Abstract
Schizophrenia is associated with recurrent hospitalizations, need for long-term community support, poor social functioning, and low employment rates. Despite the wide- ranging financial and social burdens associated with the illness, there is great uncertainty regarding prevalence, employment rates, and the societal costs of schizophrenia. The current study investigates 12-month prevalence of patients treated for schizophrenia, employment rates, and cost of schizophrenia using a population-based top-down approach. Data were obtained from comprehensive and mandatory health and welfare registers in Norway. We identified a 12-month prevalence of 0.17% for the entire population. The employment rate among working-age individuals was 10.24%. The societal costs for the 12-month period were USD 890 million. The average cost per individual with schizophrenia was USD 106 thousand. Inpatient care and lost productivity due to high unemployment represented 33% and 29%, respectively, of the total costs. The use of mandatory health and welfare registers enabled a unique and informative analysis on true population-based datasets.
Key words: schizophrenia, prevalence, employment, cost-of-illness
Introduction
Schizophrenia is a disabling psychiatric illness with severe and long-term consequences for patients and their families. The illness generally onsets during early adulthood and is often associated with recurrent hospitalizations, need for long-term community support, poor social functioning, and high-unemployment rates.1–4 Despite the wide-ranging implications associated with the illness, only one previous study has estimated the costs of schizophrenia in Norway.5 This was a prevalence-based study where direct costs of mental health services for patients with schizophrenia were estimated from data collected from treatment units in 6 catchment areas over a period of 4 weeks in 1994. This study did not include indirect costs, such as lost productivity and social security costs. Furthermore, given the changes in mental health services since 1994, this study is unlikely to offer reliable estimates of the current costs of the illness.
Cost estimates of an illness are often based on estimates of cost per patient multiplied with the prevalence of the illness.6 Prevalence estimates, however, vary greatly between studies. Perala and colleagues found a 0.87% lifetime prevalence of schizophrenia and 0.32% for schizoaffective disorder in a sample of 8028 persons,7 while Saha and colleagues8 found the lifetime prevalence of schizophrenia to be 0.4% and the period prevalence (1–12 mo) to be 0.33% in a systematic review of 1721 prevalence estimates worldwide. Furthermore, Mangalore and Knapp2 estimated 0.2% prevalence based on psychiatric morbidity surveys and past incidence estimates. Based on data from hospitals and outpatient clinics, the point prevalence in a Norwegian county was estimated at 0.15%9 while the national point prevalence was estimated to be approximately 0.2%.10 In a register-based study, Nesvag and colleagues found the 5 year prevalence of schizophrenia in the Norwegian population between 24 and 63 years of age to be 0.34%.11 These large variations highlight the need to establish reliable and current prevalence estimates in order to undertake a cost estimate.
Past cost estimates have identified lost productivity due to high unemployment to represent a large proportion of the total costs associated with schizophrenia.1,2,12 The estimates of lost productivity are, however, dependent upon reliable estimates of the employment rates. Estimated employment rates among people with schizophrenia in western societies range from 12% to 39%.1,2,13,14 A survey-based study of 4684 schizophrenia patients in Norway receiving outpatient care found that 5% had paid employment.15 Other Norwegian studies based on smaller samples have found employment rates between 4%16 and 13%.17 The uncertainty regarding employment for the schizophrenia population illustrates the need to establish employments rates based on reliable data sources.
Understanding the prevalence and cost of schizophrenia is of importance for service planning, prioritization of resources, and for establishing the cost-effectiveness of current and future interventions.18Although there are no current estimates of the cost of schizophrenia in Norway, studies from comparable countries, such as Sweden and England, have estimated the average societal costs per individual to be USD 63000 and USD 69000 per year.2,12
The objective of the current study was to access national health and welfare registers covering the entire Norwegian population to establish 12-month prevalence of patients treated for schizophrenia, 12-month employment rate, and 12-month cost of schizophrenia. To our knowledge, this is the first study to investigate prevalence, employment rates, and cost of schizophrenia on such a comprehensive data material.
Methods
We used a population-based top-down design, where we obtained data through national registers for the period January 1 to December 31, 2012. A “top-down” approach uses aggregate figures on resource consumption related to diagnoses and relies on available data. The advantages of this method are that it relates directly to the total costs of the illness without extrapolation and avoids the risk of double-counting costs. The weakness of the “top-down” approach is that only individuals registered are included, which may provide a conservative estimate.19,20 We estimated both direct (ie, treatment and community care) and indirect (ie, social security and lost productivity) costs associated with schizophrenia. Costs associated with persons with schizophrenia who committed serious crimes and were detained in forensic mental health units were included. Costs related to premature mortality, volunteer and family care, and the criminal justice system were not included.
