Abstract
Aim:
Recent evidence shows that cultured mycelium Cordyceps sinensis (CMCS) effectively protects against liver fibrosis in mice. Here, we investigated whether the anti-fibrotic action of CMCS was related to its regulation of the activity of hepatic natural killer (NK) cells in CCl4-treated mice.
Methods:
C57BL/6 mice were injected with 10% CCl4 (2 mL/kg, ip) 3 times per week for 4 weeks, and received CMCS (120 mg·kg−1·d−1, ig) during this period. In another part of experiments, the mice were also injected with an NK cell-deleting antibody ASGM-1 (20 μg, ip) 5 times in the first 3 weeks. After the mice were sacrificed, serum liver function, and liver inflammation, hydroxyproline content and collagen deposition were assessed. The numbers of hepatic NK cells and expression of NKG2D (activation receptor of NK cells) on isolated liver lymphocytes were analyzed using flow cytometry. Desmin expression and cell apoptosis in liver tissues were studied using desmin staining and TUNEL assay, respectively. The levels of α-SMA, TGF-β, RAE-1δ and RAE-1ε in liver tissues were determined by RT-qPCR.
Results:
In CCl4-treated mice, CMCS administration significantly improved liver function, attenuated liver inflammation and fibrosis, and increased the numbers of hepatic NK cells and expression level of NKG2D on hepatic NK cells. Furthermore, CMCS administration significantly decreased desmin expression in liver tissues, and increased TUNEL staining adjacent to hepatic stellate cells. Injection with NK cell-deleting ASGM-1 not only diminished the numbers of hepatic NK cells, but also greatly accelerated liver inflammation and fibrosis in CCl4-treated mice. In CCl4-treated mice with NK cell depletion, CMCS administration decelerated the rate of liver fibrosis development, and mildly upregulated the numbers of hepatic NK cells but without changing NKG2D expression.
Conclusion:
CMCS allevi¬ates CCl4-induced liver inflammation and fibrosis via promoting activation of hepatic NK cells. CMCS partially reverses ASGM-1-induced depletion of hepatic NK cells.
Keywords: liver fibrosis, Chinese herb medicine, cultured mycelium Cordyceps sinensis, carbon tetrachloride, hepatic natural killer cells, ASGM-1
Introduction
Liver fibrosis is a progressive pathological process in which wound-healing myofibroblasts of the liver respond to injury by promoting the replacement of normal hepatic tissue with a scar-like matrix composed of cross-linked collagen1. Hepatic stellate cells (HSCs) are quiescent in a healthy liver and play a central role in the storage of vitamin A. When injury occurs, HSCs become activated and transdifferentiate into myofibroblasts2, which express α-smooth muscle actin (α-SMA). Accumulated evidence suggests that the activation of HSCs is a key step in the development of liver fibrosis, and hepatic fibrosis was once considered irreversible3. By contrast, advanced liver fibrosis is potentially reversible via the induction of HSC apoptosis. Consequently, there is now considerable interest in promoting HSC apoptosis and in the discovery of drugs that will induce HSC apoptosis in a selective manner.
Natural killer (NK) cells are lymphocytes of the innate immune system and are present among total blood lymphocytes and in various tissues, including the bone marrow, spleen, liver, intestine, placenta and lung4. Accumulating evidence suggests that the function of NK cells is strongly influenced by the tissue microenvironment5. The decision to kill a target cell depends on the net balance of signals delivered by inhibitory and activating receptor molecules that are expressed on the NK cell surface. The inhibitory receptors, which subsequently inactivate NK cell functions, include killer Ig-like receptors, Ly-49A and CD94/NKG2 receptors that recognize MHC class I molecules (inhibitory ligands). The stimulatory receptors, which are collectively referred to as natural cytotoxicity receptors, include NKp46, NKp30 and NKp44, NKG2D and DNAX accessory molecule-1 (CD226)6,7,8. Among these, NKG2D is the most well-defined receptor. NKG2D binds to its ligands (eg, RAE-1δ and RAE-1ε on HSCs in C57BL/6 mice) expressed on target cells and subsequently promotes NK cell activation8. In a healthy liver, NK cells have a cytotoxic role against stressed, transformed or infected cells by integrating several signals that are transduced by various activating and inhibitory surface receptors without prior sensitization6, as compared with peripheral NK cells9. Healthy liver NK cells play critical roles in controlling liver fibrogenesis by recognizing and killing activated HSCs10,11, as demonstrated in both animal models and patients12,13,14. NK cells have been shown to selectively recognize and kill early activated HSCs rather than quiescent or fully activated HSCs (myofibroblasts)15. In addition, the anti-fibrogenic effects of NK cells have been shown to be suppressed during advanced liver injury due to the increased production of transforming growth factor-beta (TGF-β) in intermediately activated HSCs16. Thus, down-regulation of the activities of NK cells may contribute to the progression of liver fibrosis.
The cultured mycelium Cordyceps sinensis (CMCS), a Chinese herbal medicine, is capable of inhibiting inflammation and regulating the immune system17. The number and cytotoxicity of NK cells have been reported to increase significantly in response to C. sinensis both in vitro and in vivo18,19,20. Our previous study revealed that CMCS could inhibit liver fibrosis and had no nocuous effects on normal tissues21,22. Nevertheless, the mechanism by which CMCS protects against liver fibrosis and whether an immunological response may be involved in this process remain unclear. Because CMCS can rescue the functions of weakened NK cells in different types of diseases, the aim of this study was to explore whether the anti-fibrotic effect of CMCS is related to its regulation of NK cell activities.
Materials and methods
Reagents
Analytical reagent grade carbon tetrachloride (CCl4) was obtained from Sinopharm Group Co, Ltd (Shanghai, China). All other chemicals and solvents were of analytical grade.
Drug preparation
CMCS in powder form was purchased from Shanghai Sundise Chinese Medicine Technology Development Co, Ltd (Shanghai, China). The extraction process applied for CMCS and the determination and quantitation of active compounds in CMCS by HPLC have been described previously21.
Animals
Male C57BL/6 mice (8 weeks of age) were obtained from the Experimental Animal Center, Chinese Academy of Science (Shanghai, China). Our experiments conformed to the ethical guidelines outlined in the Guide for the Care and Use of Laboratory Animals by the Laboratory Animal Center at Shanghai University of Traditional Chinese Medicine.
Hepatic fibrosis induced by CCl4
To induce liver fibrosis, the mice were injected intraperitoneally (ip) with 10% CCl4/2 mL olive oil/kg body weight three times a week for 4 weeks12. After all mice were sacrificed, serum and liver samples were harvested. For histological analysis, tissue specimens were fixed in buffered formalin and embedded in paraffin wax. For immunofluorescence analysis, liver specimens were embedded in OCT compound. Serum and liver samples were kept frozen at −70 °C until analysis.
Experimental design
Two experimental protocols were performed. First, to evaluate the protective effect of CMCS against liver fibrosis, the mice were randomly divided into 4 groups (10 mice per group): normal control, CMCS control, model control and CMCS treatment. Second, to investigate the anti-fibrotic effect of CMCS in the absence of NK cells, the mice were randomly divided into 4 groups (10 mice per group): isotype+vehicle, isotype+CMCS, ASGM-1+vehicle and ASGM-1+CMCS. In the CMCS control, CMCS treatment, isotype+CMCS and ASGM-1+CMCS groups, the mice were treated orally with CMCS at a daily dose of 120 mg/kg of body weight21, which was equivalent to the dosage of a 60 kg adult. In the normal control, model control, isotype+vehicle and ASGM-1+vehicle groups, the mice received deionized water.
