Abstract
Approximately thirty percent of patients with gastric cancer undergo an avoidable lymph node dissection with a higher rate of postoperative complication. Comparing the D1 and D2 dissections, it was found that there is a significant difference in morbidity, favoured D1 dissection without any difference in overall survival. Subgroup analysis of patients with T3 tumor shows a survival difference favoring D2 lymphadenectomy, and there is a better gastric cancer-related death and non-statistically significant improvement of survival for node-positive disease in patients with D2 dissection. However, the extended lymphadenectomy could improve stage-specific survival owing to the stage migration phenomenon. The deployment of centralization and application of national guidelines could improve the surgical outcomes. The Japanese and European guidelines enclose the D2 lymphadenectomy as the gold standard in R0 resection. In the individualized, stage-adapted gastric cancer surgery the Maruyama computer program (MCP) can estimate lymph node involvement preoperatively with high accuracy and in addition the Maruyama Index less than 5 has a better impact on survival, than D-level guided surgery. For these reasons, the preoperative application of MCP is recommended routinely, with an aim to perform “low Maruyama Index surgery”. The sentinel lymph node biopsy (SNB) may decrease the number of redundant lymphadenectomy intraoperatively with a high detection rate (93.7%) and an accuracy of 92%. More accurate stage-adapted surgery could be performed using the MCP and SNB in parallel fashion in gastric cancer.
Keywords: Gastric cancer, Surgery, Lymphadenectomy, Sentinel node biopsy, Maruyama computer program
Core tip: Comparing the D1 and D2 dissections, it was found that there is a significant difference in postoperative morbidity and mortality, favoured D1 dissection without any difference in overall survival. The implementation of centralization and application of national guidelines could improve the surgical outcomes. More accurate stage-adapted surgery could be performed using the Maruyama computer program and sentinel lymph node biopsy in parallel fashion in gastric cancer.
INTRODUCTION
In most cases, modern, optimal treatment of patients with different neoplasms can be achieved with a stage adapted, combined modality therapy according to international protocols. In case of solid tumors, the lymph node (LN) involvement and its exact number is the most important prognostic factor. Adjuvant chemotherapy, as well as the oncological outcome is terminated by the tumor-node-metastasis stage. Preoperative imaging techniques provide a much more accurate determination of the T and M stage than that of the N stage. The correct status of LN metastases can be obtained only by histology following an optimally extended node dissection. The removal of further LNs on the other hand, increases operative time, the rate of complications, and if negative may be considered unnecessary.
Almost three hundred thousand patients with gastric adenocarcinoma do not have LN metastasis in the one million new cases each year[1,2]. The depth of tumor invasion[3,4], the metastatic LN status and R0 resection are the most important independent prognostic factors for overall and disease free survival (OS, DFS)[5-7]. Moreover, a lot of study proved that LN metastasis is an independent risk factor for local recurrence as well as the time interval between radical gastrectomy and hepatic metastasis in patients after R0 resection[8-10].
The aim of this review is to report the latest issues from 2014 according to lymphadenectomy in gastric cancer and compare these results with earlier studies.
LN INVOLVEMENT
Successful estimation of LN involvement may help to define which patients would or would not benefit from an extended LN dissection in association with gastrectomy[11]. However, preoperative diagnostic tools have a low sensitivity and specificity for defining these patient subpopulations. Sensitivity, specificity and accuracy of spiral computer tomography for detection of pathologic LN involvement are 73.1%, 50.0% and 84.2%, respectively[11,12]. Endoscopic ultrasonography has an accuracy of 68.6%, with a sensitivity and specificity of 66.7% and 73.7%, respectively[11,13]. The real problem of these imaging procedures is that exclusion of endoscopic ultrasonography, only the size of the LNs is taken into account.
In association with T stage, LN involvement can be found in 15% of patients with carcinoma confined to the mucosa, whereas LN metastases were detected in 23.4%, 48.2%, and 69.8% of patients with carcinoma invading the submucosa, muscularis propria and serous layer, respectively[14] Gertler et al[15] showed that not only infiltration of the submucosa but also lymphatic vessel invasion, multifocal tumor growth, younger patient age and poor tumor differentiation were associated with nodal disease. Besides T stage, LN involvement can also be influenced by tumor size. The overall accuracy of tumor size for preoperative N staging was 82.13%[16]. The incidence of LN metastasis in patients with a cancer size of 3-5 cm is 64.9%, 80% in patients with a cancer size of 5-7 cm and 84.3% in patients with a cancer size of > 7 cm[14]. Additionally, early gastric cancer (EGC) has nodal metastases in 38.9% in poorly differentiated or undifferentiated types of tumor, in 41.7% with Lauren diffuse type and in 33.3% with a size larger than 3 cm[17]. Yang et al[18] found that venous invasion, submucosal invasion or antral tumor location were independent predictors for LN metastasis in multivariate analysis. The rates of LN metastasis were 1.1% for patients with one or no predictor and 17.8% for those with two or more predictors[18].
While the prognostic significance of macrometastasis in the LNs is obvious, the role of lymphovascular invasion (LVI) or micrometastasis (MM) is controversial. Lee et al[19] confirmed that the recurrence-free survival is lower in N0/LVI(+) patients than in N0/LVI(-) patients, however they did not find any effect of LVI+ on overall survival. The incidence of LN MM is lower than 10% in patients with node negative EGC[20] but it is higher in histologically diffuse type tumors[21]. The presence of MM influenced DFS, although the OS analysis revealed no significant difference between MM-positive and MM-negative patients[19]. The reverse transcriptase polymerase chain reaction proved to be the most sensitive method in the detection of MM[22].
Meanwhile, a multivariate survival analysis concluded that the number of examined LN (eLN) was an independent predictor of overall survival of patients with node-negative gastric cancer. According to the cut-point analysis, T2-T4 patients with 11-15 eLN had a significantly longer mean OS than those with 4-10 eLN or 1-3 eLN. Patients with ≤ 15 eLN were more likely to experience locoregional and peritoneal recurrence than those with > 15 eLN[23]. However, this trend was not observed when the number of examined LN exceeded 30[24].
These results are potentially associated with the elimination of MM in negative LNs[25]. Based on these findings, LVI and MM should be considered in postoperative management of gastric cancer[19].
LYMPHADENECTOMY
D1 vs D2 lymphadenectomy
The adequate extension of lymphadenectomy differs significantly between East Asian and Western countries. Extended lymphadenectomy (D2) is the standard of care in Japan and South Korea, while for example, the majority of United States patients receive at most a limited lymphadenectomy (D1)[26,27]. This controversy may originate from different factors. First, the incidence of gastric cancer is significantly higher in Asia than in European Union, or in the United States[27,28].
Second, centralization of treatment has not yet been solved in the latter regions; 80% of Medicare patients with gastric cancer in the United States go through surgery in centers performing less than 20 procedures per year[29] and there is a significant number of low-volume surgeons performing less than two cases annually[30,31].
Table 1 shows the primary and revised results of prospective randomized trials (RCT) comparing D1 to D2 lymphadenectomy in association with postoperative morbidity, mortality, frequency of splenectomy and pancreatectomy and long term oncological outcomes such as relapse risk and overall survival (OS). The three earliest studies found a higher morbidity and mortality rate following extended LN dissection of patients with gastric cancer when compared to those undergoing D1 dissection only[11,32-34]. These higher rates were related mostly to splenectomy and pancreatectomy. Although Dent et al[32] did not perform resection of these organs, this study should be evaluated with reservations because of the small series size. Furthermore, limited surgical experience could explain these results. The quality control of lymphadenectomy was inadequate, as the non-compliance rate (absence of LNs from more than two LN stations that were supposed to be harvested) was 51% in the D2 group in the Dutch trial[34,35] and, in the extended group of the British trial, the dissection of LN station no.7 was 63.5%, and was less than 50% in station no.8 and no.9[36].
Table 1.
