Abstract
Pregnancy is a unique period during a woman's life and is characterized by complex physiological changes, which may adversely affect oral health. The present systematic review was conducted to assess knowledge and awareness regarding oral health among pregnant women in India. Relevant cross-sectional observational studies were included in the systematic review to assess the level of knowledge and awareness regarding oral health among pregnant women in India. Seven studies out of 255 were finally included in the present review after conducting both electronic and manual search of scientific databases. Potential biases were reported and appropriate data were extracted by the concerned investigators. Almost 67% of the subjects had good knowledge and awareness regarding oral health in one of the study findings. Knowledge regarding effect of decayed teeth on the appearance of the people was significantly related to the parity status of the subjects (P = 0.024) in other study reports. Very few subjects (17.1% and 37.5%) felt the need for visiting a dentist during pregnancy in two studies. The results of the present review showed that pregnant women had poor knowledge and awareness regarding oral health. Therefore, there is an urgent need for education and motivation of expectant mothers regarding oral health through various health promotion interventions.
Keywords: Adverse pregnancy outcomes, low-birth weight baby, oral health awareness, oral hygiene, premature delivery
INTRODUCTION
Recently, the dental fraternity has emphasized on potential ways in which oral health may contribute to general health and well-being. Physiological conditions such as pregnancy, puberty, menstrual cycle, menopause and nonphysiological conditions such as hormonal contraception and hormonal therapy, all influence women's oral health.[1] Pregnant women have special oral health needs due to hormonal fluctuations (estrogen and progesterone), which have a strong influence on the oral cavity.[2] World Health organization, World Health Day theme of 1998, “safe motherhood pregnancy is precious-let's make it special” draws our special attention toward this priority group, which needs special care.[3]
Maintenance of oral health during pregnancy has been recognized as an important public health issue worldwide. A number of statements and guidelines have been published emphasizing improved oral health care during pregnancy.[4] Hormonal changes in pregnancy combined with neglected oral hygiene tend to increase the incidence of oral diseases like gingivitis.[5] High levels of circulating progesterone lead to pregnancy gingivitis which is characterized by increased, redness, edema and higher tendency toward bleeding. Moreover, research continues to show an association of periodontitis and adverse pregnancy outcomes (low-birth weight and premature birth); some studies have suggested that pregnancy also increases the risk of dental caries.[6,7] In addition to this, it has been shown that mothers with poor oral health may be at a greater risk of infecting their children by passing cariogenic bacteria through improper feeding practices.[8,9]
Recent datum indicates that approximately 50% of pregnant women do not visit a dentist, even when they perceive a dental need.[10] Results of another recent study conducted in South India revealed that despite the presence of pain due to dental causes, utilization of dental services by pregnant women was poor.[11] Prevention of oral and dental problems and their complications during pregnancy is possible through having pregnant women expressing appropriate knowledge, attitude and practice and seeking dental treatment at right time. Pregnant women need to be educated regarding the possible impact of periodontal diseases on pregnancy outcomes, dental disease prevention and treatment options. Studies among pregnant women with reference to their knowledge regarding oral hygiene and practices toward oral health have been recently reported from other countries,[12] but there is dearth of literature from the Indian subcontinent in this regard. Therefore, this study was carried out to assess knowledge and awareness regarding oral health during pregnancy among pregnant women in India.
MATERIALS AND METHODS
Eligibility criteria for the studies
The present systematic review included the studies conducted on oral health knowledge and awareness among pregnant women but the authors have not attempted to conduct a thorough meta-analysis. Study selection was based on following inclusion criteria: (1) Studies conducted in India; (2) studies on pregnant women; (3) published in English language; (4) studies evaluating the knowledge and awareness as outcome measures; (5) observational cross-sectional studies. No limitation in terms of publication date was considered in the search strategy.
The studies that were excluded from the present review were: (1) Studies not conducted in India; (2) reviews; (3) studies focusing only on oral health status of pregnant women or knowledge of infant oral health (4) unpublished material and abstracts. Initial electronic and manual search yielded 255 references and only seven were retained. Full texts of all the seven articles were extracted by electronic and manual search from Institutional and PGIMER Library, Chandigarh.