Depletion of NK cells by ASGM-1 antibody
To chronically deplete NK cells (NK1.1+CD3−) in vivo, the fibrotic mice were injected ip with 20 μL an anti-asialo GM-1 (ASGM-1) antibody (WAKO Pure Chemical Industries, Osaka, Japan) 8 h prior to treatment with CMCS. Because NK cell activity has been reported to be markedly reduced on day 3 after one injection, begins to recover on day 7 and rises to more than 50% of the original value on d 1423, in the present study, the ASGM-1 injection was performed on days 0, 3, 7, 14 and 21. Simultaneously, the same lot of rabbit IgG (WAKO Pure Chemical Industries) was used as an isotype control for the ip injection. No mortality was observed in the mice that were treated with the isotype control or ASGM-1+CMCS, while three mice in the ASGM-1+vehicle group died on day 24.
Measurement of serum indicators of liver function and hydroxyproline (Hyp) content
The activities of serum ALT, aspartate aminotransferase (AST), total bilirubin (T.Bil) and albumin (Alb) were quantitated using commercial kits according to the instructions provided by the manufacturer (Nanjing JianCheng Bioengineering Institute, Nanjing, China), including the use of standardization. Hyp levels in tissues were measured using the method described by Jamall et al24.
Histopathological assessment of liver injury
After routine processing, 4-μm-thick liver sections were stained with hematoxylin and eosin (H&E) for histological analysis or Sirius red staining for collagen deposition. The images were analyzed using a light microscope (Olympus BX40, Japan).
Quantitation of fibrosis
Quantitation of fibrosis was performed as described previously25. Briefly, the relative area of the area of fibrosis was expressed as a % of the total liver area, which was analyzed based on 35 visual fields of 7 Sirius red-stained liver sections per mouse. Each field was observed at 10× magnification using a light microscope (Olympus BX40), and then Alliance software was used for the data analysis. To evaluate the relative area of fibrosis, the measured collagen area was divided by the net field area and then multiplied by 100. Subtraction of the vascular luminal area from the total field area yielded the final calculation of the net fibrosis area.
Simultaneous staining of liver tissue with desmin antibody and terminal deoxynucleotidyl transferase-mediated deoxyuridine triphosphate nick-end labeling (TUNEL)
Fresh liver tissues were embedded in OCT compound (SAKURA, CA, USA) and stored at −70 °C. The frozen tissue block was sectioned using a cryotome (Leica CM1850, Germany). Ten-micrometer-thick cryostat sections were cut, transferred to poly-L-lysine-coated slides and fixed in 4% formaldehyde (Dingguo, Shanghai, China). To identify HSCs, the sections were stained with a rabbit anti-desmin antibody (Abcam, CA, USA) as the primary antibody and then incubated with FITC-conjugated Affinipure Donkey Anti-Rabbit IgG (H+L) (Proteintech, USA) secondary antibody. Apoptosis was detected using a one-step TUNEL kit (Beyotime, Haimen, China) according to the manufacturer's protocol. The tissues were finally stained with 4′,6-diamidino-2-phenylindole (DAPI) to visualize the nuclei. Images were obtained using a confocal microscope (Fluoview FV10i, Olympus, Japan) equipped with the ultraviolet/visible light LD laser combination. Photographs were obtained with Olympus confocal software.
Isolation of liver mononuclear cells
Mouse livers were removed and pressed through 200-gauge stainless steel mesh. The liver cell suspension was collected and suspended in 0.2% BSA-PBS, a solution containing phosphate-buffered saline (PBS) and 0.2% bovine serum albumin (BSA). The parenchymal cells (pellet) were separated from the mononuclear cells (MNCs) (supernatant) by centrifugation at 650 r/min for 1 min. The supernatant containing MNCs was collected, transferred into a new tube, washed twice in 0.2% BSA-PBS and centrifuged at 1500 r/min for 5 min. The supernatant was aspirated completely, and the cell pellet was resuspended in 40% Percoll (GE Healthcare, Sweden). The Percoll (70%) was gently added from the bottom of the cell suspension and centrifuged for 20 min at 2000 r/min. The cells from the layer between the 40%–70% gradient interface were collected, washed twice in 0.2% BSA-PBS and resuspended in 0.2% BSA-PBS to count the cell numbers using the Trypan blue stain (Gibco, USA).
Flow cytometric analysis
Liver MNCs were adjusted to a concentration of 2×107 cells/mL in 0.2% BSA-PBS. A volume of 50 μL cell suspension was incubated with an anti-mouse CD16/CD32 antibody (eBioscience, San Diego, CA, USA) to block the FcR on ice for 15 min and washed with 0.2% BSA-PBS. The proportions of NK1.1+CD3− and NK1.1+CD3−NKG2D+ cells were determined using anti-NKG2D, anti-NK1.1 and anti-CD3 antibodies (BD PharMingen, San Diego, CA, USA). Flow cytometric analysis was performed using a FACSArray bioanalyzer (BD Bioscience, CA, USA).
Tissue RNA extraction, reverse transcription and real-time fluorescence quantitative PCR (RT-qPCR)
Total RNA was extracted from the frozen liver tissue using TRIzol reagent (Sangon Biotech, Shanghai, China). RNA was then used as a template for reverse transcription into single-stranded cDNA with random primers and reagents supplied in the Reverse Transcription Reagent Kit with gDNA Eraser, according to the manufacturer's protocol (TaKaRa, Dalian, China). The synthesized β-actin gene was amplified as an internal control, and the other primers used are listed in Table 1. RT-qPCR was performed using SYBR® Premix Ex Taq™ (Tli RNaseH Plus) (TaKaRa) and ViiA™ 7 Real-Time PCR System (ABI, Carlsbad, CA, USA).
Table 1. Real-time quantitative PCR primers used in this study.
| Gene | Forward (5′→3′) | Reverse (5′→3′) |
|---|---|---|
| α-SMA | ACTACTGCCGAGCGTGAGATTG | CGTCAGGCAGTTCGTAGCTCTT |
| TGF-β1 | AATTCCTGGCGTTACCTTGGT | GAAGGGTCGGTTCATGTCATG |
| RAE-1δ | GCTGCAGTTCAAGCAACCAA | CCACGAAGCACTTCACTTCA |
| RAE-1ε | GCTGCAGTTCAAGACACCAA | TCCACTGAGCACTTCACGTC |
| β-actin | TGACGAGGCCCAGAGCAAGA | ATGGGCACAGTGTGGGTGAC |
Statistical analysis
All data were analyzed using PASW Statistics 18 software. Differences between groups were assessed by nonparametric one-way analysis of variance (ANOVA) followed by the least significant difference (LSD) post hoc test. Values in the text are means±standard deviation (SD). P<0.05 was considered statistically significant.
