Abstract
There is currently growing interest in using mobile phones to support the treatment of psychotic disorders, such as schizophrenia. However, the widespread implementation of these interventions will ultimately depend upon patients’ access to mobile devices and their willingness to engage with mobile health (“mHealth”). Thus, we conducted a systematic review and meta-analysis to assess mobile phone ownership and interest in mHealth among patients with psychosis. An electronic search of Ovid MEDLINE, Embase, PsycINFO, CENTRAL, AMED, Health Technology Assessment Database, and Health Management Information Consortium Database was conducted, using search terms synonymous with mobile phones and psychotic disorders. The initial literature search yielded 2572 results. Fifteen studies matched eligibility criteria, reporting data from 12 independent samples of psychiatric patients (n = 3227). Data pertaining to mobile phone ownership, usage, and opinions on mHealth among patients with psychotic disorders were extracted from these studies, and meta-analytic techniques were applied. The overall mobile phone ownership rate was 66.4% (95% CI = 54.1%–77.6%). However, we found strong statistical evidence that mobile phone ownership has been significantly increasing since 2007, and the rate among patients surveyed in the last 2 years was 81.4% (n = 454). Furthermore, in surveys of mHealth acceptability, the majority of patients responded in favor of using mobile phones to enhance contact with services and support self-management. Considering the increasing availability of mobile phones and the broad acceptability of mHealth among patients, there is now a need to develop and evaluate mHealth interventions to enhance healthcare services for people with psychosis.
Key words: schizophrenia, cell phone, smartphone, psychotic disorder, technology, e-health
Introduction
Over recent decades, there has been a growing interest in examining the feasibility and effectiveness of using mobile phones to support medical care (“mHealth”). In addition to traditional phone calls and Short Message Service (SMS) messaging on older models, the widespread availability of wireless internet has paved the way for new forms of portable technology, such as smartphones, which can provide instant internet access across a variety of locations. Additionally, software applications (“apps”) for these devices can be developed to perform a wide variety of functions and are readily available for any device owner.
Mobile and smartphones have broad scoping clinical applications, from promoting attendance at healthcare appointments and medication adherence1,2 to communicating test results3 and monitoring patient symptoms in real time.4,5 There is also a burgeoning literature examining the efficacy of health interventions delivered via mobile phones for a wide range of outcomes, from smoking cessation6 and monitoring and treating mood disorders7 to managing chronic physical health conditions such as asthma and diabetes.8,9
The potential for applying mobile technologies within the assessment and treatment of schizophrenia has been recognized since early studies of hand-held electronic dairies to record symptoms, and text-messaging systems to engage patients with treatment.10 In recent years, mobile phones and smartphones have proven increasingly feasible for improving medication adherence,11 detecting warning signs of relapse,12 monitoring trends in psychiatric symptoms,13 and promoting self-management of mental health.14 This technology can also be used to obtain instantaneous feedback, allowing for early detection of symptoms and relapse, greater patient engagement in healthcare, and more timely responses to changes in functioning.15 However, the extent to which patient engagement with these interventions impacts on clinical outcomes has yet to be established.
As the growth in demand for mental healthcare exceeds the resources available to many national services, budget pressures will require more cost-effective and innovative methods of healthcare delivery.15 A shortage of trained clinicians means that many people who could benefit from evidence-based mental health interventions do not have access to these services.16,17 Policy documents such as “No health without mental health”18 in the United Kingdom recommends the use of information and communication technology to improve service delivery.15 Smartphone technology in particular has the potential to significantly improve mental healthcare, through extending the reach of services and providing adjunctive support to existing psychosocial interventions.
However, the potential benefits of mobile phones for mental healthcare are ultimately dependent upon levels of technology access and engagement among service users. Previous research of “digital divides” across demographic groups indicate that people with schizophrenia would be less likely to possess mobile phones and smartphones than the general population, since unemployment, poor education, and chronic medical conditions are all associated with reduced access to technology.19–21 Furthermore, although the popularity of using mobile phones to monitor and manage health has increased among the general population,22,23 previous research has expressed concerns that certain characteristics of psychotic disorders (such as paranoia, cognitive deficits, and social withdrawal) may present barriers towards wide scale use of mHealth in this population.24,25
In this review, we evaluate current and future possibilities for mHealth in psychotic disorders, through examining the rate of mobile phone adoption among patients. We also quantify patients’ endorsement of various possible mHealth services in order to inform the development of future interventions.
