Abstract
Integrated models of psychotic disorders have posited a number of putative psychological mechanisms that may contribute to the development of psychotic symptoms, but it is only recently that a modest amount of experience sampling research has provided evidence on their role in daily life, outside the research laboratory. A number of methodological challenges remain in evaluating specificity of potential causal links between a given psychological mechanism and psychosis outcomes in a systematic fashion, capitalizing on longitudinal data to investigate temporal ordering. In this article, we argue for testing ecological interventionist causal models that draw on real world and real-time delivered, ecological momentary interventions for generating evidence on several causal criteria (association, time order, and direction/sole plausibility) under real-world conditions, while maximizing generalizability to social contexts and experiences in heterogeneous populations. Specifically, this approach tests whether ecological momentary interventions can (1) modify a putative mechanism and (2) produce changes in the mechanism that lead to sustainable changes in intended psychosis outcomes in individuals’ daily lives. Future research using this approach will provide translational evidence on the active ingredients of mobile health and in-person interventions that promote sustained effectiveness of ecological momentary interventions and, thereby, contribute to ongoing efforts that seek to enhance effectiveness of psychological interventions under real-world conditions.
Key words: schizophrenia, ecological momentary intervention, experience sampling methodology, causal criteria, psychological intervention
Introduction
Recent years have seen a move toward integrated models of the etiology of psychotic disorders1–4 that consider not only the impact (and interplay) of biological and socioenvironmental factors but also posit a number of putative psychological mechanisms that may contribute to the development or exacerbation of psychosis.1–11 To date, these mechanisms have been primarily studied in the research laboratory using cross-sectional or experimental designs, and in relation to specific symptom dimensions (ie, positive symptoms, negative symptoms, disorganization, mania, and depression5,6,11) or specific symptom types (eg, hallucinations, delusions).1,6,7,12 It is only recently that, through a series of studies using experience sampling methodology13 (ESM; or, synonymously, ecological momentary assessment (EMA)14,15), we are beginning to understand the role of these putative psychological mechanisms in daily life, outside the research laboratory. ESM is a structured diary technique that allows for frequently repeated, naturalistic sampling of thoughts, feelings, and behavior experienced in the moment, nowadays typically accomplished through mobile devices.13–15 Experience sampling studies explicitly acknowledge, and purposefully seek to elucidate, the dynamic nature of psychological processes over time, harnessing the ESM’s unique advantage of capturing moment-to-moment variation in psychological processes through multiple assessments in the real world.13–15 The ESM further allows to study the impact of, and individuals’ interaction with, the microenvironment and, thereby more generally addresses calls for investigating more proximal, microlevel (rather than distal, macrolevel) environmental risks in the occurrence and persistence of psychosis.13,16
Putative Psychological Mechanisms in the Development and Exacerbation of Psychosis in Daily Life
Most experience sampling studies conducted to date have investigated stress sensitivity, characterized by increased emotional reactions to minor stressors and routine daily hassles, as a putative psychological mechanism in the development or exacerbation of psychotic symptoms in daily life using time-based designs with stratified (semi)random time sampling (ie, with ESM assessments scheduled at random or semirandom moments within set blocks of time).13,15 A number of studies have reported elevated emotional reactivity to minor stressful events, activities, and social situations in individuals with enduring psychosis and in those with higher familial or psychometric risk.17–21 Two studies in individuals at ultra high-risk (UHR) of developing psychosis,22,23 reported greater emotional reactivity to minor activity-related and social stress in this group.24,25 Findings from the only study conducted to date in individuals with first-episode psychosis (FEP),25 which allowed to minimize the impact of illness chronicity,20,24 further suggests that elevated stress sensitivity is associated with an increased intensity of psychotic experiences in FEP individuals, UHR individuals and controls, and this association is greatest in FEP individuals. In patients with psychotic disorder, stress sensitivity has also been specifically associated with positive symptoms of psychosis.26 Furthermore, it has been demonstrated that individuals with a psychotic disorder show increased reactivity to positive events happening to them.27 Specifically, they reported increased positive affect when a pleasant event was happening, suggesting an overall increased sensitivity to the environment, either positive or negative.
