Abstract
Background: Black and Hispanic older Americans are less likely than white older Americans to possess advance directives. Understanding the reasons for this racial and ethnic difference is necessary to identify targets for future interventions to improve advance care planning in these populations.
Methods: The aim of the study was to evaluate whether racial and ethnic differences in advance directive possession are explained by other demographic factors, religious characteristics, and personal health values. A general population survey was conducted in a nationally representative sample using a web-enabled survey panel of American adults aged 50 and older (n = 2154).
Results: In a sample of older Americans, white participants are significantly more likely to possess advance directives (44.0%) than black older Americans (24.0%, p < 0.001) and Hispanic older Americans (29.0%, p = 0.006). Gender, age, retired or disabled employment status, educational attainment, religious affiliation, Internet access, preferences for physician-centered decision making, and desiring longevity regardless of functional status were independent predictors of advance directive possession. In fully adjusted multivariable models with all predictors included, black older Americans remained significantly less likely than white older Americans to have an advance directive (odds ratio [OR] = 0.42, 95% confidence interval [CI] = 0.24–0.75), whereas the effect of Hispanic ethnicity was no longer statistically significant (OR = 0.65, 95% CI = 0.39–1.1).
Conclusion: In a nationally representative sample, black race is an independent predictor for advance directive possession. This association remains even after adjustment for other demographic variables, religious characteristics, and personal health values. These findings support targeted efforts to mitigate racial disparities in access to advance care planning.
Introduction
Arecent Institute of Medicine (IOM) report on care near the end of life indicates that many older adults continue to receive costly and low-quality care that may be inconsistent with their preferences, in large part due to inadequate advance care planning and patient-provider communication.1 These burdens may be disproportionately borne by members of underserved groups. As one example, black and Hispanic Americans are less likely than white Americans to have healthcare advance directives.2–7As advance directives can be important tools for protecting patient autonomy and reducing distress among surrogate decision-makers,1,8 these racial and ethnic differences may represent important disparities in quality health care at the end of life.
However, the causes of these racial and ethnic differences are poorly understood, and therefore potential targets for interventions to improve advance care planning in these populations are not well characterized. Although some have suggested that black and Hispanic Americans lack sufficient access to and education about advance care planning,7,9 an alternative hypothesis is that these differences in advance directive possession do not indicate racial and ethnic disparities, but instead reflect cultural differences. On this alternative hypothesis, race and ethnicity are merely proxies for cultural beliefs and religious values that influence individuals' willingness to undertake advance care planning.10,11 In support of this hypothesis, black and Hispanic Americans are more likely than white Americans to say religion is very important in their lives6,10 and black Americans are more likely to endorse the statement that their health outcomes are determined by God.12,13 Furthermore, whereas advance directives are often used to limit life-sustaining treatment, black and Hispanic Americans are more likely to desire life-sustaining treatment despite poor prognosis.6,14,15
Recent investigators examining associations among race/ethnicity, cultural values, and advance directive possession in non-representative convenience samples have reached conflicting conclusions6,10,11; to date, these relationships have not been evaluated in large, demographically representative samples. In this study, we investigated whether racial and ethnic differences in advance directive possession are explained by other demographic factors, religious characteristics, and personal health values, using a nationally representative sample of older U.S. adults. We constructed five logistic regression models with advance directive possession as the dependent variable to examine how alternative predictors influence the effect of race and ethnicity on advance directive possession.
Methods
Study design and participants
In this study, we used data from a broader panel-design study of medical treatment preferences, which has been previously described.16,17 Data were collected on the Time-Sharing Experiments in the Social Sciences platform, using the web-enabled GfK KnowledgePanel, a probability-based panel designed to field responses from a nationally representative U.S. sample.18 Before 2009, households were selected for this panel using random-digit dialing based on a sample frame of U.S. residential landline telephone service; after 2009, a residential address-based sampling frame was used to account for mobile phone-only households. Demographic and household variables were assessed by self-report before participants became eligible for sampling. Households that were selected for the panel but lacked Internet access were provided with a computer and Internet connection. Between February 19 and March 3, 2013, 3418 online questionnaires were fielded to U.S. adults aged 50 years and older; all questionnaires were in English. The institutional review board at the University of California, San Francisco approved this study. Participants provided informed consent before they were presented with the study instrument.
