Abstract
Objective
Previous intervention research conducted in Appalachian Kentucky resulted in extremely low uptake and adherence to the human papillomavirus (HPV) vaccine among women ages 18 –26, despite provision of free vaccine. Because of these findings, the purpose of this qualitative, follow-up study was to elicit health care providers' perspectives on barriers and facilitators to HPV vaccination and suggested strategies for improving vaccination rates.
Design and Sample
Researchers conducted semi-structured qualitative interviews with a purposive sample of eight health care providers (seven nursing professionals, one physician) at the health clinic where the original HPV vaccination intervention took place. Interviews were audio-recorded and transcribed and authors used a constant-comparative method to analyze the data.
Results
Significant themes emerged from the interviews, centering around two primary issues: vaccine uptake and vaccine adherence. Related to uptake, health care providers identified perceived patient barriers and inadequate HPV vaccine education. They also identified the vaccine schedule and clinic-centered communication deficiencies as adherence-related barriers.
Conclusion
These Appalachian Kentucky health care providers provided important insights into barriers and facilitators to HPV vaccine uptake and adherence that need to be readily addressed in this community. As informed by these providers, several suggestions for improving HPV vaccination, such as more targeted education efforts and patient-centered reminder systems, may be applicable to other nursing professionals working in rural and medically underserved communities.
Keywords: cancer, health behaviors, immunization, perceptions, qualitative research, rural health, women’s health
Uptake and adherence to the three-dose human papillomavirus (HPV) vaccine remains low, which is particularly concerning for communities that shoulder an excessive burden of cervical cancer and have limited access to health care, such as Appalachian Kentucky. A previous intervention study conducted in this geographic region revealed low HPV vaccination rates among young women ages 18–26, despite waiving the cost of the vaccine series. The current study serves as a qualitative follow-up to this previous intervention research, seeking to understand health care providers’ perspectives on actual barriers and facilitators to HPV vaccination and garnering strategies for improving vaccination rates in this region.
Background
Human papillomavirus (HPV) is the most common sexually transmitted infection (STI) and the leading cause of cervical cancer (Advisory Committee on Immunization Practices, 2010; Centers for Disease Control and Prevention [CDC], 2010). Two HPV vaccines have been developed—Gardasil (Merck) and Cervarix (GlaxoSmithKline) to protect against infection from HPV types 16 and 18 which are responsible for 70% of all cervical cancers (Advisory Committee on Immunization Practices, 2010; Markowitz et al., 2007; National Cancer Institute [NCI], 2009). Gardasil also protects against HPV types 6 and 11 which cause 90% of genital warts (NCI, 2009). The vaccines are approved for females ages 9–26, with recommendations to vaccinate adolescent girls before becoming sexually active (CDC, 2010; Markowitz et al., 2007). Despite these national guidelines, uptake rates of the HPV vaccine are low. The 2010 National Immunization Survey revealed that only 53% of girls ages 13–17 have received dose one, and only 35% have completed three doses (CDC, 2012b). In Kentucky, a state recognized for cervical cancer disparities (Hopenhayn, King, Christian, Huang, & Christian, 2008; Lengerich et al., 2005), only 46% of girls ages 13–17 have received at least dose one (CDC, 2012b). Vaccination rates are especially low for older females. Nationally, self-reported uptake rates for all three doses among women ages 19–26 is only 21% (CDC, 2012a). In addition to differences in uptake and adherence among age groups, disparities have been noted among racial and ethnic groups (e.g., Hispanic, African Americans), patients who receive the vaccine through public funding, and females who live in poverty and neighborhoods with lower levels of education (CDC, 2012b; Chao, Velicer, Slezak, & Jacobsen, 2010; Cook et al., 2010; Tan et al., 2011).
HPV vaccination research is germane in the Appalachian region of the United States, where cervical cancer rates are elevated (Huang et al., 2002; Wingo et al., 2008; Yabroff et al., 2005), suggesting a higher prevalence of oncogenic HPV infections. Specifically, Appalachian Kentucky suffers from poor socioeconomic conditions, higher cervical cancer incidence and mortality, lower screening rates, low HPV vaccination rates, geographic isolation, and limited health care services (Appalachian Regional Commission [ARC], 2008; Behringer & Friedell, 2006; Couto, Simpson, & Harris, 1994; Hopenhayn et al., 2008; Huang et al., 2002; Reiter, Katz, & Paskett, 2012; Wingo et al., 2008).
