Abstract
Background
The Connect for Health study is designed to assess whether a novel approach to care delivery that leverages clinical and community resources and addresses socio-contextual factors will improve body mass index (BMI) and family-centered, obesity-related outcomes of interest to parents and children. The intervention is informed by clinical, community, parent, and youth stakeholders and incorporates successful strategies and best practices learned from ‘positive outlier” families, i.e., those who have succeeded in changing their health behaviors and improve their BMI in the context of adverse built and social environments.
Design
Two-arm, randomized controlled trial with measures at baseline and 12 months after randomization.
Participants
2-12 year old children with overweight or obesity (BMI≥ 85th percentile) and their parents/guardians recruited from 6 pediatric practices in eastern Massachusetts.
Intervention
Children randomized to the intervention arm receive a contextually-tailored intervention delivered by trained health coaches who use advanced geographic information system tools to characterize children's environments and neighborhood resources. Health coaches link families to community-level resources and use multiple support modalities including text messages and virtual visits to support families over a one-year intervention period. The control group receives enhanced pediatric care plus non-tailored health coaching.
Main Outcome Measures
Lower age-associated increase in BMI over a 1-year period. The main parent- and child-reported outcome is improved health-related quality of life.
Conclusions
The Connect for Health study seeks to support families in leveraging clinical and community resources to improve obesity-related outcomes that are most important to parents and children.
Keywords: Randomized controlled trial, obesity, children, clinical, community, health coaching, mobile technology
BACKGROUND
Childhood overweight and obesity place a significant burden on morbidity and quality of life. In the United States, the prevalence of childhood overweight and obesity appears to have plateaued and may even be decreasing among 2- to 5-year old children as of 2012.1 Yet, overall prevalence remains at historically high levels and substantial racial/ethnic disparities continue to persist, and in the case of Hispanic children, perhaps even be widening.1,2 Health care system-based interventions to reduce obesity have been somewhat effective but are often limited in their effectiveness due to the myriad social and environmental barriers that impede improvement in obesity-related behaviors.3,4
An important, but often overlooked aspect of interventions to improve obesity and reduce disparities is the careful consideration of the socio-environmental context in which decisions are being made related to health behaviors, and in which behavior change is expected to occur. Neighborhood socioeconomic characteristics and built environment factors including the food and physical activity environments can significantly influence health behaviors.5-8 Understanding community levels of poverty and unemployment as well as individual, health-related social problems could assist health practitioners in providing targeted resources and selecting referrals to local health and social service agencies.9 Sophisticated geographic information systems (GIS) analyses can provide community-level data on access to food establishments that could assist in meal planning discussions with families. GIS methods and community mapping could also provide information about recreational spaces and playgrounds as well as transportation availability that might influence parents’ decision making regarding their child's physical activity options. Thus, characterizing the environment can assist in developing the best, flexible, clinical-community intervention that could be adapted to an individual's personal and environmental setting.
Another underused approach to obesity management and disparities reduction is to identify innovative strategies from ‘positive outliers’ (also referred to in the literature as “positive deviants”). Positive outliers are defined as individuals who have succeeded where many others have not to change their health behaviors, reduce their body mass index, and develop resilience in the context of adverse built and social environments.10,11 The central premise of this positive outlier approach is that solutions to problems that face a community often exist within that community, and that certain community members possess strategies that can be generalized and promoted to improve the outcomes of other members. Such individuals could help guide intervention development for other families in their same neighborhoods who have struggled with behavior change.
We designed the Connect for Health randomized controlled trial to leverage clinical and community resources and address socio-contextual factors to improve obesity and family-centered outcomes. The intervention was built upon practices of positive outlier families as well as strategies recommended by a diverse group of stakeholders representing parents, children, pediatric clinicians, and community/public health providers.12,13 In this paper we summarize the development and methods of Connect for Health.
INTERVENTION DEVELOPMENT
Stakeholder Engagement
The design and implementation of Connect for Health has been and will continue to be informed by a diverse group of stakeholders representing clinicians, community and public health providers, as well as parents and children. Members of the research and clinical team have long-standing collaborative relationships developing previous obesity interventions 14 and thus, a key activity in preparation for this study was to build a strong network of cross-collaboration among stakeholders who had not yet worked with each other.
Using established methods on engagement15 and the Patient-Centered Outcome Research Institute's Methodology Standards,16 we worked with our clinician team to identify “positive outlier” children and families who would be interested in participating in focus group discussions about their experiences. 12,13 Several children and parents from these focus groups now participate as ongoing members of our parent and youth advisory board. Leaders and staff of youth-serving community-based organizations, including the YMCA, provided critical input on the ideas and activities we ultimately implemented. Based on principles of engagement, the research team has delineated the role of stakeholder participants, discussed the relevance and importance of the work being developed and ways in which input from all stakeholders will be utilized. Keys to successful implementation, incorporation of study activities into practice, and sustainability of project activities rely on engagement of stakeholders at several critical points before and during the intervention. The research and stakeholder group has met on a monthly basis since the start of the study to discuss barriers and facilitators to implementation.
Parent and Youth Advisory Boards
Patient advisory committees have been increasingly used in health care systems to gather patient-centered input on a variety of health care processes and to accelerate improvement.17 Engaging patients as active participants in designing and conducting healthcare research is increasingly recognized as critical to ensuring that the research questions posed and outcomes measured are relevant and important to patients.18-20 In this study, we convened Parent and Youth Advisory Boards to inform the study development. The Parent Board consists of 11 parents whose children receive care in the participating pediatric practices and is led by a parent whose children receive their care at one of the practices. The Youth Board is made up of their children, ages 10 to 12 years. Board members were recruited from among focus group and interview participants in our formative work with positive outlier children and their parents. Board members provide in-depth information about their own successful strategies that can be generalized and promoted to improve the outcomes of other families, advise the research team on the perspectives of potential trial participants, and provide feedback on specific components of the study. The Board meets in-person 1-2 times in each study year and communicates as needed more regularly to discuss study methods and implementation, including recruitment, informed consent, outcome measures, data collection, incentives, retention, and intervention design. Parents and youth participating on the Advisory Board receive a modest stipend for their participation.