Methods
Search Strategy and Selection Criteria
An electronic database search of Ovid MEDLINE, Embase, PsycINFO, the Cochrane Central Register of Controlled Trials (CENTRAL), Allied and Complementary Medicine Database (AMED), Health Technology Assessment Database, and the Health Management Information Consortium database was conducted on June 23, 2015 using the following keyword search terms: “mhealth” or “information tech*” or “smartphone” or “mobile” or “text messag*” or “sms” AND “psychosis” or “psychotic” or “schiz*” or “psychiat*” or “severe mental” or “serious mental”. The reference lists of retrieved articles were searched. In addition, a basic search of Google Scholar and the Journal of Medical Internet Research (JMIR) was conducted in an effort to identify any additional relevant publications.
Only original, peer-reviewed, and English-language research articles were included in the review. We aimed to include all studies which reported rates of mobile phone ownership among people being treated for a psychotic disorder (schizophrenia/schizoaffective disorder, nonaffective psychotic disorders, or bipolar with psychotic features). Studies which included a broad spectrum of psychiatric disorders were only included if >66% of the sample had a clinically diagnosed psychotic disorder, as specified above. Data from studies in which <66% of the sample had a psychotic disorder were only used if mobile phone ownership specifically among the patients with a psychotic disorder could be accurately determined and extracted. Intervention studies reporting baseline rates of mobile phone ownership among patients with psychosis also eligible for inclusion.
Data Extraction and Analysis
Two reviewers (J.F. and J.C.) screened the articles independently to assess eligibility. Any disagreements were resolved through discussion until agreement was reached. A systematic tool was developed to extract and quantify the following from each study: (1) Study characteristics: sample size, sample demographics, location, data collection period, healthcare setting, and breakdown of clinical diagnoses and (2) Opportunities for mHealth: mobile phone ownership, current usage, surveyed interest in mHealth among patients, and factors associated with mobile phone ownership/usage.
Data from individual studies were pooled using the proportion meta-analysis in StatsDirect 2.7.26 We applied a random-effects model using the DerSimonian-Laird27 method in order to account for between-study variance when determining study weights and the SE of the overall estimate. Between-study variance was assessed with Cochran’s Q and quantified as I 2, which represents the degree of variance caused by between-study heterogeneity rather than chance. We examined the potential degree of publication bias using Egger’s test for small-study bias and visual inspection of funnel-plots of the association between proportion estimate and SE.
Primary analyses of phone ownership, usage, and interest in mHealth services were restricted to patients with psychotic disorders. This included only the studies for which the full sample had a psychotic disorder, or those for which exact rates of mobile phone ownership among subsamples with psychotic disorders could be determined. To examine changes in mobile phone ownership over time, we calculated the midpoint of data collection for each study (ie, the date between the start and end of data collection) and determined how this was related to the number of mobile phone owners, and number of nonowners, found in the study. The statistical software R v. 3.1.2 was used to run a generalized linear model (GLM) with quasibinomial error structure (to allow for overdispersion) and logit link, setting mobile phone ownership as the response and mid-date of data collection as the predictor.
Results
The database search returned 2572 results. This was reduced to 1776 following the removal of duplicates. A further 1711 articles were excluded at the title-abstract stage. Sixty-five-full text articles were retrieved, of which 55 were excluded for containing no relevant data (N = 33), being a review or conference abstract (N = 11), having an ineligible sample (N = 8), or being unavailable in English (N = 3). This left 10 publications which were eligible for inclusion. A further 5 articles were identified from basic searches of Google Scholar and JMIR. The full study selection process is shown in figure 1.
Fig. 1.
PRISMA54 Flow diagram of systematic search and study selection.
A total of 15 different articles were eligible for inclusion,10,24,28–38 reporting data from 12 unique samples of psychiatric patients (n = 3227). Details of included studies are available in supplementary table 1. Six were conducted in the United States,10,28–32 3 in the United Kingdom,24,33,35 2 in Canada,34,36 and 1 in India.38 Across all 3227 psychiatric patients within these studies, the mean age was 43.3 years (median = 40.3, range = 25.6–51.8). The majority were male (61.1%) and psychiatric outpatients (92%). Where race or ethnicity was specified, 42.5% were White, while 57.5% were identified as belonging to a minority within their respective countries. Eight studies (n = 2581) reported employment and/or income; 74.7% of participants were categorized as unemployed or having <$10000 annual income.
In order to explore mHealth feasibility specifically in psychosis, all meta-analyses were performed within a subgroup of 2129 participants, of whom 97% had a confirmed psychotic disorder (75% schizophrenia/schizoaffective disorder). This subsample was obtained by only including study data for which: (1) it could be confirmed that the entire (or vast majority) of the sample had a diagnosed psychotic disorder (N = 8, n = 868) or (2) ownership rates specifically among those with psychotic disorders were reported separately (N = 4, n = 1261). For 2 studies,32,36 phone ownership within the psychosis subsample was determined from original data retrieved from the corresponding authors.