Measures
The primary outcome of interest was whether participants had an advance directive, assessed using the question, “Do you have an advance directive (‘living will’) that documents your treatment preferences in case you have a medical problem that makes you unable to communicate with your doctors and family?” Participants' demographic characteristics, religious affiliation, and frequency of religious attendance were obtained from previous KnowledgePanel surveys. Personal health values on whether the participant relies solely upon their doctor's knowledge, prefers patient-centered decision making, prefers physician-centered decision making,19 fears becoming dependent on others for daily needs, desires longevity regardless of poor health,20 and is confident in receiving good care were elicited using a 6-point Likert-type scale ranging from “strongly agree” to “strongly disagree.” Responses were dichotomized to agree/disagree for analysis.
Statistical analysis
Racial and ethnic group differences in population characteristics were assessed using the Pearson's chi-squared test of independence. Demographic predictors were selected on the basis of earlier literature on advance directive possession6,7,10; income was excluded from multivariable models to avoid multicollinearity with education and employment status, particularly as income is a problematic proxy for wealth or socioeconomic status in older adults due to retirement and other sources of variability in income. Religious affiliations were collapsed into more inclusive categories to avoid model estimation errors due to small cell counts, yielding: mainline Protestant (including Methodist, Lutheran, Presbyterian, and Episcopal), Catholic, Evangelical (including Baptist and Pentecostal), other Christian (including Mormon and Eastern Orthodox), other non-Christian (including Jewish, Muslim, Hindu, and Buddhist), and None. Single variable and multivariable odds ratios (ORs) were calculated using logistic regression to examine whether demographic factors, religious characteristics, and personal health values predict advance directive possession both independently and with all predictors included.
We estimated the separate influences of other demographic factors, religious characteristics, and personal health values on the relationship between race/ethnicity and the use of advance directives by constructing five logistic regression models with advance directive possession as the dependent variable. The first model was a single variable base model to estimate the overall effect of race/ethnicity on advance directive possession. The next three multivariable models estimated the separate influence of adding each class of alternative predictors to the single variable (race/ethnicity) base model. The first of these models included other demographic variables (excluding income as described above); the second included religious affiliation and frequency of religious attendance; and the third included personal health values, in addition to race/ethnicity. Finally, we constructed a final multivariable model including all of the independent variables from the preceding models: race/ethnicity, other demographic factors, religious affiliation and attendance, and personal health values.
Questionnaire responses were weighted to match the U.S. population aged 50 years and older based on the United States Current Population Survey, using a three-step strategy to offset known selection deviations in panel recruitment, other sources of sampling error due to recruitment methods and panel attrition, and study-specific factors such as non-response and undersampling or oversampling resulting from the study-specific sample design. All statistical analyses were conducted using Stata 12.1 software (StataCorp., College Station, TX); a two-tailed p value of <0.05 was considered significant.
Results
Study population characteristics
Of 3418 questionnaires, 2154 (63.0%) were completed. Population characteristics were compared among black, Hispanic, and white older Americans (Table 1).
Table 1.
Sample Characteristics of White, Black, and Hispanic Americans Age ≥50 Yearsa
| White older Americans(n = 1702) | Black older Americans(n = 201) | Hispanic older Americans(n = 136) | P valueBlack versus white | P valueHispanic versus white | |
