Abstract
The Family Check Up (FCU) is a family-centered intervention for reducing children's problem behavior through improving parenting skills and family interactions. Although the FCU was designed to prevent conduct problems, we have also found the program to be effective in preventing escalating symptoms of depression in early adolescence. The current analyses examine heterogeneous patterns of response to treatment in an effort to identify factors associated with differential response to family intervention. We examined heterogeneity in trajectories of youth-reported depressive symptoms from grades 6 to 9, using a Latent Growth Mixture Modeling framework to identify patterns of treatment response and non-response. Three symptom trajectories were identified, including the following: 1) a large class exhibiting stable, low symptom levels, 2) a class exhibiting high and stable depressive symptoms, and 3) a class exhibiting low initial symptoms that increased over time. Significant intervention effects were identified only among the third class, as a preventive effect on depression from 7th to 9th grade for youth with low initial symptoms. No effect of intervention was observed in the other two classes. Comparisons of classes 2 and 3 suggested that class 3 members were more likely to be females with high baseline antisocial behavior, but lower initial levels of depression. The findings suggest the importance of exploring heterogeneity within a prevention design, as well as the importance of tailored approaches to the prevention of adolescent depression.
Keywords: depression, conduct disorder, prevention, parenting
Introduction
By the age of 18, nearly 20 to 25% of teens will experience a major depressive episode (Kessler, Avenevoli, & Merikangas, 2001), with particularly high rates of depression in girls following the transition into adolescence (e.g. Hyde, Mezulis, & Abramson, 2008). As such, a sizeable literature has examined psychosocial prevention and intervention efforts for depressed children and adolescents, with prevention and intervention studies differing primarily in whether youth are already experiencing depression or are at high risk for developing depression (see Horowitz & Garber, 2006). Most of these studies have focused on efforts to intervene directly with children and adolescents, seen either individually or in groups. Several such youth-focused programs have received empirical support, most of which are based upon cognitive behavioral therapy principles (CBT; see Horowitz & Garber, 2006), which focus on helping youth develop cognitive, problem solving, and coping skills to alleviate depression. While such strategies are effective for many youth, there is substantial room for improvement. Effect sizes are generally small-to-moderate (Sandler, Wolchick, Cruden, Mahrer, Ahn, Brincks, & Brown, 2014), nearly 40% of youth do not benefit from such child-directed intervention approaches and substantial relapse rates are seen for those that do (e.g. Birmaher et al., 2000), and few studies (e.g. Beardslee et al., 2013) include long-term follow-up data to demonstrate the durability of effects.
One potential avenue for improvement is to expand the focus to target family functioning. A large developmental literature has highlighted the association between youth depression and problems in parenting and family functioning, including low levels of parental warmth and support, high levels of parental criticism and negative affect, elevated levels of parental psychopathology, and high levels of family conflict and stress (see Sheeber, Hops, & Davis, 2001). Further, a number of studies have found that poorer response to child-focused intervention approaches is related to problems in family functioning, including maternal depression, parent-child conflict, low levels of parental support, and high levels of parental criticism (e.g. Asarnow, Goldstein, Thompson & Guthri, 1993; Brent et al, 1998; Birmaher et al., 2000; Lewinsohn & Clarke, 1984). Yet efforts to improve parenting and family relationships have been relatively understudied in the prevention and intervention literature for depression.
Stark and colleagues (2012) reviewed studies of youth-focused programs that included at least some parent or family sessions. The intensity and focus of such sessions varied widely, from brief psychoeducation efforts (e.g. Brent et al., 1997) to parent sessions (generally between 2 – 6 sessions) in parallel to youth-only sessions (e.g. Garber et al., 2009; Schochet et al., 2001) to more directly family-focused sessions (e.g. Compas et al., 2009). Engaging parents into such adjunctive treatments emerged as one common challenge. For instance, Schochet and colleagues (2001) offered 3 sessions of parent-training in addition to an 11-session teen-focused prevention program, and found that only 10% of families took part in all 3 sessions. Not surprisingly, such studies have yielded limited evidence of the incremental benefits to youth of such adjunctive parenting sessions. Stark and colleagues (2012) concluded that family-focused interventions appeared promising, but that additional work examining their relative benefits was needed.
While family-focused programs for youth depression have received increased attention in recent years, such programs are much better established for externalizing disorders in youth. However, many family risk processes are common across conduct problems and depression, including high levels of family stress and conflict, low levels of parental warmth and support, and hostile and coercive parent-child interactions (Dishion & Patterson, 2006). Similarly, the dual-failure model (Patterson & Stoolmiller, 1991) highlights that conduct problems may predict increased peer rejection and academic difficulties, which in turn predict increased depression. In line with the overlap between conduct problems and depression, several studies have found that parent-focused prevention programs designed for youth conduct problems lead to reductions in depression, as well (e.g. Mason et al., 2007; Trudeau, Spoth, Randall, & Azevedo, 2007), and parenting programs have been found to yield larger effect sizes for reducing internalizing than externalizing problems (e.g. Kaminski, Valle, Filene, & Boyle, 2008). Thus, the extensive literature on parent-focused interventions designed to reduce youth conduct problems may have implications for augmenting depression-focused prevention efforts.
The current study examines the effects of the Family Check Up program (FCU; see Dishion & Stormshak, 2007), a multilevel, family-focused prevention program delivered within a public middle-school setting on reductions in youth depressive symptoms across grades 6 through 9. The program follows an adaptive intervention framework (Collins, Murphy and Bierman, 2004), in which treatment targets and doses are tailored to the individual needs of families. Advantages of adaptive designs include more efficient use of resources, increased treatment compliance and intervention potency, greater resemblance to real-world clinical practice, and decreased chances of negative effects of intervention components that are inappropriate for a given individual (e.g. Collins, Murphy, & Bierman, 2004). At the core of the intervention is the FCU assessment, a brief, three session intervention designed to identify potential targets for intervention, to support parent's motivation to engage in effective family management practices, and to provide more intensive support for parents and youth in need (Dishion & Stormshak, 2007). The focus on parental motivation to engage with treatment may be particularly relevant in the context of treating depression, as parental engagement with depression-focused treatments has proven to be problematic across a number of studies (e.g. Schochet et al., 2001; Stein et al, 2001). Indeed, a prior study examining FCU program outcomes in a separate sample (Connell & Dishion, 2008) found that random assignment to the intervention predicted significantly decreased growth in depressive symptoms from 6th – 8th grade among high-risk youth (determined via teacher-report) by both youth and mother report.