The primary and revised results of prospective randomized trials comparing D1 to D2 dissection
| Ref. |
Morbidity (%) |
Mortality (%) |
Splenectomy (%) |
Pancreatectomy (%) |
RR (%) |
OS (%) |
||||||
| D1 | D2 | D1 | D2 | D1 | D2 | D1 | D2 | D1 | D2 | D1 | D2 | |
| Dent[32] | 13.6a | 38a | 0 | 0 | 0 | 0 | 0 | 0 | 81 | 76 | ||
| British[33,36] | 28a | 46a | 6.5a | 13a | 27 | 9 | 41 | 571 | NS | NS | 35 | 33 |
| Dutch[34,37] | 24a | 43a | 4a | 10a | 11 | 37 | 3 | 30 | 43 | 47 | 45 | 47 |
| Dutch - 15 yr[38] | 22a | 12a | 21 | 29 | ||||||||
| Taiwanese[39,44] | 7.3a | 17.1a | 0 | 0 | 3 | 1 | 11 | 131 | 50.6 | 40.3 | 53.6a | 59.5a |
| Italian[35,43] | 12 | 17.9 | 3 | 2.2 | 6.8 | 9.0 | 1.5 | 1.5 | 66.5 | 64.2 | ||
P < 0.05.
Pancreato-splenectomy. RR: Relapse risk; OS: Overall survival; NS: Non-significant.
Moreover, extended LN dissection did not have any effect on oncological outcomes. The relapse risk and survival were similar in these studies. Only the revision of the Dutch trial showed better survival in advanced disease in the D2 group, after 11-year follow-up[37]. The 15-year follow-up results revealed that cancer-related death rates were lower (37% vs 48%) with a lower rate of local recurrence in the D2 lymphadenectomy group (Table 1)[38]. Subgroup analysis of this trial demonstrated significantly higher survival for females (35% vs 21%) and in stage II disease (33% vs 15%) in the D2 arm. The 15-year survival in patients without pancreatico-splenectomy was significantly higher with D2 than D1 dissection (35% vs 22%)[38].
The two latest randomized trials from the 21st century did not present significant differences in postoperative mortality between the D1 and D2 group[35,39]. The morbidity rate was higher with D2 lymphadenectomy in the Taiwanese trial (which compared D1 to D3 dissection; however their D3 lymphadenectomy is similar to the current definition of D2 dissection). The Italian study did not show this difference and proved that D2 dissection could be performed safely without splenectomy and distal pancreatectomy, with comparable mortality and morbidity to those with D1 dissection in specialized centers[39,40]. These rates are comparable to the Japan Clinical Oncology Group (JCOG) 9501 trial and the nationwide Japanese registry where the mortality was less than 2% after D2 dissection[41,42]. Neither did the latter study find any survival benefit from the extended lymphadenectomy[43]. Subgroup analyses showed a 5-year disease-specific survival benefit for patients with pathological tumor 1 (pT1) disease in the D1 group (9% vs 83% for the D2 group; P = 0.015), and for patients with pT2-4 status and positive LNs in the D2 group (59% vs 38% for the D1 group; P = 0.055). However, the non-compliance rate was 33.6%[43]. It was concluded that the contamination (over-extensive nodal dissection) (18%) and the higher rate of stage IA disease in the D1 group and of stage IV in the D2 arm, apparently nullified the effect of correct extended dissection[41,43]. The other randomized trial from Taiwan proved a better (P = 0.041) survival with D2 dissection[44].
The results of these recent studies call attention to the importance of the learning curve and the necessity of standardized procedures with routine preservation of the spleen and pancreas in experienced centers[40].
Besides the RCT, the latest meta-analysis found significant differences in morbidity, anastomotic leakage, pancreatic leakage, reoperation rates, wound infection, pulmonary complications and postoperative mortality, all of which favoured D1 dissection. The conclusion was that there is no difference in OS when comparing the D1 and D2 arm. Subgroup analysis of patients with T3 tumor shows a survival difference favoring D2 lymphadenectomy (25.9% vs 11.5%), and there is a trend towards a lower risk of gastric cancer-related death among patients having a D2 dissection with preservation of the spleen or pancreas and non-statistically significant improvement of survival for node-positive patients[40,45]. Unfortunately, the main problem of meta-analysis was that it was not possible to match patient groups for treatment with age, sex, type of gastrectomy, pathological stage, tumor location, co-morbidity, treatment strategies, surgeon experience, hospital case volume and extent of LN dissection, all of which affect postoperative complications and overall survival rates[40].
Keeping this in mind, the comparison of oncological outcomes of D1 and D2 dissections in association with different T and N stages could be problematic due to the concept of stage migration. The reason for this is that a limited lymphadenectomy can not represent the adequate staging of LN involvement. Conversely, extended lymphadenectomy could improve stage-specific survival due to the stage migration phenomenon. Furthermore, Xu et al[46]demonstrated that it is necessary to examine at least 16 LNs for accurate pathological examination of gastric cancer, even in node-negative gastric cancer patients[25], and Datta et al[47], who analyzed the data of more than 22000 patients found that the examination of 15 or more LN is a reproducible prognostic factor for gastric cancer outcomes in the United States and should continue to serve as a benchmark for the quality of care.
In addition to the quality of surgery, the pathologist plays a large role in the proper identification and examination of the extracted LN[48].
EXTENSION OF LYMPHADENECTOMY BEYOND SUGGESTED LIMITS
The latest issue of the Japanese Gastric Cancer Association treatment guideline contains the standard lymphadenectomies regarding the type of gastric resection: Total gastrectomy with D2: D1 (Nos.: 1-7) + Nos. 8a, 9, 10, 11p, 11d, 12a; distal gastrectomy with D2: D1 (Nos. 1, 3, 4sb, 4d, 5, 6, 7) + Nos. 8a, 9, 11p, 12a; pylorus-preserving gastrectomy with D1+: D1 (Nos. 1, 3, 4sb, 4d, 6, 7) + Nos. 8a, 9; and in proximal gastrectomy with D1+: D1(Nos. 1, 2, 3a, 4sa, 4sb, 7) + Nos. 8a, 9, 11p[49].
In the field of tumor-location specific LN involvement recent studies can be divided into 2 cohorts depend on the position of the gastric tumor (proximal vs middle and distal).
Proximal gastric cancer
The frequency of metastasis in station no.4d, 5 and 6 LNs in patients with proximal gastric cancer is more than 10%[14,50]. The incidence of station no.10 LN metastasis is 11.82% in upper third advanced gastric cancer (AGC). The estimated OS were 46% and 37% regarding station no.10 dissection or not, which was not statistically significant. Authors suggest high-quality studies with larger sample sizes to determine the clinical significance of no.10 LN removal[51]. Following an 18 mo follow-up of 108 patients Li et al[52] concluded that routine no.10 lymphadenectomy may be unnecessary for advanced, upper third gastric cancer without serosal invasion, unless T3 tumors are located in the greater curvature.
Middle and distal gastric cancer
LN metastasis in station no.2 LNs from distal gastric cancer is only 1.0%, while the metastasis in station no.4 LNs is more than 20%. Since station no.11p is immediately adjacent to stations no.7 and no.9, in the case of distal gastric cancer, station no.11d should be preserved; however, both no.11p and no.11d stations should be removed in cases of proximal gastric cancer[14]. According to Japanese gastric cancer treatment, as station no.14v is closely adjacent to station no.6, station no.14v LNs should also be removed if suspicion of metastasis to the LNs in station no.6 arises[14,49].
As the LN metastasis rate in station no.7 was similar to that of perigastric LNs in 570 patients with advanced distal gastric tumor it is reasonable to include LNs in the no.7 station in the D1 LN dissection[53]. Evaluating LN involvement after total gastrectomy, Galizia found that the incidence of nodal involvement of stations no.10, no.11d, and no.12a was 5%, and the 5-year DFS rate was zero; they concluded that modified D2 lymphadenectomy confers the same oncologic adequacy as standard D2 lymphadenectomy, with a significant reduction of postoperative morbidity[54].
During investigation of LN involvement of the hepatoduodenal ligament (HDLN) a logistic regression analysis showed that no.5 and no.12a LN metastases were associated with a 6.9 and 11.3 fold increase respectively, for risk of no.12p and no.12b LN metastases. In addition, significant differences in 5-year OS of patients with and without no.12p and no.12b LN metastases were observed[55]. However, the clinical significance of removing these LN was not evaluated. Analyzing the data of 1872 patients, LN involvement in station no.12 was 3.6% whereas HDLN metastasis was not a significant factor for survival in multivariate analysis and the 5-year survival rate of 41 patients with HDLN metastasis without distant metastasis at any other site was significantly higher than that among 120 patients with stage IV disease without HDLN metastasis. It is suggested that the inclusion of HDLN in the distant metastatic LN group in gastric cancer is inappropriate and that the seventh American Joint Committee on Cancer criteria for node grouping should be revised[56].