All costs are reported in USD and Norwegian Kroner (NOK). For currency conversions of mental health and community care services, we used The Organization for Economic Co-operation and Development’s (OECD) 2011 purchasing power parities (PPP) benchmark results for health expenditures (9.19 NOK = 1 USD). For conversions of social security and lost productivity, we used the PPP for Gross Domestic Product (8.54 NOK = 1 USD).21
Schizophrenia was defined by ICD-10 codes, F20: schizophrenia and F25: schizoaffective disorder. The study was approved by the Norwegian Data Protection Authority, notification 70403.
Prevalence and Employment Rate
All patients in contact with Norwegian mental health services are registered in the Norwegian Patient Register (NPR). The NPR is an administrative database of records reported by all government-owned hospitals and outpatient clinics receiving governmental reimbursements. Such mental health clinics are available across the country to serve the entire population. The NPR includes each patient’s unique personal identification number, enabling access to person-specific data. We obtained data on all patients registered with a primary diagnosis of schizophrenia or schizoaffective disorder in 2012.
All new employees in Norway must be registered with the Norwegian Labor and Welfare Administration (NAV) by their employer. Those who are self-employed are required to submit a coordinated register notification to the Register of Business Enterprises. Statistics Norway control data from these registers against the individual’s tax return to generate register-based statistics on employment, self-employment, and national service. To be included in the statistics, individuals needed to be contracted to have at least 1 hour of paid work during a reference week.
We merged the unique personal identification numbers of all persons identified with schizophrenia in the NPR with employment status in the register-based employment statistics. Those younger than 15 years and those older than the retirement age (67 y) were excluded from the calculations. As the statistics do not provide actual income, we conservatively assume that those registered as employed were not reliant on social services.
Specialist Mental Health Services Cost
In accordance with Norwegian legislation, residents are entitled to free inpatient care. For outpatient care, patients are required to pay a user fee up to a maximum sum per calendar year. Thereafter, treatment (including medication) is free for the rest of the year. In 2012, the maximum user fee was USD 215 (NOK 1980).
Data on specialist mental healthcare were obtained from the NPR. Inpatient mental health services in Norway are capitation funded. All hospitals report their annual results to Statistics Norway, and mean and total costs per day in psychiatric hospitals are calculated.22 Following recommendations from The Norwegian Directorate of Health, we calculated costs of hospitalizations by multiplying the number of days of hospitalization with the mean cost of care per day in a psychiatric hospital. Outpatient visits are partially capitation funded (60%) and partially fee-for-service funded (40%). We estimated mean costs for outpatient visits by dividing the total fees paid for outpatient visits by the number of visits22 and added 60% capitation. We calculated the outpatient costs by multiplying the number of outpatient visits with the estimated mean cost. Costs for day treatment programs were estimated by multiplying the total number of days in the programs with the mean cost per day in specialized community mental health centers.22
Costs of Antipsychotic Medications
Data concerning cost of antipsychotic medications prescribed for schizophrenia were extracted from the Norwegian Prescription Database (NorPD) at the Norwegian Institute of Public Health.
Primary Health and Community Care Services Cost
A large proportion of health services in Norway are provided in the municipalities. Local authorities in each municipality are responsible for primary care services, which include general medical services, home care services, nursing home care, and primary mental healthcare. The Norwegian Health Economics Administration (HELFO) reimburses general practitioners for all consultations with patients. Patient appointments are registered with a primary diagnosis, and general practitioners bill HELFO for the consultation. We obtained the total sum of reimbursements for treatment of schizophrenia by general practitioners from HELFO.
Municipality-based institutional care and home care services are reported to the Individual-based Register of Care Services (IPLOS). Service users may refuse information concerning diagnoses being registered, hence the actual number of users of municipality services may be higher than what is reported.23 To examine how representative the IPLOS data was, we extrapolated housing data from a cohort of 744 individuals with schizophrenia from 2 ongoing research projects. Norwegian Centre for Mental Disorders Research (NORMENT) recruits persons with psychotic disorders from a large catchment area in eastern Norway, and The Job Management Program (JUMP) recruits participants from 6 catchment areas across the country. The extrapolated number of individuals receiving institutional care was lower than what was registered in the IPLOS register. Hence we assume that the vast majority of recipients of municipality-based service with schizophrenia are registered in the IPLOS register.
