Abstract
Purpose
To contrast rates of initial HPV vaccine uptake, offered at no cost, between a rural clinic, a rural community college, and an urban college clinic and to identify rural versus urban differences in uptake of free booster doses.
Methods
Young rural women attending rural clinics (n = 246), young women attending a rural community college (n = 251) and young women attending an urban university health clinic (n = 209) were recruited in Kentucky. After completing a brief questionnaire, women received a free voucher for HPV vaccination. Whether women redeemed the voucher for the initial dose of vaccine served as the study outcome variable.
Findings
In controlled analyses, the contrast in initial uptake between urban clinic women (reference category) and rural college women was significant (P < .0001). However, the contrast in initial uptake between urban clinic women (reference category) and rural clinic women was not significant (P = .42). The model predicting uptake of subsequent doses among those with initial uptake (n = 235) also indicated significant differences as a function of recruitment location, with rural clinic women being about 7 times more likely than urban clinic women (P < .0001) to not return for at least 1 follow-up dose. The contrast between urban clinic women and rural college women was also significant (P = .014).
Conclusion
Initial uptake of free HPV vaccination among young rural college women may be problematic. Moreover, uptake of subsequent free doses among rural women may be problematic regardless of whether contact is made in a clinic or through college recruitment.
Keywords: cervical cancer, Gardasil, HPV vaccine, rural, young women
Human Papillomavirus (HPV) vaccination is approved and recommended for use in females from 9 to 26 years of age.1 The vaccine protects against HPV types 16 and 18, which are implicated in about two-thirds of cervical cancers.1 The Advisory Committee on Immunization Practices (ACIP) recommends “catch-up vaccination” for females 13–26 years of age.1 Unfortunately, little research has been focused upon women in the higher end of this “catch-up” age range (ie, 18–26 years of age). Indeed, the extant research on behavioral acceptance of the vaccine is primarily centered on younger girls, with studies of older girls being restricted to intent rather than actual uptake.2–7 Thus, one potentially timely and important research question involves the actual uptake of the vaccine by older girls/young women.
From a behavioral perspective, the challenges associated with initial uptake (dose 1) of the HPV vaccine may be quite different from those associated with receipt of subsequent doses (dose 2 at 2 months and dose 3 at 6 months). One general factor that may be an important determinant of uptake is rural versus urban residence. In fact, related evidence suggests that rural health disparities may function with respect to cervical cancer prevention.8–10 Accordingly, the purpose of this study was to contrast rates of HPV vaccine uptake between young women recruited from 2 rural locations and 1 urban location. We hypothesized that uptake would be significantly lower among women recruited in the rural locations, even after controlling for rural upbringing and other potentially confounding variables.
Methods
Study Sample
Using the Beale codes from the Economic Research Service,11 our urban location was ranked as “2” meaning that it is a county in a metro area of 250,000 to 1 million people. By contrast, our selected rural counties had Beale codes ranging from “7” through the most rural designation of “9.” A code of 7 designates the county as having a population of less than 20,000 people and being non-adjacent to a metropolitan area.
Urban Recruitment
From October 2007 through May of 2008 research assistants recruited women attending the University Health Service at the University of Kentucky. Recruitment occurred in the waiting area reserved for women seeking routine gynecological care. Women were eligible to participate if they were 18 to 24 years old and had not been vaccinated with Gardasil (the only HPV vaccine approved for use at the time). Because doses 2 and 3 were, for some women, due during summer months, eligibility was also restricted to women indicating they lived within a 50-mile radius of the university. Of 231 eligible women, 209 (90.9%) agreed to participate in the study and provided written informed consent.