The incidence of no. 14v LN metastasis was 5.0% in 1661 patients who underwent curative resection for middle or lower third gastric cancer. In clinical stages I and II, no.14v LN dissection did not affect overall survival; in contrast, no.14v LN dissection was an independent prognostic factor in patients with clinical stage III/IV gastric cancer[57].
Involvement of no.13 nodes is defined as M1 in the current version of the Japanese classification. However, excision of this LN may be an option in a potentially curative gastrectomy for tumors invading the duodenum[49].
Para-aortic nodal dissection
The Japanese authors do not perform randomized trials comparing D1 and D2 dissection, because they have excellent operative and oncological outcomes with extended lymphadenectomy. The majority of trials with “super-extended” lymphadenectomy are being performed in Asia. The incidence of para-aortic lymph nodes (PALN) metastases was 8.5% in the JCOG 9501 multi-institutional randomized trial, which proved that D2 lymphadenectomy plus para-aortic nodal dissection (PAND) did not increase the OS (70.3% vs 69.2%) or 5-year recurrence-free survival (61.7% vs 62.6%) in curable gastric cancer vs D2 lymphadenectomy[58]. Robertson strengthened this finding in a prospective randomized trial from Hong Kong[59]. Junfeng et al[60] found 6 risk factors to predict the involvement of PALN: Tumor in the upper third, tumor size over 5 cm, tumor penetrating deeper than T2, tumor in stage N2 and N3, tumor regarded as the poorly differentiated type and the Borrman 3, 4 type by macroscopic classification. Additionally, the metastasis of lower lymph nodal stations may be predictors of the positive PALN especially no.1, no.3, no.7 and no.9 stations which evidently had higher odd ratios than the others[60]. de Manzoni et al[61] did not find a significant difference in the cumulative incidence of recurrence between D2 and D3 lymphadenectomy in the analysis of 568 patients. The risk of recurrence was higher after D3 than after D2 (45.1% vs 35.3%, P = 0.078) in the intestinal histotype while the pattern was reversed in the mixed/diffuse histotype (48.3% vs 61.5%, P = 0.084)[61].
In overall 5-year survival Zhang et al[62] could not demonstrate a significant difference between patients underwent D2 plus PAND surgery and those underwent D2 surgery. He suggests that this “over-extended” dissection should only be recommended for T3-4 and N2 stage gastric tumor and should not be utilized for EGC and total gastrectomy[62].
So, the D2 lymphadenectomy is the gold standard in R0 resection by the Japanese[49] and European guidelines[27].
The American NCCN guidelines recommend a D1+ or a modified D2 LN dissection, the latter performed by experienced surgeons in high-volume centers[27,63]. To support this, the deployment of centralization and implementation of national clinical guidelines in Denmark resulted in a decrease in mortality from 8.2% to 2.4% and the proportion of patients with at least 15 LNs removed has increased from 19% to 76%[64].
MARUYAMA COMPUTER PROGRAM
The Maruyama computer program (MCP) was developed and first published in 1989[65]. It was later improved as the Windows-based program WinEstimate v. 2.5 using a database of 4302 primary gastric cancer patients treated at the National Cancer Center Hospital in Tokyo between 1968 and 1989[66,67]. This program calculates the expectation (%) of lymph-node involvement in station No. 1-16. The calculation required the following prognostic factors: Age, gender, position of the tumor, Bormann’s classification or EGC classification, depth of infiltration and histological type (Figure 1)[68]. MCP was validated in Japanese patients and the program was able to predict LN involvement in 94%[69]. In the European region the accuracy of MCP was 91% in Slovenian patients[67] and 83.4% for stations 1 to 6 and 81.6% for stations 7 to 12 in Italian patients[70]. The sensitivity for LN detection was high (97%-100%) in a German study of 222 patients but a specificity as low as 20% was found for perigastric LNs (stations 1 to 6)[68,71]. Similarly in an Italian study, where the sensitivity increased to 100% with a lower cut-off level, the specificity decreased to 26%. Better prediction of LN metastases may be feasible with the artificial neural network using the following parameters: Bormann classification, depth of tumor infiltration, size, location of tumor, and LN metastases in station 3. These increased accuracy from 66% to 93%[72].
Figure 1.
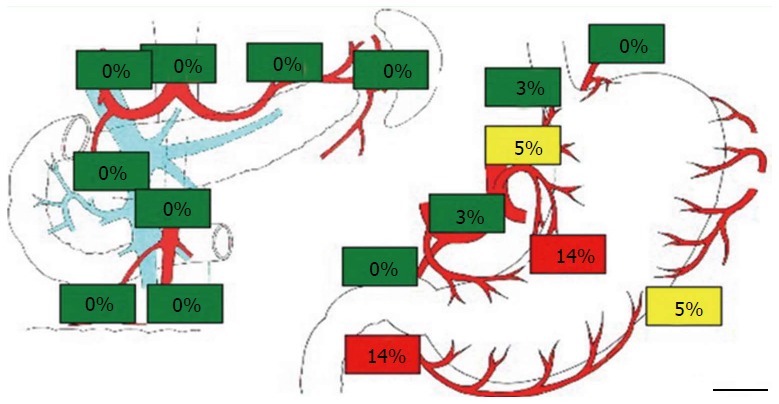
Prediction of lymph node involvement by the Maruyama computer program in a 65-year-old male patient. The tumor histology was well differentiated adenocarcinoma, showing muscular mucosa involvement, early cancer type 2B. The lesion was found in the anterior wall in the lower third of the stomach and had a maximal diameter of 30 mm.
Our study demonstrated a similar degree of reliability of MCP to those cited above, with 90.2% of sensitivity, 63.3% of specificity and 78.4% of accuracy. The rate of false negatives was 9.8%[73]. These studies demonstrate that the results of the computerized prediction of LN metastases are superior to those of the standard pre-operative imaging techniques.
Another advantage of the MCP is that it can determine long term oncological results. Hundahl defined the Maruyama Index (MI) at first in 2002 as a measure of unresected regional nodal disease in gastric cancer using the data of the Intergroup 0116 trial and he proved it is an independent predictor of survival[74,75]. Peeters et al[76] reanalyzed the data of the Dutch D1-D2 trial using univariate and multivariate analyses and showed that the MI is an independent predictor of overall survival (P = 0.016, HR = 1.45) and relapse risk (P = 0.010, HR = 1.72). It was concluded that the MI is a quantitative yardstick for assessing the adequacy of lymphadenectomy in gastric cancer patients[75,76]. Later, Hundahl evaluated autopsy findings from the Dutch D1-D2 trial and showed that MI < 5 or a low MI for surgery is associated with enhanced regional control and survival[76,77]. Dikken et al[78] proved the prognostic significance of low MI in a 2-year survival rate (82% vs 59%), as did Sachdev, who demonstrated that lower MI correlated with better survival, as a continuous (P < 0.02) and categorical (P < 0.04) variable[79].
Overall these results suggest that a Maruyama Index less than 5 has a better impact on survival, than D-level guided surgery. For these reasons, the preoperative application of MCP is recommended routinely, with an aim to perform “low Maruyama Index surgery”. In addition, the application of MCP to predict LN involvement can influence the indication for neoadjuvant chemo-therapy, and furthermore a “high Maruyama Index” could indicate the necessity for postoperative oncological treatment.