|---|---|---|---|---|---|
| Has health care advance directive, % (No.) | 44.0 (758) | 24.0 (48) | 29.0 (30) | <0.001 | 0.006 |
| Female gender, % (No.) | 51.5 (882) | 65.3 (123) | 53.5 (74) | 0.003 | 0.72 |
| Age, % (No.) | 0.009 | 0.007 | |||
| 50–59 years | 38.6 (707) | 48.8 (96) | 56.4 (72) | ||
| 60–69 years | 31.3 (581) | 35.5 (79) | 26.7 (49) | ||
| 70–79 years | 22.6 (327) | 14.3 (24) | 14.8 (13) | ||
| ≥80 years | 7.5 (87) | 1.4 (2) | 2.1 (2) | ||
| Marital status, % (No.) | <0.001 | 0.15 | |||
| Married | 62.5 (1,147) | 37.0 (74) | 53.4 (80) | ||
| Widowed | 9.9 (137) | 14.1 (24) | 6.6 (8) | ||
| Divorced | 14.1 (224) | 20.0 (49) | 19.3 (23) | ||
| Never married | 8.3 (113) | 16.5 (33) | 10.7 (14) | ||
| Other | 5.3 (81) | 12.4 (21) | 10.0 (11) | ||
| Annual household income, % (No.) | <0.001 | 0.22 | |||
| <$25,000 | 20.0 (273) | 36.6 (62) | 19.6 (28) | ||
| $25,000–$49,999 | 24.6 (399) | 25.3 (55) | 22.8 (32) | ||
| $50,000–$74,999 | 18.2 (342) | 14.4 (55) | 19.9 (30) | ||
| $75,000–$99,999 | 14.6 (241) | 11.8 (19) | 19.3 (24) | ||
| $100,000–$124,999 | 10.6 (199) | 5.6 (13) | 3.3 (5) | ||
| ≥ $125,000 | 11.9 (248) | 6.2 (14) | 15.0 (17) | ||
| Employment status, % (No.) | <0.001 | 0.11 | |||
| Employed | 41.0 (762) | 33.9 (75) | 40.5 (58) | ||
| Retired | 42.9 (674) | 34.3 (72) | 34.5 (44) | ||
| Disabled | 6.6 (113) | 24.0 (38) | 12.1 (17) | ||
| Other unemployed | 9.5 (153) | 7.8 (16) | 12.3 (17) | ||
| Highest educational attainment, % (No.) | 0.02 | 0.01 | |||
| Less than high school | 10.3 (111) | 16.5 (22) | 19.7 (20) | ||
| Completed high school | 35.1 (561) | 37.3 (68) | 22.3 (37) | ||
| Some college | 25.4 (470) | 28.7 (65) | 29.9 (39) | ||
| Bachelor's degree or higher | 29.2 (560) | 17.4 (46) | 28.1 (40) | ||
| Census region, % (No.) | <0.001 | <0.001 | |||
| Northeast | 21.1 (363) | 13.9 (30) | 8.9 (12) | ||
| Midwest | 24.1 (448) | 18.1 (46) | 14.3 (16) | ||
| South | 34.6 (558) | 56.5 (105) | 35.2 (54) | ||
| West | 20.1 (333) | 11.5 (20) | 41.6 (54) | ||
| Resides in metropolitan area, % (No.) | 78.9 (1,367) | 89.3 (187) | 95.2 (128) | 0.01 | <0.001 |
| Has Internet access, % (No.) | 70.4 (1,398) | 46.6 (119) | 78.0 (109) | <0.001 | 0.13 |
| Overall physical health, % (No.) | 0.10 | 0.45 | |||
| Excellent | 7.3 (136) | 9.3 (13) | 10.4 (11) | ||
| Very Good | 38.1 (682) | 27.0 (56) | 32.0 (45) | ||
| Good | 37.0 (596) | 38.0 (76) | 37.8 (50) | ||
| Fair | 15.2 (235) | 23.0 (50) | 18.7 (25) | ||
| Poor | 2.5 (35) | 2.7 (3) | 1.2 (2) | ||
| Religious attendance, % (No.) | <0.001 | 0.02 | |||
| More than once a week | 10.1 (180) | 31.7 (57) | 13.2 (13) | ||
| Once a week | 26.0 (444) | 27.3 (59) | 19.8 (17) | ||
| Once or twice a month | 7.1 (137) | 12.3 (20) | 13.0 (17) | ||
| A few times a year | 16.4 (277) | 12.4 (26) | 24.0 (37) | ||
| Once a year or less | 18.8 (308) | 10.0 (21) | 19.9 (26) | ||
| Never | 21.6 (355) | 6.4 (15) | 10.2 (14) | ||
| Religious denominationb | <0.001 | <0.001 | |||
| Mainline Protestant | 31.0 (522) | 7.0 (21) | 7.5 (11) | ||
| Catholic | 27.0 (441) | 7.3 (14) | 50.3 (75) | ||
| Evangelical | 14.1 (241) | 57.6 (107) | 17.5 (19) | ||
| Other Christian | 11.9 (196) | 17.0 (34) | 13.1 (18) | ||
| Other non-Christian | 4.1 (84) | 6.2 (11) | 4.3 (5) | ||
| None | 12.0 (215) | 4.9 (11) | 7.2 (8) | ||
| Health attitudes, % (No.) | |||||
| I prefer to rely upon my doctor's knowledge and not try to find out about my condition on my own. | 61.1 (970) | 63.9 (126) | 68.6 (91) | 0.53 | 0.15 |
| I prefer that my doctor offers me choices and asks my opinion. | 94.5 (1,600) | 90.4 (180) | 92.6 (122) | 0.08 | 0.48 |
| I prefer to leave the decisions about my medical care up to my doctor. | 57.8 (919) | 58.6 (108) | 66.1 (86) | 0.86 | 0.11 |
| I am afraid of becoming dependent on my family or a nursing home for my daily needs. | 74.6 (1,286) | 71.4 (136) | 81.9 (113) | 0.43 | 0.13 |
| I would like to live a long life, regardless of how healthy or independent I am. | 50.4 (784) | 67.7 (131) | 64.5 (82) | <0.001 | 0.01 |
| When I go to a hospital or doctor's office, I am confident that I will receive good care. | 85.1 (1,420) | 81.8 (164) | 85.1 (109) | 0.33 | 0.99 |
Reported percentages are weighted to represent the total population of U.S. adults age ≥50 years on the basis of the United States Current Population Survey.