The current analyses use data from a school-based prevention trial of youth followed-from grades 6 through 9. The goals of this study were to refine the FCU model to enhance its cultural sensitivity and target broader aspects of youth functioning, as well as to increase the rate of family engagement with the FCU assessment (see Stormshak et al., 2011). In addition to depression, the FCU program has been shown to predict reductions in conduct problems, substance use and family conflict, as well as improvements in academic functioning across grades 6 – 9 (Connell et al., 2007; Stormshak, Connell, & Dishion, 2009; Van Ryzin, Stormshak, & Dishion, 2012). The current analyses sought to examine variability in responsiveness to the FCU across families, which may help to identify ways to improve program effectiveness. We employed a latent growth mixture modeling approach to identify heterogeneous trajectories of depression symptoms from grades 6 to 9, and to examine variability in intervention response across the identified trajectory groups. Most research on variation in intervention impact has employed regression-based moderation analyses to identify variables associated with stronger treatment response, identifying several such factors, including maternal depression (Brent et al., 1998), problematic relationships with parents (Birmaher et al., 2000, Asarnow et al., 1993; Lewinsohn & Clarke, 1984), and baseline symptom severity (Mufson, Dorta, Wickramaratne, Nomura, Olfson, & Weissman,2004; Rohde, Lewinsohn, & Seeley, 1994; Brent et al., 1998).
While this approach has yielded important insights, one limitation is that its focus is on the identification of variables associated with the magnitude of treatment response. However, researchers may be more interested in identifying subpopulations with different responses to intervention strategies that are best characterized by a cluster of characteristics. The mixture modeling approach provides a robust method of empirically identifying subgroups of individuals who differ with respect to symptom trajectories and patterns of covariates, and the opportunity to examine variation in responsiveness to intervention across these subgroups (see Muthén, et al., 2002). Studies examining heterogeneity in depressive symptom trajectories in youth have consistently identified several distinct trajectory classes, including a large subgroup of youth exhibiting stable low symptom levels across time, and a smaller subset of youth exhibiting early-onset symptoms that remain high across time (e.g. Brendgen et al., 2005; Yaroslovsky, Pettit, Lewinsohn, Seeley, & Roberts, 2013). Some studies have also identified groups of youth exhibiting increasing or decreasing symptoms across adolescence (e.g. Brendgen et al., 2005; Wickrama & Wickrama, 2010). Several variables have been found to discriminate elevated trajectory classes relative to the stable low class, including female gender, high stress, problematic relationships with parents, co-occurring delinquent behavior, and co-occurring substance use (Yaroslavsky et al., 2013). Such developmental heterogeneity presents a challenge for prevention research, as children with different developmental profiles may have different intervention needs with respect to the timing or targets of intervention. As such, the examination of intervention effects across youth following heterogeneous trajectories of depression development is consistent with an adaptive intervention framework.
In line with prior research, we expected to identify at least stable-low and stable-high trajectory classes, as well as subgroups of youth exhibiting increasing and decreasing symptoms across adolescence, and that groups showing elevated symptoms would be discriminated from the stable-low group by a greater proportion of females, elevated family conflict, co-occurring antisocial behavior, academic difficulties, and peer relational problems at baseline. We considered three competing hypotheses regarding the effects of intervention across subgroups of youth. First, a severity hypothesis holds that the intervention may be most effective for youth with the most severe symptoms at baseline, which would be those following an early-onset trajectory. Youth with such persistent and severe symptoms may show the highest levels of baseline family and peer risk, and may have the greatest room for improvement following treatment. Several treatment studies have examined this possibility, although results have been mixed, with two studies finding some support for heightened treatment response among youth with the highest baseline symptoms (Mufson et al, 2004; Rohde, Lewinsohn, & Seeley, 1994), but two others finding the opposite pattern of response (Brent et al, 1998; Jayson et al, 1998). Second, a timing hypothesis holds that the timing of intervention relative to symptom onset may be critical, with intervention close to the period of onset being most effective. In the current study, this hypothesis suggests that the FCU program delivered in adolescence may be most effective for youth who are prone to develop symptoms in adolescence, but less effective for youth with earlier-onset symptoms. To date, we know of no prior intervention research testing this possibility, although research has shown that the timing of risk exposure is more important that the types of risks for discriminating early-onset versus later onset depression (Shanahah, Copeland, Costello, & Angold, 2011). Third, a generalized effects hypothesis holds that the effects of the intervention will be stable across heterogeneous groups of youth, as family processes that are at the heart of the FCU program may be generally important despite differences in the age of onset or other etiological factors that may differentiate trajectory classes identified via mixture modeling techniques. We also examined differences across classes with respect to intervention engagement (i.e. receiving the FCU assessment and further services) to examine if variation in dosage might be associated with differential response to prevention.
Methods
Participants
Participants were 593 adolescents and their families recruited from three public middle schools in an urban area. The sample was 51% male and represented a wide variety of ethnic backgrounds (36% European American, 18% Hispanic/Latino, 15% African American, 7% Asian, 19% biracial/mixed identity, 2% Pacific Islander, 2% Native American). All families with a child in the sixth grade were invited to participate, with 80% agreeing to do so. The average age of participants was as follows: 11 years 10 months (wave 1), 13 years 1 month (wave 2), 14 years 1 month (wave 3), and 15 years (wave 4). 80% of participants’ fathers and 79% of mothers had attained at least a high school diploma. 65% of participating children reported feeling that their family had adequate financial resources. Families were randomly assigned to receive the intervention (N = 386; 65%) or “school as usual” (N = 207; 35%), using an unbalanced approach to increase the power to detect heterogeneous patterns of intervention effects.
Assessment procedures
Every spring from the sixth through the ninth grade, student participants completed a questionnaire in school, adapted from Metzler and colleagues (2001), which assessed a wide range of domains. If a child was absent or the family had moved out of the school district, assessments were mailed to the home. Students received $20 for each completed assessment.