SENTINEL LYMPH NODE BIOPSY
While the MCP calculates the probability of LN involvement preoperatively, the concept of sentinel lymph node biopsy (SNB) can determine the existence of LN metastases intraoperatively. The first potentially affected LN, the sentinel lymph node (SLN), reliably reflects the status of the nodes in the second and third line, which is supported by data of numerous publications. If the SLN contains tumor deposit(s), extended dissection is warranted, but if findings are negative, the patient could be spared additional complications associated with extended dissection. However, the method of dye/tracer injection and the tracer’s selection is controversial. Some authors use dye alone (patent blue, indocyanine green, isosulfan blue)[11,80-82], Kitagawa et al[83] handle 99m Tc colloid, and Aikou et al[84] uses the combination of these tracers. The latest systematic review concluded that the SLN’s identification rate is the same with the dual or single mapping method[85]. It is eminent that body-mass index (BMI) affects the sentinel LN detection rate[86]. The Hungarian study proved that the identification of sentinel LNs in obese patients can be difficult owing to the feathering of blue dye in the fatty tissues[11]. This was concluded as the only patient in whom marking did not occur had a BMI significantly higher than average (26.8 vs 22.8)[11]. Then again, the application of blue dye for SNB has a beneficial side effect, as it significantly increased the number of harvested LN and the ratio of the number of the harvested LN per time[87]. To avoid quick dispersal to multiple LNs Kong applied ICG/poly-γ-glutamic acid complex, which remained longer than diluted ICG in animal models[88].
Yaguchi, Lee and Tóth have compared the subserosal to the submucosal labeling method (Figures 2 and 3) without any significant difference and they suggest the endoscopic injection of a tracer in cases of non-palpable tumors and/or laparoscopic procedures[89-91].
Figure 2.

Sentinel lymph node mapping following submucosal marking by an endoscopist.
Figure 3.
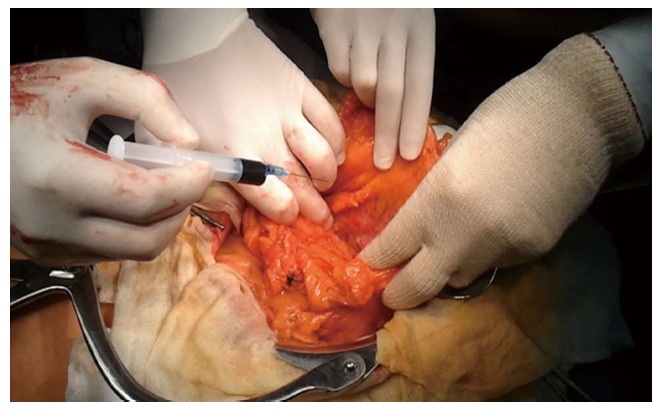
Subserosal marking by a surgeon.
The cardinal problem in the SNB concept is the intraoperative false negative rate. The JCOG 0302 trial called attention to the importance of the learning curve and the inadequacy of the pick-up method. The demand for only five patients per institute provided an insufficient learning period which presented a 46% false negative rate[92].
Lee et al[93] proved that the removal of entire nodal basins can significantly decrease this rate against the pick-up method, and Kumagai et al[94] called attention to the opportunity of introducing the one-step nucleic acid amplification test for the intraoperative diagnosis of LN metastasis with similar results to postoperative 2-mm-interval histological examination.
Miyashiro et al[95] demonstrated that an extensive surgical experience is necessary for application of SNB concept and standardization of SLN mapping technique, using improved tracer, and guideline to evaluate the positiveness of SLN specimen should be planned to incorporate SNB in routine practice[96]. Recent studies and the latest meta-analysis of SLN mapping have shown a high detection rate (93.7%) and an accuracy of 92%[97] and suggest that the SNB concept could be suitable for tumors following endoscopic resection[98] and could represent a new era of sentinel node navigation surgery in EGC[99,100]. Moreover, its success rate did not correlate to tumor grade[101].
Based on the results of the largest prospective multicenter trial from Japan with an identification rate of 97.5% and an accuracy of 99%[102], a phase III multi-center trial for individualized surgery for EGC based on SLN mapping has been commenced in the Eastern Asian countries. The long-term results of these studies will be available between 2018 and 2020.
CONCLUSION
The latest RCT comparing D1 and D2 dissections represents a higher surgical quality (more contamination, less non-compliance, low morbidity and mortality rate) than previous trials[43]. This could lead to a trend towards the execution of the less limited D1 lymphadenectomy for more experienced and well-trained surgeons, and hopefully the results of western surgeons will achieve a level similar to those of the Asian surgical outcomes in the near future.
On the other hand, the era of multimodal treatment and the increase in elderly patients with serious comorbidities indicates the necessity of a stage- and patient-adapted, individualized surgery in gastric cancer. It was conceived at an expert panel, also: “A D2 lymphadenectomy is preferred for curative-intent resection in advanced, non-metastatic gastric cancer; in patients with EGC or substantial comorbidities, a D1 lymphadenectomy is more appropriate”[103]. The Japanese guidelines enclose that the AGC should be treated with D2 lymphadenectomy. D1 or D1+ should be recommended as a choice for EGC. D1+ can be an alternate for D2 in high-risk patients[104]. Inokuchi et al[105] suggested that the presence of heart or liver disease is a significant risk factor for postoperative morbidity in patients who undergo laparoscopic gastrectomy. Although it did not reduce complications, insufficient LN dissection (for example, D1+ for advanced gastric cancer) might be permissible in high-risk patients as it had no negative impact on gastric cancer-specific survival. More accurate stage-adapted surgery could be performed using the MCP and SNB in parallel fashion.
It is generally accepted that metastases in the SLNs warrant a D2 lymphadenectomy. The authors analyzed the relevance of MCP in sentinel node positive patients in an earlier study[73]; while the efficiency of SNB method is superior to MCP, the positive predictive value of MCP and SNB was proven equivalent in the sentinel node positive group and the accuracy of MCP in these cohort of patients was 10% higher. For these reasons it would be interesting to find the appropriate combination of these techniques in the future and we suggest using them simultaneously in the operating room.
Footnotes
Conflict-of-interest statement: The authors have no conflicts of interest to disclose.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: April 26, 2015
First decision: August 1, 2015
Article in press: December 18, 2015
P- Reviewer: Nomura S S- Editor: Ji FF L- Editor: A E- Editor: Li D
References
- 1.Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 2.Kooby DA, Suriawinata A, Klimstra DS, Brennan MF, Karpeh MS. Biologic predictors of survival in node-negative gastric cancer. Ann Surg. 2003;237:828–835; discussion 835-837. doi: 10.1097/01.SLA.0000072260.77776.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nakamura K, Ueyama T, Yao T, Xuan ZX, Ambe K, Adachi Y, Yakeishi Y, Matsukuma A, Enjoji M. Pathology and prognosis of gastric carcinoma. Findings in 10,000 patients who underwent primary gastrectomy. Cancer. 1992;70:1030–1037. doi: 10.1002/1097-0142(19920901)70:5<1030::aid-cncr2820700504>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 4.Adachi Y, Mori M, Maehara Y, Sugimachi K. Long-term survival after resection for advanced gastric carcinoma. J Clin Gastroenterol. 1995;21:208–210. doi: 10.1097/00004836-199510000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Roukos DH. Current status and future perspectives in gastric cancer management. Cancer Treat Rev. 2000;26:243–255. doi: 10.1053/ctrv.2000.0164. [DOI] [PubMed] [Google Scholar]