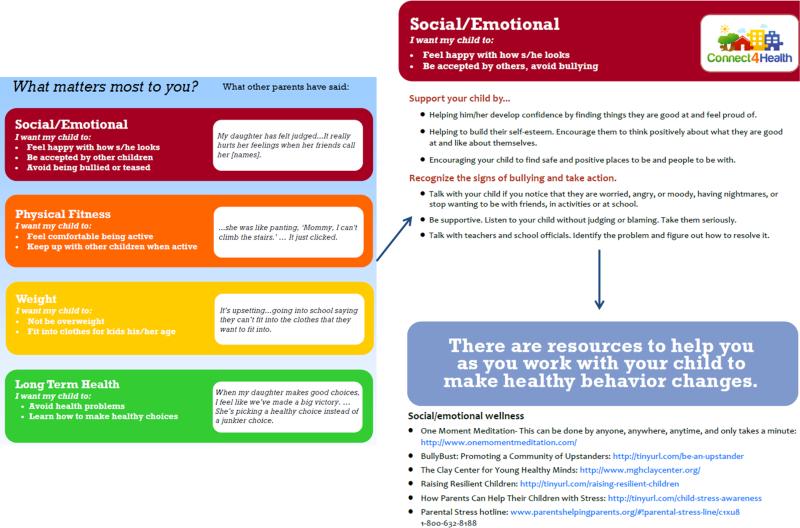
Learning from Positive Outliers
Prior to the start of the study we conducted five focus groups with parents (n=41) and 4 focus groups with children (n=21) who were identified from their electronic health record to have reduced or maintained their BMI despite having had a history of a BMI ≥ 95th percentile. We have previously published the methods and results of this formative work. 12,13 Parents reported several practices that facilitated their ability to help their child improve their BMI. Among them were: 1) making changes as a family rather than solely for the child; 2) implementing limits and rules around snacking, screen time and activity, and maintaining consistency around those rules; 3) being involved in the decision-making with their health care provider about their child's weight management; 4) using more immediate rather than long-term outcomes of weight management to motivate change, and 5) maximally leveraging community resources to support behavior change. Children emphasized the value of positive support from their family and the importance of their peer relationships in motivating their behavior change. Parents and children outlined a number of outcomes that mattered most to them related to weight management including: not being bullied or teased, feeling good about oneself, fitting into age-appropriate clothing, and being able to keep up with other children while being physical active. As a result, our intervention included an emphasis on social and emotional wellness. The feedback we received specifically informed our outcome measures, the neighborhood resources we included in our intervention, the youth-serving community-based organizations that we partnered with, as well as our approach to coaching, e.g. shared-decision making and family-centered care were key training topics for the health coaches.
METHODS
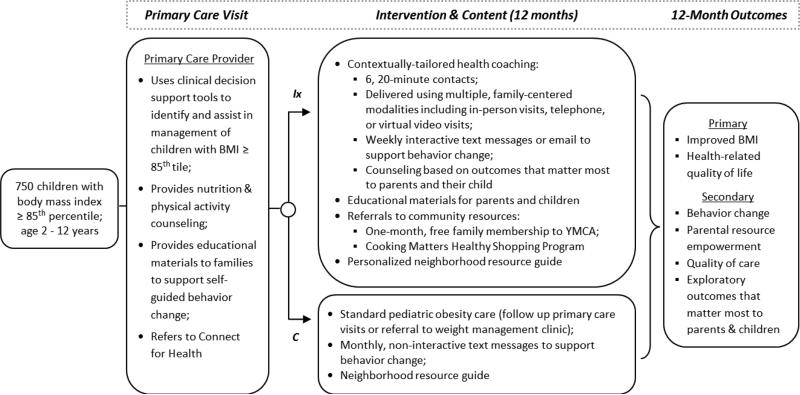
Overview of study design (Figure 1)
Figure 1.
Study Design and Intervention Components of the Connect for Health Randomized Controlled Trial
Connect for Health is a randomized controlled trial being conducted within 6 pediatric practices of Harvard Vanguard Medical Associates (HVMA), a multi-specialty group practice in eastern Massachusetts with many years of experience with an electronic health record system and advanced team-based care model. We randomly assigned patients to one of 2 arms: 1) a contextually-tailored, clinical-community intervention vs. 2) best-practice enhanced pediatric care (control). The target population is children 2-12.9 years old at the time of enrollment with a BMI > 85th percentile. The primary, intention-to-treat analysis will examine the extent to which the intervention results in a smaller age-associated increase in BMI compared to the control condition over a 1-year intervention period. Additionally, we aim to improve outcomes that matter most to parents and children including pediatric health-related quality of life. All study activities were approved by the Institutional Review Board at Partners Health Care System. The Connect for Health trial has been recorded in the clinicaltrials.gov national registry of randomized trials.