Measures
Adolescent depressive symptoms
Depressive symptoms were assessed annually using a 14-item measure. Items reflected the frequency of symptoms such as feeling sad, moody, or hopeless and having trouble sleeping, with all diagnostic criteria for depression addressed by at least one item. Participants rated each symptom on a 5-point scale that ranged from “never or almost never” to “always or almost always” for the past month, and the average across items was used in analyses. This measure exhibits high internal reliability and convergent validity (Stormshak, Fosco, & Dishion, 2010; Klostermann, Connell, & Stormshak, in press). In addition, youth in the intervention condition completed the Child Depression Inventory (CDI) as part of the FCU assessment, and scores on the two scales were significantly correlated over time (r between .49 and .53 across waves). Cronbach's alpha was between 0.92 and 0.95 across time.
Adolescent antisocial behavior (6th grade)
Youth responded to 11 items assessing participation in activities during the past month, including lying, theft, physical fights, carrying weapons, and destroying property. Responses on the measure ranged from 0 (never) to 5 (more than 20 times), and the average was used in this study. Cronbach's alpha was 0.82.
Teasing by peers (6th grade)
Youth responded to 7-items reflecting the frequency with which they were teased for things like the clothing they wear or being a good student, over the past month. Each item was rated on a 5-point scale from “never” to “always” and the average across items was used in analyses. Cronbach's alpha was 0.81.
Peer deviance (6th grade)
Association with deviant peers was assessed using 5 items regarding how often they spent time with friends who in the past month had engaged in such behaviors as stealing, lying, and fighting. Items were rated on a 5-point scale from “never” to “more than 7 times,” and the average score was used in analyses. Cronbach's alpha was 0.86.
Family conflict (6th grade)
Youth reports of conflict with parents were measured by averaging across 4 items. Items assessed youths’ reports of how often someone in their family got mad and hit someone and how often they got their own way by getting angry. Responses ranged from 0 (never or almost never) to 5 (always or almost always). Cronbach's alpha was .82.
Academic performance (6th grade)
An estimate of each child's academic performance during the current school year was obtained with one item that asked the child to rate her performance on a 5-point scale, where 1 represented “mostly A's” and 5 represented “mostly F's.” There was also an option for “not in school,” although no participants endorsed this item. Scores on this item were significantly correlated with school-reports of standardized testing in math and reading subjects (correlations ranged from −.29 to-. 48, with youth reporting better grades scoring higher on standardized tests), supporting the validity of this measure.
Gender
The gender of the child was coded as 0 = male and 1 = female.
Ethnicity
Youth ethnicity was coded as 0 = ethnic minority and 1 = Caucasian.
Intervention Protocol
The current study used data from a randomized, multilevel, school-based prevention trial (see Dishion & Stormshak, 2007; Stormshak et al, 2011). The first level was the family resource center (FRC), which was established in each school and was available to all families assigned to the intervention condition. The FRC was staffed with a parent consultant (PC). PCs’ education levels ranged from doctoral to bachelor's degree and all had prior family intervention experience. PC ethnicity was matched with family ethnicity when possible. PCs included one Latino consultant fluent in Spanish, one African American consultant, and two European American consultants. Consultants were trained through a series of workshops including one week-long initial training and several follow-up training throughout the study, and received weekly supervision by a doctoral-level practitioner. PCs attended all important school meetings related to the child's behavior and gave parents feedback regarding the child's school attendance and performance. Through the FRC, brief consultations and special seminars were also available to parents on topics such as homework completion and teen supervision. The next level of the program was the FCU assessment, which is based on motivational interviewing principles (Miller & Rollnick, 2002), and included three sessions: an initial home visit and interview, an ecological assessment, and finally a feedback session in which options for further intervention services were discussed. While the FCU assessment was offered to all families in the intervention condition, families of children identified as high-risk via teacher report were specifically targeted for recruitment. In the intervention condition, 52% of families (n = 199) consulted with the parent consultant, 42% (n = 163) received the FCU (n = 138 in 7th grade, n = 23 in 8th grade, n = 2 in 9th grade), and 76 families completed the FCU a second time (n = 69 in 8th grade, n = 33 in 9th grade). Most families (n = 131) had contact with the FRC prior to completing the FCU assessment. Of the families completing the FCU, 79% received further services, centered on delivery of a parent-management program targeting parental positive reinforcement, limit setting, and communication skills (see Dishion & Stormshak, 2007).
Analytic Approach
Primary analyses were conducted using a General Growth Mixture Modeling (GGMM) framework, using Mplus 7.1 (Muthen & Muthen, 2013) to examine hypotheses regarding whether the effect of intervention varied across developmentally-heterogeneous subgroups of youth. All analyses used full information maximum likelihood estimation, which provides a method for accommodating missing data by estimating each parameter using all available data for that specific parameter. For depressive symptoms, 11.8 % of data was missing at wave 2, 14.4% at wave 3, and 18.7% at wave 4. Little's (1988) MCAR test indicated that the data was not MCAR (χ2[107] = 168.42, p < .05). Although there are no formal tests for the Missing at Random (MAR) assumption underlying the use of FIML, examination of the patterns of missing data in relation to covariates suggest the data are likely MAR. All models were run with 500 randomly-generated start values, run for 10 iterations, and the best fitting 100 random-start values were run to convergence. Excellent replication across random start-values was found. LGMM analyses followed the framework proposed by Muthen and colleages (2002) to examine differences in intervention effects across groups of youth following heterogeneous trajectories of depression. The first goal of the LGMM analysis was to determine the optimal number of trajectory classes. All models included intercept, slope, and quadratic slope parameters. Intervention effects and other potential covariates were not included in the process of determining the optimal number of classes, and fit indices were obtained for unconditional models with 1 – 6 classes (see Muthen et al., 2002). A number of model fit-indices were examined to determine the optimal number of latent classes. Relative model-fit indices included the Bayesian Information Criteria (BIC), and the sample-sized adjusted Bayesian Information Criteria (Adj BIC), with lower scores representing better-fitting models. Additionally, the Lo-Mendell-Rubin Likelihood Ratio Test (LMR-LRT; Lo, Mendell, & Rubin, 2001), and the Bootstrapped Likelihood Ratio Test (BLRT; McLachlan & Peel, 2004), provide statistical comparisons of the fit of a given model with a model of one fewer classes. Additional criteria for model selection are primarily informal, including entropy, a summary measure of the probability of membership in the most-likely class for each individual. Entropy values range from 0 to 1.0, and values closer to 1.0 represent better classification. Additionally, the usefulness and interpretability of latent trajectory classes should be considered, with the optimal model yielding a small number of distinct trajectory classes that are large enough to permit further testing. The best-fitting model was extended to include intervention assignment as a within-class covariate. Although such Intent To Treat analyses will lose some power because not everyone assigned to the intervention condition received the selected and indicated intervention (i.e. the FCU assessment), the logic of random assignment still means that this approach tests the effects of the broad intervention package. The regression coefficients were allowed to vary across classes, and the linear and quadratic slope parameters regressed on intervention status while the regression of the intercept on intervention status was fixed to 0. Additionally, we regressed latent class membership and within-class variation in growth parameters on baseline covariates.