- 6.Siewert JR, Böttcher K, Stein HJ, Roder JD. Relevant prognostic factors in gastric cancer: ten-year results of the German Gastric Cancer Study. Ann Surg. 1998;228:449–461. doi: 10.1097/00000658-199810000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Choi YY, An JY, Cho I, Kwon IG, Kang DR, Hyung WJ, Noh SH. The assessment of the oncological safety margin of insufficient lymph node dissection in pT2 (pm) gastric cancer. Yonsei Med J. 2014;55:61–69. doi: 10.3349/ymj.2014.55.1.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Deng JY, Liang H, Sun D, Zhan HJ, Zhang RP. Analysis of risk factors for the interval time, number and pattern of hepatic metastases from gastric cancer after radical gastrectomy. World J Gastroenterol. 2008;14:2440–2447. doi: 10.3748/wjg.14.2440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nakamura K, Morisaki T, Sugitani A, Ogawa T, Uchiyama A, Kinukawa N, Tanaka M. An early gastric carcinoma treatment strategy based on analysis of lymph node metastasis. Cancer. 1999;85:1500–1505. [PubMed] [Google Scholar]
- 10.Kodera Y, Yamamura Y, Shimizu Y, Torii A, Hirai T, Yasui K, Morimoto T, Kato T, Kito T. Lymph node status assessment for gastric carcinoma: is the number of metastatic lymph nodes really practical as a parameter for N categories in the TNM Classification? Tumor Node Metastasis. J Surg Oncol. 1998;69:15–20. doi: 10.1002/(sici)1096-9098(199809)69:1<15::aid-jso4>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 11.Tóth D, Kincses Z, Plósz J, Török M, Kovács I, Kiss C, Damjanovich L. Value of sentinel lymph node mapping using a blue dye-only method in gastric cancer: a single-center experience from North-East Hungary. Gastric Cancer. 2011;14:360–364. doi: 10.1007/s10120-011-0048-y. [DOI] [PubMed] [Google Scholar]
- 12.Chamadol N, Wongwiwatchai J, Bhudhisawasd V, Pairojkul C. Accuracy of spiral CT in preoperative staging of gastric carcinoma: correlation with surgical and pathological findings. J Med Assoc Thai. 2008;91:356–363. [PubMed] [Google Scholar]
- 13.Xi WD, Zhao C, Ren GS. Endoscopic ultrasonography in preoperative staging of gastric cancer: determination of tumor invasion depth, nodal involvement and surgical resectability. World J Gastroenterol. 2003;9:254–257. doi: 10.3748/wjg.v9.i2.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zuo CH, Xie H, Liu J, Qiu XX, Lin JG, Hua X, Qin A. Characterization of lymph node metastasis and its clinical significance in the surgical treatment of gastric cancer. Mol Clin Oncol. 2014;2:821–826. doi: 10.3892/mco.2014.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gertler R, Stein HJ, Schuster T, Rondak IC, Höfler H, Feith M. Prevalence and topography of lymph node metastases in early esophageal and gastric cancer. Ann Surg. 2014;259:96–101. doi: 10.1097/SLA.0000000000000239. [DOI] [PubMed] [Google Scholar]
- 16.Huang CM, Xu M, Wang JB, Zheng CH, Li P, Xie JW, Lin JX, Lu J. Is tumor size a predictor of preoperative N staging in T2-T4a stage advanced gastric cancer? Surg Oncol. 2014;23:5–10. doi: 10.1016/j.suronc.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 17.Bravo Neto GP, dos Santos EG, Victer FC, Carvalho CE. Lymph node metastasis in early gastric cancer. Rev Col Bras Cir. 2014;41:11–17. doi: 10.1590/s0100-69912014000100004. [DOI] [PubMed] [Google Scholar]
- 18.Yang HJ, Kim SG, Lim JH, Choi J, Im JP, Kim JS, Kim WH, Jung HC. Predictors of lymph node metastasis in patients with non-curative endoscopic resection of early gastric cancer. Surg Endosc. 2015;29:1145–1155. doi: 10.1007/s00464-014-3780-7. [DOI] [PubMed] [Google Scholar]
- 19.Lee JH, Kim MG, Jung MS, Kwon SJ. Prognostic significance of lymphovascular invasion in node-negative gastric cancer. World J Surg. 2015;39:732–739. doi: 10.1007/s00268-014-2846-y. [DOI] [PubMed] [Google Scholar]
- 20.Kim JJ, Song KY, Hur H, Hur JI, Park SM, Park CH. Lymph node micrometastasis in node negative early gastric cancer. Eur J Surg Oncol. 2009;35:409–414. doi: 10.1016/j.ejso.2008.05.004. [DOI] [PubMed] [Google Scholar]
- 21.Jeuck TL, Wittekind C. Gastric carcinoma: stage migration by immunohistochemically detected lymph node micrometastases. Gastric Cancer. 2015;18:100–108. doi: 10.1007/s10120-014-0352-4. [DOI] [PubMed] [Google Scholar]
- 22.Kubota K, Nakanishi H, Hiki N, Shimizu N, Tsuji E, Yamaguchi H, Mafune K, Tange T, Tatematsu M, Kaminishi M. Quantitative detection of micrometastases in the lymph nodes of gastric cancer patients with real-time RT-PCR: a comparative study with immunohistochemistry. Int J Cancer. 2003;105:136–143. doi: 10.1002/ijc.11031. [DOI] [PubMed] [Google Scholar]
- 23.Jiao XG, Deng JY, Zhang RP, Wu LL, Wang L, Liu HG, Hao XS, Liang H. Prognostic value of number of examined lymph nodes in patients with node-negative gastric cancer. World J Gastroenterol. 2014;20:3640–3648. doi: 10.3748/wjg.v20.i13.3640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Song W, Yuan Y, Wang L, He W, Zhang X, Chen C, Zhang C, Cai S, He Y. The prognostic value of lymph nodes dissection number on survival of patients with lymph node-negative gastric cancer. Gastroenterol Res Pract. 2014;2014:603194. doi: 10.1155/2014/603194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Deng JY, Liang H. Clinical significance of lymph node metastasis in gastric cancer. World J Gastroenterol. 2014;20:3967–3975. doi: 10.3748/wjg.v20.i14.3967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schmidt B, Yoon SS. D1 versus D2 lymphadenectomy for gastric cancer. J Surg Oncol. 2013;107:259–264. doi: 10.1002/jso.23127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Verlato G, Giacopuzzi S, Bencivenga M, Morgagni P, De Manzoni G. Problems faced by evidence-based medicine in evaluating lymphadenectomy for gastric cancer. World J Gastroenterol. 2014;20:12883–12891. doi: 10.3748/wjg.v20.i36.12883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359–E386. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- 29.Smith DL, Elting LS, Learn PA, Raut CP, Mansfield PF. Factors influencing the volume-outcome relationship in gastrectomies: a population-based study. Ann Surg Oncol. 2007;14:1846–1852. doi: 10.1245/s10434-007-9381-0. [DOI] [PubMed] [Google Scholar]
- 30.Coburn NG, Swallow CJ, Kiss A, Law C. Significant regional variation in adequacy of lymph node assessment and survival in gastric cancer. Cancer. 2006;107:2143–2151. doi: 10.1002/cncr.22229. [DOI] [PubMed] [Google Scholar]
- 31.Hannan EL, Radzyner M, Rubin D, Dougherty J, Brennan MF. The influence of hospital and surgeon volume on in-hospital mortality for colectomy, gastrectomy, and lung lobectomy in patients with cancer. Surgery. 2002;131:6–15. doi: 10.1067/msy.2002.120238. [DOI] [PubMed] [Google Scholar]
