results of previous studies.17-19 Moreover, chain-owned facilities were heterogeneous with larger chain size of the affiliated facilities associated with lower rating scores. As shown in Table 1, the average overall satisfaction scores were 8.9 (range: 6.6-9.9) for independent nonprofit facilities, 8.5 (range: 6.6-9.7) for independent for-profit facilities, 8.6 (range: 7.2-9.7) for facilities in small nonprofit chains (14 facilities in 6 chains), 8.2 (range: 7.0-9.5) for facilities in small for-profit chains (20 facilities in 9 chains), 7.9 (range: 6.5-9.1) for facilities in medium for-profit chains (30 facilities in 10 chains), and 8.0 (range: 6.3-8.9) for facilities in large for-profit chains (55 facilities in 6 chains).
Multivariate analyses controlling for nursing home and county covariates, facility random effects, and clustering suggested that chain-owned facilities, especially those owned by larger chains (which were exclusively for-profit in Maryland), are associated with significantly lower scores of overall and specific areas of care. For example, the predicted overall satisfaction scores were 8.8 for independent nonprofit facilities and 7.9 for large-chain-owned facilities (p<0.01 for difference), while the predicted recommendation rates were 95% and 85% for the two groups (p<0.01) (Table 2). Similar results were found in important areas such as staff communication and quality of care. The Appendix Table 2 provides the full multivariate analyses results.
Table 2. Adjusted experience with care ratings by nursing home chain ownership groups, 2007-2010#.
| Ownership group of nursing homes | Overall satisfaction (1-10) | Recommendation (0-100) | Experience with (1-4) | ||||
|---|---|---|---|---|---|---|---|
| Staff & administration | Care provided | Food & meals | Autonomy | Physical environment | |||
| Independent nonprofit (N=191) | 8.80 | 94.99 | 3.71 | 3.61 | 3.61 | 3.57 | 3.55 |
| Independent for-profit (N=176) | 8.34*** | 89.99*** | 3.63** | 3.50*** | 3.57 | 3.41*** | 3.41*** |
| Small-chain, nonprofit (N=54) | 8.52 | 93.20 | 3.64** | 3.54** | 3.48** | 3.52 | 3.45* |
| Small-chain for-profit (N=86) | 8.11*** | 88.76*** | 3.59*** | 3.44*** | 3.44*** | 3.33*** | 3.35*** |
| Medium-chain for-profit (N=102) | 7.90*** | 84.87*** | 3.56** | 3.40*** | 3.40*** | 3.31*** | 3.29*** |
| Large-chain for-profit (N=211) | 7.92*** | 85.61*** | 3.56*** | 3.39*** | 3.39*** | 3.32*** | 3.25*** |
Predictions of adjusted ratings were based on linear random-effects models that adjusted for the nursing home and county characteristics listed in Table 1, year dummies, dummies for facility ownership groups, and the clustering of nursing homes over years.
p<0.10,
p<0.05, and
p<0.01 when compared to the adjusted rating of independent nonprofit facilities.
Discussion
Our analyses of Maryland nursing homes during 2007-2010 found that compared to independent nonprofit facilities, facilities owned by chain organizations, especially large- and medium-sized for-profit chains, had lower overall satisfaction with care and worse experiences with care in important areas such as staff communication and respect for resident autonomy. Differences in family-reported ratings persist after controlling for important quality indicators as well as other nursing home and market characteristics.
Although previous studies have suggested that nursing homes owned by for-profit chains may have worse resident outcomes and quality of care,9-13 the present study contributes to the literature by showing that chain-owned facilities are heterogeneous regarding important nursing home characteristics (e.g., Medicare census, racial composition of residents, staffing), and especially regarding family-reported experience of care. Given such patterns of differences among chain organizations, most prior studies that lump all chain-owned facilities into a single group, may have under-estimated the “chain” effect for large-chain owned facilities and over-estimated it for small-chain owned facilities.
Our results of the particularly low family-reported care experiences for residents in facilities of medium and large for-profit chains may reveal that these nursing homes provide low quality of care. A recent study on Maryland nursing home found that higher family ratings are associated with risk-adjusted quality measures,30 including but not limited to nursing staffing and deficiency citations. Therefore, it is possible that residents reporting low satisfaction ratings in facilities of medium and large for-profit chains receive worse quality of care and have worse outcomes. Moreover, nursing homes owned by large companies show complex ownership and corporate structures which may affect the day-to-day operation of facilities in important ways.31 Some investigators have raised concerns that nursing home chains, especially medium and large for-profit chains, may pursue corporate interests over resident needs and employ various strategies to maximize shareholder and investor returns at the expense of resident care.11-12
More information is needed to fully understand why medium and large chain-owned for-profit facilities are associated with lower family reported ratings. Yet, the ownership information currently available in OSCAR remains too limited to allow for causality studies. Our results provide further evidence about the value of expanded collection and disclosure of such additional ownership information for facilities of large corporations, as required by the Affordable Care Act (ACA) of 2010.32
The study has several limitations. First, our analyses focused on nursing homes and corporate chains in Maryland and results may or may not generalize to other parts of the country. Second, recall bias and non-response bias may be concerns when using consumer surveys although the Maryland nursing home family care experience surveys achieved consistently high response rates over years. 28,29 Third, our multivariate analyses comparing care experience scores over facility groups relied largely on cross-sectional identification of ownership types, and we cannot totally rule out bias due to unobserved factors that are correlated with both chain ownership and the outcomes. For example, Culture Changes, which were more likely to be implemented in nonprofit and in independent facilities, were found to have impacted clinical outcomes, quality of care, quality of life, and other resident and staff outcomes. 33, 34
In summary, our longitudinal analyses found that affiliation with large for-profit chains of Maryland nursing homes was associated with lower rating scores of family-reported experiences with care. Future studies are necessary to better understand how the complex ownership structures of large corporations may affect nursing home quality and resident welfare.