Religious denominations were collapsed into more inclusive categories for comparison. Evangelical denominations include Baptist and Pentecostal. Mainline Protestant denominations include Methodist, Lutheran, Presbyterian, and Episcopal. Other Christian denominations include Orthodox and Mormon, whereas non-Christian denominations include Jewish, Muslim, Hindu, and Buddhist.
Overall, 40.6% of Americans aged 50 and older reported having an advance directive. In population-weighted analyses, black older Americans were significantly less likely to have advance directives (24.0%) than white older Americans (44.0%, p < 0.001); as were Hispanic older Americans (29.0%, p = 0.006; Tables 1 and 2). Marked demographic differences were observed among racial/ethnic groups in the study population, including gender, age, marital status, income, employment status, education, census region, residence in a metropolitan area, and Internet access. Black older Americans attended religious services more frequently than white older Americans and were more likely to declare Evangelical religious affiliation, whereas Hispanic older Americans were more likely to declare Catholic religious affiliation. Both black and Hispanic older Americans were more likely than white older Americans to desire longevity regardless of functional status.
Table 2.
Demographic Factors, Religious Affiliation, and Personal Health Values as Predictors of Advance Directive Possession
| Predictor | Single variable OR (95% CI) | Final multivariable model OR (95% CI) |
|---|---|---|
| Race or ethnicity | ||
| White, non-Hispanic (ref) | – | – |
| Black, non-Hispanic | 0.40 (0.27–0.61) | 0.43 (0.24–0.76) |
| Other, non-Hispanic | 0.87 (0.44–1.7) | 0.98 (0.46–2.1) |
| Hispanic | 0.51 (0.31–0.83) | 0.70 (0.42–1.2) |
| Mixed, non-Hispanic | 0.95 (0.48–1.9) | 1.0 (0.48–2.2) |
| Gender | ||
| Male (ref) | – | – |
| Female | 1.2 (1.0–1.6) | 1.4 (1.1–1.8) |
| Age (per decade) | 2.0 (1.8–2.3) | 1.6 (1.4–2.0) |
| Marital status | ||
| Married (ref) | – | – |
| Widowed | 2.1 (1.4–3.1) | 1.6 (0.98–2.5) |
| Divorced | 0.78 (0.57–1.1) | 1.1 (0.75–1.6) |
| Never married | 0.43 (0.28–0.66) | 0.72 (0.45–1.2) |
| Other | 0.62 (0.37–1.0) | 1.1 (0.60–1.9) |
| Annual household income | ||
| < $25,000 (ref) | – | –a |
| $25,000–49,999 | 1.4 (0.98–2.0) | |
| $50,000–74,999 | 1.6 (1.1–2.4) | |
| $75,000–99,999 | 1.4 (0.98–2.1) | |
| $100,000–124,999 | 1.6 (1.1–2.5) | |
| ≥ $125,000 | 1.5 (1.0–2.3) | |
| Employment status | ||
| Employed (ref) | – | – |
| Retired | 3.4 (2.7–4.4) | 2.1 (1.5–2.9) |
| Disabled | 1.2 (0.75–1.8) | 1.9 (1.2–3.2) |
| Other unemployed | 0.89 (0.57–1.4) | 0.86 (0.53–1.4) |
| Highest educational attainment | ||
| Less than high school | 0.77 (0.49–1.2) | 0.63 (0.36–1.1) |
