Abstract
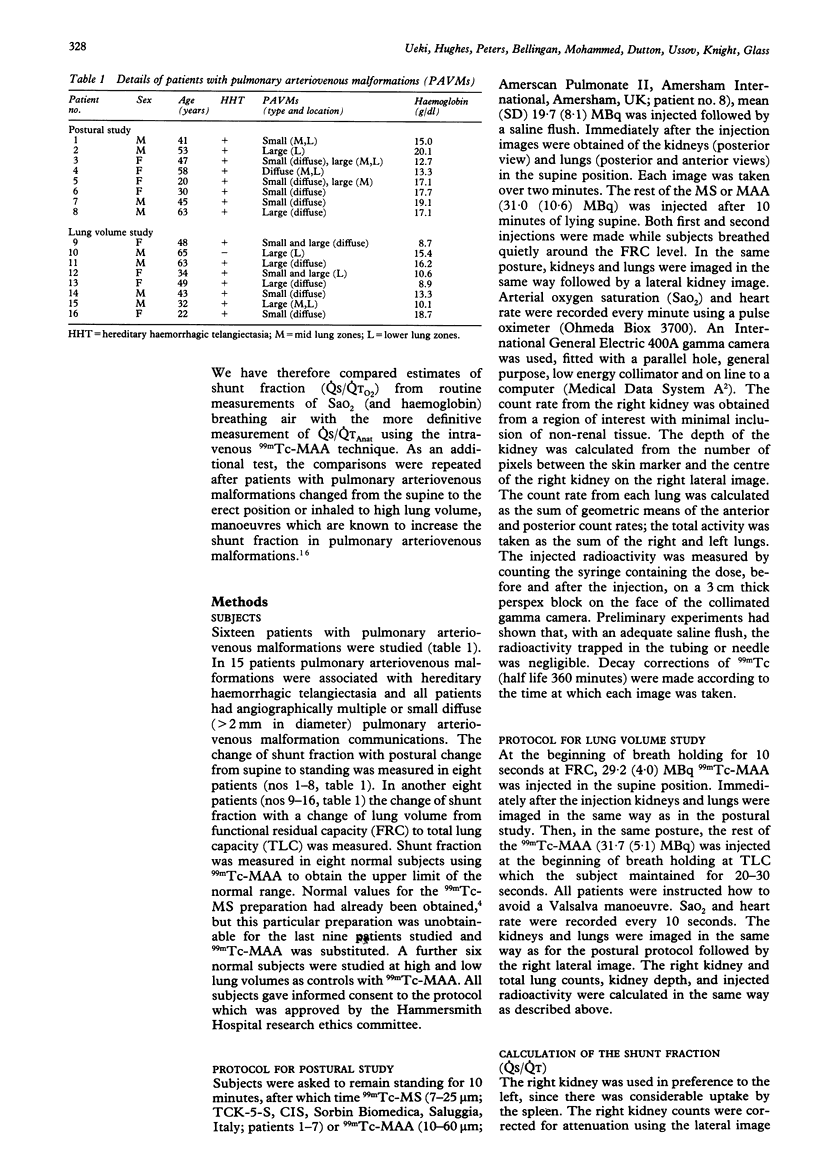
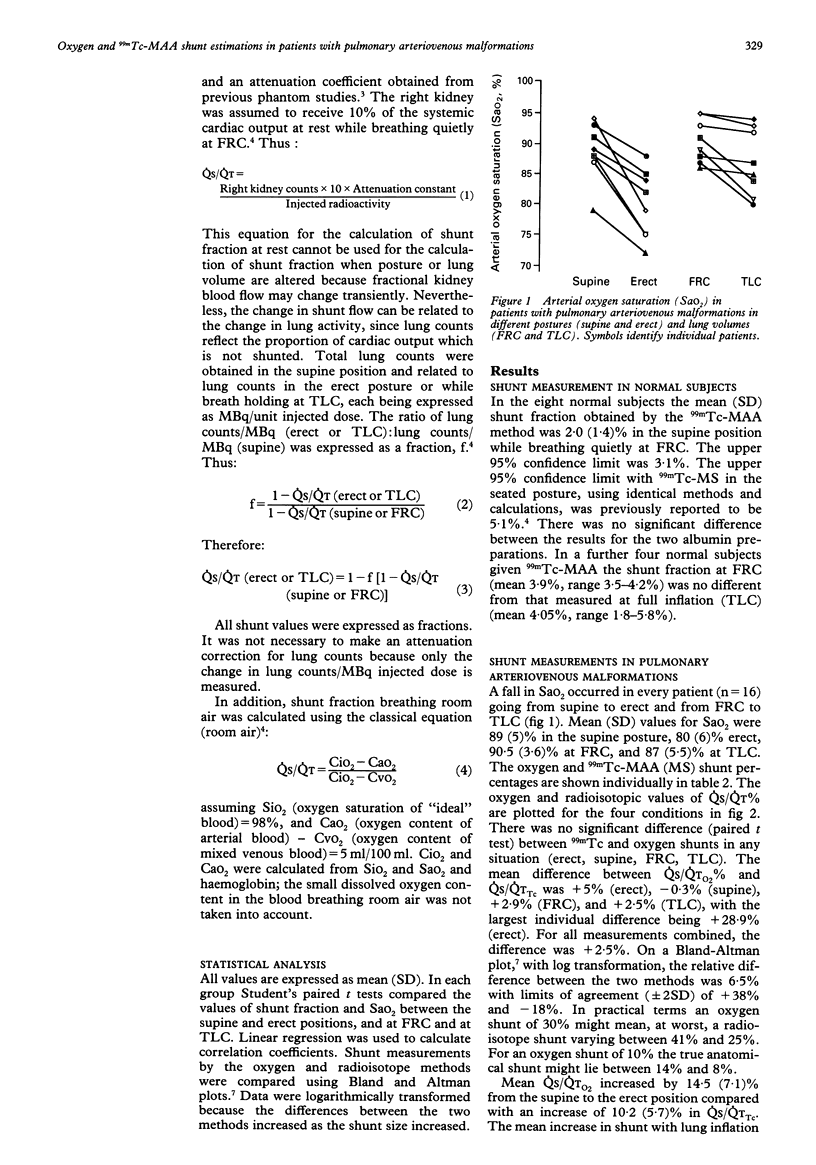
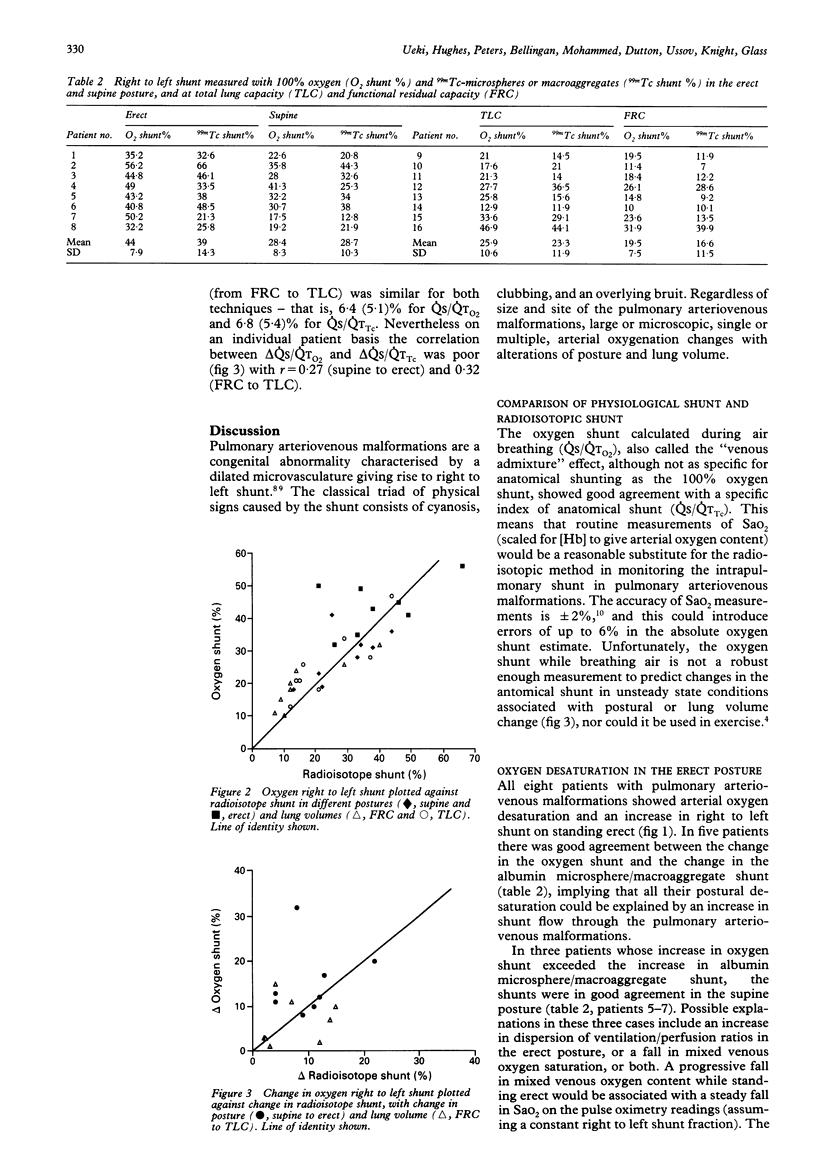
BACKGROUND--Patients with arteriovenous malformations are routinely monitored with arterial oxygen saturation (SaO2) estimations (breathing air) from which an oxygen shunt fraction can be calculated. This simple estimation has been compared with an anatomically defined estimate of the right to left shunt using a radioisotopic method. The fall in SaO2 which occurs in patients with pulmonary arteriovenous malformations in the erect posture and at high lung volumes was used to test the ability of SaO2 alone to follow changes in right to left shunt. METHODS--Radiolabelled albumin macroaggregates (99mTc-MAA) or microspheres (MS) were injected intravenously and kidneys and lungs were imaged. The shunt fraction (QS/QTTc) in the supine position at functional residual capacity (baseline) was obtained by quantifying right kidney radioactivity. On standing or while breath holding at total lung capacity, shunt fraction was calculated from baseline QS/QTTc and from lung counts and the injected dose. Arterial oxygen saturation (SaO2) was recorded by a pulse oximeter for calculation of the oxygen shunt (QS/QTO2) (breathing