Rural Recruitment
Two locations were used: a rural clinic and a rural community college. Both locations were in southeastern Kentucky—an area of rural Appalachia characterized by a predominately white population, poverty, and medially underserved residents.12 The selected area of Kentucky has also experienced a high rate of cervical cancer incidence. From 2003–2007, the age-adjusted incidence rate for cervical cancer in Kentucky was 9.22 per 100,000; the US age-adjusted rate for the same time period was 8.1. The age-adjusted incidence rate for cervical cancer in Appalachia Kentucky was 10.78 and the age-adjusted incidence rate for cervical cancer in the selected study area was 9.25.13
From March 2008 through September 2009, a research assistant recruited female patients in any of 5 regional health clinics located in 5 rural counties of southeastern Kentucky. During that same time period, a second research assistant recruited women attending a local community college (with buildings located in 4 of the same 5 counties used for the clinic sample). Women were eligible if they were not pregnant, 18–26 years old, and had not been vaccinated with Gardasil. Of 505 eligible women, 495 (98%) agreed to participate in the study and provided written informed consent. Of these, 246 were recruited from clinics and 251 were recruited from the community college. The Institutional Review Board at the University of Kentucky approved the study protocols.
Procedures
Recent findings suggest that insurance coverage14–16 and cost17 may be strongly associated with initial uptake. Thus, to control for these “cost” factors we determined that a study providing the vaccine for free was needed. In essence, because Gardasil was not universally covered by insurance plans, the cost barrier was removed to more effectively test the study hypothesis. However, the fact that Gardasil would be provided at no cost was not advertised or disclosed until after the questionnaire was completed and young women were compensated for their time. To avoid self-selection bias, the project was called the Women’s Health Study. Women completed a brief questionnaire and they were compensated for their time. After being compensated, the research assistant provided women with a voucher to receive free Gardasil at the clinic they were recruited from or, in the case of college women, a centrally located clinic. These coupons were coded with ID numbers that matched the ID numbers recorded on the women’s questionnaires. Redeemed coupons were used to create a freestanding set of medical records indicating Gardasil uptake.
Data Analysis
The descriptive analysis comparing uptake across the 3 recruitment sites was based on 3 × 2 chi-square tests, with 2 × 2 chi-square tests being conducted on a post hoc basis following a significant P value on a 3 × 2 test. To test the study hypothesis, we included a measure of rural upbringing (not always the same as rural residence) as a control variable. Young women were asked the following question. “When you were a high school student, about how large was your hometown?” Five response options were provided ranging from (1) a “large city (like Chicago, New York) or the suburban area around it” to (5) rural area. In addition to age, 3 other key variables were assessed as potential covariates: ever having an abnormal Pap test result, belief that mother “would definitely” want the daughter to be vaccinated, and belief that father “would definitely” want the daughter to be vaccinated. These 3 covariates were selected based on findings from HPV vaccine uptake studies previously published.14,17–19
Hierarchal logistic regression was used to control for rural upbringing and the other assessed covariates which differed between young women in the recruitment locations. The first block contained the control variables and the second block contained only the variable representing recruitment location. Two models were created. The first predicted initial uptake of the vaccine (dose 1). The second model predicted follow-up vaccination among those taking dose 1.
Results
Descriptive Findings
Figure 1 displays the uptake rates for each of 3 doses and each of the 3 recruitment sites. As shown, dose 1 uptake was greatest among women recruited in the urban clinic (50.7%), followed by women recruited in the rural clinic (45.1%) and those recruited from the rural college (6.8%). Dose 2 uptake was also greatest among women from the urban clinic (39.7%), followed by women from the rural clinic (13.8%) and the rural college (2.8%). Dose 3 uptake was also greatest among women from the urban clinic (28.2%), with uptake rates from the rural clinic women (4.5%) and the rural college women (1.6%) being equally low (non-significant). With only 2 exceptions the differences in the uptake of each dose, across all 3 samples, were statistically significant (P < .001). The first exception was dose 1 in the urban clinic compared to dose 1 in the rural clinic—the difference of 5.6% was not significant by chi-square test results (P = .27). The second exception was for dose 3 in the rural clinic (4.5%) versus the rural college (1.6%)—due to low numbers this difference was also not significant by chi-square test results (P = .06).
Figure 1.