| High school (ref) | – | – |
| Some college | 1.3 (0.99–1.7) | 1.7 (1.2–2.3) |
| Bachelor's or higher | 2.0 (1.5–2.6) | 2.2 (1.6–3.0) |
| Census region | ||
| Northeast | 0.77 (0.57–1.1) | 0.81 (0.56–1.2) |
| Midwest | 0.75 (0.56–1.0) | 0.77 (0.56–1.1) |
| South (ref) | – | – |
| West | 1.0 (0.76–1.4) | 0.90 (0.64–1.3) |
| Resides in metropolitan area | 1.0 (0.75–1.3) | 1.1 (0.76–1.5) |
| Has Internet access | 1.4 (1.1–1.8) | 1.6 (1.1–2.2) |
| Fair or poor physical health | 0.84 (0.63–1.1) | 1.1 (0.78–1.5) |
| Religious attendance | ||
| More than once a week | 1.2 (0.80–1.7) | 1.1 (0.73–1.7) |
| Once a week (ref) | – | – |
| Once or twice a month | 0.84 (0.54–1.3) | 1.1 (0.68–1.9) |
| A few times a year | 0.97 (0.69–1.4) | 1.1 (0.74–1.6) |
| Once a year or less | 0.69 (0.49–0.97) | 0.71 (0.49–1.0) |
| Never | 0.96 (0.69–1.3) | 1.1 (0.68–1.6) |
| Religious denomination | ||
| Mainline Protestant (ref) | – | – |
| Evangelical | 0.38 (0.27–0.53) | 0.50 (0.32–.0.76) |
| Catholic | 0.43 (0.32–0.58) | 0.54 (0.39–0.75) |
| Other Christian | 0.60 (0.41–0.87) | 0.91 (0.60–1.4) |
| Non-Christian | 0.96 (0.57–1.6) | 1.2 (0.66–2.2) |
| None | 0.67 (0.46–0.97) | 0.82 (0.51–1.3) |
| Prefers to rely on doctor's knowledge | 0.77 (0.61–0.96) | 1.0 (0.74–1.4) |
| Prefers to be offered choices and asked opinion | 0.68 (0.43–1.1) | 0.66 (0.39–1.1) |
| Prefers to leave medical care decisions up to the doctor | 0.77 (0.62–0.96) | 0.79 (0.59–1.1) |
| Fears dependence on family or nursing home | 0.97 (0.75–1.3) | 0.86 (0.65–1.1) |
| Desires longevity regardless of health and independence | 0.58 (0.47–0.73) | 0.65 (0.51–0.84) |
| Confident in receiving good care | 0.81 (0.60–1.1) | 1.1 (0.79–1.7) |
Income was excluded from the final multivariable model to avoid multicollinearity with highest educational attainment and employment status.
CI, confidence interval; OR, odds ratio.
Influence of race and ethnicity on advance directive possession
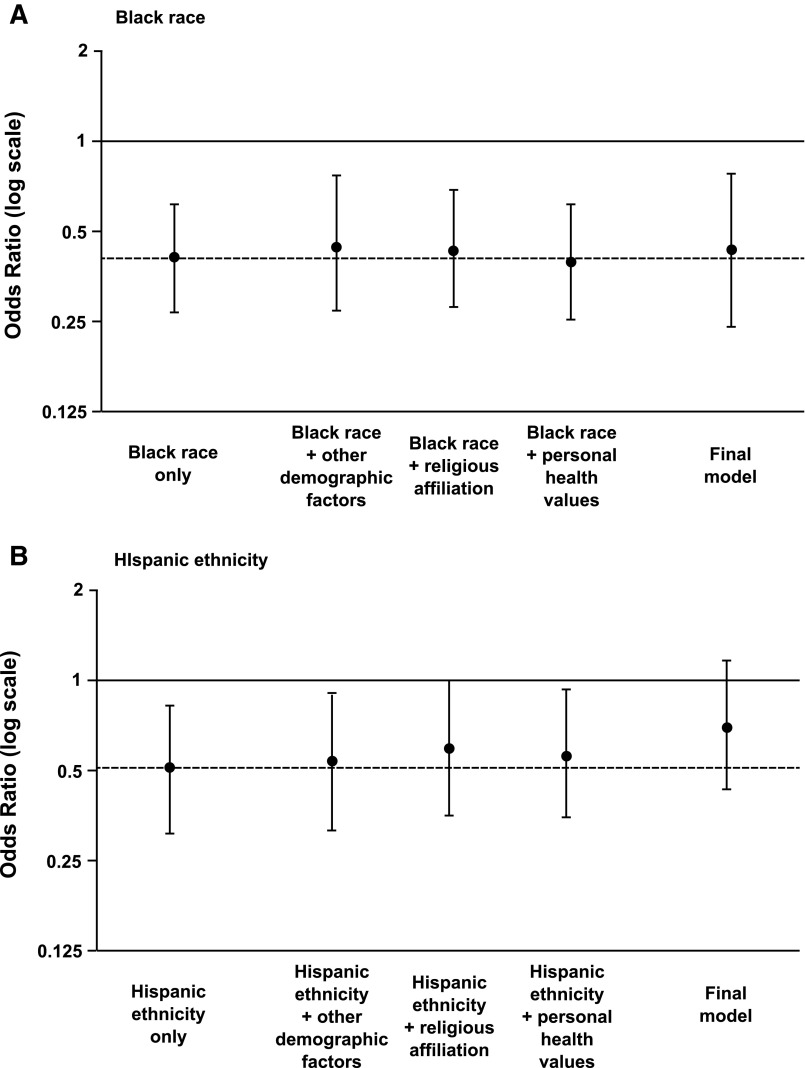
In the base single variable logistic regression model, the association of black race with advance directive possession was statistically significant (OR = 0.40, 95% confidence interval [CI] = 0.27–0.61). In a series of multivariable logistic regression models, this association was only modestly influenced by the introduction of other demographic variables (OR = 0.45, 95% CI = 0.27–0.75), religious characteristics (OR = 0.43, 95% CI = 0.28–0.68), or personal health values (OR = 0.40, 95% CI = 0.26–0.62). In a final multivariable logistic regression model including all of these predictors, the association of black race with advance directive possession remained significant (OR = 0.43, 95% CI = 0.24–0.76; Fig. 1A).