Results
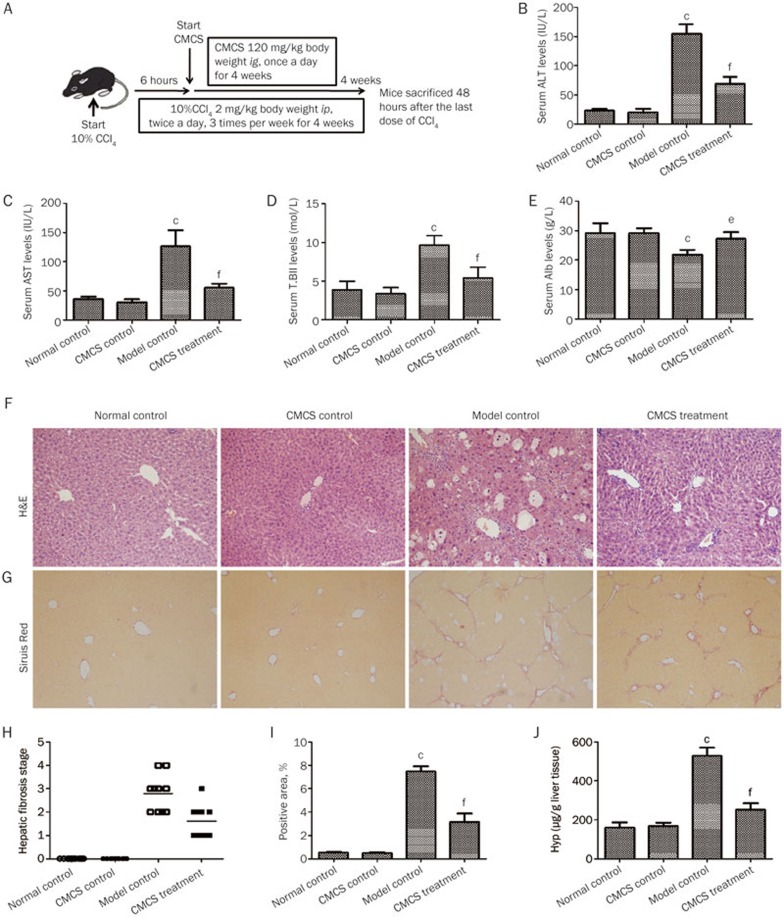
CMCS alleviates CCl4-induced liver fibrosis in mice
The effect of CMCS on liver fibrosis was observed (Figure 1A). As shown in Figure 1B, C, D & E, serum liver functions were significantly improved in CMCS-treated mice in comparison to the model control (P<0.01). Fewer vacuolated cells and less mononuclear cell infiltration were observed in the portal area, and hepatocellular degeneration was significantly decreased after CMCS treatment (Figure 1F). Furthermore, in the model control, the hepatic parenchyma was expanded by collagen fibers, and lobules were separated by fibrous septa surrounding the hepatocytes. Liver fibrosis was efficiently alleviated after CMCS treatment (Figure 1G). Both the extent of hepatic fibrosis and the ratio of the positive area of collagen deposition were significantly reduced in CMCS-treated mice compared with the model control (Figure 1H, I). In addition, hepatic Hyp content was decreased in response to CMCS treatment in the model mice (Figure 1J).
Figure 1.
Effects of CMCS on CCl4-induced liver fibrosis in mice. (A) Male mice were ip injected with 10% CCl4, 3 times per week for 4 weeks, starting at 6 weeks of age. Six hours after the first CCl4 injection, once-daily treatment with CMCS extract or control vehicle was begun. Four weeks later, mice were sacrificed 48 h after the last CCl4 injection. (B, C, D & E) Serum levels of indicators of liver function including ALT, AST, T.Bil and Alb were assayed using commercial kits. (F) H&E stained liver tissues (magnification, 200×). (G) Liver tissue sections were stained with Sirius red as described in Materials and Methods. Representative tissue sections are shown, with fibrotic septa, which were more established in the model control group than that in the CMCS treatment group (magnification, 100×). (H) Hepatic fibrosis stages of mice were analyzed according to the Knodell histological activity index. Fibrosis stages were determined by Ridit analysis. (I) Semi-quantification data for relative fibrosis levels were expressed as the % of total liver area, and the mean±SD was assessed by analyzing five fields of Sirius red stained liver sections per animal. Each field was acquired at 100× magnification, and data were acquired using Image-Pro Plus software. (J) Hyp content was quantified from 100 mg liver samples and measured by the method described by Jamall et al. Values represent mean±SD (n=10). bP<0.05, cP<0.01, versus normal control group; eP<0.05, fP<0.01, versus model control group.
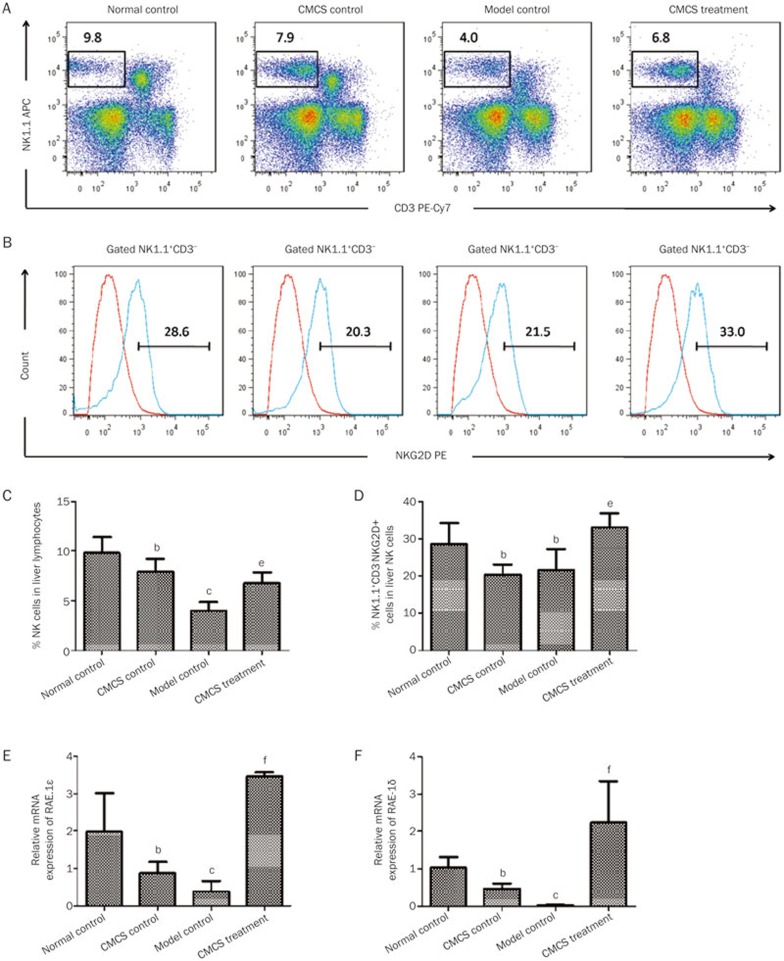
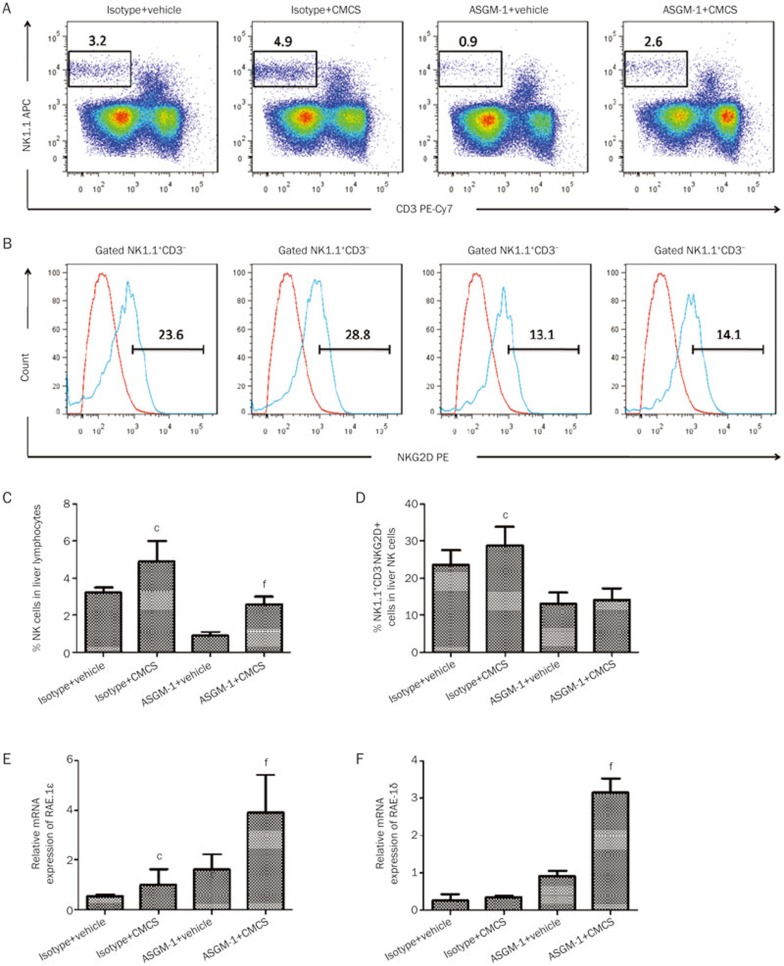