Experience sampling studies have considered the role of emotional and social experience in negative symptoms of schizophrenia in daily life.27–33 Findings from these studies suggest that, surprisingly, deficits in expression and blunted affect in individuals with psychotic disorder are not associated with a reduced intensity of emotional experience in daily life.30,31,33 However, individuals with schizophrenia and high negative symptoms have been found to show a stronger preference for being alone when in company and more social withdrawal in daily life.27 Similarly, there is evidence of a greater preference for solitude, increased time alone, and lower positive affect in the daily life of individuals with subclinical social anhedonia.28 While experience sampling studies have reported fewer goal-directed activities in individuals with schizophrenia, findings on a diminished effort in pursuit of complex goals in daily life remain equivocal.31,32
Other putative psychological mechanisms that have been investigated using ESM include cognitive self-consciousness,34 meta-cognitive beliefs,34,35 self-esteem,35–37 coping,38 self-management strategies,39,40 cognitive appraisal,41 affective disturbance,42,43 enhanced threat anticipation,25 experiences of aberrant novelty and salience,25 and their association with psychotic experiences. Taken together, ESM is an innovative method that has significantly improved our understanding of the association between a number of putative psychological mechanisms and psychotic experiences. However, notably, the number of experience sampling studies on putative psychological mechanisms that may contribute to the development of psychosis remain modest and have primarily been conducted in samples of patients with enduring psychotic disorder or individuals with increased familial or psychometric risk. Also, direct replication of findings using identical methodology across samples is rare and the role of a number of putative psychological mechanisms (eg, reasoning and attributional biases)1 proposed by contemporary models of psychosis remain to be investigated in daily life. However, probably the most important caveat of experience sampling research to date is that most studies used cross-sectional modeling without taking advantage of the longitudinal structure of ESM data. Hence, while the modest number of experience sampling studies conducted thus far suggests that there is an association between a number of potentially relevant psychological processes and psychotic experiences, the available evidence does not allow for any firm conclusions to be drawn as to whether there is a causal link between these psychological processes and the development of psychotic experiences.
Targeting Putative Psychological Mechanisms in Daily Life: An Ecological Interventionist Causal Model Approach
While to date there is no consensus on the precise definition of what constitutes a “cause” or “causation”, several criteria have been proposed by epidemiologists as guidelines for evaluating causal inferences.44 These criteria may be, as Schwartz and Susser44 have pointed out, of particular value in the planning stages of a study for evaluating the strength and consistency of the current evidence, based on all previous research44,45 (rather than for evaluating the results at the end of a single study). Consistent with Susser,46 their essential properties have been held to be: “association” (between putative mechanism and psychosis outcome; enhanced by strength and consistency), “time order” (ie, the putative mechanism precedes psychosis outcome), and “direction” (ie, a change in the putative mechanism leads to a change in the outcome),46 also referred to as “sole plausibility” (ie, elimination of any remaining plausible explanation for the association).44 While these key criteria explicitly acknowledge that causality cannot simply be operationalized as a binary concept (of presence or absence of causality) and primarily refer to (and may be best utilized for optimizing) the internal validity of a given study, it also needs to be established under what circumstances a putative causal mechanism has an effect on the outcome (external validity).
At the same time, recent years have seen calls for interventionist causal models for evaluating causal claims in psychiatry.47,48 Central to defining causation in these models is the question “...of what would happen under interventions” (Kendler and Campbell,47 p. 881), thereby taking the key practical interest of psychiatry into account, ie, to intervene, treat or prevent illness.47 Freeman48 has recently advocated an interventionist causal model approach for improving cognitive treatments for delusions. This approach adopts a strategy that: (i) targets one specific causal factor at a time; (ii) shows that an intervention can change it; and (iii) examines the subsequent effects on delusional beliefs.48
Real-time and real-world assessment (ie, ESM) and interventions (ie, ecological momentary interventions) may fundamentally contribute to and enhance such an interventionist causal model approach.