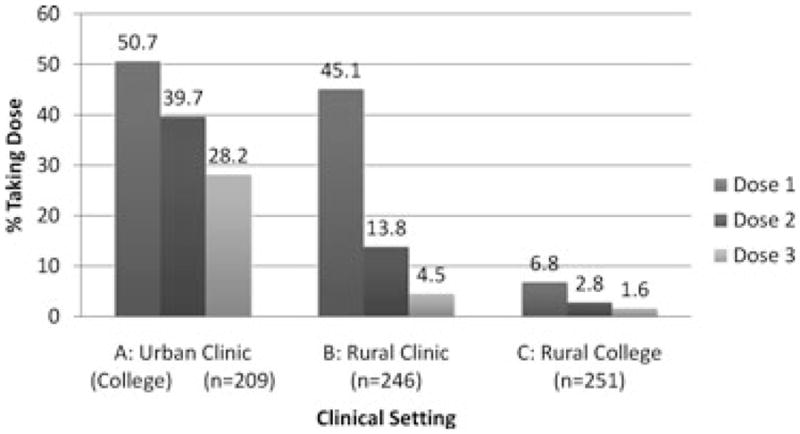
HPV Vaccine Data by Setting
Bivariate Associations
As established in the descriptive findings shown above, recruitment location was significantly associated with initial uptake (dose 1) of the vaccine when contrasting the rural college women to the urban clinic women and when contrasting the rural clinic women to the rural college women. Differences between urban clinic women and rural clinic women were not observed (P = .27). In addition, recruitment location was significantly associated with return for at least one follow-up dose of the vaccine when contrasting the rural college women (41.2%) to the urban clinic women (78.5%) (P < .001) and when contrasting the rural clinic women (30.6%) to the urban clinic women (78.5%) (P < .001). Differences between the rural clinic women (30.6%) and the urban clinic women (78.5%) were not observed (P = .39).
Rural upbringing was significantly associated with uptake (P < .0001). Uptake for those not having a rural upbringing was 39.0%, whereas uptake was 26.6% among those who reported a rural upbringing. Return for subsequent doses was also significantly more likely (P = .005) for women without a rural upbringing (60.4% of those receiving dose 1 returned for one or both booster doses) compared to women reporting a rural upbringing (41.8% of those receiving dose 1 returned for one or both booster doses).
Age, belief that mother “would definitely” want the daughter to be vaccinated, belief that father “would definitely” want the daughter to be vaccinated, and ever having an abnormal Pap test result were each analyzed using 3 × 2 chi-square tests for their association with the variable representing the 3 recruitment locations. Differences for age (P < .001), mothers’ endorsement (P = .03), and fathers’ endorsement (P = .004) were observed. Differences relative to ever having an abnormal Pap test result were not observed (P = .19). Thus, the multivariate models were constructed to control for rural upbringing, age, mothers’ endorsement, and fathers’ endorsement.
Multivariate Associations
The model predicting initial uptake (n = 710) was significant (chi-square with 4df = 173.5, P < .0001) and achieved an excellent fit with the data (Goodness of fit chi-square with 3 df = 3.73, P = .88). Other than mothers’ endorsement (AOR = .37; 95% CI, 0.26–0.54; P < .0001) none of the other covariates obtained multivariate significance. Recruitment location was significant for the contrast between urban clinic women (reference category) and rural college women (AOR = 13.10; 95% CI, 7.3–23.4; P < .0001). However, the contrast between urban clinic women (reference category) and rural clinic women was not significant (AOR = 1.18; 95% CI, 0.79–1.78; P = .42).
The model predicting subsequent doses among those with initial uptake (n = 235) was significant (chi-square with 4 df = 60.8, P < .0001) and achieved satisfactory fit with the data (Goodness of fit chi-square with 7 df = 4.03, P = .78). The effect of age was significant (AOR = 1.21; 95% CI, 1.05–1.39; P = .009), with older women being less likely to return for follow-up doses. None of the other covariates obtained multivariate significance. Again, however, recruitment location was significant, with rural clinic women being about 7 times more likely than urban clinic women (AOR = 6.98; 95% CI, 3.61–13.48; P < .0001) to not return for at least one follow-up dose. The contrast between urban clinic women and rural college women was also significant (AOR = 4.20; 95% CI, 1.33–13.23; P = .014).