Social Security Payments
The Norwegian welfare system provides all unemployed residents with a base income. The NAV provides sick leave payments, disability pensions, and other benefits associated with absence from work. These benefits are linked to the individual’s diagnosis and were acquired directly from NAV’s registers. Sick leave benefits are paid for up to 12 months. If still unable to return to work, the most common income allowance is a work assessment allowance. This allowance is not linked to a diagnosis. It is intended to ensure income during and between employment schemes, medical treatment, or other follow-up measures from NAV and is commonly provided for long durations in lieu of disability benefits. We assumed that the vast majority of individuals with schizophrenia who were not working, studying, or receiving a disability or aged pension were receiving a work assessment allowance. We have conservatively used the minimum work assessment allowance rate for our estimates.
Results
Twelve-Month Prevalence
There were 8399 individuals in the NPR registered with a primary diagnosis of schizophrenia or schizoaffective disorders of which 59% were men. We divided this number by the average population (N = 498587024) for 2012 to calculate the 12-month prevalence of 0.17% for the entire population. Assuming all individuals with schizophrenia were over the age of 18, the 12-month prevalence for the population 18 and older was 0.22%. Table 1 displays prevalence rates based on age and sex.
Table 1. Twelve-Month Prevalence of Schizophrenia Per Sex and Age Group
| Age | Men (%) | Women (%) | Total (%) |
|---|---|---|---|
| 10–19 | 0.02 | 0.02 | 0.01 |
| 20–29 | 0.30 | 0.15 | 0.22 |
| 30–39 | 0.40 | 0.21 | 0.31 |
| 40–49 | 0.34 | 0.24 | 0.29 |
| 50–59 | 0.24 | 0.24 | 0.24 |
| 60 and older | 0.09 | 0.11 | 0.10 |
| Overall | 0.20 | 0.14 | 0.17 |
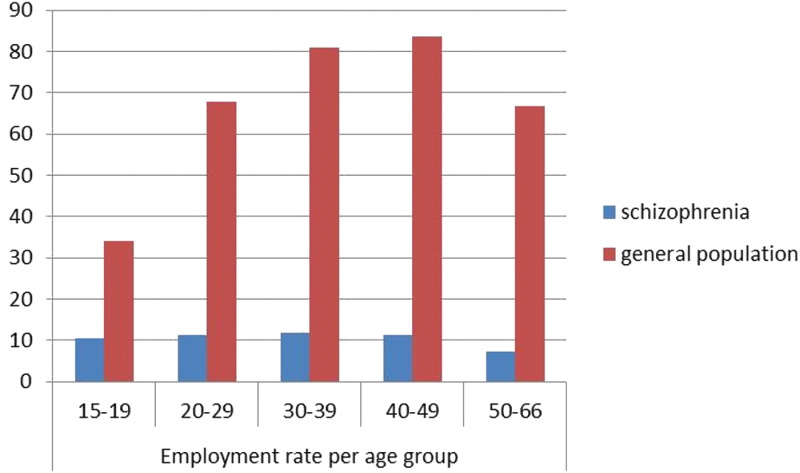
Employment
There were 817 individuals with schizophrenia who were employed and 413 who received age care pension. The employment rate (full time and part time) among those of working age was 10.24%–10.5% of the men and 9.8% of the women. The employment rate for the schizophrenia population was consistently low across all age groups in contrast to the general population where the employment rate peaks in the 40–49 age group (figure 1).
Fig. 1.
Employment rate per age group for the schizophrenia population and the general population. Employment = at least 1 hour competitive work per week.
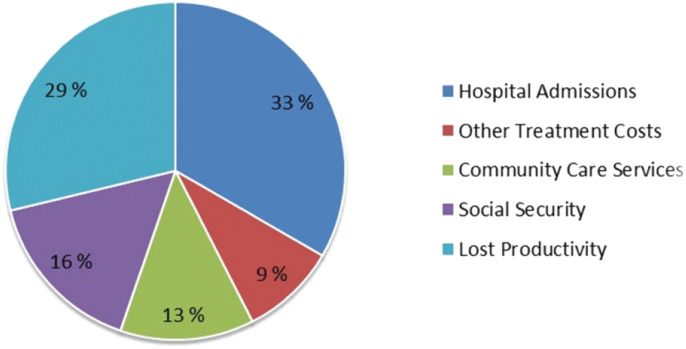
Costs
Observed and estimated total national costs associated with schizophrenia were USD 890,413,045.00 (NOK 7,913,534,423.00). The average cost per individual with schizophrenia was USD 106,014.00 (NOK 942,199.00). Details regarding these costs are presented below and in table 2.
Table. 2.