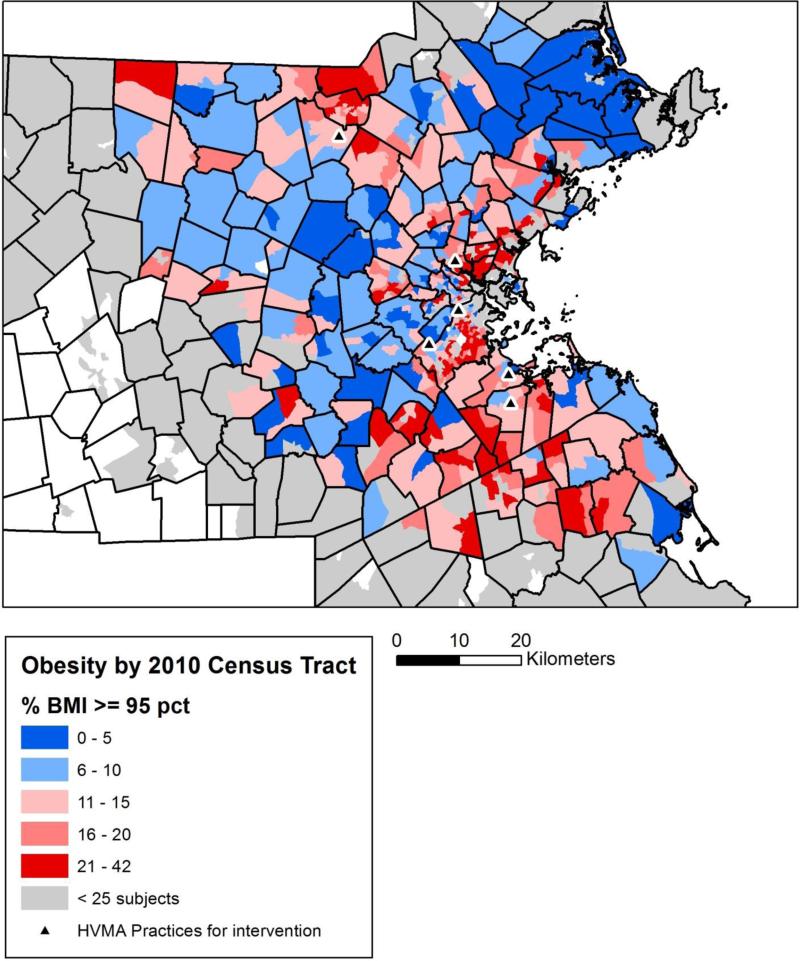
Selection of Participating Pediatric Practices
To select the pediatric practices for this study we used residential addresses and BMI obtained from the electronic health record of 49,770 children and adolescents (<19 years), seen at the 14 pediatric practices of HVMA from August 2011 to August 2012. Using geographic information software, we identified the zip codes in eastern MA where the prevalence of childhood obesity for children ages 2 to 12 years (age-criteria for enrollment in Connect for Health) was greater than the national average of 15% and defined these as geographic clusters of high childhood obesity prevalence or “obesity hot spots”.21 We selected the 6 HVMA health centers that care for the greatest number of children living in obesity hot spots. Figure 2 shows a map of the obesity hot spots and the locations of our participating pediatric practices. Preliminary data of children who receive their care at the 6 health centers indicates that 46% of children are white, 28% black, 15% Hispanic or Latino, and 11% of mixed or other race/ethnicity.
Figure 2.
Geographic Clusters of High Childhood Obesity Prevalence in Eastern Massachusetts and Selected Pediatric Practices for the Connect for Health Study
Randomization
We randomized study participants from 6 centralized randomization lists, one for each of the participating pediatric practices. The lists were generated by the study biostatistician (JO) and maintained by the study project manager (CH). We organized the lists into blocks of size 4 in order to maintain balance between the two study arms in each of the practices. Patients were randomized according to the order in which their consent was obtained. No one except the study project manager and study biostatistician had access to the randomization lists - the study project manager to allocate participants to the proper intervention and the study biostatistician to provide blinded reports of study progress and safety data. Unblinding of study investigators will not occur until after the final follow-up visit is completed and the database is locked.
Blinding
All research staff performing assessments, study participants, and referring pediatricians are blinded to specific study hypotheses and to intervention assignment. Health coaches delivering the intervention are not blinded but only worked with participants in the intervention arm.
Eligibility and Recruitment
Eligibility for Connect for Health included: 1) child was 2.0-12.9 years old at enrollment, 2) child's BMI was ≥85th percentile for age and sex at enrollment, 3) at least 1 parent had an active email address and 4) at least one parent was comfortable communicating in English. Children were excluded if: 1) their family was planning to leave HVMA within the study time frame, 2) their clinician did not feel the study was appropriate for them or their families, e.g., emotional or cognitive difficulties, 3) their sibling was already enrolled in the study, 4) they or their parents were part of the study's parent/youth advisory board, or 5) they had a chronic medical condition or take medication that substantially interferes with growth or physical activity participation.
Recruitment began in July 2014 and ended in March 2015. At the time of a scheduled visit with a child between the ages of 2-12 years with a BMI > 85th percentile, clinicians received a BestPractice® alert in the electronic health record. The alert triggered as a new window “in front of” the screen on which the clinician was working. The alert contained a link to refer children to the Connect for Health study. Clinicians briefly discussed the study and if the parent and clinician agreed, referred the family to the study. Research staff provided HVMA clinicians with a one-page handout to give parents with more information about the study, including next steps and a phone number to call to begin the enrollment process if interested.
After receiving the referral, study staff sent each family a letter introducing the study and inviting the family to participate. The mailing included a fact sheet with information about study participation as well as an opt-out phone number to call if parents did not want to be contacted. We called parents who did not refuse additional contact beginning 5 days after mailing the letter. Research assistants establish eligibility, explain the study, answer questions, obtain verbal consent, and complete a baseline survey over the phone. While establishing eligibility the research assistants are blinded to study arm assignment. Research assistants then verified contact information and emailed parents a $25 gift card for completing the baseline survey. We then randomized participants and mailed parents an enrollment letter. For children between the ages of 8 and 12 years old, we also mailed a brief survey for the child to complete, along with a $2 bill as an incentive for the child, and a postage-paid business reply envelope. The participant flow for the study is included as supplementary material. .
Intervention
All pediatric primary care providers received a computerized, clinical decision support (CDS) alert during primary care visits, identifying children as overweight or obese, and two additional CDS tools to assist in management and follow up of overweight or obese children.14,22 These tools included pre-populated, standardized note templates specific for obesity that included options for: 1) documenting and coding for BMI percentile, 2) documenting and coding for nutrition and physical activity counseling, 3) placing referrals to weight management programs, 4) placing orders for laboratory studies if appropriate, and 5) printing educational materials.
We provided a comprehensive set of educational materials focusing on specified behavioral targets (Table 1) to providers to give to their patients at well-child and obesity follow-up visits. These materials were based on our previous STAR trial and have been shown to be effective in improving child BMI.14 The materials focus primarily on decreases in screen time and sugar-sweetened beverages; increases in moderate and vigorous physical activity; and improvement of sleep duration and quality. Based on our qualitative work with positive outlier families and feedback from our parent and youth advisory board, we also developed materials to promote social and emotional wellness.