Identification of appropriate studies
Search strategy utilized in the present systematic review is depicted in Figure 1. The present review was conducted according to the mentioned protocol and guidelines.[13] Relevant literature search was carried out through search of scientific databases like MEDLINE, EMBASE, PubMed databases, preMEDLINE electronic databases and manual search irrespective of the date of publication using medical subject heading terms - “pregnant women,” and “India.” We identified 255 papers with this method. Various key words utilized in search strategy included-knowledge, awareness, self-care, pregnant women, India, oral health, periodontal health etc., Various combinations of key words were made using “and” “or” as Boolean operators [Table 1]. Where possible, all terms were included as full text, with truncation used where possible to capture variation in the terminology.
Figure 1.
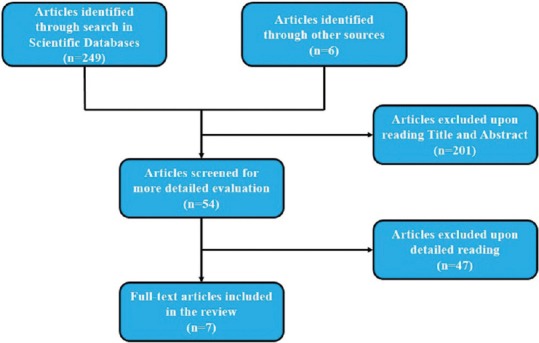
Flow diagram of various studies included in the review
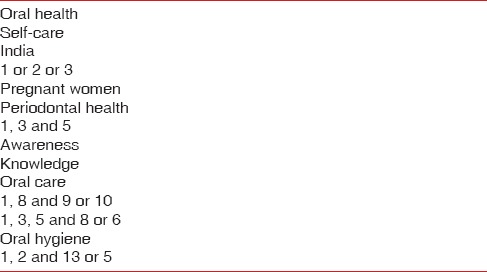
Table 1.
Various key words and their combinations used
Selection of studies
After retrieval of references yielded by the electronic and manual searches, duplicates studies were identified and excluded by two authors (RSG and AN), who then screened the abstracts and titles to identify the publications fulfilling the inclusion criteria for the review. Reviews were not included though their reference lists were searched in turn for any studies not retrieved by the electronic search. For the remaining studies, full text articles were recovered that met the inclusion criteria. Selected studies were screened using strengthening the reporting of observational studies in Epidemiology (STROBE) checklist for observational cross-sectional studies.[14] The STROBE statement is a checklist of items that should be addressed in articles reporting on the three main study designs of analytical epidemiology: Cohort, case-control, and cross-sectional studies. These items relate to the article's title and abstract, the introduction, methods, results and discussion sections and other information. All the seven studies fulfilled the requirements in the checklist.
Control of bias assessment
Articles or websites were searched that described a tool suitable for assessing quality of observational studies. Following issues were included in the risk of bias or quality assessment in the present systematic review: (1) Completeness of reporting information regarding oral health, (2) selective outcome reporting, (3) choice of outcome measures (knowledge or awareness levels regarding oral health), (4) study design, and (5) conflict of interest in the conduct of the study. When all criteria were met, the overall plausible risk of bias was estimated as low.
Collection and extraction of data
The quality assessment of the studies was done on the basis of guidelines set forth by preferred reporting items for systematic reviews and meta-analyses.[15] All the studies satisfactorily met the quality criteria. Two of the authors (TG and TSS) independently used a predetermined data collection form to extract the following information: (1) Title of the study; (2) year of publication; (3) place of origin; (4) number of participants; (5) study design; and (6) knowledge and awareness level regarding oral health. Any kind of disagreement regarding article screening and extraction was sorted out by other author. Experts in the concerned field and corresponding authors of selected studies were also contacted through E-mails for obtaining full text of included studies and missing or unclear data whenever deemed essential. We contacted four authors for further information. All responded and one provided numerical data that had only been presented graphically in the published paper.
RESULTS
Description of selected studies
The original search identified 255 studies and only seven studies were potentially eligible for the present systematic review after performing necessary exclusions.[16,17,18,19,20,21,22] The study population in all the studies comprised of pregnant women except two studies in which the results were compared with nonpregnant females also. A summary of various study characteristics is mentioned in Table 2. All the seven studies were conducted in different geographical regions of the country (Andhra Pradesh, Karnataka, Chandigarh and Rajasthan). All the studies were cross-sectional in nature and used a self-structured questionnaire (close-ended) for gathering the relevant data on knowledge regarding oral health among pregnant women.
Table 2.