CMCS promotes hepatic NK cell activation in CCl4-induced liver fibrosis in mice
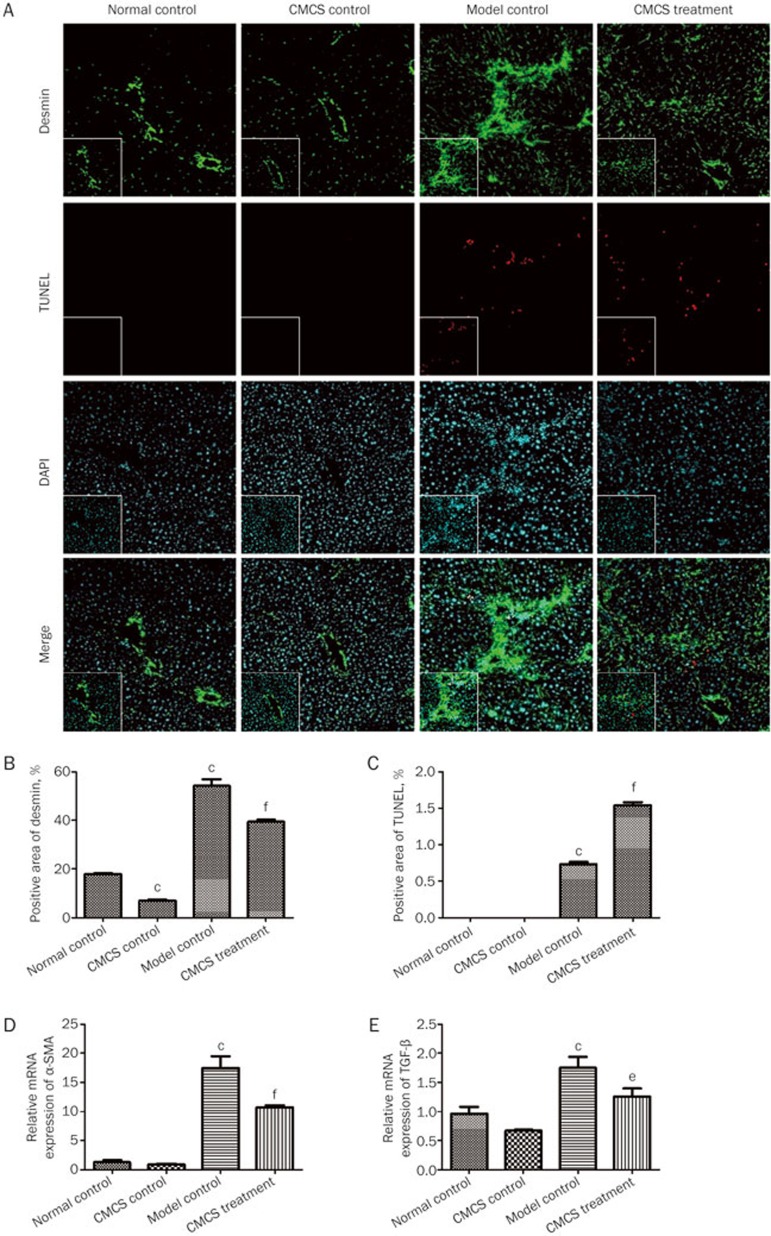
Next, we examined the effects of CMCS on the activities of liver NK cells in CCl4-induced liver fibrosis. As shown in Figure 2A and C, the frequency of liver NK cells (NK1.1+CD3−) was significantly decreased after CCl4 treatment, whereas the frequency of liver NK cells in the CMCS treatment group was significantly elevated. The expression of NKG2D, which is a C-type lectin-like activation receptor on the surface of NK cells, was also assayed. With the decreasing trend in the frequency of liver NK cells after CCl4 injection, the expression of NKG2D was diminished accordingly in the model control group while they were up-regulated in the CMCS treatment group (Figure 2B, D), suggesting that CMCS treatment could strengthen the activity of hepatic NK cells in CCl4-induced liver fibrosis. Because NK cells have been shown to exert anti-fibrotic activity on activated HSCs by the upregulation of the NKG2D ligand RAE-112, we assumed that CMCS could promote NK cell activity by elevating the levels of RAE-1 on HSCs. To test this hypothesis, the expression levels of RAE-1ε and RAE-1δ mRNA were assessed. As expected, both RAE-1ε and RAE-1δ, which are ligands of NKG2D on the surface of HSCs, were upregulated in response to CMCS treatment, whereas they declined sharply in the model control group (Figure 2E, F). Subsequently, lower expression levels of desmin and greater numbers of TUNEL-positive cells were found in the CMCS treatment group compared with the model control group (Figure 3A–C). The mRNA expression levels of α-SMA and TGF-β were significantly decreased in CMCS-treated mice (Figure 3D, E). These results revealed that CMCS could ameliorate CCl4-induced liver fibrosis by promoting the activation of hepatic NK cells against HSCs in mice.
Figure 2.
CMCS treatment promotes activation of hepatic NK cells in mice with CCl4-induced liver fibrosis. (A) Liver lymphocytes were analyzed by FACS with APC-conjugated rat anti-mouse NK1.1 antibody and PE-Cy7-conjugated rat anti-mouse monoclonal antibody. (B) For NKG2D identification, a PE-conjugated rat anti-mouse NKG2D antibody was used. The expression of NKG2D from A was analyzed by FACS. (C) Numbers of NK1.1+CD3− cells in liver lymphocytes were counted. (D) Expression of NKG2D in NK1.1+CD3− cells was quantified. (E & F) mRNA levels of RAE-1δ and RAE-1ε in liver samples were analyzed by RT-qPCR. Values represent mean±SD (n=10). bP<0.05, cP<0.01, versus normal control group; eP<0.05, fP<0.01, versus model control group.