FIG. 1.
The influence of (A) black race and (B) Hispanic ethnicity on advance directive possession in adjusted and unadjusted models.
In the base single variable logistic regression model, the association of Hispanic ethnicity with possession of an advance directive was also statistically significant (OR = 0.51, 95% CI = 0.31–0.83). This association was modestly diminished by the introduction of other demographic variables (OR = 0.54, 95% CI = 0.33–0.90), as well as by religious characteristics (OR = 0.60, 95% CI = 0.36–1.0) and personal health values (OR = 0.57, 95% CI = 0.35–0.93), and the influence of these alternative predictors was more pronounced than in the case of black race. In a final multivariable logistic regression model including all of these predictors, the association of Hispanic ethnicity with advance directive possession was no longer statistically significant (OR = 0.70, 95% CI = 0.42–1.2; Fig. 1B).
Other factors predicting advance directive completion
Our final multivariable model revealed other demographic variables, religious characteristics, and personal health values that are independently associated with possession of an advance directive (Table 2). In particular, increasing age (OR = 1.6, 95% CI = 1.4–2.0), retired or disabled employment status (OR = 2.1, 95% CI = 1.5–2.9; OR = 1.9, 95% CI = 1.2–3.2), and receiving a bachelor's degree or higher as educational attainment (OR = 2.2, 95% CI = 1.6–3.0) were demographic variables with associations with advance directive possession comparable to those of race and ethnicity. Internet access was also associated with advance directive possession (OR = 1.6, 95% CI = 1.1–2.2). Evangelical and Catholic religious affiliation were negatively associated with advance directive possession (OR = 0.50, 95% CI = 0.32–0.76; OR = 0.54, 95% CI = 0.39–0.75), whereas frequency of religious attendance was not associated with advance directive possession. Finally, among the personal health values that we elicited, only a desire for longevity regardless of health and independence was independently associated with possession of advance directives (OR = 0.65, 95% CI = 0.51–0.84).
Discussion
These findings within a nationally representative sample indicate that black race is an independent predictor of advance directive possession rather than a mere proxy for religious and cultural factors that influence advance care planning, whereas the influence of Hispanic ethnicity on advance directive possession may be explained by these alternative predictors. Racial differences in advance directive possession between black and white older Americans remained statistically significant after adjustment for other demographic factors, religious characteristics, and personal health values in a multivariable model. In fact, the point estimate for the effect of black race was only minimally affected by the inclusion of all of these predictors in the final model. After adjustment for these alternative predictors, differences in advance directive possession between Hispanic and white older Americans were no longer statistically significant. However, as the final model point estimate for the effect of Hispanic ethnicity remained low with a confidence interval just including unity, it is plausible that a study with a larger sample size would find persisting ethnic differences in advance directive possession after adjustment.