Results
Descriptive Statistics
Descriptive statistics and correlations between variables are shown in Table 1. Preliminary analyses examined baseline predictors of family receipt of the FCU assessment within the intervention condition. Only baseline peer deviance was associated with receipt of the FCU, with lower baseline peer deviance in youth whose families received the FCU (mean = .54, SD = .89) than those whose families did not (mean = .71, SD = .96; F (1, 382) = 3.94, p = .05).
Table 1.
Correlations and descriptive statistics.
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Depression (6th grade) | -- | ||||||||||
| 2. Depression (7th grade) | .45* | -- | |||||||||
| 3. Depression (8th grade) | .34* | .51* | -- | ||||||||
| 4. Depression (9th grade) | .29* | .47* | .64* | -- | |||||||
| 5. Treatment assignment | −.01 | −.01 | .01 | .01 | -- | ||||||
| 6. Female gender | .06 | .19* | .30* | .25* | −.01 | -- | |||||
| 7. Ethnic minority family | .02 | −.04 | −.02 | −.09 | −.01 | −.05 | -- | ||||
| 8. Antisocial (6th grade) | .24* | .17* | .17* | .17* | .04 | −.10* | −.17* | -- | |||
| 9. Deviant peers (6th grade) | .17* | .12* | .12* | .14* | .06 | −.11* | −.14* | .54* | -- | ||
| 10. Teasing by students (6th grade) | .32* | .22* | .18* | .17* | .08 | −.10* | .05 | .20* | .10* | -- | |
| 11. Poor academic functioning (6th grade) | .09* | .11* | .05 | .04 | .03 | −.13* | −.20* | .26* | .24* | .12* | -- |
| 12. Family conflict (6th grade) | .35* | .25* | .23* | .14* | .03 | .08 | −.07 | .31* | .33* | .05 | .03 |
| Mean: | 1.84 | 1.91 | 1.96 | 1.95 | .65 | .51 | .36 | 1.19 | 0.6 | 1.65 | 2.03 |
| SD: | 0.77 | 0.8 | 0.86 | 0.84 | .48 | .50 | .48 | 0.37 | 0.91 | 0.68 | 1.07 |
p < .05
LGMM analyses
Identifying the optimal number of trajectory classes
First, a latent growth model (LGM) analysis of depression symptoms was run to examine the need to include both linear and quadratic change parameters in subsequent LGMM analyses. This model yielded significant intercept and slope means and residual variances. The mean of the quadratic slope parameter was non-significant, but significant residual variance in this parameter was observed. Additionally, we compared the fit of a model including only a linear slope term and one including a quadratic slope term, and found that adding a quadratic slope parameter lead to a significant improvement in model fit (Δχ2 (Δdf = 4) = 10.16, p < .05). As such, subsequent LGMM analyses included latent intercept, slope, and quadratic slope parameters.
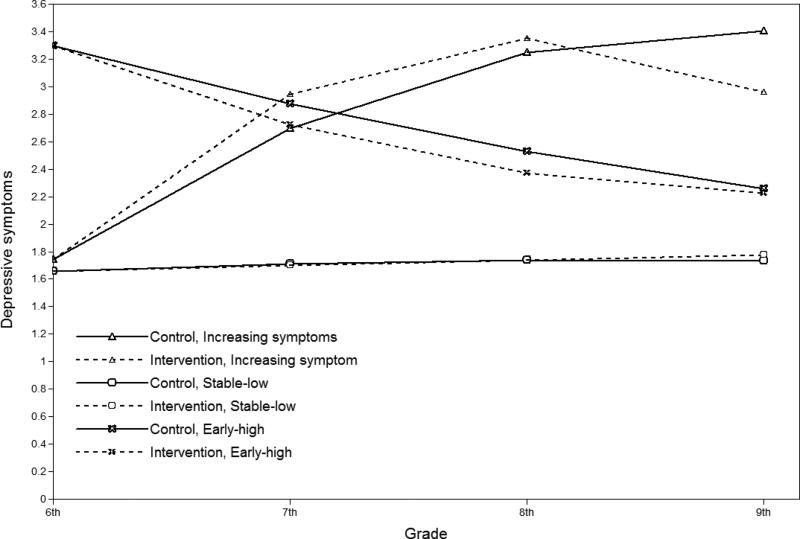
Second, we examined a series of LGMM analyses including increasing numbers of latent classes. Fit indices are shown in Table 2. Results of the LMR-LRT pointed to a 3-class solution. Additionally, models with more than 3 classes exhibited problems with negative residual variances in time-specific depression scores and in growth parameters, and included very small classes (i.e. less than 3% of the sample). Further, the additional classes in these models were not qualitatively distinct compared to the first 3 classes. For instance, the small 4th class in the 4-class model appeared to divide the difference between the “increasing” and “stable-low” classes, yielding a group of youth showing moderately increasing symptoms. As such, subsequent models used a 3-class solution, as shown in Figure 1. The three-class solution included a large group of youth (Stable-Low: 78.7% of the sample) reporting low levels of depressive symptoms across time, a group (Increasing-symptoms : 9.8% of the sample) exhibiting low symptoms in 6th grade that increased significantly across time but showed significant reduction in the rate of change across study waves, and a group exhibiting high symptom levels in 6th grade that were relatively stable over time (Early-high:11.5% of the sample).
Table 2.