Discussion
In an era of intensified government enthusiasm for prevention as a solution to escalating health care costs, the observed rate of vaccine uptake among young rural women (a population recognized for cervical cancer disparities) is disheartening. It appears that offering the vaccine for free is not enough; it must also be convenient and this factor may be lacking in rural areas. The extremely large discrepancy in initial uptake between women recruited from the 2 clinics and those recruited from community college demonstrates this point about convenience. Clearly, the greater initial uptake observed among clinic-recruited women is potentially attributable to a convenience factor. This convenience factor, of course, applied only to dose 1 and it explains the lack of significance between initial uptake in the rural versus the urban clinic. In essence, the convenience factor negated the “rural factor.”
Because we controlled for the influence of rural versus urban upbringing, and other likely confounding variables, it is fair to speculate that the observed dramatic differences in subsequent vaccine uptake are attributable to the rural factor. Rural clinic-recruited women as well as rural college-recruited women were significantly less likely to return for subsequent doses, even after controlling for the assessed covariates. Although there is no doubt that an endless number of differences may exist between rural and urban women, “teasing out” these differences is not a necessary exercise to promote completion of HPV vaccine series. It is, in fact, the case that intensified efforts are required to continue the vaccine series among rural women.
One possible explanation for vaccine uptake issues in rural areas is distance to the clinic. Distance may indeed be a key factor in the observed drop from 40% dose 2 uptake in the urban clinic to just under 14% in the rural clinic and not even 3% in the sample of rural college students. The drop was even more dramatic when considering dose 3. However, we hesitate to speculate as to why the return for dose 2 was so much higher for rural women recruited from the clinic versus rural women recruited from the community college. Of course, it is possible that women recruited from the clinic had a proclivity for health care and that proclivity also applied to vaccination.
Findings are limited by the use of a convenience sample and the validity of the self-reported data pertaining to rural upbringing. It is, however, well worth noting that our use of coded coupons to collect the primary outcome variable (ie, vaccine uptake) is a clear asset to the rigor of this study. The study findings represent the first comparison of Gardasil uptake between young women residing in rural areas versus their urban counterparts. Although more in-depth investigation is required, the results provide an early demonstration suggesting that rural health disparities extend to the somewhat simplistic health behavior of HPV vaccination. This disparity may be resolved, in part, by making the vaccine available at easy-to-access locations (eg, larger grocery stores and community events) in rural communities.
Acknowledgments
This study was funded, in part, by a grant from Merck Pharmaceuticals. This publication was also supported by Cooperative Agreement Number 1U48DP001932-01 from the Centers for Disease Control and Prevention. The findings and conclusions in this article are those of the author(s) and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- 1.Markowitz LE, Dunne EF, Saraiya M, et al. Quadrivalent human Papillomavirus vaccine: recommendations of the advisory committee on immunization practices. Morb Mort Wkly Rev. 2007;56:1–24. [PubMed] [Google Scholar]
- 2.Jain N, Euler GL, Shefer A, Lu P, Yankey D, Markowitz L. Human papillomavirus (HPV) awareness and vaccination initiation among women in the United States, National Immunization Survey-Adult 2007. Prev Med. 2009;48:426–431. doi: 10.1016/j.ypmed.2008.11.010. [DOI] [PubMed] [Google Scholar]