Although much attention has focused on young women’s perceptions of the HPV vaccine and their vaccination decisions (Fazekas, Brewer, & Smith, 2008; Hall, Howard, & McCaffery, 2008; Short et al., 2010; Wang, Simoni, & Wu, 2006), little research has focused on rural health care providers’ perceptions (Katz, Reiter, Heaner et al., 2009; Katz, Reiter, Kennedy et al., 2009; Keating et al., 2008). The perceptions of nursing professionals are particularly important as previous research suggests most nurses are supportive of HPV vaccination and are in an ideal position to provide related HPV education to young women compared to other clinicians (Duval et al., 2008; Teitelman, Stringer, Averbuch, & Witkoski, 2009). In rural locales, it is important to hear from nursing staff as these providers help offset physician shortages in geographically isolated communities (Gamm, Castillo, & Pittman, 2003). Further, nursing professionals play a variety of professional and personal roles in rural areas including a formal caretaker, neighbor, church member, community stakeholder, and friend (Long & Weinert, 2010). Nursing professionals, especially, play a key role in HPV vaccination decisions (Chao et al., 2010; Rosenthal et al., 2010; Teitelman et al., 2009) and may offer important perceptions of patient health that differ from the patients themselves (Fitzgerald et al., 2008). In summary, the literature is lacking perspectives from rural health care providers, particularly from rural nursing professionals, on cervical cancer prevention through HPV vaccination; this group of providers may provide important insights for improving this important public health behavior.
Research questions
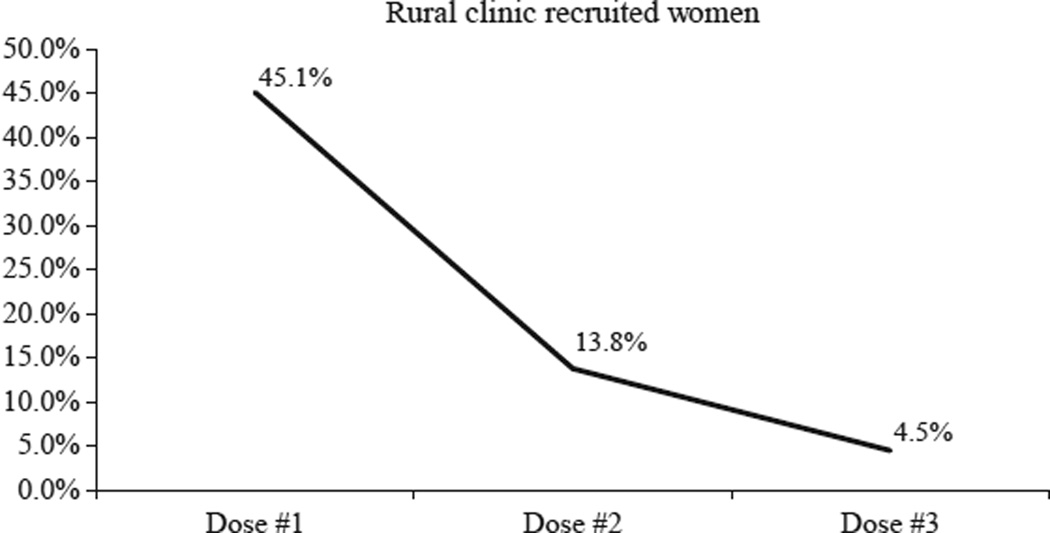
The purpose of this study was to address this gap in the literature by seeking to understand health care providers’ perspectives on HPV vaccination uptake and adherence in rural Appalachian Kentucky. Specifically, this work served as a qualitative follow-up to research conducted by Crosby, Casey, Vanderpool, Collins, and Moore (2011) which compared HPV vaccination rates (specifically, Gardasil) among females ages 18–26 in Appalachian Kentucky to an urban Kentucky sample. Those researchers found that young rural women were significantly less likely to return for subsequent doses of the HPV vaccine compared to their urban counterparts. This finding was noteworthy, given that the vaccine series was offered free of charge to all participants (vaccine costs were covered by the original Crosby et al. study’s grant funding). Of the 246 rural clinic-recruited women, only 45% initiated dose one. Furthermore, only 14% of those who received dose one returned for dose two and only 5% received dose three (Crosby et al., 2011).