Fit indices for determining optimal number of latent classes (unconditional model)
| Number of Classes | # of Free Parameters | Entropy | BIC | Adj BIC | LMR-LRT | B-LRT |
|---|---|---|---|---|---|---|
| 1 | 13 | N/A | 4621.26 | 4579.99 | N/A | N/A |
| 2 | 17 | .88 | 4513.87 | 4459.90 | 127.92, p < .05 | 132.93, p < .05 |
| 3 | 21 | .86 | 4451.48 | 4384.81 | 87.92, p = .05 | 87.92, p < .05 |
| 4* | 25 | .87 | 4436.78 | 4357.41 | 42.67, n.s. | 42.67, p < .05 |
| 5* | 29 | .87 | 4407.32 | 4315.25 | 47.36, n.s. | 49.22, p < .05 |
| 6* | 33 | .86 | 4410.09 | 4305.33 | 34.24, n.s. | 34.24 p < .05 |
Notes: BIC = Bayesian Information Criteria; Adj BIC = Sample size adjusted Bayesian Information Criteria; LMR-LRT = Lo Mendel Rubin Likelihood Ratio Test; B-LRT = Bootstrapped Likelihood Ratio Test. Bolded numbers denote best fitting model according to that criteria.
Models with more than 3 classes exhibited problems with negative residual variances in time-specific depression scores and latent slope scores, as well as small sizes of specific classes, and problems with replications for LMR-LRT and B-LRT tests.
Figure 1.
Intervention effects across trajectory classes.
Intervention effects within classes
The three-class model was extended to include intervention assignment as a within-class covariate. As shown in table 3, intervention was significantly negatively related to the quadratic slope parameter within the “increasing symptoms” class. Within this class, youth in the intervention condition exhibited a significantly stronger symptom deceleration across time, compared to youth in the control condition, leading to significantly lower depressive symptoms at 9th grade. The effect size for intervention on 9th grade symptoms was moderate to large (Cohen's d = .74) within the “increasing symptoms” class. No other significant effects of intervention were observed across other classes.
Table 3.
Intervention effects within classes
| Increasing symptoms class (9.8%) | Early-high class (10.7%) | Stable-low class (79.5%) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Intercept | Slope | Slope2 | Intercept | Slope | Slope2 | Intercept | Slope | Slope2 | |
| Intervention | Fixed at 0 | .48 (.28) | −.64 (.27)* | Fixed at 0 | −.26 (.32) | .28 (.41) | Fixed at 0 | −.04 (.10) | .06 (.11) |
| Male Gender | −.02 (.06) | −.25 (.12)* | .15 (.10) | −.02 (.06) | −.25 (.12)* | .15 (.10) | −.02 (.06) | −.25 (.12)* | .15 (.10) |
| Antisocial behavior | .33 (.13)* | −.26 (.26) | .13 (.28) | .33 (.13)* | −.26 (.26) | .13 (.28) | .33 (.13)* | −.26 (.26) | .13 (.28) |
| Peer Deviance | −.02 (.10) | .02 (.16) | .08 (.16) | −.02 (.10) | .02 (.16) | .08 (.16) | −.02 (.10) | .02 (.16) | .08 (.16) |
| Family Conflict | .49 (.10)* | −.19 (.17) | .04 (.14) | .49 (.10)* | −.19 (.17) | .04 (.14) | .49 (.10)* | −.19 (.17) | .04 (.14) |
| Poor grades | .04 (.06) | .01 (.10) | −.04 (.10) | .04 (.06) | .01 (.10) | −.04 (.10) | .04 (.06) | .01 (.10) | −.04 (.10) |
| Teasing by peers | .34 (.10)* | −.16 (.17) | .10 (.12) | .34 (.10)* | −.16 (.17) | .10 (.12) | .34 (.10)* | −.16 (.17) | .10 (.12) |
| Parameter intercept | .86 (.22)* | 1.70 (.31)* | −.29 (.10)* | 2.42 (.18)* | .09 (.31)* | −.05 (.10) | .78 (.12)* | .62 (.21)* | −.10 (.07) |
| Residual variance | .10 (.07) | .10 (.10) | .01 (.01) | .10 (.07) | .10 (.10) | .01 (.01) | .10 (.07) | .10 (.10) | .01 (.01) |
Covariate effects
The model was extended to include baseline predictors of latent class membership, as well as covariate effects on growth parameters within classes. We first examined whether within-class covariate effects should be allowed to vary across classes. Allowing such variation across classes did not significantly improve model fit (ΔΧ2 (Δdf = 30) = 45.87, n.s.), and so covariate effects were held equal across classes in the final model. Across classes, higher initial levels of depression were predicted by higher antisocial behavior, family conflict, and teasing by peers in 6th grade. Male gender predicted a more negative linear change in depressive symptoms over time. Other than intervention effects on the quadratic slope parameter in the increasing symptoms class, there were no other predictors of the quadratic slope parameter.
The stable-low class served as the reference class for the prediction of class membership. Relative to the stable-low class, membership in the increasing symptoms class was significantly predicted by female gender (estimate = −1.57, SE = .65), greater antisocial behavior at baseline (estimate = .94, SE = .46), and greater teasing by peers at baseline (estimate = .71, SE = .25). Membership in the early-high class (relative to the stable-low class) was significantly predicted by greater family conflict at baseline (estimate = .25, SE = .12), and greater teasing by peers at baseline (estimate = .86, SE = .26). Finally, we compared the early-high and increasing symptoms classes. The early-high class exhibited lower levels of baseline antisocial behavior, compared to the increasing symptoms class (estimate = .87, SE = .45). No differences across classes were observed for ethnicity peer deviance, or baseline academic problems.
We also conducted follow-up analyses to examine differences across classes in terms of the likelihood of random assignment to intervention, the proportion of families receiving the FCU assessment, and the number of minutes spent in further intervention services. These follow-up analyses were conducted using exported estimates of class membership from the final mixture model, rather than being incorporated into the latent variable model directly, because such data is only present for families assigned to intervention. There were no significant differences across classes for the proportion of families assigned to intervention versus control conditions (Stable high: 69.1% intervention; Increasing: 66.7% intervention; Stable low: 64.5% intervention; Χ2 (df = 2) = .62, n.s.). Among families assigned to the intervention condition, no differences were found across classes for the percentage of families who received the FCU (Stable high: 35.0% FCU; Increasing: 35.3% FCU; Stable low: 43.1% FCU; Χ2 (df = 2) = 1.57, n.s.). Similarly, no differences were found across classes for the number of minutes in post-FCU intervention services (Stable high: mean = 179.92, SD = 106.24; Increasing: mean = 167.83, SD = 261.31; Stable low: mean = 116.93, SD = 164.01; F (2, 157) = 1.21, n.s. Three outlier cases with scores 3 to 8 SD above the mean were removed). These results highlight that differences in the effect of intervention for the increasing symptoms class relative to the remaining classes was not due to differences in the receipt of intervention components. Finally, we examined changes in the covariates included in the model as possible mediators of intervention effects in the increasing symptoms class. None of the changes were found to mediate the intervention effects, although statistical power is limited for such sub-group analyses (details are available upon request).