Total National Costs for Schizophrenia in 2012
| Total Cost (NOK) | Total Cost (USD) | |||
|---|---|---|---|---|
| Mental health treatment | N | Mean no d (SD) | ||
| Hospital admissionsa | 9411 | 23.82 (44.08) | 2639071456 | 287167732 |
| Outpatient visitsa | 177971 | 401752500 | 43716268 | |
| Day treatmentsa | 5867 | 1.48 (6.96) | 61251435 | 6665009 |
| GP consultationsa | 100216 | 82403408 | 8966639 | |
| Antipsychotic medicationa | 179212356 | 19500800 | ||
| Total treatment costs | 3363691155 | 366016448 | ||
| Community care services | N | Cost (NOK) | ||
| Institutional or staffed housinga (d) | 1056 | 2603 | 1003300320 | 109173049 |
| Home assistance (h)* | 1390 | 515 | 715850 | 77894 |
| Home nursing (h)* | 7591 | 900 | 6831900 | 743406 |
| Total community care services | 1010848070 | 109994349 | ||
| Social security | N | Mean (NOK) | ||
| Disability pensiona | 3141 | 194823 | 611939043 | 71655626 |
| Sick leave benefitsa | 359 | 90031 | 32321129 | 3784676 |
| Work assessment allowanceb | 3706 | 164244 | 608688264 | 71274972 |
| Basic benefitsa | 709 | 13003 | 9218828 | 1079488 |
| Total social security | 1262167264 | 147794762 | ||
| Lost productivity costs | N | Mean (NOK) | ||
| Lost FTEsb | 5231 | 363800 | 1903037800 | 222838150 |
| Absence from worka | 359 | 21226 | 7620134 | 892287 |
| Lost taxes deducted subsidiesb | 5231 | 70000 | 366170000 | 42877049 |
| Total lost productivity costs | 2276827934 | 266607486 | ||
| Total costs | 7913534423 | 890413045 |
Note: NOK, Norwegian Krone; USD, US Dollar
aRegistered data.
bEstimated data.
Mental Health Treatment Costs.
In 2012, there were a total of 9411 hospital admissions with schizophrenia as the primary diagnosis. These inpatients spent a total of 224144 (mean 23.8, range = 361) days in hospital, which constituted 18% of the total number of hospitalization days for all psychiatric conditions.25 The mean cost per day in a psychiatric hospital was USD 1,280.00 (NOK 11,774.00),22 and 33% of the societal costs associated with schizophrenia were related to hospitalizations (figure 2). The daily cost of day treatment programs was USD 770.00 (NOK 7077.00).22 Individuals with schizophrenia participated in 5867 day treatment programs over a total of 8655 days (mean 1.48, range = 253). The schizophrenia population had 177971 outpatient visits in 2012, which constituted 14% of all outpatient visits in the mental health services. The cost per outpatient visit was USD 246.00 (NOK 2257.00).22 Independent t tests revealed no sex difference in number of days in hospital, day treatment programs, or outpatient visits.
Fig. 2.
Distribution of societal costs of schizophrenia.
Community Care Services. We identified 1717 individuals with a schizophrenia diagnosis as receiving community care services, of which 1056 lived in institutions or accommodation with 24-hour staffing at a mean annual cost of USD 103,378.00 (NOK 950,047.00) per resident.26 A total of 7591 hours of home nursing at an hourly rate of USD 105 (NOK 900)27 and 1390 hours of home assistance at an hourly rate of USD 60 (NOK 515)27 were recorded.
Social Security Costs. Of the 8399 individuals registered with schizophrenia in 2012, 817 individuals were registered as working, 3141 were on a disability pension, and 359 received sick leave benefits. In addition, 709 individuals received basic benefits to cover extra expenses incurred as result of their illness. In the general population, 22.9% of individuals aged 19–29 years were students living off student loans and scholarships,28 while 1.2% were receiving a disability pension.29 The proportion of individuals with schizophrenia receiving a disability pension is 17%. Controlling for the higher rate of disability pensioners, we estimated that 282 individuals aged between 19 and 29 years with schizophrenia were students, and that 413 were receiving an age pension. It was assumed that the vast majority of the remaining 3746 individuals with schizophrenia received a work assessment allowance at a minimum annual cost of USD 19,232.00 (NOK 164,244.00) per person.30
Lost Productivity
We found that 7162 individuals with schizophrenia who were of working age were unemployed. The estimate of the monetary value of lost productivity was based on the human capital approach. This method estimates the value of potentially lost income as a consequence of the illness.31 We calculated the difference between employment rates among persons with schizophrenia and general working-age population (75.8%21) to be 5231 persons. Lost productivity in terms of potentially lost income was calculated as 5231 persons multiplied by the sum of the average wages and remuneration of USD 42,600.00 (NOK 363,800.00) plus average lost taxes deducted subsidies of USD 8,197.00 (NOK 70,000.00) for full-time employees during the 2012 tax year.32,33
Discussion
This study established a 12-month prevalence rate of 0.17% for individuals treated for schizophrenia in Norway. An employment rate of 10.24% and societal costs of USD 890 million (NOK 7.9 billion) was also found for this patient group using comprehensive healthcare and welfare registers.