Table 1.
Parent- and Child-Reported Outcomes Measures in the Connect for Health Study.
| Parent- and Child-Reported, Obesity-Related Outcomes of Interest | Measures & Source | Reported By: | |
|---|---|---|---|
| Parent | Child | ||
|
Health-Related Quality of Life Intervention goals: Improve parent- and child-report of child health-related quality of life |
• Health-Related Quality of Life: Parents report their child's quality of life using the 4 subscales of the PedsQL-4.0; children report their own quality of life using the child version of the PedsQL validated among children ages 8 and over.32,33 | X | X |
|
Social and Emotional Wellness Intervention goals: Assist parents in finding people, places, and resources to help reduce parent and child stress and improve parental empowerment related to their child's healthy body weight |
• Perceived Stress: Parent and child report of the amount of general stress in their life; major predictor for suicide in Nurses' Health Study.41 | X | X |
| • Parental Resource Empowerment- Parent report of knowledge of, ability to access, and comfort accessing resources, as well as knowledge of the strategies needed to identify new resources, and ability to obtain those resources.34 | X | ||
|
Sleep Routines and Behaviors Intervention goals: Meet age-appropriate recommendations for sleep duration to; promote a regular bedtime; adopt a calming nighttime routine |
• Sleep duration: Parent report of average amount of daily sleep their children obtained including naps from the Pediatric Sleep Questionnaire.42-45 | X | |
| • Regular bedtime: Parent and child report of typical bedtime on weekdays and weekend days.46 | X | X | |
|
Screen time Intervention goals: Limit screen-viewing and gaming time to < 2 hours/day |
• TV and video viewing: Average daily hours spent watching TV or videos.47 | X | X |
| • Gaming: Average daily hours spent playing games on media such as television, desktop computers, laptops, portable DVD players, iPads, or smartphones48 | X | ||
|
Diet Quality Intervention goals: Reduce sugar-sweetened beverages; replace non-nutritive snacks with fruits and vegetables; reduce fast food intake. |
• Sugar-sweetened beverage and fruit & vegetable intake: fruit, vegetable, sugar-sweetened beverage (i.e., regular (not diet) sodas or soft drinks, including Malta, Penafiel, or Sumol, punch, Kool-Aid, Tampico, sports drinks, Goya juice or other fruit-flavored drinks) and water consumption are assessed using six questions drawn from the School Physical Activity and Nutrition monitoring system.49,50 | X | X |
| • Fast food intake: Modified question adapted from the Growing Up Today Study 51; associated with BMI. | X | X | |
|
Physical activity Intervention goals: Increase the number of days that child is physically active for at least 60 minutes. |
• Physical activity: Youth Risk Behavior Survey; examines the number of days in the past 7 days the child was physically active for a total of at least 60 minutes.52 | X | X |
|
Quality of Obesity-Related Health Care Services Intervention goals: Improve the quality of obesity-related health care services provided by primary care provider. |
• Quality of Obesity-Related Health Care Services: Assessed using 8 modified questions from the Patient Assessment of Chronic Illness Care.35 | X | |
|
Exploratory Obesity-Related Outcomes That Matter Most to Parents & Children Intervention goals: Improve weight-related outcomes that matter most to children and parents |
• Exploratory questions: Five closed-ended questions for parents and children about the weight-related outcomes that mattered most to them. We asked parents, “How important is it to you for your child to...”, and asked children ages 8-12 years, “How important is it to you to...”. The items were: (1) not be overweight; (2) not be bullied or teased; (3) fit into clothing for children his or her age; (4) be accepted by other children his or her age; and (5) avoid health problems like diabetes or heart disease. | X | X |
Enhanced Primary Care (Control)
Participants in the control group were exposed to the clinical best practices described above. In addition, participants received monthly text messages that contained links to publically-available resources to support behavior change, e.g. links to the Let's Move! program.23 Participants also received a Neighborhood Resource Guide listing places that support healthy living in their community and surrounding areas.
Contextually-Tailored Clinical-Community Intervention
Following their pediatric primary care visit, parents of children randomized to the intervention arm receive health coaching that is tailored to their socio-environmental context. Health coaching is delivered by trained research staff using telephone, email, mail, text messages, virtual video visits (using Vidyo®, a HIPAA compliant, password-protected software offered for free to families), and in-person visits, according to parent preference. The study aims to make weekly contact with families using interactive texts messages or emails. We also aim to provide 6, approximately 20-minute contacts that are scheduled every other month over the course of the 1-year intervention period. These one-on-one contacts or “visits” with health coaches are in-person, by telephone, or by virtual video calls.. Prior to the start of the intervention, the two health coaches received training from a senior health educator (S.P.) in behavior change theory and counseling, childhood obesity risk factors and management, providing family-centered care,24 motivational interviewing,25,26 and shared decision-making.27,28 Throughout the intervention period, the coaches meet regularly both together and individually with the senior health educator to discuss their coaching visits. To ensure fidelity to protocol and consistency across health coaches, a quality assurance protocol is being implemented to record and review participant visits. At two points in the intervention period, the health coaches will audio-record 10 visits, and these recordings will be reviewed by the senior health educator and assessed using a quality assurance checklist developed by our study team.
Following randomization, parents receive a mailed welcome brochure introducing them to the health coaching team. At the first contact, health coaches use the families’ residential address to tailor community-specific resources and connections. Following that first contact, parents begin to receive interactive text messages. Information about the text message platform, design and delivery are published elsewhere.29 Using an online community map developed for the study,30 health coaches identify resources for each family's community including social support services (i.e. Supplemental Nutrition Program for Women, Infants and Children offices), nutritional support (i.e. local farmers markets, supermarkets) and places for physical activity (i.e. Boys and Girls Clubs, swimming pools, recreation centers, ice rinks, and YMCAs). In addition, through a partnership with the YMCA, health coaches offer families a 1-month free family membership to area YMCAs to encourage physical activity and community connections. Families are also offered the opportunity to take part in a healthy grocery shopping program led by a community partner, Cooking Matters®, empowering families to cook healthy meals and learn ways to shop and eat on a limited budget.