Discussion
The aims of this study were twofold. First, we examined heterogeneity in trajectories of depressive symptoms over early adolescence, with special attention to onset timing and course. Second, we examined the patterns of response to the Family Check Up across the diverse trajectories of depressive symptoms from 6th to 9th grade. In line with prior studies of depressive symptom trajectories (e.g. Brendgen et al., 2005), we identified three groups, including a large group of youth that consistently showed low levels of symptoms across early adolescence. Of interest, however, were two smaller groups of youth, one showing stable high symptom levels. Given that youth in the high stable group reported relatively high symptoms at age 10-11 (sixth grade) and remained high in symptoms, it seems reasonable to think of them as an early-onset group. The final group, however, had very few symptoms initially, but grew in depression through grade 9 (approximately age 14 years). This group could be thought of as adolescent onset, and youth in this group were mostly female, with elevated antisocial behavior and teasing by peers in 6th grade. Significant intervention effects on depressive symptoms were only observed in this “increasing symptoms” class, with a moderate to large effect at 9th grade. Finding that intervention effects do not emerge until grade 9 likely reflects that the intervention was delivered across grades 7 and 8, the full effect of which would not be observed until grade 9.
The significant effect of intervention for youth in the increasing symptoms class is consistent with the timing hypothesis, suggesting that the timing of intervention relative to the onset of symptoms may be particularly important factor in predicting who responds to prevention programs. Developmental studies have generally found that rates of depression begin to escalate in early adolescence (Hyde et al., 2008), and preventive interventions delivered close in time to this symptom increase may be particularly powerful for youth who might otherwise begin to show increasing symptoms within this timeframe. Further, the predominance of female youth in this class, relative to the stable low class, is also consistent with the timing hypothesis, as the adolescent increase in depression is particularly strong for girls (e.g. Hyde, Mezulis, & Abramson, 2008). The increasing symptoms class was also discriminated from the other classes by elevated antisocial behavior. Given that the FCU was originally designed for adolescent conduct problems and substance use, it may be particularly powerful for disrupting depression development among youth with co-occurring antisocial behavior. Similar results were observed in a trial of the FCU in early childhood, with youth with co-occurring internalizing and externalizing symptoms appearing particularly responsive to family intervention (Connell et al., 2008), suggesting that family-focused prevention may be particularly powerful for this group.
Because the FCU is tailored to family needs, we explored aspects of treatment engagement in relation to class membership. We did not find significant differences across classes in terms of assignment to intervention or control groups, the likelihood of receiving the FCU for youth in the intervention condition, or the number of hours of intervention services. As such, treatment response and non-response classes were not simply discriminated by the receipt of services. Rather, response to the intervention appears to be primarily a function of the timing of services with respect to symptom onset, and the match between services and baseline risk.
The most interesting finding related to treatment non-response is the lack of response of the early onset persistently depressed youth. There are several possible explanations for this lack of response. First, youth and families were not targeted for depression in this study, and therefore aspects of the family environment, peer environment, or the youth herself may have been missed with respect to intervention focus within this group. Prevention services for the early-high group may need to be broadly focused (targeting family and peer relationships) to be maximally effective. Second, youth in this class already reported elevated symptoms in 6th grade. It is possible that these youth would be more responsive to services delivered earlier in childhood. Developmental research indicates that the recency of risk exposure (compared to the specific types of risks) may be crucial for distinguishing earlier vs. later depression onset (Shanahan et al, 2011), suggesting that the timing of intervention services relative to depression onset may be a crucial determinant of intervention effectiveness. Of note, we have found that an early-childhood version of the FCU lead to significant reductions in internalizing and externalizing problems across childhood, with improvements mediated by changes in parenting quality and reductions in maternal depressive symptoms (Shaw et al., 2008). As youth in that study are followed into adolescence, it will be important to examine whether the FCU is associated with diminished symptoms for youth with earlier-onset internalizing problems.
While youth in the increasing symptoms class appeared responsive to the FCU, youth exhibiting stable-low levels of depression did not. Youth in the stable-low class generally had low depression levels and the lowest levels of risk on a number of indices. Thus, these youth reflect a class of “non-responders” with little room for symptom reduction, and little need for intervention, at least with respect to depression. One advantage of an adaptive prevention design is that these youth can be identified, and resources reserved for youth in greater need of services.
Limitations and future directions
As with any study, there are a number of limitations that point to the need for future research. First, the variables used in these analyses were measured via adolescent self-report. While the use of adolescent-report measures has advantages (for example, parents may be less aware of adolescent depression than are teens), multiple informant data, and objective measures including diagnostic interview data, should be used in future studies to limit the potential influence of mono-rater bias. Additionally, the depression inventory was developed for this prevention trial, based upon diagnostic criteria for depression. However, the measure was found to be reliable, and correlations with other variables support its validity, as they are in the predicted direction, and similar in magnitude to other studies in this age range that have used established depression measures (e.g. Connell & Dishion, 2008). Further, LGMM analytic methods are an evolving area of statistics, and have been the subject of several cautionary papers (e.g. Sher, Jackson, & Steinley, 2011). It will be important for future research to replicate the current results in independent samples. Additionally, it will be important for future research to examine why variability in treatment response might be present, including the identification of mediators that may differ across groups. Unfortunately, mediation is challenging in the context of LGMM analyses, and preliminary mediation analyses in the increasing symptoms class did not reveal significant mediation, perhaps due to limited statistical power. However, other studies with the FCU have found that reductions in family conflict and parental depression, and improvements in positive parenting, may mediate prevention effects on youth behavior problems (Shaw, Connell, Dishion, Wilson, & Gardner, 2009; Fosco, Van Ryzin, Stormshak, & Dishion, 2014; Van Ryzin & Dishion, 2012). It is possible that such processes may be relevant for depression effects, as well. Despite the need for further research, the current results highlight the importance of examining variability in treatment response in the context of prevention programs, and identify several possible ways of continuing to refine the FCU intervention model.