It is difficult to compare the costs found in this study with previous cost estimates based on 1994 data.5 Corrected for consumer price index, the 2012 value of the 1994 estimate was USD 186 million (NOK 1.65 billion).34 This sum only included direct treatment costs in specialized mental health services. Furthermore, a bottom-up approach was undertaken in a small sample of 412 patients over just a 4-week period. In contrast, the current study used a population-based design with registered data over a 12-month period to estimate the cost of a comprehensive list of services used by individuals with schizophrenia; our study also included estimated indirect costs such as lost productivity and social security.
The 12-month prevalence of 0.17% was close to past 12-month prevalence estimates of 0.2%,2,10 and approximately half of the median period prevalence found in the review by Saha and colleagues.8 Traditional prevalence studies generate estimates based on the population residing within a defined catchment area. Within such sites, there may be variations in terms of age patterns, mortality rates, and social risk factors associated with schizophrenia (eg, urbanization, migration, poverty, and social exclusion) that may influence prevalence estimates.8,35,36 Although there is a significant migration towards the largest cities in Norway,37 two-thirds of the population live rural or in small cities with populations of less than 100000,38 which may partially explain our lower figures. Furthermore, due to a supportive welfare system, the prevalence of poverty and social exclusion in Norway is relatively low at 14% compared to the average for the European Union countries at 18.2%.39 It should also be noted that the 0.17% prevalence is based on the entire population. Considering that a schizophrenia diagnosis generally is established when individuals are in their late teens or later it may be more appropriate to use the prevalence of 0.22% for the population 18 and older. Also, our figures are based on treated prevalence of schizophrenia which is lower than the true prevalence. A recent study identified 10632 individuals registered in the NPR with schizophrenia or schizoaffective disorder over a 5-year period (2009–2013).11 As governmentally funded in- and out-patient mental health clinics service the entire population and are obliged to report data to the NPR, we believe this is close to the true prevalence, which indicate that 78% of those with schizophrenia access mental health services during a 12-month period.
The distribution of costs in this study is different from what has been found in comparable studies from Sweden and England.2,12 These studies have identified inpatient costs to represent between 8% and 16%, and indirect costs to represent between 46% and 60% of the total costs. In contrast, we estimate that 33% of the costs are related to inpatient care and 45% to indirect costs. This may be explained by methodological differences between the studies, and differences in the mental healthcare systems between countries. Norwegian mental health services have 83 psychiatric hospital beds per 100000 capita compared to 54 in the United Kingdom and 47 in Sweden.40 More patients receive services in specialized mental healthcare facilities41 and there is a higher density of psychiatrists in Norway than in most OECD countries,42 potentially explaining the high portion of costs associated with inpatient services in Norway. Factors such as availability of first-episode psychosis services, antipsychotic prescription practices, and prevalence of comorbid substance use disorders (SUD) may affect the course of the illness, and in turn the overall costs associated with schizophrenia. Reducing the duration of untreated psychosis (DUP) has received considerable attention following the results of the Scandinavian TIPS (early Treatment and Intervention in Psychosis) project,43 and it has been included as a national quality indicator.44 The median DUP in Norway is reported to be 9.7 weeks.41 A multicenter study investigating antipsychotic prescription practices for patients with schizophrenia in Norway found that the prescription pattern was partly in disagreement with international guidelines with use of polypharmacy in 35.6% and first-generation antipsychotics in 41.9% of the discharged patients. Also 35.6% received long-acting injectable antipsychotic drugs and clozapine was prescribed for 8% of the patients.45 Prevalence of SUD among individuals with schizophrenia in Norway has been found to be 25.1%.11 This is, however based on formal diagnoses registered in the NPR, so it is likely that the true prevalence of substance users is closer to past international estimates of 40%–50%.46,47
In line with previous studies, lost productivity due to unemployment had a substantial impact on the total costs associated with schizophrenia.1,2,12 We found that unemployment in the schizophrenia population follows a different pattern to the general population. In the general population, the employment rate rises from 68% in the 20- to 29-year-old age group up to 84% in the 40- to 49-year-old age group. In the schizophrenia population, however, employment rates were stable at just over 10% across all age groups with a drop to 7% after age 50. These rates are lower than the 12 to 39% employment rates reported in a recent international review.14 Limited access to supported employment services,48 ineffective vocational rehabilitation services in sheltered enterprises, and generous sick leave and disability benefits in Norway may provide an explanation for the differences.42
In recent years, there has been an increased focus on the benefits of employment for persons with schizophrenia and several studies have found reduced reliance on mental health services among those who obtain a job through employment services tailored for persons with severe mental illnesses.49,50 Considering the substantial costs associated with treatment and lost productivity for this patient group, shifting resources from inpatient care to tailored employment services may be an efficient treatment approach.