air). RESULTS--In the postural study (n = 8) SaO2 decreased from a mean (SD) value of 89 (5)% supine to 80 (6)% erect, corresponding to QS/QTO2 28 (8)% and 44 (8)% respectively. QS/QTTc increased from 28.7 (10.3)% to 39 (14.3)%. In the lung volume study (n = 8) QS/QTTc increased from 16.6 (11.5)% at functional residual capacity to 23.3 (11.9)% at total lung capacity while QS/QTO2 increased from 19.5 (7.5)% to 25.9 (10.6)% respectively. When all measurements were compared for QS/QTTc% and QS/QTO2% (n = 32) the difference in the mean values was 2.5% (absolute) and the limits of agreement between the two methods were +38% to -18% (relative). In neither the postural nor the volume study did delta (QS/QTO2) reliably predict delta (QS/QTTc)%. CONCLUSIONS--In pulmonary arteriovenous malformations the simple physiological shunt calculated from SaO2 breathing air agreed well with the anatomical right to left shunt measured with 99mTc-MAA, but predicted poorly the changes in anatomical shunt induced by postural or lung volume changes.
Full text
PDF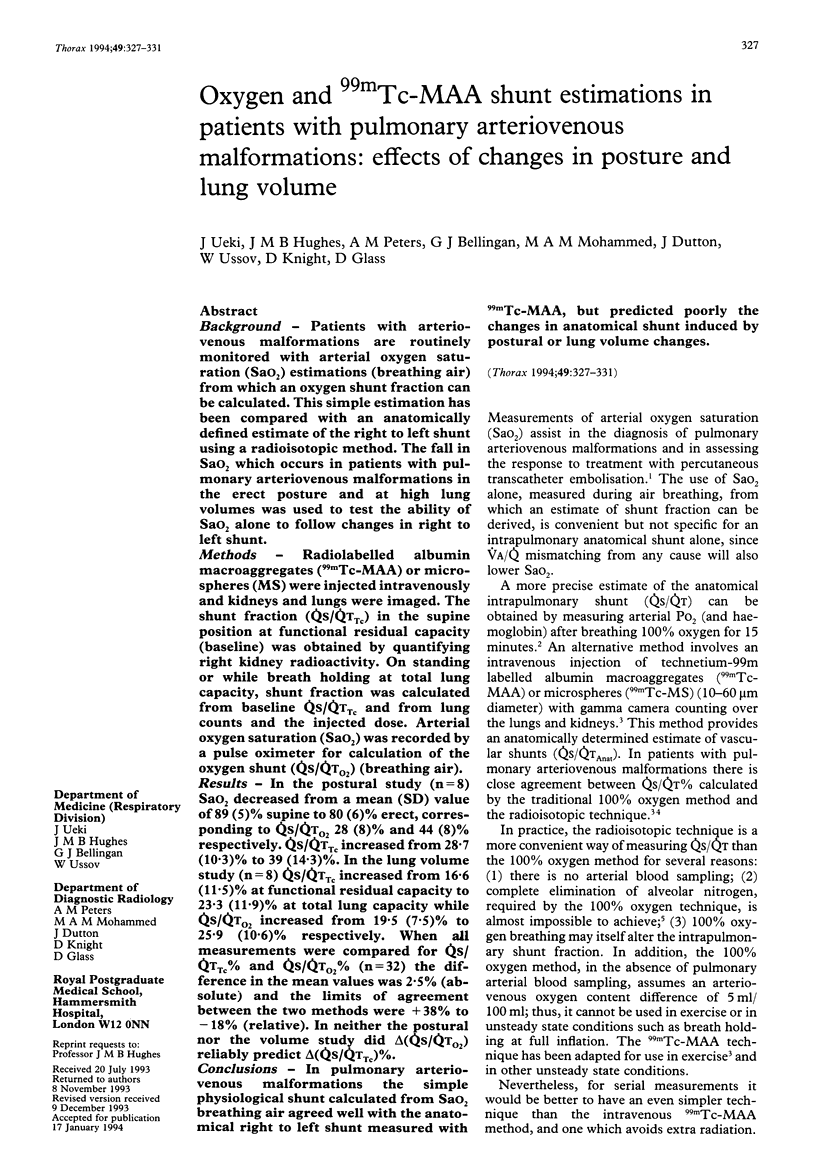
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bland J. M., Altman D. G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986 Feb 8;1(8476):307–310. [PubMed] [Google Scholar]