Mobile Phone Ownership and Usage in Psychosis
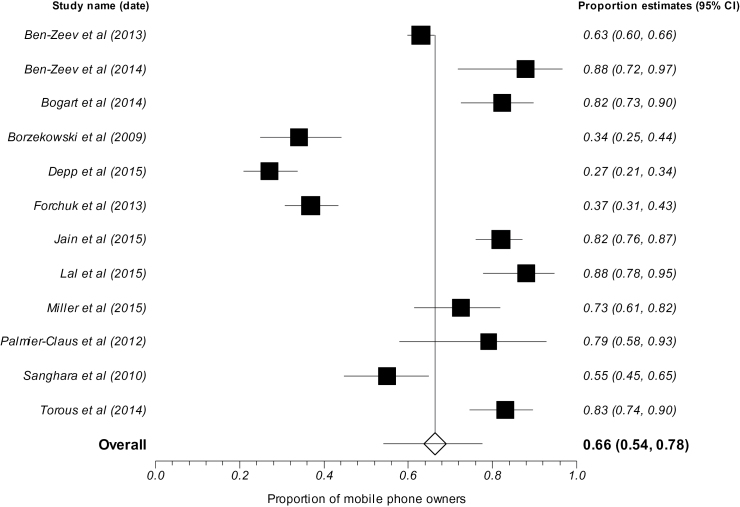
Proportional meta-analytic techniques were applied. As can be seen in figure 2, the overall rate of mobile phone ownership among people with psychosis was 66.4% (95% CI = 54.1%–77.6%). There was significant heterogeneity between studies (Cochran’s Q = 320.758498, df = 11, P < .0001, I 2 = 96.6% [95% CI = 95.7%−97.2%]). However, there was no indication of publication bias found by either visual inspection of funnel plot asymmetry or Eggers test (bias = 1.547216 [95% CI = −7.6 to 10.7), P = .713).
Fig. 2.
Proportional meta-analysis of mobile phone ownership among patients with psychosis. The forest plot shows the mobile phone ownership rates among eligible samples (see “Methods” section) in each study, including each study’s proportion estimate (Box points) and the 95% CI (horizontal lines). The diamond shows the overall ownership rate estimated from a random-effects model.
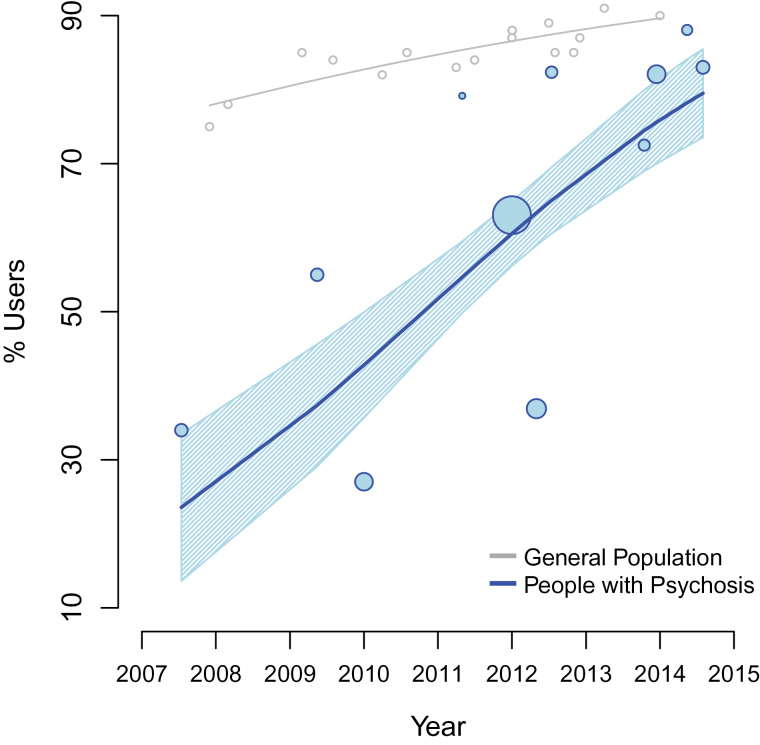
Time of data collection was reported in 7 studies28–30,33,36–38 and was retrieved from the corresponding author for 4 more.24,31,32,35 The GLM showed that mobile phone ownership has increased over time (figure 3), as there was a statistically significant, positive relationship between mid-date of data collection and mobile phone ownership (t = 3.019, P = .0145, coefficient = .001, which is equivalent to an estimate of a 3% increase in the OR of owing a cell phone with every month). The same was found when considering start or end date of data collection (supplementary figure 1A and 1B). Due to the increases in mobile phone ownership over time, a sensitivity analysis was conducted on data collected from 2013 to present (N = 4, n = 454). Across patients with psychosis surveyed within the last 2 years, 81.4% owned a mobile phone (95% CI = 75.8%–86.3%).