Strengths and Limitations
A major strength of this study was that the prevalence rate and utilization of mental health services was extracted from a mandatory health registry covering the entire population. Based on unique personal identification numbers, we were also able to obtain employment status of the entire national schizophrenia population, providing a reliable and accurate estimate of the unemployment rate.
Limitations of this study include that data from the NPR only included individuals who were in contact with mental health services during the 2012 calendar year and that costs associated with primary health resources, antipsychotic medications, community care services, and social security were extracted from mandatory registers based on diagnoses rather than unique identification numbers. Consequently, we cannot be certain that all individuals from these registers are included in the NPR. Diagnoses of psychotic disorders in the NPR also have not yet been subjected to formal validity testing, but a recent report comparing clinical and research-based diagnostic evaluations demonstrated good agreement for schizophrenia.51 Costs of medications are limited to antipsychotics as reliable data on other medications were not available. We could not access reliable data regarding the criminal justice system costs associated with schizophrenia. It has, however, been reported that police resources used on individuals with psychiatric conditions in total amount to only USD 7.26 million per year.52 We chose not to include this in the study as the figure is based on all mental illness related contact, and identification of schizophrenia specific contacts was not possible. Furthermore, according to Norwegian legislation, individuals with active psychoses should be detained in mental health hospitals rather than prisons, thus the costs incurred are accounted for as inpatient treatment. Also, our estimates are limited to costs directly linked to the primary schizophrenia diagnoses. Schizophrenia is associated with an excess risk for a number of medical conditions that may affect the overall costs, and the prevalence of smoking, obesity, hypertension, and dyslipidemia in a Norwegian sample has been found to be about twice those in a reference population.53 Finally, Norway’s high income and strong welfare system affect the generalizability of our results.
Conclusion
This study estimated the 12-month treated prevalence, employment rate, and societal cost of schizophrenia using comprehensive health and welfare registers. The results reiterate points made in earlier cost estimates of schizophrenia that the total burden of the disease is significant. We estimated the total annual direct and indirect cost for 8399 individuals with schizophrenia who made contact with mental health services in Norway to be USD 890 million (NOK 7.9 billion). Inpatient care accounted for 33% of the total cost. The unemployment rate of almost 90% generated lost productivity costs accounting for 29% of the total costs. Our use of mandatory health and welfare registers enabled a unique and informative analysis on true population-based datasets. This study highlights the significant costs associated with schizophrenia and also sheds light on the distribution of costs borne by different public services and by the society at large.
Funding
This work was supported by The Norwegian Directorate of Health (14/4607-13).
Acknowledgments
The authors have declared that there are no conflicts of interest in relation to the subject of this study. We thank the NPR, NAV, Statistics Norway, HELFO, NorPD, and the IPLOS registers for providing data for this study. We also thank the NORMENT and JUMP studies for providing a cohort to investigate representativity of data from the IPLOS register.
References
- 1. Knapp M, Mangalore R, Simon J. The global costs of schizophrenia. Schizophr Bull. 2004;30:279–293. [DOI] [PubMed] [Google Scholar]
- 2. Mangalore R, Knapp M. Cost of schizophrenia in England. J Ment Health Policy Econ. 2007;10:23–41. [PubMed] [Google Scholar]
- 3. Neil AL, Carr VJ, Mihalopoulos C, Mackinnon A, Morgan VA. Costs of psychosis in 2010: findings from the second Australian National Survey of Psychosis. Aust N Z J Psychiatry. 2014;48:169–182. [DOI] [PubMed] [Google Scholar]