Our overall findings are concordant with two recent studies of advance directive possession in large representative samples of older Americans.2,21 The prevalence of advance directive possession in this study is comparable to that observed in these two studies, and in all three studies female gender, increasing age, and educational attainment are positively associated with advance directive possession. Our specific findings on the relationships between race/ethnicity, culture, and advance directive possession conflict with earlier reports from less demographically representative samples. Johnson and colleagues have reported that racial differences in advance directive possession are no longer significant after adjustment for cultural beliefs and values, sampling 205 older adults recruited from one university health center; Ko and Lee have reported that Latino-white differences in advance directive possession are explained by differences in knowledge, sampling 256 older adults from the same urban area.10,11 Carr reported that black-white differences in advance directive possession are limited to those of low socioeconomic status, although this national sample of 2111 adults was limited to those in stable romantic partnerships (potentially screening for high socioeconomic status and more conservative cultural values).22
In our study, participants who reported Catholic and Evangelical religious affiliations were less likely than mainline Protestants to have advance directives, even after adjusting for personal health values. Members of these religious communities may have other established plans for advance care that preclude needing advance directives, or may perceive that advance directive possession is inconsistent with their religious beliefs. Along these lines, Garrido and colleagues have reported that conservative Protestants, including Baptists and other Evangelicals, were most likely to report that religious beliefs would influence their medical decisions and to endorse the claim that the length of one's life is determined by God.23
In addition, we identified other factors that independently predict advance directive possession. The effects of retirement and disability on advance directive possession are as strong as that of black race, suggesting that employment transitions prompt many older adults to complete advance directives as part of comprehensive estate or disability planning. Such employment transitions may be useful targets for promoting advance care planning in underserved groups. We also found that Internet access is independently associated with advance directive possession even after adjustment for income and educational attainment, suggesting an effect of current access to information.
To our knowledge, this is the first study designed to examine cultural explanations for racial and ethnic differences in advance directive possession in a nationally representative sample of older Americans. We also recognize several limitations. In particular, all surveys were conducted in English, which suggests further caution in interpreting our findings about Hispanic older Americans. Although our national sample is demographically representative, it may not be culturally representative of Spanish-only-speaking Hispanic Americans. Also, our sample did not include enough respondents of Asian-American or mixed race to allow for analyses of these populations. Our study outcome of interest was the possession of an advance directive, although we recognize that other elements of advance care planning (such as having conversations with one's primary physician and family, or designating a surrogate) may be of equal or greater clinical importance. The web-based testing platform limited our ability to qualitatively explore individual participants' rationales for either having or not having advance directives. In addition, some other alternative predictors of interest could not be examined, such as access to information on advance directives,7,9,11 the quality of the patient-provider relationship,1,4,24,25 and health literacy (as distinct from educational attainment).26,27
In summary, low adoption of advance directives among black older Americans (as compared with white older Americans) is not explained by other demographic factors, religious characteristics, or personal health values. As a matter of policy, these findings support targeted efforts and reimbursement models to promote advance care planning among members of underserved groups, as an individual's religious beliefs and personal health values do not fully explain the racial difference in advance directive possession. Additional findings suggest that employment transitions and access to information (such as through the Internet) may be promising targets for promoting advance care planning and, ultimately, closer adherence to older adults' wishes near the end of life. In clinical practice, these findings suggest that clinicians should not assume that black and Hispanic older Americans will be culturally unreceptive to advance care planning, although more work remains to be done to identify culturally appropriate methods for promoting such planning.
Acknowledgments
The authors gratefully recognize the contributions of Sarah Hooper, Laura Koehn, Rebecca Brown, Caroline Stephens, and the UCSF Health Disparities Research Symposium. Funding was provided by the National Institute on Aging (K23AG043553), National Center for Advancing Translational Sciences (KL2TR000143), and the American Brain Foundation Clinical Research Training Fellowship Program.