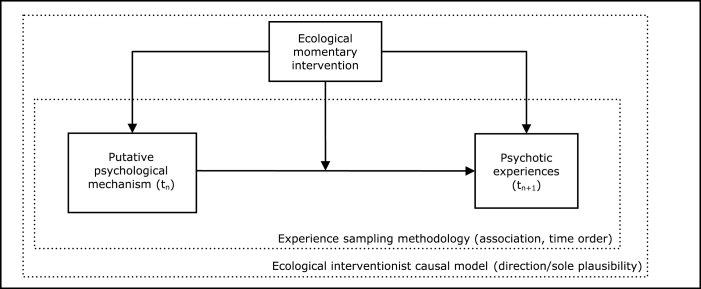
An essential first step in this approach is the assessment of the psychological mechanism and psychosis outcome, which we have already argued ESM can contribute to by capturing psychological processes in interaction with the proximal, microlevel environment. Second, drawing on the above causal criteria, it needs to be shown that the putative causal mechanism precedes the outcome of psychotic experiences (and not vice versa) in daily life for establishing time order (see figure 1). Intensive longitudinal assessments obtained in the real world with ESM are perfectly fit to capture and test this temporal order (using lagged analyses). However, this does still not rule out that there is an alternative explanation of the association between the putative mechanism and psychosis outcome, or, in other words, a common underlying factor that causes the putative mechanism on the one hand and psychotic experiences on the other (ie, evidence of direction or sole plausibility). Therefore, an ecological interventionist causal model approach moves beyond investigating temporal order in an observational design, by targeting the putative psychological mechanism to investigate whether changes in the psychological mechanisms ultimately result in changes in the symptoms they are supposed to be causing.
Fig. 1.
Targeting psychological mechanisms in daily life: an ecological interventionist causal model approach.
Leveraging the immense processing power of mobile devices, a variety of studies have utilized real-time data to scaffold targeted psychological interventions. As psychological mechanisms are dynamic processes affected by, and interacting with, the microlevel environment, the effectiveness of any intervention targeting mechanisms is likely to be greater if delivered in real life, outside the clinician’s office. These real-world and real-life interventions, now commonly referred to as ecological momentary interventions,14,49 may be particularly useful for testing causal criteria under real-world conditions. The ecological interventionist causal model approach thus targets the putative psychological mechanism in daily life to test whether an ecological momentary intervention can (i) modify this mechanism and (ii) produce changes in the mechanism that lead to changes in intended psychosis outcomes (ie, whether the effect of an ecological momentary intervention on psychotic symptoms is mediated via pathways through this mechanism)50 (see figure 1). Such interventions could be scalable given the ubiquity of mobile devices, and thus corresponds to calls for research that identifies mechanisms in clinical trials,51 provides the best evidence to relevant clinical problems of everyday practice,52 which is generalizable to both social contexts in the real world13,53–55 and heterogeneous patient populations across the transdiagnostic psychosis disorder spectrum,56,57 and informs the service user as well as clinician perspective.58–61
The benefits of such an ecological interventionist causal model approach are at least 2-fold. First of all, this approach allows for generating evidence on several causal criteria simultaneously, including association, time order, and direction/sole plausibility (all contributing to internal validity), while being explicitly pragmatic in nature, with the goal of optimizing generalizability of findings to both real-world contexts (outside the research laboratory) and heterogeneous populations, contributing to external validity. Second, it is translational in that it provides robust evidence whether the ecological momentary intervention is an effective treatment for reducing psychotic experiences in daily life.48 This approach will, thereby, contribute to ongoing efforts that seek to enhance effectiveness of psychological interventions under real-world conditions.52,56,62–64 A key distinction in intervention development is that ecological causal momentary interventions strive for sustainable change rather than compensation for deficits. For example, an intervention designed to promote medication adherence might deliver targeted reminders to accommodate for memory deficits, whereas an ecological causal interventionist approach would target the social-contextual factors and beliefs about medications that increase risk of poor adherence. The latter approach would theoretically generate more lasting changes in medication adherence behavior that limit the degree to which mobile interventions would be needed in perpetuity. Given that ecological momentary interventions for chronic illnesses, as with e-health approaches and in-person therapies, generally have diminishing engagement over time,65,66 targeting mechanisms that will generate sustained changes after cessation of engagement with the intervention maximizes the potential impact.