Follow up visits are conducted using a family-centered approach, and include most of the following components: establishing rapport, summarizing the content of the last visit, following up on goals set, progress, setbacks, resources and text messages, reviewing study recommendations and setting new goal, identifying strategies/barriers/facilitators, continuing to build motivation, skills, and support, summarizing plans, and scheduling the next check in. Contact attempts and completed visits are logged in a study database by the health coaches. We measure the length of the visit, the mode of the visit and the time and date of the contact. At follow up visits, health coaches use a behavior change decision aid tool, developed by our study team, to engage parents and often their child as well (Figure 3). The tool, heavily informed by the experiences and best practices of positive outlier families, allows the health coaches to explore outcomes that matter most to families and potential motivators for engaging in behavior change. The tool was also meant to facilitate shared decision making to determine parents’ goals and “set the agenda” for health coaching. The health coaches then discuss recommendations for supporting behavior change to achieve each outcome of interest. Families are also asked to select behavioral goals that they are most interested in working on with their child. The health coach then discusses the behavior and the associated study recommendations, as well as tips for making changes to work towards the goal. Health coaches use a motivational interviewing counseling style to assist parents in realistic goal setting, make a plan for how to work towards the goal, and identify potential barriers to achieving the goal. At follow-up visits, health coaches re-establish rapport and check in on goals that families set and resources they provided to parents. Following each visit, the health coach mails the family a packet of educational materials. Mailings include issues of a healthy cooking magazine for children, handouts for parents about behavior change goals, as well as materials designed specifically for children. Intervention materials for children are tailored to their age. . Also following the visits, health coaches send out emails to parents receptive to this method of communication that are more personalized with resources tailored to the participants’ goals and community. Health coaches are also available to assist families with written applications and program enrollment, if requested.
Figure 3.
Health Coaching Tool Developed and Used with Families in the Connect for Health Intervention
Outcome Measures
The primary outcome of the intervention is 1-year change in child BMI (in kg/m2) obtained from the child's electronic health record from well-child care visits at enrollment and at 1-year. We will also examine change in BMI z-scores. In routine practice standardized across all 6 study sites, medical assistants measure children's weight, without shoes, using electronic, calibrated scales, and height using a stadiometer. We calculate BMI and age- and sex-specific BMI z-scores.31
We assess parent- and child-reported outcomes at baseline and at 1-year. (Table 1) Parent-reported outcomes are assessed using telephone surveys; child-reported outcomes are assessed among children ages 8-12 years using a mailed, written survey. Parents report their child's health-related quality of life using the 4 subscales of the PedsQL-4.0; children report their own quality of life using the child version of the PedsQL validated among children ages 8 and over.32,33 We measure parent- and child-report of children's sleep duration and routines, screen time, stress, and participation in moderate to vigorous physical activity as well as intakes of sugar-sweetened beverages, fruits and vegetables, and fast food. Parents self-report their height and weight at baseline and weight at follow up, their weight-related resource empowerment,34 and their rating of their child's obesity-related care using modified questions from the 20-item Patient Assessment of Chronic Illness Care survey.35
Exploratory Parent- and Child-Reported Outcome Measures
Based on formative, qualitative studies with parents and children, we developed 8 closed-ended questions for parents and 6 for children about the weight-related outcomes that mattered most to them. We asked parents, “How important is it to you for your child to...”, and asked children ages 8-12 years, “How important is it to you to...”. The 5 common parent- and child-reported items were are follows: (1) not be overweight; (2) not be bullied or teased; (3) fit into clothing for children his or her age; (4) be accepted by other children his or her age; and (5) avoid health problems like diabetes or heart disease. The parent items also included: feel happy with how he or she looks; learn to make healthy choices on his or her own, and keep up with other children when exercising or being active. The child survey included: be better at sports or exercise. We pilot-tested and finalized the items based on input from parents and children in our Parent and Youth Advisory Board. The parent items were measured using a 5-point Likert-type scale ranging from “not at all important” to “extremely important”. The child items were measured using a 4-point Likert-type scale ranging from “not at all important” to “totally important”.
Process Outcomes
To understand more fully the intervention effect, we will collect information on the acceptability, feasibility, uptake of components of the intervention (e.g. use of the YMCA family memberships), and family engagement in the study from the parent's and children's perspectives. We will measure the following implementation domains at 12 months: a) reach, b) extent of implementation, c) fidelity to protocol, d) parent and child satisfaction with multiple aspects of the intervention, and e) the extent that the intervention was family-centered.
Statistical Analysis
We will examine baseline distributions of participant characteristics by intervention status. Our primary analyses will be based on the principle of intent-to-treat so that all patients who are randomized will be included. We will examine the difference from baseline to 1 year between the intervention and control groups. For the continuous measures, we will develop linear regression models; for binary measures, we will start with Fisher exact tests and develop logistic regression models.
Power Estimations
Connect for Health intended to recruit a total of 750 children and their parents across 6 practices of HVMA between July 2014 and March 2015. Based on previous studies within this setting in which we achieved over 90% follow up at 1-year, we anticipate that 713 children will complete the study.14,36 The key variable for sample size calculations is the naturally occurring standard deviation in the change of BMI (in kg/m2) during a 12 month period. From a large population-based study the estimated standard deviation in BMI change was 0.96 for boys and 0.95 for girls.37 Based on prior work, we expect over 95% to have follow-up BMI measures, but will use a conservative 90% for power calculations (n=338 per arm). Based on these assumptions and a 5% Type I error, our study is powered at 90% to detect a difference between arms in the change in BMI as small as 0.24. Even in the unlikely case that follow-up retention is as low as 80%, we will still be able to detect a 0.26 point difference in BMI with 90% power. These intervention effects are sufficiently small to capture any clinically meaningful change in BMI as a result of our intervention, increasing the relevance of our study design to our partner health care systems.