Figure 3.
CMCS treatment restrains HSCs activation in mice with CCl4-induced liver fibrosis. (A) Liver sections were subjected either to immunohistochemical staining for desmin (green) for detection of HSCs, the TUNEL assay to detect cell apoptosis (red) or blue-fluorescent DAPI nucleic acid staining (magnification, 200×). Desmin-positive (B) and TUNEL-positive (C) areas were quantified. (D and E) Relative mRNA expression levels of α-SMA (D) and TGF-β (E) were assayed by RT-qPCR. Values represent mean±SD (n=10). bP<0.05, cP<0.01 versus normal control group; eP<0.05, fP<0.01 versus model control group.
CMCS inhibits the depletion of hepatic NK cells in CCl4-induced liver fibrosis in mice
ASGM-1 is a rabbit polyclonal antibody that reacts with a neutral glycosphingolipid that is expressed on the surface of numerous hematopoietic cells, including NK, NKT, CD8+T, γδT, and some CD4+T cells, macrophages, eosinophils and basophils26,27,28,29,30. Nevertheless, ASGM-1 only effectively eliminates NK cells and basophils in vivo27,31. Other methods, such as the application of anti-NK1.1 and anti-CD122 antibodies, are not ideal for the depletion of NK cells. The NK1.1 antibody is expressed on both NK cells (NK1.1+CD3−) and NKT cells (NK1.1+CD3+). Therefore, anti-NK1.1 also depletes NKT cells. CD122 is expressed on CD8+T lymphocytes, NK cells, NKT cells, dendritic epidermal T cells, subsets of intraepithelial lymphocytes, and macrophages. Thus, the anti-CD122 antibody might deplete NK cells and other lymphocytes simultaneously. Furthermore, genetically modified mice with NK cell deficiencies, such as Beige and Stat5(f/f) Ncr1-iCreTg mice, are available. Unfortunately, neither of these models is ideal for assessing the role of NK cells. While Beige mice completely lack NK cells, they are also deficient in cytotoxic T cells and have impaired neutrophil activity. In contrast, while NK cell depletion in Stat5(f/f) Ncr1-iCreTg mice is selective, it is not complete, demonstrating residual NK cell numbers that are comparable to WT mice treated with ASGM-132,33. Therefore, ASGM-1 is one of the most precise tools available to specifically eliminate NK cells in vivo.
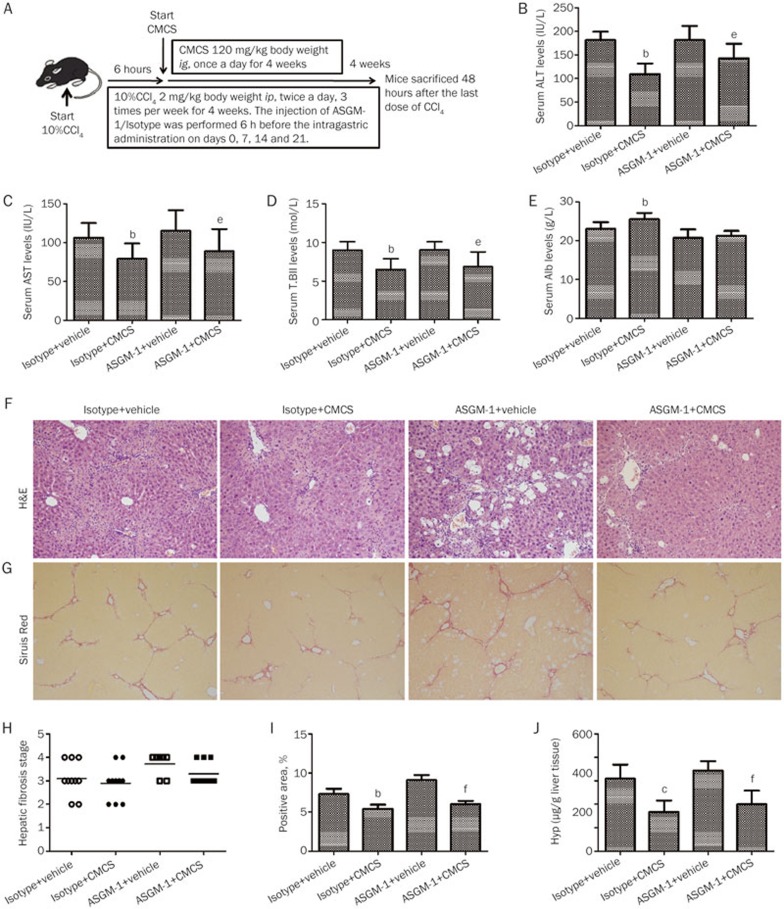
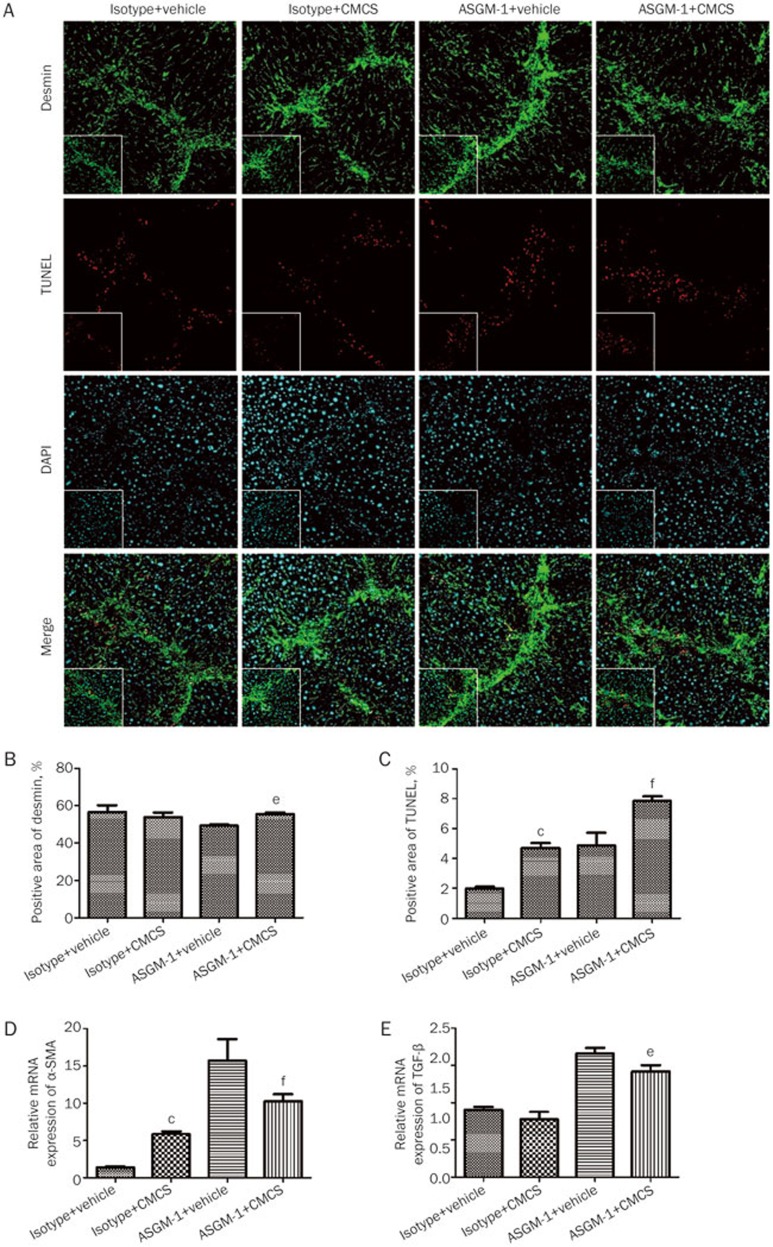
In the present study, we used an anti-ASGM-1 antibody to deplete NK cells to investigate the effects of CMCS on liver fibrosis under the condition of NK cell depletion (Figure 4A). As expected, the depletion of NK cells led to severe serum liver function and aggravated fibrosis progressioin in ASGM-1+vehicle group (Figure 4F-I), though serum liver function and Hyp remained no significance with Isotype+vehicle group (Figure 4B-E). After CMCS treatment, liver inflammation was relieved, and collagen deposition in the liver tissue decreased (Figure 4F, G). Similarly, the hepatic Hyp content was reduced in response to CMCS treatment in the model mice (Figure 4J). Simultaneously, the frequency of hepatic NK cells was significantly increased despite NK depletion by injection of the anti-ASGM-1 antibody (Figure 5A, C). The expression of NKG2D on NK cells remained nearly equivalent to that in the vehicle group after CMCS treatment (Figure 5B, D). The mRNA expression levels of RAE-1ε and RAE-1δ were elevated after CMCS treatment compared with the vehicle group (Figure 5E, F). Furthermore, greater TUNEL staining was observed around areas with reduced desmin expression after CMCS treatment (Figure 6A–C). The mRNA expression of α-SMA and TGF-β also decreased in CMCS-treated mice (Figure 6D, E). Therefore, our results indicated that liver fibrosis could be improved and NK depletion could be partly inhibited by CMCS treatment.
Figure 4.
Depletion of hepatic NK cells by ASGM-1 accelerates CCl4-induced liver fibrosis, which is attenuated by CMCS treatment in the absence of NK cells. (A) All mice were ip injected with 10% CCl4, 3 times per week, starting at 6 weeks of age. Six hours after the first CCl4 injection, daily treatment with CMCS was begun. Injection of NK cell-depleting Abs (anti-asialo GM1, ASGM1) or isotype control was performed 6 h before the intragastric administration on days 0, 7, 14 and 21. Four weeks later, mice were sacrificed 48 h after the last CCl4 injection. (B, C, D & E) Serum levels of liver function indicators including ALT, AST, T.Bil and Alb were assayed using commercial kits. (F) H&E staining of liver tissues (magnification, 200×). (G) Liver tissue sections were stained with srius red as described in Materials and Methods (magnification, 100×). (H) Hepatic fibrosis stages of mice were analyzed according to the Knodell histological activity index. Ranked data for fibrosis stages were determined by Ridit analysis. (I) Semi-quantification data for relative fibrosis levels were expressed as a % of total liver area, and the mean±SD was assessed by analyzing five fields of sirius red stained liver sections per animal. Each field was acquired at 100 × magnification and then calculated with Image-Pro Plus software. (J) Hyp content was quantified from 100 mg of each liver sample and measured using the method by Jamall et al. Values represent mean±SD (n=10). bP<0.05, cP<0.01 versus normal control group; eP<0.05, fP<0.01 versus model control group.