Supplementary Material
Appendix Table 1: Number of nursing homes (chains) in our sample, by ownership type and year.
Appendix Table 2: Linear random-effects regression results of care ratings by nursing home chain ownership groups, 2007-2010
Acknowledgments
This study is funded by the National Institute on Aging (NIA) under grant R01AG042418. The views expressed in this article are those of the authors and do not necessarily represent the views of the NIA of the NIH. Dr. Stevenson's time was supported by NIH-NIA K01 AG038481.
Footnotes
Conflicts of Interests: no conflict of interest for any author.
References
- 1.Wunderlich GS, Kohler PO, editors. Improving the quality of care in nursing homes. Washington, DC: National Academies Press; 2001. [PubMed] [Google Scholar]
- 2.Li Y, Yin J, Cai X, Temkin-Greener J, Mukamel DB. Association of race and sites of care with pressure ulcers in high-risk nursing home residents. JAMA. 2011 Jul 13;306(2):179–186. doi: 10.1001/jama.2011.942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mor V, Gruneir A, Feng Z, Grabowski DC, Intrator O, Zinn J. The effect of state policies on nursing home resident outcomes. Journal of the American Geriatrics Society. 2011 Jan;59(1):3–9. doi: 10.1111/j.1532-5415.2010.03230.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Intrator O, Grabowski DC, Zinn J, et al. Hospitalization of nursing home residents: the effects of states' Medicaid payment and bed-hold policies. Health Serv Res. 2007 Aug;42(4):1651–1671. doi: 10.1111/j.1475-6773.2006.00670.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Walsh EG, Wiener JM, Haber S, Bragg A, Freiman M, Ouslander JG. Potentially avoidable hospitalizations of dually eligible Medicare and Medicaid beneficiaries from nursing facility and Home- and Community-Based Services waiver programs. J Am Geriatr Soc. 2012 May;60(5):821–829. doi: 10.1111/j.1532-5415.2012.03920.x. [DOI] [PubMed] [Google Scholar]
- 6.Ouslander JG, Berenson RA. Reducing unnecessary hospitalizations of nursing home residents. N Engl J Med. 2011 Sep 29;365(13):1165–1167. doi: 10.1056/NEJMp1105449. [DOI] [PubMed] [Google Scholar]
- 7.Chen Y, Briesacher BA, Field TS, Tjia J, Lau DT, Gurwitz JH. Unexplained variation across US nursing homes in antipsychotic prescribing rates. Arch Intern Med. 2010 Jan 11;170(1):89–95. doi: 10.1001/archinternmed.2009.469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grabowski DC, Hirth RA. Competitive spillovers across non-profit and for-profit nursing homes. J Health Econ. 2003 Jan;22(1):1–22. doi: 10.1016/s0167-6296(02)00093-0. [DOI] [PubMed] [Google Scholar]
- 9.Stevenson DG, Grabowski DC. Private equity investment and nursing home care: is it a big deal? Health Aff (Millwood) 2008 Sep-Oct;27(5):1399–1408. doi: 10.1377/hlthaff.27.5.1399. [DOI] [PubMed] [Google Scholar]
- 10.Harrington C, Olney B, Carrillo H, Kang T. Nurse staffing and deficiencies in the largest for-profit nursing home chains and chains owned by private equity companies. Health Serv Res. 2012 Feb;47(1 Pt 1):106–128. doi: 10.1111/j.1475-6773.2011.01311.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Harrington C, Woolhandler S, Mullan J, Carrillo H, Himmelstein DU. Does investor ownership of nursing homes compromise the quality of care? Am J Public Health. 2001 Sep;91(9):1452–1455. doi: 10.2105/ajph.91.9.1452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Banaszak-Holl J, Berta WB, Bowman DM, Baum J, Mitchell W. The rise of human service chains: Antecedents to acquisitions and their effects on the quality of care in US nursing homes. Managerial and Decision Economics. 2002;23:261–282. [Google Scholar]
- 13.U.S. Government Accountability Office. Nursing homes: Private investment homes sometimes differed from others in deficiencies, staffing, and financial performance. GAO-11-571; Washington, DC: 2011. [Google Scholar]
- 14.Institute of Medicine. Crossing the quality chasm: A new health system for the 21st century [Internet] 2001 Available from: http://www.iom.edu/Reports/2001/Crossing-the-Quality-Chasm-A-New-Health-System-for-the-21st-Century.aspx. [PubMed]
- 15.Koren MJ. Person-centered care for nursing home residents: the culture-change movement. Health Aff (Millwood) 2010 Feb;29(2):312–317. doi: 10.1377/hlthaff.2009.0966. [DOI] [PubMed] [Google Scholar]