- 32.Dent DM, Madden MV, Price SK. Randomized comparison of R1 and R2 gastrectomy for gastric carcinoma. Br J Surg. 1988;75:110–112. doi: 10.1002/bjs.1800750206. [DOI] [PubMed] [Google Scholar]
- 33.Cuschieri A, Fayers P, Fielding J, Craven J, Bancewicz J, Joypaul V, Cook P. Postoperative morbidity and mortality after D1 and D2 resections for gastric cancer: preliminary results of the MRC randomised controlled surgical trial. The Surgical Cooperative Group. Lancet. 1996;347:995–999. doi: 10.1016/s0140-6736(96)90144-0. [DOI] [PubMed] [Google Scholar]
- 34.Bonenkamp JJ, Songun I, Hermans J, Sasako M, Welvaart K, Plukker JT, van Elk P, Obertop H, Gouma DJ, Taat CW. Randomised comparison of morbidity after D1 and D2 dissection for gastric cancer in 996 Dutch patients. Lancet. 1995;345:745–748. doi: 10.1016/s0140-6736(95)90637-1. [DOI] [PubMed] [Google Scholar]
- 35.Degiuli M, Sasako M, Ponti A. Morbidity and mortality in the Italian Gastric Cancer Study Group randomized clinical trial of D1 versus D2 resection for gastric cancer. Br J Surg. 2010;97:643–649. doi: 10.1002/bjs.6936. [DOI] [PubMed] [Google Scholar]
- 36.Cuschieri A, Weeden S, Fielding J, Bancewicz J, Craven J, Joypaul V, Sydes M, Fayers P. Patient survival after D1 and D2 resections for gastric cancer: long-term results of the MRC randomized surgical trial. Surgical Co-operative Group. Br J Cancer. 1999;79:1522–1530. doi: 10.1038/sj.bjc.6690243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bonenkamp JJ, Hermans J, Sasako M, van de Velde CJ, Welvaart K, Songun I, Meyer S, Plukker JT, Van Elk P, Obertop H, et al. Extended lymph-node dissection for gastric cancer. N Engl J Med. 1999;340:908–914. doi: 10.1056/NEJM199903253401202. [DOI] [PubMed] [Google Scholar]
- 38.Songun I, Putter H, Kranenbarg EM, Sasako M, van de Velde CJ. Surgical treatment of gastric cancer: 15-year follow-up results of the randomised nationwide Dutch D1D2 trial. Lancet Oncol. 2010;11:439–449. doi: 10.1016/S1470-2045(10)70070-X. [DOI] [PubMed] [Google Scholar]
- 39.Wu CW, Hsiung CA, Lo SS, Hsieh MC, Shia LT, Whang-Peng J. Randomized clinical trial of morbidity after D1 and D3 surgery for gastric cancer. Br J Surg. 2004;91:283–287. doi: 10.1002/bjs.4433. [DOI] [PubMed] [Google Scholar]
- 40.Jiang L, Yang KH, Chen Y, Guan QL, Zhao P, Tian JH, Wang Q. Systematic review and meta-analysis of the effectiveness and safety of extended lymphadenectomy in patients with resectable gastric cancer. Br J Surg. 2014;101:595–604. doi: 10.1002/bjs.9497. [DOI] [PubMed] [Google Scholar]
- 41.Sano T, Sasako M, Yamamoto S, Nashimoto A, Kurita A, Hiratsuka M, Tsujinaka T, Kinoshita T, Arai K, Yamamura Y, et al. Gastric cancer surgery: morbidity and mortality results from a prospective randomized controlled trial comparing D2 and extended para-aortic lymphadenectomy--Japan Clinical Oncology Group study 9501. J Clin Oncol. 2004;22:2767–2773. doi: 10.1200/JCO.2004.10.184. [DOI] [PubMed] [Google Scholar]
- 42.Fujii M, Sasaki J, Nakajima T. State of the art in the treatment of gastric cancer: from the 71st Japanese Gastric Cancer Congress. Gastric Cancer. 1999;2:151–157. doi: 10.1007/s101200050039. [DOI] [PubMed] [Google Scholar]
- 43.Degiuli M, Sasako M, Ponti A, Vendrame A, Tomatis M, Mazza C, Borasi A, Capussotti L, Fronda G, Morino M. Randomized clinical trial comparing survival after D1 or D2 gastrectomy for gastric cancer. Br J Surg. 2014;101:23–31. doi: 10.1002/bjs.9345. [DOI] [PubMed] [Google Scholar]
- 44.Wu CW, Hsiung CA, Lo SS, Hsieh MC, Chen JH, Li AF, Lui WY, Whang-Peng J. Nodal dissection for patients with gastric cancer: a randomised controlled trial. Lancet Oncol. 2006;7:309–315. doi: 10.1016/S1470-2045(06)70623-4. [DOI] [PubMed] [Google Scholar]
- 45.El-Sedfy A, Dixon M, Seevaratnam R, Bocicariu A, Cardoso R, Mahar A, Kiss A, Helyer L, Law C, Coburn NG. Personalized Surgery for Gastric Adenocarcinoma: A Meta-analysis of D1 versus D2 Lymphadenectomy. Ann Surg Oncol. 2015;22:1820–1827. doi: 10.1245/s10434-014-4168-6. [DOI] [PubMed] [Google Scholar]
- 46.Xu D, Huang Y, Geng Q, Guan Y, Li Y, Wang W, Yuan S, Sun X, Chen Y, Li W, et al. Effect of lymph node number on survival of patients with lymph node-negative gastric cancer according to the 7th edition UICC TNM system. PLoS One. 2012;7:e38681. doi: 10.1371/journal.pone.0038681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Datta J, Lewis RS, Mamtani R, Stripp D, Kelz RR, Drebin JA, Fraker DL, Karakousis GC, Roses RE. Implications of inadequate lymph node staging in resectable gastric cancer: a contemporary analysis using the National Cancer Data Base. Cancer. 2014;120:2855–2865. doi: 10.1002/cncr.28780. [DOI] [PubMed] [Google Scholar]
- 48.Estes NC, MacDonald JS, Touijer K, Benedetti J, Jacobson J. Inadequate documentation and resection for gastric cancer in the United States: a preliminary report. Am Surg. 1998;64:680–685. [PubMed] [Google Scholar]
- 49.Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2010 (ver. 3) Gastric Cancer. 2011;14:113–123. doi: 10.1007/s10120-011-0042-4. [DOI] [PubMed] [Google Scholar]
- 50.Li C, Oh SJ, Kim S, Hyung WJ, Yan M, Zhu ZG, Noh SH. Macroscopic Borrmann type as a simple prognostic indicator in patients with advanced gastric cancer. Oncology. 2009;77:197–204. doi: 10.1159/000236018. [DOI] [PubMed] [Google Scholar]
- 51.Yang K, Zhang WH, Chen XZ, Chen XL, Zhang B, Chen ZX, Zhou ZG, Hu JK. Survival benefit and safety of no. 10 lymphadenectomy for gastric cancer patients with total gastrectomy. Medicine (Baltimore) 2014;93:e158. doi: 10.1097/MD.0000000000000158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Li P, Huang CM, Zheng CH, Xie JW, Wang JB, Lin JX, Lu J, Wang Y, Chen QY. Laparoscopic spleen-preserving splenic hilar lymphadenectomy in 108 consecutive patients with upper gastric cancer. World J Gastroenterol. 2014;20:11376–11383. doi: 10.3748/wjg.v20.i32.11376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Song W, He Y, Wang S, He W, Xu J. Significance of the lymph nodes in the 7th station in rational dissection for metastasis of distal gastric cancer with different T categories. Chin J Cancer Res. 2014;26:423–430. doi: 10.3978/j.issn.1000-9604.2014.08.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Galizia G, Lieto E, De Vita F, Castellano P, Ferraraccio F, Zamboli A, Mabilia A, Auricchio A, De Sena G, De Stefano L, et al. Modified versus standard D2 lymphadenectomy in total gastrectomy for nonjunctional gastric carcinoma with lymph node metastasis. Surgery. 2015;157:285–296. doi: 10.1016/j.surg.2014.09.012. [DOI] [PubMed] [Google Scholar]
- 55.Feng JF, Huang Y, Liu J, Liu H, Sheng HY, Wei WT, Lu WS, Chen DF, Chen WY, Zhou XM. Risk factors for No. 12p and No. 12b lymph node metastases in advanced gastric cancer in China. Ups J Med Sci. 2013;118:9–15. doi: 10.3109/03009734.2012.729103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lee SL, Lee HH, Ko YH, Song KY, Park CH, Jeon HM, Kim SS. Relevance of hepatoduodenal ligament lymph nodes in resectional surgery for gastric cancer. Br J Surg. 2014;101:518–522. doi: 10.1002/bjs.9438. [DOI] [PubMed] [Google Scholar]