Testing Ecological Interventionist Causal Models in Psychotic Disorders
To date, ecological momentary interventions for psychosis spectrum disorders have been largely evaluated in uncontrolled “proof-of-concept” studies and mechanistic hypotheses have not been tested. Granholm et al67 evaluated a text-messaging approach to targeting maladaptive beliefs corresponding to 3 outcomes, socialization, medication adherence, and voices. Findings indicated changes in maladaptive beliefs (eg, perceptions of lack of control over voices) related to changes in outcomes (eg, perceived distress about voices).67 Ben-Zeev et al68 evaluated a smartphone-based system with similar targets, but with user-driven interaction. Further, Steinhart et al69 have developed and are currently evaluating the effectiveness of an ecological momentary intervention that targets elevated stress sensitivity, altered reward-experience, and psychological flexibility based on principles of acceptance and commitment therapy (ACT) in UHR individuals. This ongoing ACT in daily life study extends standard ACT therapy with real life training and exercises through a dedicated device (ie, the PsyMate®), thereby enhancing participants’ ACT-based skills and techniques. It remains to be demonstrated whether this approach indeed is effectively reducing symptoms through altering stress sensitivity, reward-experience, and psychological flexibility. Further highlighting the need for causal interventionist models, in one of only ecological momentary randomized controlled trials to include a follow up assessment, Depp et al39 evaluated an ecological momentary intervention that delivered real-time targeted coping strategies mapped to specific illness states. Although depressive symptoms declined substantially more in the ecological momentary intervention group compared to an active control group, this separation was minimal 3 months after intervention participation had stopped. One takeaway from this clinical trial was that perhaps intervention content focused on the psychological mechanisms that create vulnerabilities illnesses states (rather than adaptive means of managing those states) may have sustained the intervention impact consistent with the approach described in this article.
Conclusion and Future Prospects
Although putative psychological mechanisms that may contribute to the development or exacerbation of psychotic experiences have been investigated for decades, it is only recently that a modest amount of experience sampling research has provided evidence on their role in daily life, outside the research laboratory. A number of methodological challenges remain in validating psychological mechanistic theories in a systematic fashion, capitalizing on longitudinal data to test temporal ordering, and evaluating specificity of potential causal links between a given psychological mechanism and psychosis outcomes under real-world conditions. We have argued here for testing ecological interventionist causal models that allow for generating evidence on several causal criteria simultaneously (association, time order, and direction/sole plausibility), while maximizing generalizability to heterogeneous populations and social contexts. Future research using this approach will further provide translational evidence on the active ingredients of mobile health and in-person interventions that promote sustained effectiveness of ecological momentary interventions and, thereby, contribute to ongoing efforts that seek to enhance effectiveness of psychological interventions under real-world conditions.
Funding
Veni grant from the Netherlands Organisation for Scientific Research (451-13-022 to U.R.). National Institute of Mental Health (NIMH) (MH100417 to C.D.). ERC consolidator grant (ERC-2012-StG, project 309767 – INTERACT to I.M.-G.).
Acknowledgment
The authors have declared that there are no conflicts of interest in relation to the subject of this study.