Figure 5.
CMCS treatment inhibits the depletion of hepatic NK cells in mice with CCl4-induced liver fibrosis. Animals underwent the same experimental protocol as presented in Figure. 4. (A) Liver lymphocytes were analyzed by FACS with an APC-conjugated rat anti-mouse NK1.1 antibody and PE-Cy7-conjugated rat anti-mouse monoclonal antibody. (B) For NKG2D identification, a PE-conjugated rat anti-mouse NKG2D antibody was used. The expression of NKG2D from A was analyzed by FACS. (C) Numbers of NK1.1+CD3− cells in liver lymphocytes were counted. (D) Expression of NKG2D in NK1.1+CD3− cells was quantified. (E & F) mRNA levels of RAE-1δ and RAE-1ε in liver samples were analyzed by RT-qPCR. Values represent means±SD (n=10). bP<0.05, cP<0.01 versus isotype+vehicle group; eP<0.05, fP<0.01 versus ASGM-1 + vehicle group.
Figure 6.
CMCS treatment restrains HSC activation in the absence of NK cells. (A) Liver sections were subjected either to immunohistochemical staining for desmin (green) for detection of HSCs, the TUNEL assay to detect cell apoptosis (red) or blue-fluorescent DAPI nucleic acid staining (magnification, 200×). Desmin expression (green) was observed around the collagen deposits, and fewer apoptotic cells (red) were adjacent to the desmin (green) in the ASGM-1 + vehicle group compared with those in the ASGM-1 + CMCS group. Desmin-positive (B) and TUNEL-positive (C) areas were quantified. (D&E) Relative mRNA expression of α-SMA (D) and TGF-β (E) were assayed by RT-qPCR. Values represent mean±SD (n=10). bP<0.05, cP<0.01 versus isotype+vehicle group; eP<0.05, fP<0.01 versus ASGM-1 + vehicle group.
Discussion
Chronic hepatic diseases, such as liver cirrhosis, hepatocellular carcinoma, viral hepatitis and autoimmune liver diseases, affect billions of people worldwide. These diseases are commonly associated with liver fibrosis initially. The liver, as the principal detoxifying organ in the human body, removes various pathogens, toxic chemicals and antigens from the blood, as well as metabolic waste from the circulatory system. When the liver is exposed to different types of injury, the pathological by-products lead to apoptosis or necrosis of hepatocytes. In these pathophysiological conditions, hepatic resident immune cells are recruited and infiltrate the affected areas of the organ. However, when the balance shifts toward injury, chronic inflammation of the liver occurs, which can aggravate the liver fibrosis.
As the largest immune organ in the body, the liver is enriched with different types of immunocytes, including T lymphocytes, B lymphocytes, Kupffer cells, NK cells and natural killer T cells. Among these immune cells, the liver lymphocyte population consists of large numbers of NK cells, which play a crucial role in host defense against viral infection and tumor transformation. Additionally, the functions of NK cells have garnered much attention because they have been found to be markedly altered in various liver diseases, especially in the inhibition of liver fibrosis by killing early activated HSCs34.
Although various anti-fibrotic drugs, therapies and advanced diagnostic equipment are currently used, there remain side effects associated with anti-fibrotic treatment and challenges related to the diagnosis of asymptomatic patients. The development of a suitable medication remains a major barrier. Chinese herbal medicines have been widely used in China from the earliest times to the present day, and their medicinal value is strongly supported by clinical applications35. One of these herbal medicines, CMCS, is generally known for its tonic properties. It is widely used to treat conditions such as chronic liver diseases, lupus nephritis and autoimmune thyroid disease in the clinic. In our previous study, CMCS displayed beneficial effects in attenuating liver injury21. However, little is known about the immunological mechanism by which CMCS protects against hepatic fibrosis. Therefore, the aim of the present study was to investigate the effects of CMCS on the functions of liver NK cells during liver fibrosis.