Fig. 3.
The increase in mobile phone ownership over time. Blue points show individual studies, and point size represents sample size (square-rooted for scale). Blue line shows the fit of the GLM (see “Methods” section) and blue shading shows the SE. Grey line shows ownership among the general population in the United States.55
Device Type and Usage
Across 5 studies (n = 443) that examined type of mobile device, smartphones were owned by 35.4% of people with psychosis (95% CI = 12.3%–63.0%). Reports of mobile usage were aggregated and showed that 56.5% (95% CI = 39.5%–72.8%) of people with psychosis who owned phones used their device on a daily basis (N = 5, n = 890).
Interest in mHealth
Opinions on specific mHealth services were surveyed in 7 studies, across a total of 1172 patients with psychotic disorders. The proportion of favorable responses for the most popular mHealth services was: 60.2% of service users in favor of using mobile phones for tracking/monitoring their mental health (95% CI = 42.6%–76.5%, N = 3, n = 251), 56.1% for receiving information about physical or mental health (95% CI = 33.4%–77.5%, N = 4, n = 944), 55.5% for appointment/medication reminders via text (95% CI= 35.8%–74.3%, N = 5, n = 968), and 51.1% for facilitating patient contact with health professionals (95% CI = 36.4%–65.6%, N = 5, n = 989).
Predictors of Mobile Ownership and Usage
Relationships between patient characteristics and mobile phone ownership/usage were reported in 6 studies. The only variables examined across multiple studies were: diagnosis, age, ethnicity, education, and income. Findings in each these areas were synthesized and are presented below.
Three studies considered clinical characteristics in relationship to mobile phone ownership. Ben-Zeev et al28 found that ownership was 23% lower among patients with schizophrenia/schizoaffective disorder than those with mood disorders. Similarly, Sanghara et al24 found 23% lower ownership rates among patients with “psychotic disorders” (primarily schizophrenia/schizoaffective disorder) than those with other psychiatric diagnoses. One study further exploring predictors of ownership in patients with schizophrenia/schizoaffective disorder30 found that those with more severe functional disability were less likely to have owned a mobile phone.
The relationship between age and mobile phone ownership among psychiatric patients was examined in 4 studies,24,28,30,32 all of which found younger patients were significantly more likely to own mobile phones. Due to the consistency of these findings, a post-hoc analysis was conducted to examine the relationship between age and ownership at the studylevel. However, mobile phone ownership across studies was not predicted by mean sample age (t = −1.41, P = .193, coefficient = .065; supplementary figure 1C). Additionally, 2 studies which investigated the association between age and text-messaging found no significant relationship of age with either use of texting31 or interest in receiving SMS medication reminders.33
Two studies examined relationships with education. Although “level of education” (eg, high school vs college graduate) did have a significant association with phone ownership,28 “total years in education” did not.30 Level of income also had a significant impact, as those with annual incomes of >$1000028 were 33% more likely to own a mobile phone than those without. However, interest in receiving mHealth services was equally high among both employed and unemployed participants.28 Three studies examined ethnicity and mobile phone ownership/usage in the United Kingdom33 and the United States.30,31 However, none of these studies found a significant association.
Discussion
Mobile Device Ownership Among People With Psychosis
This study used proportional meta-analyses across 12 independent samples to examine the feasibility of mHealth for psychosis. Overall, 66.4% of 2129 people with psychotic disorders (mostly schizophrenia or schizoaffective disorder) surveyed between 2007 and 2015 owned a mobile phone (figure 2). However, ownership rates have been increasing substantially, and significantly, over time (figure 3). Sensitivity analyses indicated that mobile phone ownership among people with psychosis is now around 81.4%, which is not dissimilar to the 90% observed in the general population.39
Previous research has raised the possibility that the feasibility of mHealth may be compromised in psychotic disorders, as a result of symptoms, cognitive dysfunction, or social isolation reducing technology adoption.24,25 Although some barriers will still exist, our findings largely dispel these particular concerns of availability and access. As shown in figure 3, the previously large divide between people with psychosis and the general population has closed substantially since 2007. Any remaining discrepancies are likely accounted for by economic factors, since the vast majority of our sample (75%) was unemployed or earning under $10000 perannum. Across 2 studies which explored barriers towards mHealth for people with psychosis, the most commonly cited issue was indeed affordability.28,38 Indeed, the most recent data from the United States shows that only 84% of people earning under $30000 perannum own a mobile phone,39 vs the 81.4% observed in people with psychosis surveyed within the last 2 years.