- Burke C. M., Safai C., Nelson D. P., Raffin T. A. Pulmonary arteriovenous malformations: a critical update. Am Rev Respir Dis. 1986 Aug;134(2):334–339. doi: 10.1164/arrd.1986.134.2.334. [DOI] [PubMed] [Google Scholar]
- Chilvers E. R., Peters A. M., George P., Hughes J. M., Allison D. J. Quantification of right to left shunt through pulmonary arteriovenous malformations using 99Tcm albumin microspheres. Clin Radiol. 1988 Nov;39(6):611–614. doi: 10.1016/s0009-9260(88)80065-5. [DOI] [PubMed] [Google Scholar]
- Chilvers E. R., Whyte M. K., Jackson J. E., Allison D. J., Hughes J. M. Effect of percutaneous transcatheter embolization on pulmonary function, right-to-left shunt, and arterial oxygenation in patients with pulmonary arteriovenous malformations. Am Rev Respir Dis. 1990 Aug;142(2):420–425. doi: 10.1164/ajrccm/142.2.420. [DOI] [PubMed] [Google Scholar]
- Dines D. E., Seward J. B., Bernatz P. E. Pulmonary arteriovenous fistulas. Mayo Clin Proc. 1983 Mar;58(3):176–181. [PubMed] [Google Scholar]
- Genovesi M. G., Tierney D. F., Taplin G. V., Eisenberg H. An intravenous radionuclide method to evaluate hypoxemia caused by abnormal alveolar vessels. Limitation of conventional techniques. Am Rev Respir Dis. 1976 Jul;114(1):59–65. doi: 10.1164/arrd.1976.114.1.59. [DOI] [PubMed] [Google Scholar]