For child health related quality of life, as measured by the PedsQL-4.0, a prior study shows a standard deviation of 9.7 for a 24-week change in quality of life. 38 If we assume the same standard deviation in this study, 90% follow-up (n=338/arm) and a Type I error of 5%, then we will have 90% power as long as the intervention children improve by at least 2.5 points while the control children's quality of life remains constant. Even if the follow-up rate is as low as 80%, we will still have 90% power as long as the intervention children have at least a 3-point improvement. We believe that this magnitude of improvement is reasonable to expect given similar previous interventions that achieved 5 to 7.5 point improvement.38,39
DISCUSSION
The Connect for Health study is a randomized controlled trial designed to assess whether a novel approach to care delivery that leverages clinical and community resources and addresses socio-contextual factors will improve child BMI and family-centered, obesity-related outcomes of interest to parents and children. Connect for Health was developed and is continually informed by input from a diverse group of stakeholders representing children, parents, community and public health providers, as well as pediatric primary care clinicians. In particular, the study is implementing best practices of positive outlier children and families who successfully improved their BMI through behavior change and clinical-community supports. If successful, this study can provide the foundation for a widely disseminated, family-centered model of obesity management that maximally leverages clinical and community resources.
As with any large study, this one is subject to potential challenges. The family-centered approach and tailoring to match family preferences requires flexibility and the resources to provide families with multiple options to meet their needs. If successful, however, and after the groundwork is laid, this flexibility and practical approach may keep families more engaged in the intervention. Such a practical approach has been increasingly recognized as a way to ensure relevance of study findings to families, clinicians and other stakeholder and to help reduce the gap between research and practice.40 Another challenge will be to accurately and reliably measure parent- and child-report of quality of life and behaviors. To the extent possible, we are using reliable, validated measures for our parent- and child-reported outcomes. However, in some cases, validated measures do not exist that capture outcomes that matter most to children, e.g. fitting into clothing, or parents, e.g. having their child “fit in” with other children their age. Pediatric patient reported outcomes in chronic diseases are becoming increasingly available and thus the outcomes we propose may be easier to measure in the future.
Supplementary Material
ACKNOWLEDGEMENTS
The authors would like to thank the providers and staff at Harvard Vanguard Medical Associates for their ongoing collaboration in pediatric obesity research efforts. We would like to thank the clinical research coordinators Kelsey Nichols, Jaymi Cohen, Dominique Dupont-Dubois, Savannah Vicente, Andrew Shawhan and Bianca Verma as well as health coaches Caitlin Perry, Gabriella Puente and Katie Garneau for their assistance with the study. We thank the parents and children who serve on our advisory boards and offered their input to help shape the intervention. And lastly, we thank our community partners, Cooking Matters and multiple area YMCAs, for making their resources available to study participants.
Funding Acknowledgement:
This work was supported through a Patient-Centered Outcomes Research Institute (PCORI) Award (IH-1304-6739). Dr. Sharifi is supported by an AHRQ Mentored Career Development Award for Child and Family Centered Outcomes Research (1 K12 HS 022986-01). None of the authors have conflicts of interest to declare.
Abbreviations
- BMI
body mass index
- GIS
geographic information systems
Footnotes
ClinicalTrials.gov Identifier: NCT02124460
Disclaimer:
All statements in this report, including its findings and conclusions, are solely those of the authors and do not necessarily represent the views of the Patient-Centered Outcomes Research Institute (PCORI), its Board of Governors or Methodology Committee
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014 Feb 26;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Olds T, Maher C, Zumin S, et al. Evidence that the prevalence of childhood overweight is plateauing: data from nine countries. International journal of pediatric obesity : IJPO : an official journal of the International Association for the Study of Obesity. 2011 Oct;6(5-6):342–360. doi: 10.3109/17477166.2011.605895. [DOI] [PubMed] [Google Scholar]
- 3.Dietz WH, Baur LA, Hall K, et al. Management of obesity: improvement of health-care training and systems for prevention and care. Lancet. 2015 Feb 18; doi: 10.1016/S0140-6736(14)61748-7. [DOI] [PubMed] [Google Scholar]
- 4.Smedley B, Syme S, Institute of Medicine . Promoting health: intervention strategies from social and behavioral research. National Academies Press; Washington, DC: 2000. Committee on capitalizing on social science and behavioral research to improve the public's health. [PubMed] [Google Scholar]
- 5.Papas MA, Alberg AJ, Ewing R, Helzlsouer KJ, Gary TL, Klassen AC. The built environment and obesity. Epidemiol Rev. 2007;29:129–143. doi: 10.1093/epirev/mxm009. [DOI] [PubMed] [Google Scholar]