References
- 1. Garety PA, Bebbington P, Fowler D, Freeman D, Kuipers E. Implications for neurobiological research of cognitive models of psychosis: a theoretical paper. Psychol Med. 2007;37:1377–1391. [DOI] [PubMed] [Google Scholar]
- 2. Howes OD, Murray RM. Schizophrenia: an integrated sociodevelopmental-cognitive model. Lancet. 2014;383:1677–1687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Morgan C, Charalambides M, Hutchinson G, Murray RM. Migration, ethnicity, and psychosis: toward a sociodevelopmental model. Schizophr Bull. 2010;36:655–664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Reininghaus U, Morgan C. Integrated models in psychiatry: the state of the art. Soc Psychiatry Psychiatr Epidemiol. 2014;49:1–2. [DOI] [PubMed] [Google Scholar]
- 5. Akdeniz C, Tost H, Meyer-Lindenberg A. The neurobiology of social environmental risk for schizophrenia: an evolving research field. Soc Psychiatry Psychiatr Epidemiol. 2014;49:507–517. [DOI] [PubMed] [Google Scholar]
- 6. Bentall RP, de Sousa P, Varese F, et al. From adversity to psychosis: pathways and mechanisms from specific adversities to specific symptoms. Soc Psychiatry Psychiatr Epidemiol. 2014;49:1011–1022. [DOI] [PubMed] [Google Scholar]
- 7. Freeman D, Garety P. Advances in understanding and treating persecutory delusions: a review. Soc Psychiatry Psychiatr Epidemiol. 2014;49:1179–1189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Morgan C, Reininghaus U, Fearon P, et al. Modelling the interplay between childhood and adult adversity in pathways to psychosis: initial evidence from the AESOP study. Psychol Med. 2014;44:407–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Pishva E, Kenis G, van den Hove D, et al. The epigenome and postnatal environmental influences in psychotic disorders. Soc Psychiatry Psychiatr Epidemiol. 2014;49:337–348. [DOI] [PubMed] [Google Scholar]
- 10. Reininghaus U, Craig TK, Fisher HL, et al. Ethnic identity, perceptions of disadvantage, and psychosis: findings from the AESOP study. Schizophr Res. 2010;124:43–48. [DOI] [PubMed] [Google Scholar]
- 11. Reininghaus U, Morgan C, Simpson J, et al. Unemployment, social isolation, achievement-expectation mismatch and psychosis: findings from the AESOP Study. Soc Psychiatry Psychiatr Epidemiol. 2008;43:743–751. [DOI] [PubMed] [Google Scholar]
- 12. Cannon TD, Keller MC. Endophenotypes in the genetic analyses of mental disorders. Annu Rev Clin Psychol. 2006;2:267–290. [DOI] [PubMed] [Google Scholar]
- 13. Myin-Germeys I, Oorschot M, Collip D, Lataster J, Delespaul P, van Os J. Experience sampling research in psychopathology: opening the black box of daily life. Psychol Med. 2009;39:1533–1547. [DOI] [PubMed] [Google Scholar]
- 14. Myin-Germeys I, Birchwood M, Kwapil T. From environment to therapy in psychosis: a real-world momentary assessment approach. Schizophr Bull. 2011;37:244–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annu Rev Clin Psychol. 2008;4:1–32. [DOI] [PubMed] [Google Scholar]
- 16. Moffitt TE, Caspi A, Rutter M. Strategy for investigating interactions between measured genes and measured environments. Arch Gen Psychiatry. 2005;62:473–481. [DOI] [PubMed] [Google Scholar]
- 17. Collip D, Nicolson NA, Lardinois M, Lataster T, van Os J, Myin-Germeys I; G.R.O.U.P Daily cortisol, stress reactivity and psychotic experiences in individuals at above average genetic risk for psychosis. Psychol Med. 2011;41:2305–2315. [DOI] [PubMed] [Google Scholar]