Finally, we now have three randomized trials that suggest improvements in depression as a function of the FCU intervention (Connell & Dishion, 2008; Connell, Bullock et al, 2008; Shaw et al, 2009). In each of these studies, finding mediators that are specific to the effects of the FCU on depression has been elusive. It seems advisable at this juncture to design an FCU randomized trial that specifically targets adolescent depression, with a focus on measuring and testing a mediation model, incorporating an array of social, cognitive, and neurobiological processes with demonstrated links to depression. The current findings do suggest that the intervention model for the treatment and prevention of adolescent depression will by nature be developmentally specific, as the data are clear that the heterogeneity in symptom expression likely reflects diverse biological and environmental risks and vulnerabilities. An advantage of the FCU intervention framework is that it can be adapted to be responsive to heterogeneity.
Footnotes
The authors declare that they have no conflict of interest.
Contributor Information
Arin M. Connell, Case Western Reserve University
Elizabeth Stormshak, University of Oregon.
Thomas Dishion, Arizona State University.
Gregory Fosco, The Pennsylvania State University.
Mark Van Ryzin, University of Oregon.
References
- Asarnow J, Goldstein M, Tompson M, Guthrie D. One-year outcomes of depressive disorders in child psychiatric in-patients. Journal of Child Psychology and Psychiatry. 1993;34:129–137. doi: 10.1111/j.1469-7610.1993.tb00975.x. [DOI] [PubMed] [Google Scholar]
- Beardslee W, Brent D, Weersing V, Clarke G, Porta G, Hollon S, Garber J. Prevention of depression in at-risk adolescents. JAMA psychiatry. 2013;70:1161–1170. doi: 10.1001/jamapsychiatry.2013.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birmaher B, Brent D, Kolko D, Baugher M, Bridge J, Holder D, Ulloa R. Clinical outcome after short-term psychotherapy for adolescents with major depressive disorder. Archives of General Psychiatry. 2000;57:29–36. doi: 10.1001/archpsyc.57.1.29. [DOI] [PubMed] [Google Scholar]
- Brendgen M, Wanner B, Morin A, Vitaro F. Relations with parents and with peers, temperament, and trajectories of depressed mood during early adolescence. Journal of Abnormal Child Psychology. 2005;33:579–594. doi: 10.1007/s10802-005-6739-2. [DOI] [PubMed] [Google Scholar]
- Brent D, Kolko D, Birmaher B, Baugher M, Bridge J, Roth C, Holder D. Predictors of treatment efficacy in a clinical trial of three psychosocial treatments for adolescent depression. Journal of the American Academy of Child Psychology. 1998;37:906–914. doi: 10.1097/00004583-199809000-00010. [DOI] [PubMed] [Google Scholar]
- Collins L, Murphy S, Bierman K. A Conceptual Framework for Adaptive Preventive Interventions. Prevention Science. 2004;5:185–196. doi: 10.1023/b:prev.0000037641.26017.00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connell A, Bullock B, Dishion T, Shaw D, Wilson M, Gardner F. Family intervention effects on co-occurring early childhood behavioral and emotional problems: A latent transition analysis approach. Journal of Abnormal Child Psychology. 2008;36:1211–1225. doi: 10.1007/s10802-008-9244-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connell A, Dishion T. Reducing depression among at-risk early adolescents. Journal of Family Psychology. 2008;22:574–585. doi: 10.1037/0893-3200.22.3.574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compas B, Forehand R, Keller G, Champion J, Rakow A, Reeslund K, Cole D. Randomized controlled trial of a family cognitive-behavioral preventive intervention for children of depressed parents. Journal of Consulting & Clinical Psychology. 2009;77:1007–1020. doi: 10.1037/a0016930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dishion T, Patterson G. The development and ecology of antisocial behavior in children and adolescents. In: Cicchetti D, Cohen DJ, editors. Developmental Psychopathology. Vol. 3. Wiley; New York: 2006. pp. 503–541. [Google Scholar]
- Dishion T, Stormshak E. Intervening in children's lives: An ecological, family-centered approach to mental health care. American Psychological Association; Washington, DC: 2007. [Google Scholar]
- Fosco G, Van Ryzin M, Stormshak E, Dishion T. Putting theory to the test: Examining family context, caregiver motivation, and conflict in the Family Check-Up model. Development and psychopathology. 2014;26:305–318. doi: 10.1017/S0954579413001004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garber J, Clarke G, Weersing V, Beardslee W, Brent D, Gladstone T, Iyengar S. Prevention of depression in at-risk adolescents: a randomized controlled trial. JAMA. 2009;301:2215–2224. doi: 10.1001/jama.2009.788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horowitz J, Garber J. The prevention of depressive symptoms in children and adolescents: A meta-analytic review. Journal of Consulting & Clinical Psychology. 2006;74:401–415. doi: 10.1037/0022-006X.74.3.401. [DOI] [PubMed] [Google Scholar]
- Hyde J, Mezulis A, Abramson L. The ABCs of depression: integrating affective, biological, and cognitive models to explain the emergence of the gender difference in depression. Psychological Review. 2008;115:291–313. doi: 10.1037/0033-295X.115.2.291. [DOI] [PubMed] [Google Scholar]
- Kaminski J, Valle L, Filene J, Boyle C. A Meta-analytic Review of Components Associated with Parent Training Program Effectiveness. Journal of Abnormal Child Psychology. 2008;36:567–589. doi: 10.1007/s10802-007-9201-9. [DOI] [PubMed] [Google Scholar]
- Little R. A test of missing completely at random for multivariate data with missing values. Journal of the American Statistical Association. 1988;83:1198–1202. [Google Scholar]
- Lo Y, Mendell N, Rubin D. Testing the number of components in a normal mixture. Biometrika. 2001;88:767–778. [Google Scholar]
- Mason W, Kosterman R, Hawkins J, Haggerty K, Spoth R, Redmond C. Influence of a family-focused substance use preventive intervention on growth in adolescent depressive symptoms. Journal of Research on Adolescence. 2007;17:541–564. [Google Scholar]