Data collection was provided by Time-sharing Experiments in the Social Sciences, NSF Grant 0818839, Jeremy Freese, PhD, and James Druckman, PhD, principal investigators. Sponsors had no role in the study concept, design, analysis, interpretation, and conclusions of the study, nor preparation and editing of the manuscript.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Dying in America: Improving Quality and Honoring Individual Preferences Near the End of Life. Institute of Medicine Committee on Approaching Death: Addressing Key End of Life Issues, 2014. (online). www.iom.edu/Reports/2014/Dying-In-America-Improving-Quality-and-Honoring-Individual-Preferences-Near-the-End-of-Life.aspx (Last accessed November5, 2014)
- 2.Rao JK, Anderson LA, Lin F, et al. : Completion of advance directives among U.S. consumers. Am J Prev Med 2014;46:65–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Silveira MJ, Wiitala W, Piette P: Advance directive completion by elderly Americans: A decade of change. J Am Geriatr Soc 2014;62:706–710 [DOI] [PubMed] [Google Scholar]
- 4.Teno JM, Gruneir A, Schwartz Z, et al. : Association between advance directives and quality of end-of-life care: A national study. J Am Geriatr Soc 2007;55:189–194 [DOI] [PubMed] [Google Scholar]
- 5.Frahm KA, Brown LM, Hyer K: Racial disparities in receipt of hospice services among nursing home residents. Am J Hosp Palliat Care 2015;32:233–237 [DOI] [PubMed] [Google Scholar]
- 6.Smith AK, McCarthy EP, Paulk E, et al. : Racial and ethnic differences in advance care planning among patients with cancer: Impact of terminal illness acknowledgment, religiousness, and treatment preferences. J Clin Oncol 2008;26:4131–4137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kwak J, Haley WE: Current research findings on end-of-life decision making among racially or ethnically diverse groups. Gerontologist 2005;45:634–641 [DOI] [PubMed] [Google Scholar]
- 8.Hickman RL, Jr, Pinto MD: Advance directives lessen the decisional burden of surrogate decision-making for the chronically critically ill. J Clin Nurs 2014;23:756–765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.West SK, Hollis M: Barriers to completion of advance care directives among African Americans ages 25–84: A cross-generational study. Omega (Westport) 2012;65:125–137 [DOI] [PubMed] [Google Scholar]
- 10.Johnson KS, Kuchibhatla M, Tulsky JA: What explains racial differences in the use of advance directives and attitudes toward hospice care? J Am Geriatr Soc 2008;56:1953–1958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ko E, Lee J: Completion of advance directives among low-income older adults: Does race/ethnicity matter? Am J Hosp Palliat Care 2014;31:247–253 [DOI] [PubMed] [Google Scholar]
- 12.Jonnalagadda S, Lin JJ, Nelson JE, et al. : Racial and ethnic differences in beliefs about lung cancer care. Chest 2012;142: 1251–1258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bergamo C, Lin JJ, Smith C, et al. : Evaluating beliefs associated with late-stage lung cancer presentation in minorities. J Thorac Oncol 2013;8:12–18 [DOI] [PubMed] [Google Scholar]
- 14.Barnato AE, Anthony DL, Skinner J, et al. : Racial and ethnic differences in preferences for end-of-life treatment. J Gen Intern Med 2009;24:695–701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Raghavan M, Smith AK, Arnold RM: African Americans and end-of-life care #204. J Palliat Med 2010;13:1382–1383 [DOI] [PubMed] [Google Scholar]
- 16.Chiong W, Kim AS, Huang IA, et al. : Testing the presumption of consent to emergency treatment for acute ischemic stroke. JAMA 2014;311:1689–1691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chiong W, Kim AS, Huang IA, et al. : Inability to consent does not diminish the desirability of stroke thrombolysis. Ann Neurol 2014;76:296–304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Callegaro M, DiSogra C: Computing response metrics for online panels. Public Opin Q 2008;7:1008–1032 [Google Scholar]
- 19.Levinson W, Kao A, Kuby A, Thisted RA: Not all patients want to participate in decision making. J Gen Intern Med 2005;20:531–535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Slot KB, Berge E: Thrombolytic treatment for stroke: patient preferences for treatment, information, and involvement. J Stroke Cerebrovasc Dis 2009;18:17–22 [DOI] [PubMed] [Google Scholar]
- 21.Pollack KM, Morhaim D, Williams MA: The public's perspectives on advance directives: Implications for state legislative and regulatory policy. Health Policy 2010;96:57–63 [DOI] [PubMed] [Google Scholar]
- 22.Carr D: Racial and ethnic differences in advance care planning: Identifying subgroup patterns and obstacles. J Aging Health 2012;24:923–947 [DOI] [PubMed] [Google Scholar]
- 23.Garrido MM, Idler EL, Leventhal H, et al. : Pathways from religious to advance care planning: Beliefs about control over length of life and end-of-life values. Gerontologist 2013;53:801–816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Piamjariyakul U, Myers S, Werkowitch M, et al. : End-of-life preferences and presence of advance directives among ethnic populations with severe chronic cardiovascular illnesses. Eur J Cardiovasc Nurs 2014;13:185–189 [DOI] [PubMed] [Google Scholar]
- 25.Smith AK, Davis RB, Krakauer EL: Differences in the quality of the patient-physician relationship among terminally ill African-American and white patients: Impact on advance care planning and treatment preferences. J Gen Intern Med 2007;22:1579–1582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sudore RL, Landefeld CS, Barnes DE, et al. : An advance directive redesigned to meet the literacy level of most adults: A randomized trial. Patient Educ Couns 2007;69:165–195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Waite KR, Federman AD, McCarthy DM, et al. : Literacy and race as risk factors for low rates of advance directives in older adults. J Am Geriatr Soc 2013;61:403–406 [DOI] [PMC free article] [PubMed] [Google Scholar]