Summary of studies reviewed for knowledge regarding oral health among pregnant women
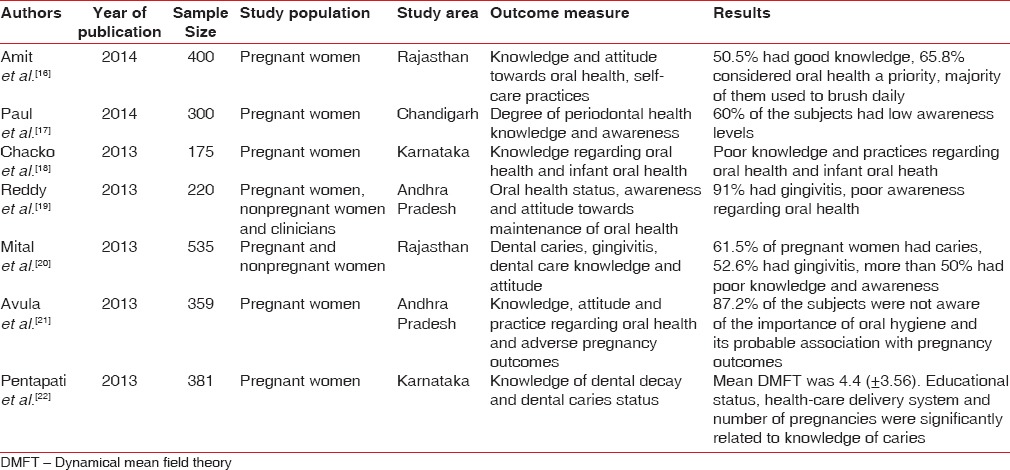
Knowledge and awareness regarding oral health
Figure 2 depicts the knowledge and awareness regarding oral health among pregnant women in different studies. Approximately 67% of the subjects had good knowledge and awareness regarding oral health in study findings of Pentapati et al.[22] It was very surprising to note that none of the subjects were aware or bothered about their oral condition in the study reports of Reddy et al.[19] Only three studies compared the knowledge of subjects regarding oral health with their educational status.[17,21,22] However, statistically significant results were obtained only to some of the questions regarding knowledge in two studies (P < 0.05)[21,22] whereas they were nonsignificant in the third study.[17]
Figure 2.
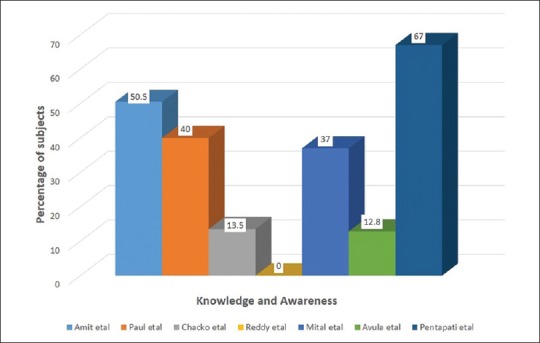
Knowledge and awareness among subjects in different studies
Parity status (no. of pregnancies) of study subjects
Figure 3 depicts the parity of subjects enrolled in different studies.[16,18,21,22] It can be noted from the figure that about 70% of the subjects were in their second or third pregnancy in the study reports of Amit et al.[16] Knowledge regarding effect of decayed teeth on the appearance of the people was significantly related to the parity status of the subjects (P = 0.024) in the study findings of Pentapati et al.[22] Conversely, nonsignificant results were obtained between parity status and knowledge of decayed teeth affecting people's work, causing serious and other health problems (P > 0.05) in the same study.
Figure 3.
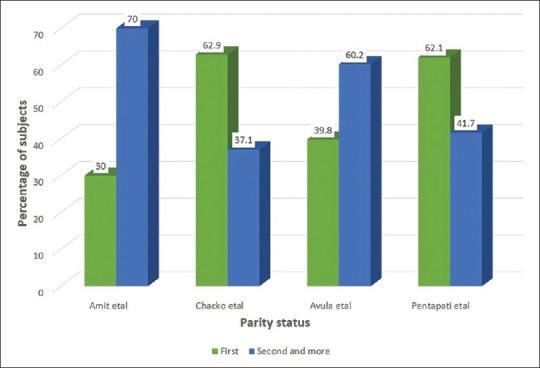
Parity status of different study subjects
Trimester during which subjects were enrolled in the studies
Information regarding trimester of pregnancy during which the subjects were enrolled in the respective studies (four)[18,19,21,22] is cited in Figure 4. Comparatively more number of subjects were in their third trimester of pregnancy as compared to subjects in first trimester in all the four studies. When trimester of pregnancy was compared with the knowledge regarding decayed teeth, no significant differences (P > 0.05) were observed in the knowledge for any of the questions in the study reported of Pentapati et al.[22]
Figure 4.