In contrast, smartphone ownership among people with psychosis was found to be only 35%. However, this was slightly higher in studies conducted in the United Kingdom, United States, or Canada, averaging 49%. Whereas smartphone ownership in these populations is currently around 63%,39,40 this drops to 50% among the lowest earners, indicating that reduced smartphone adoption among people with psychosis is again attributable to economic factors. Nonetheless, it may still be premature to roll out large scale “app-based” interventions for schizophrenia, since less than half of patients would currently be able to access these services. This would particularly exclude older patients with more severe functional impairments, who are less likely to own and use mobile technologies.24,28,30 Furthermore, financial barriers towards device ownership may also impact on patients’ ability to afford the necessary data plans for fully engaging with smartphone interventions.
However, we can predict that smartphone ownership will continue to increase among people with psychosis, on the basis of the aforementioned trends in regular mobile phone ownership, and also observations in the general population. For instance, the greatest growth in smartphone adoption in recent years has been observed among disadvantaged groups, with ownership among the lowest earners in the United States more than doubling since 2011.20,39 Additionally, relatively high levels of smartphone ownership (of around 68%) are already observed among younger patients, in earlier stages of psychotic disorders.34,37 Along with presenting immediate opportunities for early intervention services, this also suggests it would be astute to begin developing and testing applications now, so that scalable interventions are ready by the time widespread adoption has occurred.
Opinions of mHealth Services Among People With Psychosis
While the majority of patients responded in favor of the mHealth services surveyed, endorsement for each option was far from unanimous. However, the single study which reported overall interest in mHealth among people with serious mental illness found that 81% of phone owners were interested in at least one of the options presented.28 Therefore, offering a range of mobile interventions to all service users, for them to choose which areas of healthcare they feel most willing to engage with via their mobile phones, could be the most accessible route towards implementing mHealth in the treatment of psychotic disorders.
Of all the mHealth options surveyed, the most popular was mobile tracking and/or monitoring of health status. Around 60% of people with psychosis agreed that this is something they would use. Novel smartphone applications for symptom monitoring in psychosis are in development and have proved highly feasible in pilot studies.35 Furthermore, patients may find smartphone monitoring easier than text-message monitoring and have higher adherence to app-based interventions.5 However, it should be considered that even for this most popular option, 40% of patients did not feel this is something they would engage with at this point.
The most commonly surveyed mHealth options were (1) text-message reminders for appointments or medications and (2) enhancing patient-to-service contact using mobile phones. Both of these were widely acceptable, with the majority of service users responding in favor. A key benefit of text-message reminders and mobile phone-contact is that they are both possible without smartphone devices, and thus will be immediately accessible to the large majority of patients. Previous studies which have implemented these simple interventions have found they can reduce service costs, increase treatment adherence, and improve clinical outcomes in psychosis.11,13,41 Such interventions may confer maximum benefits when applied in an adjunctive manner to support the delivery of pharmacological and psychological treatment programs.41 Due to the current penetration of regular mobile devices, and the clear benefits for both healthcare services and their patients, services should now consider offering these as standard in the treatment of psychosis.