As an extension of the Crosby et al. (2011) quantitative findings, we sought in this study to engage health care providers who were familiar with the previous research in in-depth conversations to elicit their perspectives on why uptake and adherence rates were minimal among their young adult female population when considering cost had been removed as a barrier to vaccination. In addition, we sought to solicit suggestions for strategies to improve HPV vaccination rates in their community.
Methods
In consultation with both the principal investigator of the previous HPV vaccination intervention and the director of the rural, Federally Qualified Health Center (FQHC) where the intervention took place, the research team designed a study protocol which invited health care providers (e.g., nursing professionals, physicians) to participate in semi-structured, in-depth interviews. The study protocol was approved by the University of Kentucky’s Institutional Review Board.
Design and sample
Formal invitation letters were sent to all health care providers (N = 15; six licensed practical nurses, three nurse practitioners, six physicians) on staff at the regional FQHC which served as the primary rural study site in the original Crosby et al. intervention. Given the variety of medical professions represented in this sample, we use the term “health care providers” broadly to encompass all our study participants. Eight individuals (53% response rate) agreed to participate in the current qualitative study and each received $75 for their participation. See Table 1 for participant demographics and professional qualifications.
TABLE 1.
Participant Characteristics
| Participant | Sex | Age | Race | Medical qualification |
Years in practice |
Specialty area |
|---|---|---|---|---|---|---|
| HP1 | Female | 31 | White | NP/CNM | 8 | OB/GYN |
| HP2 | Female | 34 | White | LPN | 11 | OB/GYN and Family medicine |
| HP3 | Female | 34 | White | LPN | 13 | Family medicine |
| HP4 | Female | 32 | White | LPN | 12 | Family medicine |
| HP5 | Female | 34 | White | MD | 5 | Family medicine |
| HP6 | Female | 56 | White | NP | 36 | Family medicine |
| HP7 | Female | 41 | White | LPN | 5 | OB/GYN |
| HP8 | Female | 39 | White | NP | 5 | Family medicine |
The interviews were conducted in May 2010 and took place in a private room at the FQHC; each interview lasted approximately 1 hr. Participants provided informed consent before the interview began. The interviewer (second author) followed a semi-structured interview protocol informed by an in-depth review of the HPV vaccine literature (Brewer et al., 2007; Katz, Reiter, Heaner et al., 2009; Katz, Reiter, Kennedy et al., 2009; Rosenthal et al., 2010), as well as the quantitative findings of Crosby et al. (2011). Related, the interviewer presented a line graph (see Fig. 1) generated from the Crosby et al. intervention to prompt study participants in conversation about why vaccine uptake and adherence rates would be so low for these young adult women from the surrounding rural community.
Figure 1. Line Graph Originated by Crosby et al. (2011).
Note: This line graph was presented to the clinicians as a topic of discussion during the in-depth interviews. Data represents initial uptake of dose 1 of the vaccine among those women recruited from the rural, FQHC, as well as subsequent receipt of doses 2 and 3. HPV vaccine receipt was tracked using redeemed free vouchers. While doses 2 and 3 should be given at 2 and 6 months, respectively, from dose 1, the intervention allowed for three extra months at each time point. Despite this time allowance and provision of free vaccine, the rates are strikingly low.
Interview questions specifically focused on health care providers’ perceptions of barriers and facilitators to HPV vaccination uptake and adherence. For example, questions inquired about religious, familial, peer, and socioeconomic influences on women’s vaccination decisions as well as patients’ general understanding of HPV, HPV-related diseases, and the value of the vaccine. In addition, questions addressed potential issues related to non-compliance with the full vaccine series (e.g., transportation, clinic reminder systems, and clinic appointment protocols). Participants were specifically asked to a) focus on the communication interactions that take place with their patients at the point of care (i.e., discussion on HPV and cervical cancer prevention with their patients) and b) articulate changes, strategies, and/or approaches that would help eliminate barriers to HPV vaccination uptake and adherence, thereby improving overall vaccination acceptance and compliance. Each session was audio-recorded and transcribed verbatim. Participants were given a pseudonym which corresponded with the order in which the interviews were conducted (HP1 = Health Care Provider Interview 1).