- 16.Frentzel EM, Sangl JA, Evensen CT, et al. Giving Voice to the Vulnerable: The Development of a CAHPS Nursing Home Survey Measuring Family Members' Experiences. Med Care. 2012 Nov;50(Suppl):S20–27. doi: 10.1097/MLR.0b013e31826b1068. [DOI] [PubMed] [Google Scholar]
- 17.Li Y, Cai X, Ye Z, Glance LG, Harrington C, Mukamel DB. Satisfaction with massachusetts nursing home care was generally high during 2005-09, with some variability across facilities. Health Aff (Millwood) 2013 Aug;32(8):1416–1425. doi: 10.1377/hlthaff.2012.1416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li Y, Ye Z, Glance LG, Temkin-Greener H. Trends in family ratings of experience with care and racial disparities among Maryland nursing homes. Med Care. 2014 Jul;52(7):641–648. doi: 10.1097/MLR.0000000000000152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Calikoglu S, Christmyer CS, Kozlowski BU. My Eyes, Your Eyes-The Relationship between CMS Five-Star Rating of Nursing Homes and Family Rating of Experience of Care in Maryland. J Healthc Qual. 2011 Aug 29; doi: 10.1111/j.1945-1474.2011.00159.x. [DOI] [PubMed] [Google Scholar]
- 20.Maryland Health Care Commission and Market Decisions, LLC. 2008 Maryland nursing facility family survey: Statewide report. 2009 Mar; [Google Scholar]
- 21.Maryland Health Care Commission and Market Decisions, LLC. 2009 Maryland nursing facility family survey: Statewide report. 2010 Feb; [Google Scholar]
- 22.Maryland Health Care Commission and Macro International Inc. 2010 Maryland nursing facility family survey: Statewide report. 2011 Apr; [Google Scholar]
- 23.Kozlowski BU, Christmyer CS. Maryland nursing home family survey; presented at the 11th CAHPS and 1st SOPS user group meeting on December 3-5, 2008. 2008 [Google Scholar]
- 24.Intrator O, Hiris J, Berg K, Miller SC, Mor V. The residential history file: studying nursing home residents' long-term care histories. Health Serv Res. 2011 Feb;46(1 Pt 1):120–137. doi: 10.1111/j.1475-6773.2010.01194.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rural health research center RUCA data version 2.0. [Accessed on September 19, 2013];2005 Available at http://depts.washington.edu/uwruca/ruca-data.php.
- 26.Hsiao C. Analysis of panel data 2nd version. Cambridge University Press; 2003. [Google Scholar]
- 27.White H. A heteroskedasticity-consistent covariance matrix estimator and a direct test for heteroskedasticity. Econometrica. 1980;48:817–830. [Google Scholar]
- 28.Castle NG. Family members as proxies for satisfaction with nursing home care. Jt Comm J Qual Patient Saf. 2006 Aug;32(8):452–458. doi: 10.1016/s1553-7250(06)32059-4. [DOI] [PubMed] [Google Scholar]
- 29.Gasquet I, Dehe S, Gaudebout P, Falissard B. Regular visitors are not good substitutes for assessment of elderly patient satisfaction with nursing home care and services. J Gerontol A Biol Sci Med Sci. 2003 Nov;58(11):1036–1041. doi: 10.1093/gerona/58.11.m1036. [DOI] [PubMed] [Google Scholar]
- 30.Li Y, Li Q, Tang Y. Associations Between Family Ratings on Experience With Care and Clinical Quality-of-Care Measures for Nursing Home Residents. Medical Care Research and Review. 2015 doi: 10.1177/1077558715596470. 1077558715596470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.U.S. Government Accountability Office. Nursing homes: Complexity of private investment purchases demonstrates need for CMS to improve the usability and completeness of ownership data. GAO-10-710; Washington, DC: 2010. [Google Scholar]
- 32.Public Law No. 111-148, 6101, 124 Stat. 119, 699.
- 33.Grabowski DC, O'Malley AJ, Afendulis CC, Caudry DJ, Elliot A, Zimmerman S. Culture change and nursing home quality of care. The Gerontologist. 2014;54(Suppl 1):S35–S45. doi: 10.1093/geront/gnt143. [DOI] [PubMed] [Google Scholar]
- 34.Grabowski DC, Elliot A, Leitzell B, Cohen LW, Zimmerman S. Who are the innovators? Nursing homes implementing culture change. The Gerontologist. 2014;54(Suppl 1):S65–S75. doi: 10.1093/geront/gnt144. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix Table 1: Number of nursing homes (chains) in our sample, by ownership type and year.
Appendix Table 2: Linear random-effects regression results of care ratings by nursing home chain ownership groups, 2007-2010