- McLachlan G, Peel D. Finite mixture models. John Wiley & Sons; New York: 2004. [Google Scholar]
- Metzler C, Biglan A, Rusby J, Sprague J. Evaluation of a comprehensive behavior management program to improve school-wide positive behavior support. Education & Treatment of Children. 2001;24:448–479. [Google Scholar]
- Miller W, Rollnick S. Motivational interviewing: Preparing people for change. Guilford press; New York: 2002. [Google Scholar]
- Mufson L, Dorta K, Wickramaratne P, Nomura Y, Olfson M, Weissman M. A randomized effectiveness trial of interpersonal psychotherapy for depressed adolescents. Archives of General Psychiatry. 2004;61:577–584. doi: 10.1001/archpsyc.61.6.577. [DOI] [PubMed] [Google Scholar]
- Muthén B, Brown C, Masyn K, Jo B, Khoo S, Yang C, Liao J. General growth mixture modeling for randomized preventive interventions. Biostatistics. 2002;3:459–475. doi: 10.1093/biostatistics/3.4.459. [DOI] [PubMed] [Google Scholar]
- Muthén L, Muthén B. Mplus User's Guide, V. 7. Muthen & Muthen; Los Angeles: 2013. [Google Scholar]
- Patterson G, Stoolmiller M. Replications of a dual failure model for boys’ depressed mood. Journal of Consulting and Clinical Psychology. 1991;59:491–498. doi: 10.1037//0022-006x.59.4.491. [DOI] [PubMed] [Google Scholar]
- Rohde P, Lewinsohn P, Seeley J. Response of depressed adolescents to cognitive-behavioral treatment: do differences in initial severity clarify the comparison of treatments? Journal of Consulting & Clinical Psychology. 1994;62:851–854. doi: 10.1037//0022-006x.62.4.851. [DOI] [PubMed] [Google Scholar]
- Sandler I, Wolchik S, Cruden G, Mahrer N, Ahn S, Brincks A, Brown C. Overview of Meta-Analyses of the Prevention of Mental Health, Substance Use, and Conduct Problems. Annual review of clinical psychology. 2014;10:243–273. doi: 10.1146/annurev-clinpsy-050212-185524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shanahan L, Copeland WE, Costello EJ, Angold A. Child-, adolescent-and young adult-onset depressions: differential risk factors in development? Psychological medicine. 2011;41:2265–2274. doi: 10.1017/S0033291711000675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw DS, Connell A, Dishion TJ, Wilson MN, Gardner F. Improvements in maternal depression as a mediator of intervention effects on early childhood problem behavior. Development and psychopathology. 2009;21:417–439. doi: 10.1017/S0954579409000236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheeber L, Hops H, Davis B. Family processes in adolescent depression. Clinical child and family psychology review. 2001;4:19–35. doi: 10.1023/a:1009524626436. [DOI] [PubMed] [Google Scholar]
- Sher K, Jackson K, Steinley D. Alcohol use trajectories and the ubiquitous cat's cradle: cause for concern? Journal of Abnormal Psychology. 2011;120:322. doi: 10.1037/a0021813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shirk S, Karver M. Prediction of treatment outcome from relationship variables in child and adolescent therapy: a meta-analytic review. Journal of Consulting & Clinical Psychology. 2003;71:452–464. doi: 10.1037/0022-006x.71.3.452. [DOI] [PubMed] [Google Scholar]
- Shochet I, Dadds M, Holland D, Whitefield K, Harnett P, Osgarby S. The Efficacy of a Universal School-Based Program to Prevent Adolescent Depression. Journal of clinical child psychology. 2001;30:303–315. doi: 10.1207/S15374424JCCP3003_3. [DOI] [PubMed] [Google Scholar]
- Stark K, Banneyer K, Wang L, Arora P. Child and adolescent depression in the family. Couple and Family Psychology: Research and Practice. 2012;1:161–184. [Google Scholar]
- Stein D, Brent DA, Bridge J, Kolko D, Birmaher B, Baugher M. Predictors of parent-rated credibility in a clinical psychotherapy trial for adolescent depression. The Journal of psychotherapy practice and research. 2001;10:1–7. [PMC free article] [PubMed] [Google Scholar]
- Stormshak E, Connell A, Dishion T. An adaptive approach to family-centered intervention in schools. Prevention Science. 2009;10:221–235. doi: 10.1007/s11121-009-0131-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stormshak E, Connell A, Véronneau MH, Myers M, Dishion T, Kavanagh K, Caruthers A. An ecological approach to promoting early adolescent mental health and social adaptation. Child Development. 2011;82:209–225. doi: 10.1111/j.1467-8624.2010.01551.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stormshak E, Fosco G, Dishion T. Implementing interventions with families in schools to increase youth school engagement. School Mental Health. 2010;2:82–92. doi: 10.1007/s12310-009-9025-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trudeau L, Spoth R, Randall G, Azevedo K. Longitudinal Effects of a Universal Family-Focused Intervention on Growth Patterns of Adolescent Internalizing Symptoms and Polysubstance Use: Gender Comparisons. Journal of Youth and Adolescence. 2007;36:725–740. [Google Scholar]
- Van Ryzin M, Dishion T. The impact of a family-centered intervention on the ecology of adolescent antisocial behavior: Modeling developmental sequelae and trajectories during adolescence. Development and Psychopathology. 2012;24:1139–1155. doi: 10.1017/S0954579412000582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang M, Dishion T, Stormshak E, Willett J. Trajectories of family management practices and early adolescent behavioral outcomes. Developmental Psychology. 2011;47:1324–1341. doi: 10.1037/a0024026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wickrama T, Wickrama K. Heterogeneity in adolescent depressive symptom trajectories. Journal of Adolescent Health. 2010;47:407–413. doi: 10.1016/j.jadohealth.2010.02.013. [DOI] [PubMed] [Google Scholar]
- Yaroslavsky I, Pettit JW, Lewinsohn P, Seeley J, Roberts R. Heterogeneous trajectories of depressive symptoms. Journal of Affective Disorders. 2013;148:391–399. doi: 10.1016/j.jad.2012.06.028. [DOI] [PMC free article] [PubMed] [Google Scholar]