- 18. Lataster T, Wichers M, Jacobs N, et al. Does reactivity to stress cosegregate with subclinical psychosis? A general population twin study. Acta Psychiatr Scand. 2009;119:45–53. [DOI] [PubMed] [Google Scholar]
- 19. Myin-Germeys I, van Os J. Stress-reactivity in psychosis: evidence for an affective pathway to psychosis. Clin Psychol Rev. 2007;27:409–424. [DOI] [PubMed] [Google Scholar]
- 20. Myin-Germeys I, van Os J, Schwartz JE, Stone AA, Delespaul PA. Emotional reactivity to daily life stress in psychosis. Arch Gen Psychiatry. 2001;58:1137–1144. [DOI] [PubMed] [Google Scholar]
- 21. Oorschot M, Kwapil T, Delespaul P, Myin-Germeys I. Momentary assessment research in psychosis. Psychol Assess. 2009;21:498–505. [DOI] [PubMed] [Google Scholar]
- 22. Fusar-Poli P, Borgwardt S, Bechdolf A, et al. The psychosis high-risk state: a comprehensive state-of-the-art review. JAMA Psychiatry. 2013;70:107–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Yung AR, Yuen HP, McGorry PD, et al. Mapping the onset of psychosis: the Comprehensive Assessment of At-Risk Mental States. Aust N Z J Psychiatry. 2005;39:964–971. [DOI] [PubMed] [Google Scholar]
- 24. Palmier-Claus JE, Dunn G, Lewis SW. Emotional and symptomatic reactivity to stress in individuals at ultra-high risk of developing psychosis. Psychol Med. 2012;42:1003–1012. [DOI] [PubMed] [Google Scholar]
- 25. Reininghaus U, Kempton MJ, Valmaggia L, et al. Stress sensitivity, aberrant salience, and threat anticipation in early psychosis: an experience sampling study. Schizophr Bull. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lataster T, Collip D, Lardinois M, van Os J, Myin-Germeys I. Evidence for a familial correlation between increased reactivity to stress and positive psychotic symptoms. Acta Psychiatr Scand. 2010;122:395–404. [DOI] [PubMed] [Google Scholar]
- 27. Oorschot M, Lataster T, Thewissen V, et al. Emotional experience in negative symptoms of schizophrenia--no evidence for a generalized hedonic deficit. Schizophr Bull. 2013;39:217–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Brown LH, Silvia PJ, Myin-Germeys I, Kwapil TR. When the need to belong goes wrong: the expression of social anhedonia and social anxiety in daily life. Psychol Sci. 2007;18:778–782. [DOI] [PubMed] [Google Scholar]
- 29. Husky MM, Grondin OS, Swendsen JD. The relation between social behavior and negative affect in psychosis-prone individuals: an experience sampling investigation. Eur Psychiatry. 2004;19:1–7. [DOI] [PubMed] [Google Scholar]
- 30. Myin-Germeys I, Delespaul PA, deVries MW. Schizophrenia patients are more emotionally active than is assumed based on their behavior. Schizophr Bull. 2000;26:847–854. [DOI] [PubMed] [Google Scholar]
- 31. Gard DE, Kring AM, Gard MG, Horan WP, Green MF. Anhedonia in schizophrenia: distinctions between anticipatory and consummatory pleasure. Schizophr Res. 2007;93:253–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Gard DE, Sanchez AH, Cooper K, Fisher M, Garrett C, Vinogradov S. Do people with schizophrenia have difficulty anticipating pleasure, engaging in effortful behavior, or both? J Abnorm Psychol. 2014;123:771–782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Sanchez AH, Lavaysse LM, Starr JN, Gard DE. Daily life evidence of environment-incongruent emotion in schizophrenia. Psychiatry Res. 2014;220:89–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Palmier-Claus JE, Dunn G, Taylor H, Morrison AP, Lewis SW. Cognitive-self consciousness and metacognitive beliefs: Stress sensitization in individuals at ultra-high risk of developing psychosis. Br J Clin Psychol. 2013;52:26–41. [DOI] [PubMed] [Google Scholar]