Our findings further indicate that the majority of people with psychosis are interested in not only monitoring, but also improving their health via mobile phones, since another well-received option was using mobile devices for health information. Although possible through regular devices, smartphone technology also broadens the horizons for novel interventions in this area. Feasibility studies have found that smartphone applications which provide personalized health information and self-management tools to psychiatric outpatients can improve health status, independence, and clinical outcomes.10,42
Along with enhancing psychiatric care, smartphone applications could also provide novel methods for tackling the physical health inequalities associated with psychotic disorders.43 The popularity of fitness apps in the general population is growing faster than any other app category,23,44 with around one-third of smartphone owners use such apps on a regular basis.22,23 Since physical exercise can be an effective complimentary therapy for many symptoms of psychotic disorders,45 future research should aim to develop suitable fitness apps for people with psychosis. Indeed, feasibility trials of using smartphone apps to support healthy lifestyles for people with serious mental illness have showed initial success.46 Most recently, remote monitoring devices and wearable sensors which monitor exercise, heart rate, and even sleep have been integrated with smartphone app interfaces to provide real-time feedback and personalized activity recommendations for people with mental health problems.47–49
Limitations and Future Directions
One limitation of this review is the broad diagnostic inclusion criteria of “psychotic illness” or “psychosis”. This was used to maximize external validity of the findings but may reduce the accuracy of phone ownership estimations for any specific diagnostic group. Three studies which examined the relationship between clinical variables and mobile phones collectively indicated that illness severity is negatively associated with ownership and usage.24,28,30 However, although a range of nonaffective and affective psychoses were present within the sample, 75% of the included subjects did have schizophrenia/schizoaffective disorder. An additional limitation is that while most of these patients did feel they would use mHealth services, we cannot necessary expect that these broadly positive attitudes will translate directly into adherent behaviors, due to the attitude-behavior gap.50
A major challenge is introducing new mHealth services into routine mental healthcare. Currently, community mental health services are often unable to provide sufficient access to psychosocial interventions for psychosis, with treatments such as cognitive behavioral therapy available to only 10% of patients or less, due to resource constraits.16,17 Thus, community-based treatment for psychosis could be enhanced through providing a range of mHealth interventions, which can be broadly disseminated across any number of patients, in order to provide adjunctive support within existing treatment programs.10,41 These digital solutions to mental healthcare may prove particularly valuable in regions of the world where there is a scarcity of traditional resources or poor access to services.51
While early results of mHealth interventions in psychosis appear promising, a number of important practical and ethical issues have also been highlighted, such as data protection, privacy, safety, and security, to ensure public and patient trust in new technologies.15,52,53 Furthermore, many interventions have been developed without significant service user or clinician involvement, and clinical efficacy is largely unknown. Future research should aim to build the currently limited evidence base, in order to develop accessible, user-led mHealth services which are capable of enhancing and expanding the provision of care for people with psychosis.
Supplementary Materials
Supplementary material is available at http://schizophreniabulletin.oxfordjournals.org
Funding
S.B. is in receipt of a research grant from the Medical Research Council (UK) to support the development and feasibility testing of a smartphone application for psychosis.
Supplementary Material
Acknowledgment
The authors declare that there are no conflicts of interest in relation to the subject of this study.
References
- 1. Horvath T, Azman H, Kennedy GE, Rutherford GW. Mobile phone text messaging for promoting adherence to antiretroviral therapy in patients with HIV infection. Cochrane Database Syst Rev. 2012;4:CD009756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Gurol‐Urganci I, de Jongh T, Vodopivec‐Jamsek V, Atun R, Car J. Mobile phone messaging reminders for attendance at healthcare appointments. Cochrane Database Syst Rev. 2013;12:CD007458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Gurol‐Urganci I, de Jongh T, Vodopivec‐Jamsek V, Car J, Atun R. Mobile phone messaging for communicating results of medical investigations. Cochrane Database Syst Rev 2012;6:CD007456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kauer SD, Reid SC, Crooke AH, et al. Self-monitoring using mobile phones in the early stages of adolescent depression: randomized controlled trial. J Med Internet Res. 2012;14:e67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ainsworth J, Palmier-Claus JE, Machin M, et al. A comparison of two delivery modalities of a mobile phone-based assessment for serious mental illness: native smartphone application vs text-messaging only implementations. J Med Internet Res. 2013;15:e60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bricker JB, Mull KE, Kientz JA, et al. Randomized, controlled pilot trial of a smartphone app for smoking cessation using acceptance and commitment therapy. Drug Alcohol Depend. 2014;143:87–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Torous J, Powell AC. Current research and trends in the use of smartphone applications for mood disorders. Internet Interv. 2015;2:169–173 [Google Scholar]