- 57.Eom BW, Joo J, Kim YW, Reim D, Park JY, Yoon HM, Ryu KW, Lee JY, Kook MC. Improved survival after adding dissection of the superior mesenteric vein lymph node (14v) to standard D2 gastrectomy for advanced distal gastric cancer. Surgery. 2014;155:408–416. doi: 10.1016/j.surg.2013.08.019. [DOI] [PubMed] [Google Scholar]
- 58.Sasako M, Sano T, Yamamoto S, Kurokawa Y, Nashimoto A, Kurita A, Hiratsuka M, Tsujinaka T, Kinoshita T, Arai K, et al. D2 lymphadenectomy alone or with para-aortic nodal dissection for gastric cancer. N Engl J Med. 2008;359:453–462. doi: 10.1056/NEJMoa0707035. [DOI] [PubMed] [Google Scholar]
- 59.Robertson CS, Chung SC, Woods SD, Griffin SM, Raimes SA, Lau JT, Li AK. A prospective randomized trial comparing R1 subtotal gastrectomy with R3 total gastrectomy for antral cancer. Ann Surg. 1994;220:176–182. doi: 10.1097/00000658-199408000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Junfeng Z, Yingxue H, Peiwu Y. Systematic review of risk factors for metastasis to para-aortic lymph nodes in gastric cancer. Surg Oncol. 2013;22:210–216. doi: 10.1016/j.suronc.2013.10.003. [DOI] [PubMed] [Google Scholar]
- 61.de Manzoni G, Verlato G, Bencivenga M, Marrelli D, Di Leo A, Giacopuzzi S, Cipollari C, Roviello F. Impact of super-extended lymphadenectomy on relapse in advanced gastric cancer. Eur J Surg Oncol. 2015;41:534–540. doi: 10.1016/j.ejso.2015.01.023. [DOI] [PubMed] [Google Scholar]
- 62.Zhang Y, Tian S. Does D2 plus para-aortic nodal dissection surgery offer a better survival outcome compared to D2 surgery only for gastric cancer consistently? A definite result based on a hospital population of nearly two decades. Scand J Surg. 2013;102:251–257. doi: 10.1177/1457496913491343. [DOI] [PubMed] [Google Scholar]
- 63.Ajani JA, Bentrem DJ, Besh S, D’Amico TA, Das P, Denlinger C, Fakih MG, Fuchs CS, Gerdes H, Glasgow RE, et al. Gastric cancer, version 2.2013: featured updates to the NCCN Guidelines. J Natl Compr Canc Netw. 2013;11:531–546. doi: 10.6004/jnccn.2013.0070. [DOI] [PubMed] [Google Scholar]
- 64.Jensen LS, Nielsen H, Mortensen PB, Pilegaard HK, Johnsen SP. Enforcing centralization for gastric cancer in Denmark. Eur J Surg Oncol. 2010;36 Suppl 1:S50–S54. doi: 10.1016/j.ejso.2010.06.025. [DOI] [PubMed] [Google Scholar]
- 65.Kampschöer GH, Maruyama K, van de Velde CJ, Sasako M, Kinoshita T, Okabayashi K. Computer analysis in making preoperative decisions: a rational approach to lymph node dissection in gastric cancer patients. Br J Surg. 1989;76:905–908. doi: 10.1002/bjs.1800760910. [DOI] [PubMed] [Google Scholar]
- 66.Siewert JR, Kelsen D, Maruyama K, Feussner H, Omote K, Etter M, Hoos A. Gastric cancer diagnosis and treatment. An interactive training program. Windows Version. CD-ROM. Berlin Heidelberg. Springer-Verlag. 2000. [Google Scholar]
- 67.Omejc M, Mekicar J. Role of computer analysis in gastric cancer surgery: evaluation of the WinEstimate v. 2.5 computer program. World J Surg. 2004;28:59–62. doi: 10.1007/s00268-003-7007-7. [DOI] [PubMed] [Google Scholar]
- 68.Gretschel S, Bembenek A, Ulmer Ch, Hünerbein M, Markwardt J, Schneider U, Schlag PM. Prediction of gastric cancer lymph node status by sentinel lymph node biopsy and the Maruyama computer model. Eur J Surg Oncol. 2005;31:393–400. doi: 10.1016/j.ejso.2004.11.014. [DOI] [PubMed] [Google Scholar]
- 69.Maruyama K, Gunvén P, Okabayashi K, Sasako M, Kinoshita T. Lymph node metastases of gastric cancer. General pattern in 1931 patients. Ann Surg. 1989;210:596–602. doi: 10.1097/00000658-198911000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Guadagni S, de Manzoni G, Catarci M, Valenti M, Amicucci G, De Bernardinis G, Cordiano C, Carboni M, Maruyama K. Evaluation of the Maruyama computer program accuracy for preoperative estimation of lymph node metastases from gastric cancer. World J Surg. 2000;24:1550–1558. doi: 10.1007/s002680010276. [DOI] [PubMed] [Google Scholar]
- 71.Bollschweiler E, Boettcher K, Hoelscher AH, Sasako M, Kinoshita T, Maruyama K, Siewert JR. Preoperative assessment of lymph node metastases in patients with gastric cancer: evaluation of the Maruyama computer program. Br J Surg. 1992;79:156–160. doi: 10.1002/bjs.1800790221. [DOI] [PubMed] [Google Scholar]
- 72.Bollschweiler EH, Mönig SP, Hensler K, Baldus SE, Maruyama K, Hölscher AH. Artificial neural network for prediction of lymph node metastases in gastric cancer: a phase II diagnostic study. Ann Surg Oncol. 2004;11:506–511. doi: 10.1245/ASO.2004.04.018. [DOI] [PubMed] [Google Scholar]
- 73.Tóth D, Török M, Kincses Z, Damjanovich L. Prospective, comparative study for the evaluation of lymph node involvement in gastric cancer: Maruyama computer program versus sentinel lymph node biopsy. Gastric Cancer. 2013;16:201–207. doi: 10.1007/s10120-012-0170-5. [DOI] [PubMed] [Google Scholar]
- 74.Hundahl SA, Macdonald JS, Benedetti J, Fitzsimmons T. Surgical treatment variation in a prospective, randomized trial of chemoradiotherapy in gastric cancer: the effect of undertreatment. Ann Surg Oncol. 2002;9:278–286. doi: 10.1007/BF02573066. [DOI] [PubMed] [Google Scholar]
- 75.Yoo MW, Park do J, Ahn HS, Jeong SH, Lee HJ, Kim WH, Kim HH, Lee KU, Yang HK. Evaluation of the adequacy of lymph node dissection in pylorus-preserving gastrectomy for early gastric cancer using the maruyama index. World J Surg. 2010;34:291–295. doi: 10.1007/s00268-009-0318-6. [DOI] [PubMed] [Google Scholar]
- 76.Peeters KC, Hundahl SA, Kranenbarg EK, Hartgrink H, van de Velde CJ. Low Maruyama index surgery for gastric cancer: blinded reanalysis of the Dutch D1-D2 trial. World J Surg. 2005;29:1576–1584. doi: 10.1007/s00268-005-7907-9. [DOI] [PubMed] [Google Scholar]
- 77.Hundahl SA. Low maruyama index surgery for gastric cancer. Scand J Surg. 2006;95:243–248. doi: 10.1177/145749690609500406. [DOI] [PubMed] [Google Scholar]
- 78.Dikken JL, Jansen EP, Cats A, Bakker B, Hartgrink HH, Kranenbarg EM, Boot H, Putter H, Peeters KC, van de Velde CJ, et al. Impact of the extent of surgery and postoperative chemoradiotherapy on recurrence patterns in gastric cancer. J Clin Oncol. 2010;28:2430–2436. doi: 10.1200/JCO.2009.26.9654. [DOI] [PubMed] [Google Scholar]
- 79.Sachdev JC, Evangelist M, Orr WS. Maruyama index (MI) and outcomes of gastric cancer resection. J Clin Oncol. 2010:28 suppl; abstr 4154. [Google Scholar]
- 80.Rino Y, Takanashi Y, Hasuo K, Kawamoto M, Ashida A, Harada H, Inagaki D, Hatori S, Ohshima T, Yamada R, et al. The validity of sentinel lymph node biopsy using dye technique alone in patients with gastric cancer. Hepatogastroenterology. 2007;54:1882–1886. [PubMed] [Google Scholar]
- 81.Tajima Y, Yamazaki K, Masuda Y, Kato M, Yasuda D, Aoki T, Kato T, Murakami M, Miwa M, Kusano M. Sentinel node mapping guided by indocyanine green fluorescence imaging in gastric cancer. Ann Surg. 2009;249:58–62. doi: 10.1097/SLA.0b013e3181927267. [DOI] [PubMed] [Google Scholar]
- 82.Ryu KW, Lee JH, Kim HS, Kim YW, Choi IJ, Bae JM. Prediction of lymph nodes metastasis by sentinel node biopsy in gastric cancer. Eur J Surg Oncol. 2003;29:895–899. doi: 10.1016/j.ejso.2003.09.008. [DOI] [PubMed] [Google Scholar]