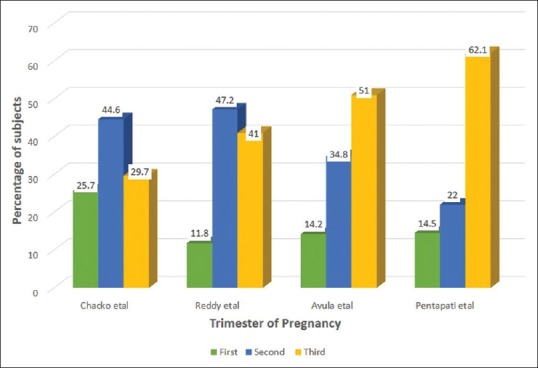
Status of study subjects according to their trimester of pregnancy
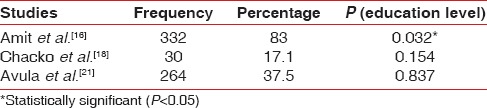
Necessity of dental visits during pregnancy
Only three studies provided information regarding the necessity of dental visits during pregnancy.[16,18,21] Table 3 depicts the number of subjects who felt the need for dental visits during pregnancy in three studies. Study findings of Amit et al.[16] revealed that more than 80% of subjects felt the necessity of dental visits during pregnancy. This finding was significantly related to the educational level of the study subjects (P = 0.032). However, during the previous 12 months only 11.8% of women surveyed had attended the dentist in the same study. Very few subjects (17.1% and 37.5%) in the other two studies felt the need for regular dental visits during pregnancy.[18,21]
Table 3.
Necessity of dental visits during pregnancy felt among subjects in three studies
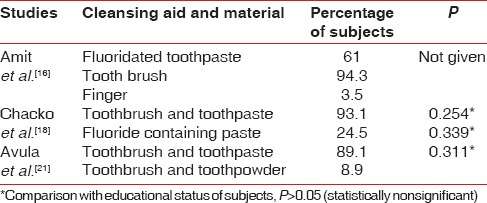
Cleansing aids used by subjects
Information regarding cleansing aids used by study subjects has been cited only in 3 out of 7 studies.[16,18,21] Almost 90% of subjects in all the three studies were using toothbrush and toothpaste to clean their teeth [Table 4]. On the contrary, 3.5% of subjects were using finger to clean their teeth in the study findings of Amit et al.[16] However, educational status did not have any impact on the oral hygiene practices of the subjects in both the studies (P > 0.05).
Table 4.
Cleaning aid and material used by subjects in different studies
Periodontal infection and pregnancy outcome
Only 40% of study subjects in the study reports of Avula et al.[21] were of the opinion that tooth and gum problems could affect the pregnancy outcome. This finding was statistically significant with regard to educational qualification of the subjects (P = 0.001). It was also reported in the study findings of Reddy et al.[19] that only 35% of the clinical staff managing pregnant women had ever advised them to maintain good oral hygiene and get routine check-up done.
DISCUSSION
The emphasis of the present systematic review was on the oral health knowledge and awareness among pregnant women in India and no attempt was made to compare the oral health status of pregnant women. Various parameters were utilized in order to accumulate oral health information among pregnant women which is evident from the results. Knowledge and awareness regarding oral health was found to be low among the study subjects and showed contrasting results in different studies. This could be attributed to variation in sample size and different study settings. A self-reported questionnaire was used for gathering information regarding oral health from the study subjects. This can increase the risk of bias while evaluating studies on knowledge and awareness. All the studies used a close-ended questionnaire to obtain information about various aspects of oral health and pregnancy. Such type of questionnaire reduces recall bias and such questions are easy to analyze and may achieve quicker response from the subjects.
It is reported by Amit et al.[16] and Avula et al.[21] that more than 60% of the women already had one or two children and now were in their second or third pregnancy respectively. This indicates failure of family welfare programs in India which are aimed at reducing the birth rate to the extent necessary to stabilize the population at a level consistent with the requirement of the national economy. The Family Welfare Programme in India is recognized as a priority area, and is being implemented as a 100% centrally sponsored program.[23] Parity status was significantly related to knowledge about the appearance of decayed teeth. This could be due to possibly younger age of subjects who give more importance on aesthetic appearance.[22]
Among the women of different trimesters, there was no difference in knowledge for any of the questions that were asked.[22] This could be due to the reason that during pregnancy, beliefs and perceptions are not likely to change and tend to be stable during the course of pregnancy. Only few subjects felt the need for dental visits during pregnancy in the study reports of Chacko et al.[18] and Avula et al.[21] This could be attributed to various factors like poor knowledge, poor education, limited access to dental care, as well as various sociocultural factors and perceptions among pregnant women in India.