- 8. Marcano Belisario JS, Huckvale K, Greenfield G, Car J, Gunn LH. Smartphone and tablet self management apps for asthma. Cochrane Database Syst Rev. 2013;11:CD010013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dobson R, Carter K, Cutfield R, et al. Diabetes Text-Message Self-Management Support Program (SMS4BG): A Pilot Study. JMIR Mhealth Uhealth. 2015;3:e32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ben-Zeev D. Mobile technologies in the study, assessment, and treatment of schizophrenia. Schizophr Bull. 2012;38:384–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sims H, Sanghara H, Hayes D, et al. Text message reminders of appointments: a pilot intervention at four community mental health clinics in London. Psychiatr Serv. 2012;63:161–168. [DOI] [PubMed] [Google Scholar]
- 12. Španiel F, Hrdlicka J, Novák T, et al. Effectiveness of the information technology-aided program of relapse prevention in schizophrenia (ITAREPS): a randomized, controlled, double-blind study. J Psychiatr Pract. 2012;18:269–280. [DOI] [PubMed] [Google Scholar]
- 13. Palmier-Claus JE, Rogers A, Ainsworth J, et al. Integrating mobile-phone based assessment for psychosis into people’s everyday lives and clinical care: a qualitative study. BMC Psychiatry. 2013;13:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ben-Zeev D, Brenner CJ, Begale M, Duffecy J, Mohr DC, Mueser KT. Feasibility, acceptability, and preliminary efficacy of a smartphone intervention for schizophrenia. Schizophr Bull. 2014;40:1244–1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hollis C, Morriss R, Martin J, et al. Technological innovations in mental healthcare: harnessing the digital revolution. Br J Psychiatry. 2015;206:263–265. [DOI] [PubMed] [Google Scholar]
- 16. Haddock G, Eisner E, Boone C, Davies G, Coogan C, Barrowclough C. An investigation of the implementation of NICE-recommended CBT interventions for people with schizophrenia. J Ment Health. 2014;23:162–165. [DOI] [PubMed] [Google Scholar]
- 17. Schizophrenia Commission. The abandoned illness: a report from the Schizophrenia Commission. London: Rethink Mental Illness; 2012. [Google Scholar]
- 18. Department of Health. No health without mental health: a cross-government mental health outcomes strategy for people of all ages. London, UK: Stationery Office; 2011. [Google Scholar]
- 19. Wang J-Y, Bennett K, Probst J. Subdividing the digital divide: differences in internet access and use among rural residents with medical limitations. J Med Internet Res. 2011;13:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Smith A. 46% of American adults are smartphone owners http://www.pewinternet.org/2012/03/01/nearly-half-of-american-adults-are-smartphone-owners Accessed June 21, 2015.
- 21. Zickuhr K, Smith A. Digital differences http://www.pewinternet.org/2012/04/13/digital-differences Accessed June 21, 2015.
- 22. Fox S, Duggan M. Mobile health 2012. http://www.pewinternet.org/2012/11/08/mobile-health-2012 Accessed June 21, 2015.
- 23. Jahns R, Houck P. Mobile Health Market Report 2013–2017. Research2Guidance 2013. http://www.research2guidance.com/shop/index.php/mobile-healthtrends-and-figures. Accessed June 21, 2015 [Google Scholar]
- 24. Sanghara H, Kravariti E, Jakobsen H, Okocha CI. Using short message services in mental health services: assessing feasibility. Ment Health Rev. 2010;15:28–33. [Google Scholar]
- 25. Daker-White G, Rogers A. What is the potential for social networks and support to enhance future telehealth interventions for people with a diagnosis of schizophrenia: a critical interpretive synthesis. BMC Psychiatry. 2013;13:279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. StatsDirect. StatsDirect statistical software. StatsDirect, UK 2005. [Google Scholar]
- 27. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. [DOI] [PubMed] [Google Scholar]
- 28. Ben-Zeev D, Davis KE, Kaiser S, Krzsos I, Drake RE. Mobile technologies among people with serious mental illness: opportunities for future services. Adm Policy Ment Health. 2013;40:340–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Borzekowski DL, Leith J, Medoff DR, et al. Use of the internet and other media for health information among clinic outpatients with serious mental illness. Psychiatr Serv. 2009;60:1265–1268. [DOI] [PubMed] [Google Scholar]
- 30. Depp CA, Harmell AL, Vahia IV, Mausbach BT. Neurocognitive and functional correlates of mobile phone use in middle-aged and older patients with schizophrenia [published online ahead of print March 13, 2015]. Aging Ment Health. doi: 10.1080/13607863.2015.1008987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Miller BJ, Stewart A, Schrimsher J, Peeples D, Buckley PF. How connected are people with schizophrenia? Cell phone, computer, email, and social media use. Psychiatry Res. 2015;225:458–463. [DOI] [PubMed] [Google Scholar]
- 32. Torous J, Chan SR, Tan SY-M, et al. Patient smartphone ownership and interest in mobile apps to monitor symptoms of mental health conditions: A survey in four geographically distinct psychiatric clinics. JMIR Mental Health. 2014;1:e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Bogart K, Wong SK, Lewis C, et al. Mobile phone text message reminders of antipsychotic medication: is it time and who should receive them? A cross-sectional trust-wide survey of psychiatric inpatients. BMC Psychiatry. 2014;14:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Lal S, Dell’Elce J, Malla AK. Technology Access and Use Among Young Adults With a First Episode of Psychosis. Psychiatr Serv. 2015;66:764–765. [DOI] [PubMed] [Google Scholar]
- 35. Palmier-Claus JE, Ainsworth J, Machin M, et al. The feasibility and validity of ambulatory self-report of psychotic symptoms using a smartphone software application. BMC Psychiatry. 2012;12:172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Forchuk C, Rudnick A, Hoch J, et al. Mental health engagement network: Innovating community-based mental healthcare. J Gen Pract. 2013;2. [Google Scholar]
- 37. Lal S, Dell’Elce J, Tucci N, Fuhrer R, Tamblyn R, Malla A. Preferences of young adults with first-episode psychosis for receiving specialized mental health services using technology: a survey study. JMIR Mental Health. 2015;2:e18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Jain N, Singh H, Koolwal GD, Kumar S, Gupta A. Opportunities and barriers in service delivery through mobile phones (mHealth) for Severe Mental Illnesses in Rajasthan, India: A multi-site study. Asian J Psychiatr. 2015;14:31–35. [DOI] [PubMed] [Google Scholar]
- 39. Pew Research Center. The Smartphone Difference 2015 http://www.pewinternet.org/2015/04/01/us-smartphone-use-in-2015 Accessed June 21, 2015.