- Harris E. A., Kenyon A. M., Nisbet H. D., Seelye E. R., Whitlock R. M. The normal alveolar-arterial oxygen-tension gradient in man. Clin Sci Mol Med. 1974 Jan;46(1):89–104. doi: 10.1042/cs0460089. [DOI] [PubMed] [Google Scholar]
- Huseby J. S., Culver B. H., Butler J. Pulmonary arteriovenous fistulas: increase in shunt at high lung volume. Am Rev Respir Dis. 1977 Feb;115(2):229–232. doi: 10.1164/arrd.1977.115.2.229. [DOI] [PubMed] [Google Scholar]
- Nickerson B. G., Sarkisian C., Tremper K. Bias and precision of pulse oximeters and arterial oximeters. Chest. 1988 Mar;93(3):515–517. doi: 10.1378/chest.93.3.515. [DOI] [PubMed] [Google Scholar]
- Rodríguez-Roisin R., Agustí A. G., Roca J. The hepatopulmonary syndrome: new name, old complexities. Thorax. 1992 Nov;47(11):897–902. doi: 10.1136/thx.47.11.897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whyte M. K., Peters A. M., Hughes J. M., Henderson B. L., Bellingan G. J., Jackson J. E., Chilvers E. R. Quantification of right to left shunt at rest and during exercise in patients with pulmonary arteriovenous malformations. Thorax. 1992 Oct;47(10):790–796. doi: 10.1136/thx.47.10.790. [DOI] [PMC free article] [PubMed] [Google Scholar]