More than half of pregnant women did not felt the need for dental visits during pregnancy in the study reports of Chacko et al.[18] and Avula et al.[21] This could be due to the reason that their obstetric provider did not encourage them to see a dentist during pregnancy or themselves lacked understanding about the importance of oral health in pregnancy. Only 40% of women believed that tooth and gum problems could influence pregnancy outcome and this was significantly related to educational status of subjects.[21] This indicates that there is an imperative need to impart oral health education to pregnant women, with the greatest need in the lower education strata.
The present review had some limitations as well. There was under-reporting of some relevant information (descriptive data, questionnaire) related to knowledge, attitude and awareness among pregnant women in three studies.[17,19,20] As a result of this, some important aspects pertaining to knowledge and awareness were not included and compared with other studies that were included in the review. This study was based on a review of previous studies, which were conducted in different time periods by different authors. Therefore, it may be difficult to generalize the results on the entire population. The present review compared and discussed some common and relevant aspects regarding oral health knowledge of pregnant women. Because of the marked variability in the questionnaire and outcomes of the included studies, it was not possible to combine the data and perform meta-analysis. Moreover, sample in two studies comprised of different type of subjects; one study compared knowledge levels of pregnant with nonpregnant women,[20] whereas in the other study, clinical staff who were managing pregnant women were enquired about the oral conditions in pregnancy or if they offered any advice.[19] Therefore, this type of sample could account towards different levels of knowledge and awareness.
The present systematic review involved the electronic and manual search of multiple scientific databases, with no restriction regarding year of publication. The reference lists of literature reviews were searched for other studies that could also be included. However, it is possible that some relevant data may have been left behind in terms of fugitive literature (conference proceedings, dissertations, technical reports, etc). This could have accounted for some publication bias and any important information will undoubtedly be overlooked with the type of literature search strategy as used to conduct the present review.
CONCLUSION
Good oral health during pregnancy can not only improve the health of the pregnant mother, but also potentially the health of her child. The present review showed that pregnant women's knowledge and awareness regarding oral health was poor as displayed from the results. Most of the women were unaware of the potential consequences of neglecting oral hygiene during pregnancy. Pregnancy is a “teachable” moment when women are motivated to adopt healthy behavior. Women and families need to hear from a variety of sources about the importance and safety of dental care during pregnancy. Therefore, various health promotion interventions should be carried out during pregnancy in order to motivate and educate expectant mothers on importance of good oral health. Moreover, if obstetric providers could talk with their pregnant patients about oral health; there is a high probability the patient will pay more attention to their oral health and may schedule a dental visit. There is a need for creative, consistent, and comprehensive public health communication strategies that promote oral health to women in accessible and timely manners.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Patil SN, Kalburgi NB, Koregol AC, Warad SB, Patil S, Ugale MS. Female sex hormones and periodontal health-awareness among gynecologists – A questionnaire survey. Saudi Dent J. 2012;24:99–104. doi: 10.1016/j.sdentj.2011.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kloetzel MK, Huebner CE, Milgrom P, Littell CT, Eggertsson H. Oral health in pregnancy: Educational needs of dental professionals and office staff. J Public Health Dent. 2012;72:279–86. doi: 10.1111/j.1752-7325.2012.00333.x. [DOI] [PubMed] [Google Scholar]
- 3.Fathalla M. Women have a right to safe motherhood. Plan Parent Chall. 1998;1:1–2. [PubMed] [Google Scholar]
- 4.Buerlein J, Peabody H, Santoro K. NIHCM Foundation Improving Access to Perinatal Oral Health Care: Strategies and Considerations for Health Plans: Issue Brief July 2010 National Institute for Health Care Management. [Last accessed on 2014 Dec 01]. Available from: www.nihcm.org/pdf/NIHCM-OralHealth-Final.pdf .