- 3.Zimet GD. Improving adolescent health: focus on HPV vaccine acceptance. J Adolesc Health. 2005;37:S17–S23. doi: 10.1016/j.jadohealth.2005.09.010. [DOI] [PubMed] [Google Scholar]
- 4.Zimet G, Mays RM, Fortenberry JD. Vaccines against sexually transmitted infections: promise and problems of the magic bullets for prevention and control. Sex Transm Dis. 2000;27(1):49–52. doi: 10.1097/00007435-200001000-00010. [DOI] [PubMed] [Google Scholar]
- 5.Crosby RA, Schoenberg N, Hopenhayn C, et al. Correlates of intent to be vaccinated against HPV: an exploratory study of college-age women. Sex Health. 2007;4:71–73. doi: 10.1071/sh06046. [DOI] [PubMed] [Google Scholar]
- 6.Zimet GD, Shew ML, Kahn JA. Appropriate use of cervical cancer vaccine. Annu Rev Med. 2008;59:223–236. doi: 10.1146/annurev.med.59.092806.131644. [DOI] [PubMed] [Google Scholar]
- 7.Brabin L, Roberts SA, Stretch R, et al. Uptake of first two doses of human Papillomavirus vaccine by adolescent schoolgirls in Manchester: prospective cohort study. BMJ. 2008;336:1056–1058. doi: 10.1136/bmj.39541.534109.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Benard V, Coughlin SS, Thompson T, et al. Cervical cancer incidence in the United States by area of residence, 1998–2001. Obstet Gynecol. 2007;110:681–686. doi: 10.1097/01.AOG.0000279449.74780.81. [DOI] [PubMed] [Google Scholar]
- 9.Freeman HP, Wingrove BK. Excess Cervical Cancer Mortality: A Marker of Low Access To Health Care In Poor Communities. Rockville, MD: National Cancer Institute, Center to Reduce Cancer Health Disparities; 2005. [Google Scholar]
- 10.Akers AY, Newmann SJ, Smith JS. Factors underlying disparities in cervical cancer incidence, screening, and treatment in the United States. Curr Probl Cancer. 2007;31:157–181. doi: 10.1016/j.currproblcancer.2007.01.001. [DOI] [PubMed] [Google Scholar]
- 11.Economic Research Service. [Accessed November 3, 2010];Rural-Urban Continuum Codes. Available at: http://www.ers.usda.gov/Data/RuralUrbanContinuumCodes/2003/LookUpRUCC.asp?C=R&S=KY.
- 12.Isserman A, Rephann T. The economic effects of the Appalachian Regional Commission: An empirical assessment of 26 years of regional development planning. J Am Planning Assoc. 1995;61:345–364. [Google Scholar]
- 13.Registry, Kentucky Cancer. [Accessed September 8, 2009];Cancer Incidence and Mortality Rates in Kentucky. 2010 Available at: http://www.kcr.uky.edu/
- 14.Conroy K, Rosenthal SL, Zimet GD, et al. Human papillomavirus vaccine uptake, predictors of vaccination, and self-reported barriers to vaccination. J Women’s Health. 2009;18(10):1679–1686. doi: 10.1089/jwh.2008.1329. [DOI] [PubMed] [Google Scholar]
- 15.Neubrand TP, Breitkopf CR, Rupp R, et al. Factors associated with completion of the human papillomavirus vaccine series. Clin Pediatr. 2009;48(9):966–969. doi: 10.1177/0009922809337534. [DOI] [PubMed] [Google Scholar]
- 16.Jain N, Euler G, Shefer A, et al. Human papillomavirus (HPV) awareness and vaccination initiation among women in the United States National Immunization Survey—Adult 2007. Prev Med. 2009;48:426–431. doi: 10.1016/j.ypmed.2008.11.010. [DOI] [PubMed] [Google Scholar]
- 17.Caskey R, Lindau ST, Alexander GC. Knowledge and early adoption of the HPV vaccine among girls and young women: results of a national survey. J Adolesc Health. 2009;45:453–462. doi: 10.1016/j.jadohealth.2009.04.021. [DOI] [PubMed] [Google Scholar]
- 18.Roberts ME, Gerrard M, Reimer R, Gibbons FX. Mother–daughter communication and human papillomavirus vaccine uptake by college students. Pediatrics. 2010;125:982–989. doi: 10.1542/peds.2009-2888. [DOI] [PubMed] [Google Scholar]
- 19.Moore GR, Crosby RC, Charnigo R, Young A. Low rates of free human Papillomavirus among young women. Sex Health. 2010;7:287–290. doi: 10.1071/SH09136. [DOI] [PubMed] [Google Scholar]