- 35. Palmier-Claus JE, Dunn G, Morrison AP, Lewis SW. The role of metacognitive beliefs in stress sensitisation, self-esteem variability, and the generation of paranoia. Cogn Neuropsychiatry. 2011;16:530–546. [DOI] [PubMed] [Google Scholar]
- 36. Thewissen V, Bentall RP, Lecomte T, van Os J, Myin-Germeys I. Fluctuations in self-esteem and paranoia in the context of daily life. J Abnorm Psychol. 2008;117:143–153. [DOI] [PubMed] [Google Scholar]
- 37. Thewissen V, Bentall RP, Oorschot M, et al. Emotions, self-esteem, and paranoid episodes: an experience sampling study. Br J Clin Psychol. 2011;50:178–195. [DOI] [PubMed] [Google Scholar]
- 38. Lardinois M, Myin-Germeys I, Bak M, Mengelers R, van Os J, Delespaul PA. The dynamics of symptomatic and non-symptomatic coping with psychotic symptoms in the flow of daily life. Acta Psychiatr Scand. 2007;116:71–75. [DOI] [PubMed] [Google Scholar]
- 39. Depp CA, Ceglowski J, Wang VC, et al. Augmenting psychoeducation with a mobile intervention for bipolar disorder: a randomized controlled trial. J Affect Disord. 2015;174:23–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Depp CA, Stricker JL, Zagorsky D, et al. Disability and self-management practices of people with bipolar disorder: a web-based survey. Commun Ment Health J. 2009;45(3):179–187. [DOI] [PubMed] [Google Scholar]
- 41. Peters E, Lataster T, Greenwood K, et al. Appraisals, psychotic symptoms and affect in daily life. Psychol Med. 2012;42:1013–1023. [DOI] [PubMed] [Google Scholar]
- 42. Ben-Zeev D, Ellington K, Swendsen J, Granholm E. Examining a cognitive model of persecutory ideation in the daily life of people with schizophrenia: a computerized experience sampling study. Schizophr Bull. 2011;37:1248–1256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Ben-Zeev D, Morris S, Swendsen J, Granholm E. Predicting the occurrence, conviction, distress, and disruption of different delusional experiences in the daily life of people with schizophrenia. Schizophr Bull. 2012;38:826–837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Schwartz S, Susser E. Relationships among causes. In: Susser E, Schwartz S, Morabia A, Bromet E, eds. Psychiatric Epidemiology: Searching for Causes of Mental Disorders. Oxford, UK: Oxford University Press; 2006:62–74. [Google Scholar]
- 45. Maclure M. Popperian refutation in epidemiology. Am J Epidemiol. 1985;121:343–350. [DOI] [PubMed] [Google Scholar]
- 46. Susser M. What is a cause and how do we know one? A grammar for pragmatic epidemiology. Am J Epidemiol. 1991;133:635–648. [DOI] [PubMed] [Google Scholar]
- 47. Kendler KS, Campbell J. Interventionist causal models in psychiatry: repositioning the mind-body problem. Psychol Med. 2009;39:881–887. [DOI] [PubMed] [Google Scholar]
- 48. Freeman D. Improving cognitive treatments for delusions. Schizophr Res. 2011;132:135–139. [DOI] [PubMed] [Google Scholar]
- 49. Heron KE, Smyth JM. Ecological momentary interventions: incorporating mobile technology into psychosocial and health behaviour treatments. Br J Health Psychol. 2010;15:1–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Emsley R, Dunn G, White IR. Mediation and moderation of treatment effects in randomised controlled trials of complex interventions. Stat Methods Med Res. 2010;19:237–270. [DOI] [PubMed] [Google Scholar]
- 51. Insel TR, Gogtay N. National Institute of Mental Health clinical trials: new opportunities, new expectations. JAMA Psychiatry. 2014;71:745–746. [DOI] [PubMed] [Google Scholar]
- 52. Hotopf M, Churchill R, Lewis G. Pragmatic randomised controlled trials in psychiatry. Br J Psychiatry. 1999;175:217–223. [DOI] [PubMed] [Google Scholar]