- 4. Rössler W, Salize HJ, van Os J, Riecher-Rössler A. Size of burden of schizophrenia and psychotic disorders. Eur Neuropsychopharmacol. 2005;15:399–409. [DOI] [PubMed] [Google Scholar]
- 5. Rund BR, Ruud T. Costs of services for schizophrenic patients in Norway. Acta Psychiatr Scand. 1999;99:120–125. [DOI] [PubMed] [Google Scholar]
- 6. Ekman M, Granström O, Omérov S, Jacob J, Landén M. Costs of bipolar disorder, depression, schizophrenia and anxiety. The right treatments can have significant positive socio-economic effects. Lakartidningen. 2014;111:1362–1364. [PubMed] [Google Scholar]
- 7. Perälä J, Suvisaari J, Saarni SI, et al. Lifetime prevalence of psychotic and bipolar I disorders in a general population. Arch Gen Psychiatry. 2007;64:19–28. [DOI] [PubMed] [Google Scholar]
- 8. Saha S, Chant D, Welham J, McGrath J. A systematic review of the prevalence of schizophrenia. PLoS Med. 2005;2:e141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Johannessen JO. Schizofreni-forekomst i et norsk fylke, Rogaland. Nord Psykiatr Tidsskr 1985;39:217–223. [Google Scholar]
- 10. Johannessen JO. Schizophrenia–incidence and significance. Tidsskr Nor Laegeforen. 2002;122:2011–2014. [PubMed] [Google Scholar]
- 11. Nesvåg R, Knudsen GP, Bakken IJ, et al. Substance use disorders in schizophrenia, bipolar disorder, and depressive illness: a registry-based study. Soc Psychiatry Psychiatr Epidemiol. 2015;50:1267–1276. [DOI] [PubMed] [Google Scholar]
- 12. Ekman M, Granstrom O, Omerov S, Jacob J, Landen M. The societal cost of schizophrenia in Sweden. J Ment Health Policy Econ. 2013;16:13–25. [PubMed] [Google Scholar]
- 13. Kozma C, Dirani R, Canuso C, Mao L. Change in employment status over 52 weeks in patients with schizophrenia: an observational study. Curr Med Res Opin. 2011;27:327–333. [DOI] [PubMed] [Google Scholar]
- 14. Jonsdottir A, Waghorn G. Psychiatric disorders and labour force activity. Ment Health Rev Jr 2015;20:13. [Google Scholar]
- 15. Helle S, Gråwe R. Employment and social benefit among persons with schizophrenia in Norway. Journal of the Norwegian Psychological Association 2007;44:1358–1362. [Google Scholar]
- 16. Melle I, Friis S, Hauff E, Vaglum P. Social functioning of patients with schizophrenia in high-income welfare societies. Psychiatr Serv. 2000;51:223–228. [DOI] [PubMed] [Google Scholar]
- 17. Tandberg M, Sundet K, Andreassen OA, Melle I, Ueland T. Occupational functioning, symptoms and neurocognition in patients with psychotic disorders: investigating subgroups based on social security status. Soc Psychiatry Psychiatr Epidemiol. 2013;48:863–874. [DOI] [PubMed] [Google Scholar]
- 18. Hu TW. Perspectives: an international review of the national cost estimates of mental illness, 1990-2003. J Ment Health Policy Econ. 2006;9:3–13. [PubMed] [Google Scholar]
- 19. Henriksson F, Jönsson B. The economic cost of multiple sclerosis in Sweden in 1994. Pharmacoeconomics. 1998;13:597–606. [DOI] [PubMed] [Google Scholar]
- 20. Henriksson F, Fredrikson S, Masterman T, Jönsson B. Costs, quality of life and disease severity in multiple sclerosis: a cross-sectional study in Sweden. Eur J Neurol. 2001;8:27–35. [DOI] [PubMed] [Google Scholar]
- 21. OECD. Purchasing Power Parities for GDP and Related Indicators. Paris, France: OECD Publishing; 2015. [Google Scholar]
- 22. Huseby BM, Gjøen IJ, Sundet IB, et al. Samdata Sepsialisthelsetjenesten 2012. Oslo, Norway: Helsedirektoratet; 2013. [Google Scholar]
- 23. Helsedirektoratet. Information on the IPLOS Register. Oslo, Norway: Norwegian Directorate of Health; 2013. [Google Scholar]
- 24. Statistics Norway. Population and Population Changes. Oslo: Statistics Norway; 2015. [Google Scholar]
- 25. Indergård PJ, Skiri J-A, Solbakken T, Urfjell B. Aktivitetsdata Fra Psykisk Helsevern for Voksne Og Tverrfaglig Spesialisert Behandling Av Rusmiddelmisbruk 2012. Oslo, Norway: The Norwegian Directorate of Health; 2013. [Google Scholar]
- 26. Statistics Norway. KOSTRA - Municipality-State-reporting. Oslo: Statistics Norway; 2015. [Google Scholar]
- 27. Tenden L, Pettersen L. Omsorgstjenester Bransjestatistikk 2012: NHO Service; 2012. [Google Scholar]
- 28. Statistics Norway. Students at Universities and Colleges: Statistics Norway. Oslo: Statistics Norway; 2015. [Google Scholar]