- 83.Kitagawa Y, Fujii H, Mukai M, Kubota T, Otani Y, Kitajima M. Radio-guided sentinel node detection for gastric cancer. Br J Surg. 2002;89:604–608. doi: 10.1046/j.1365-2168.2002.02065.x. [DOI] [PubMed] [Google Scholar]
- 84.Aikou T, Higashi H, Natsugoe S, Hokita S, Baba M, Tako S. Can sentinel node navigation surgery reduce the extent of lymph node dissection in gastric cancer? Ann Surg Oncol. 2001;8:90S–93S. [PubMed] [Google Scholar]
- 85.Cardoso R, Bocicariu A, Dixon M, Yohanathan L, Seevaratnam R, Helyer L, Law C, Coburn NG. What is the accuracy of sentinel lymph node biopsy for gastric cancer? A systematic review. Gastric Cancer. 2012;15 Suppl 1:S48–S59. doi: 10.1007/s10120-011-0103-8. [DOI] [PubMed] [Google Scholar]
- 86.Nakahara T, Kitagawa Y, Yakeuchi H, Fujii H, Suzuki T, Mukai M, Kitajima M, Kubo A. Preoperative lymphoscintigraphy for detection of sentinel lymph node in patients with gastric cancer--initial experience. Ann Surg Oncol. 2008;15:1447–1453. doi: 10.1245/s10434-008-9829-x. [DOI] [PubMed] [Google Scholar]
- 87.Aoyama T, Fujikawa H, Cho H, Ogata T, Shirai J, Hayashi T, Rino Y, Masuda M, Oba MS, Morita S, et al. A methylene blue-assisted technique for harvesting lymph nodes after radical surgery for gastric cancer: a prospective, randomized, controlled study. Am J Surg Pathol. 2015;39:266–273. doi: 10.1097/PAS.0000000000000336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Kong SH, Noh YW, Suh YS, Park HS, Lee HJ, Kang KW, Kim HC, Lim YT, Yang HK. Evaluation of the novel near-infrared fluorescence tracers pullulan polymer nanogel and indocyanine green/γ-glutamic acid complex for sentinel lymph node navigation surgery in large animal models. Gastric Cancer. 2015;18:55–64. doi: 10.1007/s10120-014-0345-3. [DOI] [PubMed] [Google Scholar]
- 89.Yaguchi Y, Ichikura T, Ono S, Tsujimoto H, Sugasawa H, Sakamoto N, Matsumoto Y, Yoshida K, Kosuda S, Hase K. How should tracers be injected to detect for sentinel nodes in gastric cancer--submucosally from inside or subserosally from outside of the stomach? J Exp Clin Cancer Res. 2008;27:79. doi: 10.1186/1756-9966-27-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Lee JH, Ryu KW, Kim CG, Kim SK, Choi IJ, Kim YW, Chang HJ, Bae JM, Hong EK. Comparative study of the subserosal versus submucosal dye injection method for sentinel node biopsy in gastric cancer. Eur J Surg Oncol. 2005;31:965–968. doi: 10.1016/j.ejso.2005.03.006. [DOI] [PubMed] [Google Scholar]
- 91.Tóth D, Kathy S, Csobán T, Kincses Z, Török M, Plósz J, Damjanovich L. [Prospective comparative study of sentinel lymph node mapping in gastric cancer -- submucosal versus subserosal marking method] Magy Seb. 2012;65:3–8. doi: 10.1556/MaSeb.65.2012.1.1. [DOI] [PubMed] [Google Scholar]
- 92.Miyashiro I, Hiratsuka M, Sasako M, Sano T, Mizusawa J, Nakamura K, Nashimoto A, Tsuburaya A, Fukushima N. High false-negative proportion of intraoperative histological examination as a serious problem for clinical application of sentinel node biopsy for early gastric cancer: final results of the Japan Clinical Oncology Group multicenter trial JCOG0302. Gastric Cancer. 2014;17:316–323. doi: 10.1007/s10120-013-0285-3. [DOI] [PubMed] [Google Scholar]
- 93.Lee YJ, Ha WS, Park ST, Choi SK, Hong SC, Park JW. Which biopsy method is more suitable between a basin dissection and pick-up biopsy for sentinel nodes in laparoscopic sentinel-node navigation surgery (LSNNS) for gastric cancer? J Laparoendosc Adv Surg Tech A. 2008;18:357–363. doi: 10.1089/lap.2007.0024. [DOI] [PubMed] [Google Scholar]
- 94.Kumagai K, Yamamoto N, Miyashiro I, Tomita Y, Katai H, Kushima R, Tsuda H, Kitagawa Y, Takeuchi H, Mukai M, et al. Multicenter study evaluating the clinical performance of the OSNA assay for the molecular detection of lymph node metastases in gastric cancer patients. Gastric Cancer. 2014;17:273–280. doi: 10.1007/s10120-013-0271-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Miyashiro I, Hiratsuka M, Kishi K, Takachi K, Yano M, Takenaka A, Tomita Y, Ishiguro S. Intraoperative diagnosis using sentinel node biopsy with indocyanine green dye in gastric cancer surgery: an institutional trial by experienced surgeons. Ann Surg Oncol. 2013;20:542–546. doi: 10.1245/s10434-012-2608-8. [DOI] [PubMed] [Google Scholar]
- 96.Yashiro M, Matsuoka T. Sentinel node navigation surgery for gastric cancer: Overview and perspective. World J Gastrointest Surg. 2015;7:1–9. doi: 10.4240/wjgs.v7.i1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Wang Z, Dong ZY, Chen JQ, Liu JL. Diagnostic value of sentinel lymph node biopsy in gastric cancer: a meta-analysis. Ann Surg Oncol. 2012;19:1541–1550. doi: 10.1245/s10434-011-2124-2. [DOI] [PubMed] [Google Scholar]
- 98.Mayanagi S, Takeuchi H, Kamiya S, Niihara M, Nakamura R, Takahashi T, Wada N, Kawakubo H, Saikawa Y, Omori T, et al. Suitability of sentinel node mapping as an index of metastasis in early gastric cancer following endoscopic resection. Ann Surg Oncol. 2014;21:2987–2993. doi: 10.1245/s10434-014-3662-1. [DOI] [PubMed] [Google Scholar]
- 99.Wang L, Ren W, Fan CQ, Li YH, Zhang X, Yu J, Zhao GC, Zhao XY. Full-thickness endoscopic resection of nonintracavitary gastric stromal tumors: a novel approach. Surg Endosc. 2011;25:641–647. doi: 10.1007/s00464-010-1189-5. [DOI] [PubMed] [Google Scholar]
- 100.Kong SH, Diana M, Liu YY, Lee HJ, Legner A, Soares R, Swanström L, Dallemagne B, Yang HK, Marescaux J. Novel method for hybrid endo-laparoscopic full-thickness gastric resection using laparoscopic transgastric suture passer device. Surg Endosc. 2015:Epub ahead of print. doi: 10.1007/s00464-015-4375-7. [DOI] [PubMed] [Google Scholar]
- 101.Lavy R, Kapiev A, Hershkovitz Y, Poluksht N, Rabin I, Chikman B, Shapira Z, Wasserman I, Sandbank J, Halevy A. Tumor differentiation as related to sentinel lymph node status in gastric cancer. World J Gastrointest Surg. 2014;6:1–4. doi: 10.4240/wjgs.v6.i1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Kitagawa Y, Takeuchi H, Takagi Y, Natsugoe S, Terashima M, Murakami N, Fujimura T, Tsujimoto H, Hayashi H, Yoshimizu N, et al. Sentinel node mapping for gastric cancer: a prospective multicenter trial in Japan. J Clin Oncol. 2013;31:3704–3710. doi: 10.1200/JCO.2013.50.3789. [DOI] [PubMed] [Google Scholar]
- 103.Brar S, Law C, McLeod R, Helyer L, Swallow C, Paszat L, Seevaratnam R, Cardoso R, Dixon M, Mahar A, et al. Defining surgical quality in gastric cancer: a RAND/UCLA appropriateness study. J Am Coll Surg. 2013;217:347–57.e1. doi: 10.1016/j.jamcollsurg.2013.01.067. [DOI] [PubMed] [Google Scholar]
- 104.Sano T, Aiko T. New Japanese classifications and treatment guidelines for gastric cancer: revision concepts and major revised points. Gastric Cancer. 2011;14:97–100. doi: 10.1007/s10120-011-0040-6. [DOI] [PubMed] [Google Scholar]
- 105.Inokuchi M, Kato K, Sugita H, Otsuki S, Kojima K. Impact of comorbidities on postoperative complications in patients undergoing laparoscopy-assisted gastrectomy for gastric cancer. BMC Surg. 2014;14:97. doi: 10.1186/1471-2482-14-97. [DOI] [PMC free article] [PubMed] [Google Scholar]