- 6.Fiechtner L, Block J, Duncan DT, et al. Proximity to supermarkets associated with higher body mass index among overweight and obese preschool-age children. Preventive medicine. 2013 Mar;56(3-4):218–221. doi: 10.1016/j.ypmed.2012.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Duncan DT, Sharifi M, Melly SJ, et al. Characteristics of walkable built environments and BMI z-scores in children: evidence from a large electronic health record database. Environmental health perspectives. 2014 Dec;122(12):1359–1365. doi: 10.1289/ehp.1307704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Christine PJ, Auchincloss AH, Bertoni AG, et al. Longitudinal Associations Between Neighborhood Physical and Social Environments and Incident Type 2 Diabetes Mellitus: The Multi-Ethnic Study of Atherosclerosis (MESA). JAMA internal medicine. 2015 Jun 29; doi: 10.1001/jamainternmed.2015.2691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fleegler EW, Lieu TA, Wise PH, Muret-Wagstaff S. Families’ health-related social problems and missed referral opportunities. Pediatrics. 2007 Jun;119(6):e1332–1341. doi: 10.1542/peds.2006-1505. [DOI] [PubMed] [Google Scholar]
- 10.Bradley EH, Curry LA, Ramanadhan S, Rowe L, Nembhard IM, Krumholz HM. Research in action: using positive deviance to improve quality of health care. Implement Sci. 2009;4:25. doi: 10.1186/1748-5908-4-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sharifi M, Marshall G, Marshall R, et al. Accelerating progress in reducing childhood obesity disparities: exploring best practices of positive outliers. Journal of health care for the poor and underserved. 2013;24(2 Suppl):193–199. doi: 10.1353/hpu.2013.0099. [DOI] [PubMed] [Google Scholar]
- 12.Sharifi M, Marshall G, Goldman R, et al. Exploring innovative approaches and patient-centered outcomes from positive outliers in childhood obesity. Academic pediatrics. 2014 Nov-Dec;14(6):646–655. doi: 10.1016/j.acap.2014.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sharifi M, Marshall G, Goldman RE, Cunningham C, Marshall R, Taveras EM. Engaging children in the development of obesity interventions: Exploring outcomes that matter most among obesity positive outliers. Patient Education and Counseling. 2015 doi: 10.1016/j.pec.2015.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Taveras EM, Marshall R, Kleinman KP, et al. Comparative effectiveness of childhood obesity interventions in pediatric primary care: a cluster-randomized clinical trial. JAMA pediatrics. 2015 Jun 1;169(6):535–542. doi: 10.1001/jamapediatrics.2015.0182. [DOI] [PubMed] [Google Scholar]
- 15.Guise JM, O'Haire C, McPheeters M, et al. A practice-based tool for engaging stakeholders in future research: a synthesis of current practices. Journal of clinical epidemiology. 2013 Jun;66(6):666–674. doi: 10.1016/j.jclinepi.2012.12.010. [DOI] [PubMed] [Google Scholar]
- 16.Patient Centered Outcomes Research Institute Methology Committee . PCORI Methodology Standards. Washington, DC: 2012. (as adopted by the PCORI Board, Nov. 19; published Dec. 14) [Google Scholar]
- 17.Ponte PR, Conlin G, Conway JB, et al. Making patient-centered care come alive: achieving full integration of the patient's perspective. The Journal of nursing administration. 2003 Feb;33(2):82–90. doi: 10.1097/00005110-200302000-00004. [DOI] [PubMed] [Google Scholar]
- 18.Domecq JP, Prutsky G, Elraiyah T, et al. Patient engagement in research: a systematic review. BMC health services research. 2014;14:89. doi: 10.1186/1472-6963-14-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Concannon TW, Fuster M, Saunders T, et al. A systematic review of stakeholder engagement in comparative effectiveness and patient-centered outcomes research. Journal of general internal medicine. 2014 Dec;29(12):1692–1701. doi: 10.1007/s11606-014-2878-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Frank L, Forsythe L, Ellis L, et al. Conceptual and practical foundations of patient engagement in research at the patient-centered outcomes research institute. Qual Life Res. 2015 Jan 6; doi: 10.1007/s11136-014-0893-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sequist TD, Taveras EM. Clinic-community linkages for high-value care. The New England journal of medicine. 2014 Dec 4;371(23):2148–2150. doi: 10.1056/NEJMp1408457. [DOI] [PubMed] [Google Scholar]
- 22.Taveras EM, Marshall R, Horan CM, et al. Improving children's obesity-related health care quality: process outcomes of a cluster-randomized controlled trial. Obesity (Silver Spring, Md.) 2014 Jan;22(1):27–31. doi: 10.1002/oby.20612. [DOI] [PubMed] [Google Scholar]
- 23. [August 11, 2015];Let's Move! America's Move to Raise a Healthier Generation of Kids. http://www.letsmove.gov/.
- 24.Wells N, Bronheim S, Zyzanski S, Hoover C. Psychometric Evaluation of a Consumer-Developed Family-Centered Care Assessment Tool. Maternal and child health journal. 2015 Apr 8; doi: 10.1007/s10995-015-1709-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Miller WR, Rollnick S. Motivational Interviewing- Motivational Enhancement Therpy. 2002 [Google Scholar]
- 26.Rollnick S, Miller William R, Butler CC. Motivational Interviewing in Health Care: Helping Patients Change Behavior. Taylor & Francis Group; 2008. [Google Scholar]
- 27.Stacey D, Bennett CL, Barry MJ, et al. Decision aids for people facing health treatment or screening decisions. The Cochrane database of systematic reviews. 2011;(10):CD001431. doi: 10.1002/14651858.CD001431.pub3. [DOI] [PubMed] [Google Scholar]
- 28.Braddock CH, 3rd, Edwards KA, Hasenberg NM, Laidley TL, Levinson W. Informed decision making in outpatient practice: time to get back to basics. JAMA : the journal of the American Medical Association. 1999 Dec 22-29;282(24):2313–2320. doi: 10.1001/jama.282.24.2313. [DOI] [PubMed] [Google Scholar]
- 29.Price S, Ferisin S, Sharifi M, et al. Development and Implementation of an Interactive Text Messaging Campaign to Support Behavior Change in a Childhood Obesity Randomized Controlled Trial. Journal of health communication. 2015 Jul;20(7):843–850. doi: 10.1080/10810730.2015.1018582. [DOI] [PubMed] [Google Scholar]
- 30.Fiechtner L, Sharifi M, Marshall R, et al. Use of geographic information systems and electronic health records to integrate primary care with community assets to reduce childhood obesity.. Oral Presentation at The Obesity Society annual meeting; November 2014.2014. [Google Scholar]