- 53. Heinz A, Deserno L, Reininghaus U. Urbanicity, social adversity and psychosis. World Psychiatry. 2013;12:187–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Kirkbride JB, Jones PB. The prevention of schizophrenia–what can we learn from eco-epidemiology? Schizophr Bull. 2011;37:262–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. March D, Hatch SL, Morgan C, et al. Psychosis and place. Epidemiol Rev. 2008;30:84–100. [DOI] [PubMed] [Google Scholar]
- 56. Hotopf M. The pragmatic randomised controlled trial. Advances in Psychiatric Treatment. 2002;2002:326–333. [Google Scholar]
- 57. Reininghaus U, Böhnke J, Hosang G, et al. Probing the boundaries of the Kraepelinian dichotomy: Evidence for a transdiagnostic psychosis spectrum encompassing schizophrenia and bipolar disorder. Br J Psychiatry. In press. [DOI] [PubMed] [Google Scholar]
- 58. Lasalvia A, Bonetto C, Tansella M, Stefani B, Ruggeri M. Does staff-patient agreement on needs for care predict a better mental health outcome? A 4-year follow-up in a community service. Psychol Med. 2008;38:123–133. [DOI] [PubMed] [Google Scholar]
- 59. Reininghaus U, McCabe R, Slade M, Burns T, Croudace T, Priebe S. The validity of patient- and clinician-rated measures of needs and the therapeutic relationship in psychosis: a pooled analysis. Psychiatry Res. 2013;209:711–720. [DOI] [PubMed] [Google Scholar]
- 60. Reininghaus U, Priebe S. Measuring patient-reported outcomes in psychosis: conceptual and methodological review. Br J Psychiatry. 2012;201:262–267. [DOI] [PubMed] [Google Scholar]
- 61. Rose D, Thornicroft G, Slade M. Who decides what evidence is? Developing a multiple perspectives paradigm in mental health. Acta Psychiatr Scand Suppl. 2006:109–114. [DOI] [PubMed] [Google Scholar]
- 62. Birchwood M, Trower P. The future of cognitive-behavioural therapy for psychosis: not a quasi-neuroleptic. Br J Psychiatry. 2006;188:107–108. [DOI] [PubMed] [Google Scholar]
- 63. Garety PA, Fowler DG, Freeman D, Bebbington P, Dunn G, Kuipers E. Cognitive–behavioural therapy and family intervention for relapse prevention and symptom reduction in psychosis: randomised controlled trial. Br J Psychiatry. 2008;192:412–423. [DOI] [PubMed] [Google Scholar]
- 64. Wykes T. Cognitive-behaviour therapy and schizophrenia. Evid Based Ment Health. 2014;17:67–68. [DOI] [PubMed] [Google Scholar]
- 65. Tatara N, Arsand E, Skrøvseth SO, Hartvigsen G. Long-term engagement with a mobile self-management system for people with type 2 diabetes. JMIR Mhealth Uhealth. 2013;1:e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Wolin KY, Steinberg DM, Lane IB, et al. Engagement with eHealth self-monitoring in a primary care-based weight management intervention. PLoS One. 2015;10:e0140455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Granholm E, Ben-Zeev D, Link PC, Bradshaw KR, Holden JL. Mobile Assessment and Treatment for Schizophrenia (MATS): a pilot trial of an interactive text-messaging intervention for medication adherence, socialization, and auditory hallucinations. Schizophr Bull. 2012;38:414–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Ben-Zeev D, Brenner CJ, Begale M, Duffecy J, Mohr DC, Mueser KT. Feasibility, acceptability, and preliminary efficacy of a smartphone intervention for schizophrenia. Schizophr Bull. 2014;40:1244–1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Steinhart H, Vaessen T, Batink T, Myin-Germeys I. ACT in daily life: a momentary intervention approach. [Google Scholar]