First, we found that CMCS treatment significantly alleviated CCl4-induced high serum aminotransferase levels and reduced liver inflammation and fibrosis by suppressing the expression of α-SMA and TGF-β in liver tissue. Remarkably, the function of NK cells has been shown to be weakened in patients with chronic liver disease, including primary biliary cirrhosis and hepatitis C virus36. Collectively, our results provide novel insight regarding the mechanism by which CMCS impacts liver fibrosis. In addition, effective CMCS therapy in CCl4-induced liver fibrosis correlated with increased hepatic NK cell activity. The results also demonstrated that the anti-fibrotic effects of CMCS were manifested through the elevated frequency of hepatic NK cells because NKG2D, the activation receptor of NK cells, appeared to be upregulated in response to CMCS treatment.
Because hepatic NK cells were drastically reduced in the liver fibrosis model and could be significantly increased by CMCS treatment, we questioned whether CMCS could affect the depletion of NK cells during liver fibrosis. Moreover, we wondered whether the depletion of NK cells would lead to a diminished anti-fibrotic therapeutic effect of CMCS. To decipher the contribution of CMCS to the activation of liver NK cells, we opted to systemically deplete NK cells over the course of liver fibrosis development using the ASGM-1 antibody, which was injected at different times during the CCl4-induced liver fibrotic phase.
Simultaneously, CMCS was administered orally with the daily dosage. Liver inflammation and fibrosis were aggravated, and the frequency of hepatic NK cells was greatly decreased in response to the ASGM-1 antibody in the model mice. By contrast, after continuous administration of CMCS for 4 weeks, the rate of liver fibrosis development decelerated, and the frequency of hepatic NK cells was mildly upregulated. Although NKG2D was not augmented, the number of NK cells increased significantly following CMCS treatment. This result implied that CMCS could protect the impaired NK cells, and the ASGM-1-induced depletion of NK cells in the fibrosis model could be competitively restrained by raising the frequency of hepatic NK cells. Furthermore, when NK cells were depleted, HSCs were still inhibited because the expression levels of α-SMA and TGF-β were decreased by CMCS in a manner similar to those in the ASGM-1 vehicle group. The activation of HSCs is a key step in the development of liver fibrosis. Desmin, an intermediate filament that is typical of contractile cells, has been widely used as the “gold standard” to identify all stages of HSCs in rodent livers37. In the present study, we discovered a greater number of TUNEL-positive cells adjacent to the desmin-stained cells in the ASGM-1 plus CMCS group compared with the ASGM-1 vehicle group, suggesting that CMCS treatment induced the apoptosis of activated HSCs. Taken together, these results demonstrated that CMCS was also effective in relieving CCl4-induced liver fibrosis and promoting NK cell activation in the background of ASGM-1-induced NK cell depletion.
Conclusion
CMCS was effective for alleviating liver fibrosis induced by CCl4 by promoting the activity of hepatic NK cells. Furthermore, CMCS could improve liver fibrosis by partially inhibiting the inactivation of NK cells by ASGM-1.
Author contribution
Yuan PENG performed the research and wrote the manuscript; Kai HUANG assisted with the animal experiments; Li SHEN analyzed the data; Yan-yan TAO designed the research and revised the manuscript; Cheng-hai LIU critically revised the manuscript.
Abbreviations
hepatic stellate cells (HSCs); natural killer (NK) cells; cultured mycelium Cordyceps sinensis (CMCS); α-smooth muscle actin (α-SMA); anti-asialo GM-1 antibody (ASGM-1); transforming growth factor-beta (TGF-β); carbon tetrachloride (CCl4); alanine aminotransferase (ALT); aspartate aminotransferase (AST); total bilirubin (T.Bil); albumin (Alb); hydroxyproline (Hyp); hematoxylin and eosin (H&E); terminal deoxynucleotidyl transferase-mediated deoxyuridine triphosphate nick-end labeling (TUNEL); 4′,6-diamidino-2-phenylindole (DAPI); phosphate-buffered saline (PBS); bovine serum albumin (BSA); mononuclear cells (MNCs); nonparametric One-way analysis of variance (ANOVA); least significant difference (LSD); standard deviation (SD); real-time fluorescence quantitative PCR (RT-qPCR).
Acknowledgments
This work was supported by grants from the National Natural Science Foundation of China (No 81173405, 81102701 and 81503322), the National Science and Technology Major Project (2014ZX10005001), the International S&T Cooperation Program of China (2014DFA31440), the Program for Outstanding Medical Academic Leader of Shanghai Municipality (LJ10005), the E-Institute (E03008), “Three-year action plan” for Development of TCM in Shanghai (ZY3-CCCX-2-1003) and China Postdoctoral Science Foundation (No 2015M571595).
References
- 1Elsharkawy AM, Oakley F, Mann DA. The role and regulation of hepatic stellate cell apoptosis in reversal of liver fibrosis. Apoptosis 2005; 10: 927–39. [DOI] [PubMed] [Google Scholar]
- 2Pinzani M, Macias-Barragan J. Update on the pathophysiology of liver fibrosis. Expert Rev Gastroenterol Hepatol 2010; 4: 459–72. [DOI] [PubMed] [Google Scholar]
- 3Issa R, Zhou X, Constandinou CM, Fallowfield J, Millward-Sadler H, Gaca MD, et al. Spontaneous recovery from micronodular cirrhosis: evidence for incomplete resolution associated with matrix cross-linking. Gastroenterology 2004; 126: 1795–808. [DOI] [PubMed] [Google Scholar]
- 4Farag SS, Caligiuri MA. Human natural killer cell development and biology. Blood Rev 2006; 20: 123–37. [DOI] [PubMed] [Google Scholar]
- 5Tian Z, Chen Y, Gao B. Natural killer cells in liver disease. Hepatology 2013; 57: 1654–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6Lanier LL. NK cell recognition. Annu Rev Immunol 2005; 23: 225–74. [DOI] [PubMed] [Google Scholar]
- 7Raulet DH. Roles of the NKG2D immunoreceptor and its ligands. Nat Rev Immunol 2003; 3: 781–90. [DOI] [PubMed] [Google Scholar]
- 8Ortaldo JR, Young HA. Mouse Ly49 NK receptors: balancing activation and inhibition. Mol Immunol 2005; 42: 445–50. [DOI] [PubMed] [Google Scholar]
- 9Ishiyama K, Ohdan H, Ohira M, Mitsuta H, Arihiro K, Asahara T. Difference in cytotoxicity against hepatocellular carcinoma between liver and periphery natural killer cells in humans. Hepatology 2006; 43: 362–72. [DOI] [PubMed] [Google Scholar]