- 5.Cengiz SB. The pregnant patient: Considerations for dental management and drug use. Quintessence Int. 2007;38:e133–42. [PubMed] [Google Scholar]
- 6.George A, Shamim S, Johnson M, Ajwani S, Bhole S, Blinkhorn A, et al. Periodontal treatment during pregnancy and birth outcomes: A meta-analysis of randomised trials. Int J Evid Based Healthc. 2011;9:122–47. doi: 10.1111/j.1744-1609.2011.00210.x. [DOI] [PubMed] [Google Scholar]
- 7.American Academy of Pediatric Dentistry, Clinical Affairs Committee-Infant Oral Health Subcommittee. Guideline on infant oral health care. Pediatr Dent. 2012;34:148–52. [Google Scholar]
- 8.Cucó G, Fernández-Ballart J, Sala J, Viladrich C, Iranzo R, Vila J, et al. Dietary patterns and associated lifestyles in preconception, pregnancy and postpartum. Eur J Clin Nutr. 2006;60:364–71. doi: 10.1038/sj.ejcn.1602324. [DOI] [PubMed] [Google Scholar]
- 9.George A, Johnson M, Blinkhorn A, Ajwani S, Bhole S, Yeo AE, et al. The oral health status, practices and knowledge of pregnant women in south-western Sydney. Aust Dent J. 2013;58:26–33. doi: 10.1111/adj.12024. [DOI] [PubMed] [Google Scholar]
- 10.Hwang SS, Smith VC, McCormick MC, Barfield WD. Racial/ethnic disparities in maternal oral health experiences in 10 states, pregnancy risk assessment monitoring system, 2004-2006. Matern Child Health J. 2011;15:722–9. doi: 10.1007/s10995-010-0643-2. [DOI] [PubMed] [Google Scholar]
- 11.Shenoy R, Chacko V. Utilization of dental services due to dental pain by pregnant women in India: A qualitative analysis. J Interdiscip Dent. 2013;3:18–20. [Google Scholar]
- 12.Bamanikar S, Kee LK. Knowledge, attitude and practice of oral and dental healthcare in pregnant women. Oman Med J. 2013;28:288–91. doi: 10.5001/omj.2013.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.York: University of York; 2009. [Last cited on 2015 Apr 15]. Centre for Reviews and Dissemination. Systematic Reviews: CRD's Guidance for Undertaking Reviews in Health Care. Available from: http://www.york.acuk/inst/crd/systematic_reviews_book.htm . [Google Scholar]
- 14.Switzerland: 2007. [Last cited on 2014 Dec 01]. STROBE Statement. Strengthening the Reporting of Observational Studies in Epidemiology [Monograph on the Internet] Available from: http://www.strobe-statementorg/indexphp?id= Available from: [Google Scholar]
- 15.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions. Explanation and elaboration. J Clin Epidemiol. 2009;62:e1–34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 16.Agarwal A, Mital P, Hooja N, Mital P, Salvi A, Fatima A. Oral and dental health knowledge, attitude and practice among pregnant Women. Sch Acad J Biosci. 2014;2:627–32. [Google Scholar]
- 17.Paul Y, Singh P, Singla P, Rathore S, Vaid R. Periodontal health – Awareness among pregnant females in semi urban population of Chandigarh – A cross-sectional survey. BFUDJ. 2014;5:49–53. [Google Scholar]
- 18.Chacko V, Shenoy R, Prasy HE, Agarwal S. Self-reported awareness of oral health and infant oral health among pregnant women in Mangalore, India – A prenatal survey. Int J Health Rehabil Sci. 2013;2:109–15. [Google Scholar]
- 19.Reddy RS, Amara SL, Tatapudi R, Koppolu P, Nimma VL, Reddy RL. Awareness and attitude towards maintenance of oral health during pregnancy among patients and clinicians attending obstetrics and gynecology ward. J Dr NTR Univ Health Sci. 2013;2:102–8. [Google Scholar]
- 20.Mital P, Agarwal A, Raisingani D, Mital P, Hooja N, Jain P. Dental caries and gingivitis in pregnant women. Sch Acad J Biosci. 2013;1:718–23. [Google Scholar]
- 21.Avula H, Mishra A, Arora N, Avula J. KAP assessment of oral health and adverse pregnancy outcomes among pregnant women in Hyderabad, India. Oral Health Prev Dent. 2013;11:261–70. doi: 10.3290/j.ohpd.a30481. [DOI] [PubMed] [Google Scholar]
- 22.Pentapati KC, Acharya S, Bhat M, Rao SK, Singh S. Knowledge of dental decay and associated factors among pregnant women: A study from rural India. Oral Health Prev Dent. 2013;11:161–8. doi: 10.3290/j.ohpd.a29734. [DOI] [PubMed] [Google Scholar]
- 23.Zodgekar AV. Family welfare programme and population stabilization strategies in India. Asia Pac Popul J. 1996;11:3–24. [PubMed] [Google Scholar]