- 31.Kuczmarski RJ, Ogden CL, Guo SS, et al. CDC Growth Charts for the United States: methods and development. Vital and health statistics. Series 11, Data from the national health survey. 2000 May;2002(246):1–190. [PubMed] [Google Scholar]
- 32.Varni JW, Limbers CA, Burwinkle TM. Parent proxy-report of their children's health-related quality of life: an analysis of 13,878 parents’ reliability and validity across age subgroups using the PedsQL 4.0 Generic Core Scales. Health and quality of life outcomes. 2007;5:2. doi: 10.1186/1477-7525-5-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Varni JW, Limbers CA, Burwinkle TM. How young can children reliably and validly self-report their health-related quality of life?: an analysis of 8,591 children across age subgroups with the PedsQL 4.0 Generic Core Scales. Health and quality of life outcomes. 2007;5:1. doi: 10.1186/1477-7525-5-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jurkowski JM, Lawson HA, Green Mills LL, Wilner PG, 3rd, Davison KK. The empowerment of low-income parents engaged in a childhood obesity intervention. Family & community health. 2014 Apr-Jun;37(2):104–118. doi: 10.1097/FCH.0000000000000024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Glasgow RE, Wagner EH, Schaefer J, Mahoney LD, Reid RJ, Greene SM. Development and validation of the Patient Assessment of Chronic Illness Care (PACIC). Medical care. 2005 May;43(5):436–444. doi: 10.1097/01.mlr.0000160375.47920.8c. [DOI] [PubMed] [Google Scholar]
- 36.Taveras EM, Gortmaker SL, Hohman KH, et al. Randomized controlled trial to improve primary care to prevent and manage childhood obesity: the High Five for Kids study. Archives of pediatrics & adolescent medicine. 2011 Aug;165(8):714–722. doi: 10.1001/archpediatrics.2011.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wen X, Gillman MW, Rifas-Shiman SL, Sherry B, Kleinman K, Taveras EM. Decreasing prevalence of obesity among young children in Massachusetts from 2004 to 2008. Pediatrics. 2012 May;129(5):823–831. doi: 10.1542/peds.2011-1833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Foster GD, Sundal D, McDermott C, Jelalian E, Lent MR, Vojta D. Feasibility and preliminary outcomes of a scalable, community-based treatment of childhood obesity. Pediatrics. 2012 Oct;130(4):652–659. doi: 10.1542/peds.2012-0344. [DOI] [PubMed] [Google Scholar]
- 39.Yackobovitch-Gavan M, Nagelberg N, Demol S, Phillip M, Shalitin S. Influence of weight-loss diets with different macronutrient compositions on health-related quality of life in obese youth. Appetite. 2008 Nov;51(3):697–703. doi: 10.1016/j.appet.2008.06.010. [DOI] [PubMed] [Google Scholar]
- 40.Glasgow RE, Magid DJ, Beck A, Ritzwoller D, Estabrooks PA. Practical clinical trials for translating research to practice: design and measurement recommendations. Medical care. 2005 Jun;43(6):551–557. doi: 10.1097/01.mlr.0000163645.41407.09. [DOI] [PubMed] [Google Scholar]
- 41.Feskanich D, Hastrup JL, Marshall JR, et al. Stress and suicide in the Nurses’ Health Study. Journal of epidemiology and community health. 2002 Feb;56(2):95–98. doi: 10.1136/jech.56.2.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Taveras EM, Rifas-Shiman SL, Oken E, Gunderson EP, Gillman MW. Short sleep duration in infancy and risk of childhood overweight. Archives of pediatrics & adolescent medicine. 2008 Apr;162(4):305–311. doi: 10.1001/archpedi.162.4.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bell JF, Zimmerman FJ. Shortened nighttime sleep duration in early life and subsequent childhood obesity. Arch Pediatr Adolesc Med. 2010 Sep;164(9):840–845. doi: 10.1001/archpediatrics.2010.143. [DOI] [PubMed] [Google Scholar]
- 44.Lumeng JC, Somashekar D, Appugliese D, Kaciroti N, Corwyn RF, Bradley RH. Shorter sleep duration is associated with increased risk for being overweight at ages 9 to 12 years. Pediatrics. 2007 Nov;120(5):1020–1029. doi: 10.1542/peds.2006-3295. [DOI] [PubMed] [Google Scholar]
- 45.Chervin RD, Hedger K, Dillon JE, Pituch KJ. Pediatric sleep questionnaire (PSQ): validity and reliability of scales for sleep-disordered breathing, snoring, sleepiness, and behavioral problems. Sleep Med. 2000 Feb 1;1(1):21–32. doi: 10.1016/s1389-9457(99)00009-x. [DOI] [PubMed] [Google Scholar]
- 46.Crosby B, LeBourgeois MK, Harsh J. Racial differences in reported napping and nocturnal sleep in 2- to 8-year-old children. Pediatrics. 2005 Jan;115(1 Suppl):225–232. doi: 10.1542/peds.2004-0815D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Robinson TN. Reducing children's television viewing to prevent obesity: a randomized controlled trial. JAMA. 1999;282:1561–1567. doi: 10.1001/jama.282.16.1561. [DOI] [PubMed] [Google Scholar]
- 48.Roberts DR, Foehr UG, Rideout VJ, Brodie M, Henry J, Kaiser Family Foundation . Kids and Media in America. Cambridge University Press; New York: 2004. [Google Scholar]
- 49.Hoelscher D, Day R, Kelder S, Ward J. Reproducibility and validity of the secondary level School-Based Nutrition Monitoring student questionnaire. Journal of the American Dietetic Association. 2003;103(2):186–194. doi: 10.1053/jada.2003.50031. [DOI] [PubMed] [Google Scholar]
- 50.Thiagarajah K, Fly A, Hoelscher D, et al. Validating the food behavior questions from the elementary school SPAN questionnaire. Journal of Nutrition Education and Behavior. 2008;40(5):305–310. doi: 10.1016/j.jneb.2007.07.004. [DOI] [PubMed] [Google Scholar]
- 51.Taveras EM, Berkey CS, Rifas-Shiman SL, et al. Association of Consumption of Fried Food Away From Home With Body Mass Index and Diet Quality in Older Children and Adolescents. Pediatrics. 2005 Oct 1;116(4):e518–524. doi: 10.1542/peds.2004-2732. 2005. [DOI] [PubMed] [Google Scholar]
- 52.Helmerhorst HJ, Brage S, Warren J, Besson H, Ekelund U. A systematic review of reliability and objective criterion-related validity of physical activity questionnaires. The international journal of behavioral nutrition and physical activity. 2012;9:103. doi: 10.1186/1479-5868-9-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.