- 40. Ofcom. The Communications Market Report 2014 http://stakeholders.ofcom.org.uk/binaries/research/cmr/cmr14/2014_UK_CMR.pdf Accessed 21 June, 2015.
- 41. Drake RJ, Nordentoft M, Haddock G, et al. Modeling determinants of medication attitudes and poor adherence in early nonaffective psychosis: implications for intervention. Schizophr Bull. 2015;41:584–596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Forchuk C, Donelle L, Ethridge P, Warner L. Client erceptions of the mental health engagement network: a secondary analysis of an intervention using smartphones and desktop devices for individuals experiencing mood or psychotic disorders in canada. JMIR Mental Health. 2015;2:e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Mitchell AJ, Vancampfort D, Sweers K, van Winkel R, Yu W, De Hert M. Prevalence of metabolic syndrome and metabolic abnormalities in schizophrenia and related disorders–a systematic review and meta-analysis. Schizophr Bull. 2013;39:306–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Khalaf S. Health and fitness apps finally take off, fueled by fitness fanatics http://www.flurry.com/blog/flurry-insights/health-and-fitness-apps-finally-take-fueled-fitness-fanatics Accessed June 21, 2015.
- 45. Firth J, Cotter J, Elliott R, French P, Yung AR. A systematic review and meta-analysis of exercise interventions in schizophrenia patients. Psychol Med. 2015;45:1343–1361. [DOI] [PubMed] [Google Scholar]
- 46. Macias C, Panch T, Hicks YM, et al. Using Smartphone Apps to Promote Psychiatric and Physical Well-Being [published online ahead of print January 31, 2015]. Psychiatr Q. doi: 10.1007/s11126-015-9337-7 [DOI] [PubMed] [Google Scholar]
- 47. Naslund JA, Aschbrenner KA, Barre LK, Bartels SJ. Feasibility of popular m-health technologies for activity tracking among individuals with serious mental illness. Telemed J E Health. 2015;21:213–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Puiatti A, Mudda S, Giordano S, Mayora O. Smartphone-centred wearable sensors network for monitoring patients with bipolar disorder. Conf Proc IEEE Eng Med Biol Soc. 2011;2011:3644–3647. [DOI] [PubMed] [Google Scholar]
- 49. Lanata A, Valenza G, Nardelli M, Gentili C, Scilingo EP. Complexity index from a personalized wearable monitoring system for assessing remission in mental health. IEEE J Biomed Health Inform. 2015;19:132–139. [DOI] [PubMed] [Google Scholar]
- 50. Ajzen I. The theory of planned behavior. Organ Behav Hum Dec. 1991;50:179–211. [Google Scholar]
- 51. Brian RM, Ben-Zeev D. Mobile health (mHealth) for mental health in Asia: objectives, strategies, and limitations. Asian J Psychiatr. 2014;10:96–100. [DOI] [PubMed] [Google Scholar]
- 52. Abebe NA, Capozza KL, Des Jardins TR, et al. Considerations for community-based mHealth initiatives: insights from three Beacon Communities. J Med Internet Res. 2013;15:e221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Giota KG, Kleftaras G. Mental health apps: innovations, risks and ethical considerations. E-Health Telecommunication Systems and Networks 2014;3:49481. [Google Scholar]
- 54. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Pew Research Center. Device ownership over time http://www.pewinternet.org/data-trend/mobile/device-ownership Accessed 21 June, 2015.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.