- 29. Ellingsen J. Utviklingen i uførepensjon per 31. desember 2012. Oslo, Norway: Arbeids- og velferdsdirektoratet; 2013. [Google Scholar]
- 30. Kann IC, Kristoffersen P, Thune O. Arbeidsavklaringspenger – gjennomstrømming og avgang fra ordningen. Arbeid og Velferd 2013;1:41–57. [Google Scholar]
- 31. Koopmanschap MA, Rutten FF. A practical guide for calculating indirect costs of disease. Pharmacoeconomics. 1996;10:460–466. [DOI] [PubMed] [Google Scholar]
- 32. Statistics Norway. Tax Statistics for Personal Tax Payers. Oslo: Statistics Norway; 2015. [Google Scholar]
- 33. Statistics Norway. Average Labour Costs Per Full-time Equivalent Employee, by Industry (SIC2007). Oslo: Statistics Norway; 2015. [Google Scholar]
- 34. Statistics Norway. Consumer Price Index. Oslo: Statistics Norway; 2015. [Google Scholar]
- 35. Krabbendam L, van Os J. Schizophrenia and urbanicity: a major environmental influence–conditional on genetic risk. Schizophr Bull. 2005;31:795–799. [DOI] [PubMed] [Google Scholar]
- 36. Cantor-Graae E, Selten JP. Schizophrenia and migration: a meta-analysis and review. Am J Psychiatry. 2005;162:12–24. [DOI] [PubMed] [Google Scholar]
- 37. Høydahl E. Befolkningsvekst rundt Oslo. Samfunnsspeilet/Statistisk sentralbyrå 2010;5:11–19. [Google Scholar]
- 38. Statistics Norway. Population and Land Area in Urban Settlements. Oslo: Statistics Norway; 2015. [Google Scholar]
- 39. Di-Meglio E, Rusu C, Rybkowska A. Living Conditions in Europe. Luxembourg, Europe: Publications Office of the European Union; 2014. [Google Scholar]
- 40. OECD. Making Mental Health Count: The Social and Economic Costs of Neglecting Mental Health Care. OECD Health Policy Studies, Paris, France: OECD Publishing; 2014. [Google Scholar]
- 41. Ministerråd N. Kvalitetsmåling I Psykiatrien I De Nordiske lande. Copenhagen, Denmark: Nordisk Ministerråd; 2011. [Google Scholar]
- 42. OECD. Mental Health and Work: Norway. Paris, France: OECD Publishing;2013. [Google Scholar]
- 43. Melle I, Larsen TK, Haahr U, et al. Reducing the duration of untreated first-episode psychosis: effects on clinical presentation. Arch Gen Psychiatry. 2004;61:143–150. [DOI] [PubMed] [Google Scholar]
- 44. Ruud T. Mental health quality and outcome measurement and improvement in Norway. Curr Opin Psychiatry. 2009;22:631–635. [DOI] [PubMed] [Google Scholar]
- 45. Kroken RA, Johnsen E, Ruud T, Wentzel-Larsen T, Jørgensen HA. Treatment of schizophrenia with antipsychotics in Norwegian emergency wards, a cross-sectional national study. BMC Psychiatry. 2009;9:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Volkow ND. Substance use disorders in schizophrenia–clinical implications of comorbidity. Schizophr Bull. 2009;35:469–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Kavanagh DJ, McGrath J, Saunders JB, Dore G, Clark D. Substance misuse in patients with schizophrenia: epidemiology and management. Drugs. 2002;62:743–755. [DOI] [PubMed] [Google Scholar]
- 48. Falkum E, Evensen S, Lystad J, Bull HC, Ueland T. Effektevaluering av Jobbmestrende Oppfølging (JMO): Kognitiv Atferdsterapi og Kognitiv Trening I Arbeidsrehabilitering for Personer Med Psykoselidelser. Oslo, Norway: Helsedirektoratet; 2015. [Google Scholar]
- 49. Knapp M, Patel A, Curran C, et al. Supported employment: cost-effectiveness across six European sites. World Psychiatry. 2013;12:60–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Bush PW, Drake RE, Xie H, McHugo GJ, Haslett WR. The long-term impact of employment on mental health service use and costs for persons with severe mental illness. Psychiatr Serv. 2009;60:1024–1031. [DOI] [PubMed] [Google Scholar]
- 51. Oiesvold T, Nivison M, Hansen V, Skre I, Ostensen L, Sørgaard KW. Diagnosing comorbidity in psychiatric hospital: challenging the validity of administrative registers. BMC Psychiatry. 2013;13:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Nygaard E, Wie-Groenhof A. Drap i Norge i perioden 2004–2009. Oslo, Norway: Departementenes servicesenter; 2010. [Google Scholar]
- 53. Birkenaes AB, Søgaard AJ, Engh JA, et al. Sociodemographic characteristics and cardiovascular risk factors in patients with severe mental disorders compared with the general population. J Clin Psychiatry. 2006;67:425–433. [DOI] [PubMed] [Google Scholar]