- 10Gur C, Doron S, Kfir-Erenfeld S, Horwitz E, Abu-Tair L, Safadi R, et al. NKp46-mediated killing of human and mouse hepatic stellate cells attenuates liver fibrosis. Gut 2012; 61: 885–93. [DOI] [PubMed] [Google Scholar]
- 11Melhem A, Muhanna N, Bishara A, Alvarez CE, Ilan Y, Bishara T, et al. Anti-fibrotic activity of NK cells in experimental liver injury through killing of activated HSC. J Hepatol 2006; 45: 60–71. [DOI] [PubMed] [Google Scholar]
- 12Radaeva S, Sun R, Jaruga B, Nguyen VT, Tian Z, Gao B. Natural killer cells ameliorate liver fibrosis by killing activated stellate cells in NKG2D-dependent and tumor necrosis factor-related apoptosis-inducing ligand-dependent manners. Gastroenterology 2006; 130: 435–52. [DOI] [PubMed] [Google Scholar]
- 13Jeong WI, Park O, Radaeva S, Gao B. STAT1 inhibits liver fibrosis in mice by inhibiting stellate cell proliferation and stimulating NK cell cytotoxicity. Hepatology 2006; 44: 1441–51. [DOI] [PubMed] [Google Scholar]
- 14Yoshida K, Ohishi W, Nakashima E, Fujiwara S, Akahoshi M, Kasagi F, et al. Lymphocyte subset characterization associated with persistent hepatitis C virus infection and subsequent progression of liver fibrosis. Hum Immunol 2011; 72: 821–6. [DOI] [PubMed] [Google Scholar]
- 15Gao B, Radaeva S. Natural killer and natural killer T cells in liver fibrosis. Biochim Biophys Acta 2013; 1832: 1061–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16Jeong WI, Park O, Suh YG, Byun JS, Park SY, Choi E, et al. Suppression of innate immunity (natural killer cell/interferon-gamma) in the advanced stages of liver fibrosis in mice. Hepatology 2011; 53: 1342–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17Won SY, Park EH. Anti-inflammatory and related pharmacological activities of cultured mycelia and fruiting bodies of Cordyceps militaris. J Ethnopharmacol 2005; 96: 555–61. [DOI] [PubMed] [Google Scholar]
- 18Lee HH, Park H, Sung GH, Lee K, Lee T, Lee I, et al. Anti-influenza effect of Cordyceps militaris through immunomodulation in a DBA/2 mouse model. J Microbiol 2014; 52: 696–701. [DOI] [PubMed] [Google Scholar]
- 19Yoon TJ, Yu KW, Shin KS, Suh HJ. Innate immune stimulation of exo-polymers prepared from Cordyceps sinensis by submerged culture. Appl Microbiol Biotechnol 2008; 80: 1087–93. [DOI] [PubMed] [Google Scholar]
- 20Liu C, Lu S, Ji MR. Effects of Cordyceps sinensis (CS) on in vitro natural killer cells. Zhongguo Zhong Xi Yi Jie He Za Zhi 1992; 12: 267–9, 59. Chinese. [PubMed] [Google Scholar]
- 21Peng Y, Chen Q, Yang T, Tao Y, Lu X, Liu C. Cultured mycelium Cordyceps sinensis protects liver sinusoidal endothelial cells in acute liver injured mice. Mol Biol Rep 2014; 41: 1815–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22Peng Y, Tao Y, Wang Q, Shen L, Yang T, Liu Z, et al. Ergosterol Is the Active Compound of Cultured Mycelium Cordyceps sinensis on Antiliver Fibrosis. Evid Based Complement Alternat Med 2014; 2014: 537234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23Habu S, Fukui H, Shimamura K, Kasai M, Nagai Y, Okumura K, et al. In vivo effects of anti-asialo GM1. I. Reduction of NK activity and enhancement of transplanted tumor growth in nude mice. J Immunol 1981; 127: 34–8. [PubMed] [Google Scholar]
- 24Jamall IS, Finelli VN, Que Hee SS. A simple method to determine nanogram levels of 4-hydroxyproline in biological tissues. Anal Biochem 1981; 112: 70–5. [DOI] [PubMed] [Google Scholar]
- 25Safadi R, Ohta M, Alvarez CE, Fiel MI, Bansal M, Mehal WZ, et al. Immune stimulation of hepatic fibrogenesis by CD8 cells and attenuation by transgenic interleukin-10 from hepatocytes. Gastroenterology 2004; 127: 870–82. [DOI] [PubMed] [Google Scholar]
- 26Kataoka S, Konishi Y, Nishio Y, Fujikawa-Adachi K, Tominaga A. Antitumor activity of eosinophils activated by IL-5 and eotaxin against hepatocellular carcinoma. DNA Cell Biol 2004; 23: 549–60. [DOI] [PubMed] [Google Scholar]
- 27Nishikado H, Mukai K, Kawano Y, Minegishi Y, Karasuyama H. NK cell-depleting anti-asialo GM1 antibody exhibits a lethal off-target effect on basophils in vivo. J Immunol 2011; 186: 5766–71. [DOI] [PubMed] [Google Scholar]
- 28Slifka MK, Pagarigan RR, Whitton JL. NK markers are expressed on a high percentage of virus-specific CD8+ and CD4+ T cells. J Immunol 2000; 164: 2009–15. [DOI] [PubMed] [Google Scholar]
- 29Trambley J, Bingaman AW, Lin A, Elwood ET, Waitze SY, Ha J, et al. Asialo GM1(+) CD8(+) T cells play a critical role in costimulation blockade-resistant allograft rejection. J Clin Invest 1999; 104: 1715–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30Wiltrout RH, Santoni A, Peterson ES, Knott DC, Overton WR, Herberman RB, et al. Reactivity of anti-asialo GM1 serum with tumoricidal and non-tumoricidal mouse macrophages. J Leukoc Biol 1985; 37: 597–614. [DOI] [PubMed] [Google Scholar]
- 31Kasai M, Iwamori M, Nagai Y, Okumura K, Tada T. A glycolipid on the surface of mouse natural killer cells. Eur J Immunol 1980; 10: 175–80. [DOI] [PubMed] [Google Scholar]
- 32Eckelhart E, Warsch W, Zebedin E, Simma O, Stoiber D, Kolbe T, et al. A novel Ncr1-Cre mouse reveals the essential role of STAT5 for NK-cell survival and development. Blood 2011; 117: 1565–73. [DOI] [PubMed] [Google Scholar]
- 33Jessen B, Maul-Pavicic A, Ufheil H, Vraetz T, Enders A, Lehmberg K, et al. Subtle differences in CTL cytotoxicity determine susceptibility to hemophagocytic lymphohistiocytosis in mice and humans with Chediak-Higashi syndrome. Blood 2011; 118: 4620–9. [DOI] [PubMed] [Google Scholar]
- 34Gao B, Radaeva S, Park O. Liver natural killer and natural killer T cells: immunobiology and emerging roles in liver diseases. J Leukoc Biol 2009; 86: 513–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35Fowell AJ, Iredale JP. Emerging therapies for liver fibrosis. Dig Dis 2006; 24: 174–83. [DOI] [PubMed] [Google Scholar]
- 36Matheson DS, Green BJ, Minuk GY. Natural killer-cell activity and the response to interferons alpha, beta, and gamma in patients with primary biliary cirrhosis. J Allergy Clin Immunol 1989; 84: 214–8. [DOI] [PubMed] [Google Scholar]
- 37Friedman SL. Hepatic stellate cells: protean, multifunctional, and enigmatic cells of the liver. Physiol Rev 2008; 88: 125–72. [DOI] [PMC free article] [PubMed] [Google Scholar]