Analytic strategy
This study used a constant-comparative method to analyze the data (Lindlof & Taylor, 2002; Schoenberg, Hatcher, & Dignan, 2008; Strauss & Corbin, 1990). All three authors read the transcripts line-by-line and generated initial codes through code notes and analytic memos. The authors then met to discuss these initial findings and develop more comprehensive categories; this led to the development of a codebook. The first author returned to the transcripts and coded them using the generated codebook, gathering key exemplars for each emerging finding. All three authors met repeatedly to discuss the findings to resolve any discrepancies and come to consensus about coding and interpretations of data.
The research team did not use qualitative analysis software due to the limited number of transcripts; however, three steps were taken to ensure rigor in the data analysis. First, the research team has previous research experience working with Appalachian Kentucky residents and with this rural FQHC in particular; this allowed the researchers to evaluate the findings based on their past experiences in the field. Findings were also discussed with the authors of the original HPV vaccination intervention; this team consists of public health practitioners, academic researchers, and clinicians. Second, the research team has members from three different disciplines (e.g., health communication, public health, and cancer control) which allowed for multiple perspectives during the coding and interpretation of data. Third, saturation was reached with just these eight participants; these women voiced strikingly similar perspectives on this topic which was not surprising given their related backgrounds and that they serve the same patient population.
Results
Before discussing the larger emergent themes from the data, two small, though significant, findings are worth noting. First, five HPs acknowledged the high rates of abnormal Pap tests, HPV infections, genital warts, and related treatment procedures they see in this rural Kentucky region. HP1 explicitly noted, “[it’s] getting so widespread, it’s out of control.” Second, six HPs voiced strong personal confirmation in the efficacy of the vaccine and indicated that they use their personal beliefs when discussing it with their patients. Specifically, three HPs indicated that they would obtain the vaccine if they were age-eligible. These initial findings provide the reader with an understanding of the HPs’ experience with cervical-related health issues among their patients and provide tangible evidence of their support for protecting women against HPV infection.
The main themes of this qualitative study are grouped into two categories. First, HPs identified reasons they believed there was low vaccine uptake (dose one) in this rural area. Specifically, these rural HPs identified specific patient barriers to HPV vaccination and inadequate HPV vaccine education in the community. Second, HPs identified reasons they believed there was low vaccine adherence (doses two and three) among those women who initiated the vaccine series. Specifically, these rural HPs acknowledged patient beliefs about the inconvenience of adhering to the three-dose vaccine schedule and clinic-centered communication deficiencies. Within each theme, HPs detailed barriers, but were also prompted to provide suggestions for overcoming these barriers in their rural clinic population. Each theme is presented below.
Reasons for low HPV vaccination uptake
Patient barriers to vaccination
The HPs identified two reasons why patients in their clinic population do not receive dose one. First, they believed that young women are reticent to receive the vaccine because “they just do not want to have a shot” (HP5) and “the pain of the shot” (HP6). This was especially the case when trying to understand why women in the intervention study did not come in even when cost was eliminated as a barrier. HP5 compared those findings to females in younger age groups (9–17 years old) where she thought “it would probably be more parents not wanting their child to have the shot” and went on to say that “in the older population…that makes their own decisions, I would think it would be just not getting a shot.” HP3 believed the pain from the initial shot makes some patients she sees “real reluctant to…get the [next] dose even when they are there for their next scheduled follow-up.” HP1 acknowledged to her patients that while the shot does burn, “it is only going to last, you know, a minute and [it will] be over with.” HP7 emphasized to her patients “if they get the disease…warts…letting us take stuff or do colopos…then that is painful compared to the shots.”
The second reason (or, patient barrier) is that HPs believed young women from this area do not believe the HPV vaccine is important to their health. For instance, HPs voiced that many of their patients do not understand the link between this STI and cervical cancer and therefore do not believe they need to take steps to protect themselves from HPV. Five HPs stressed with their patients how HPV is the most common STI in the United States but interestingly, HP8 noted that many women are more worried about other sexually transmitted diseases. She said “you never hear a patient say, I think I have HPV…since the research started, we became more knowledgeable and more apt to talk to them about [HPV].” HP8 emphasized to her patients how easily HPV is spread without a person even knowing it; she tells her patients “you may never know where you got it…but you will have a remembrance from now on.” Despite media coverage, even basic awareness of the vaccine is low in this area, as HP3 said that “a lot of folks just do not know what that [HPV] is.” HP1 stresses the importance of the HPV vaccine by educating young women about how “you never know that the guy has it until it is too late, until you have that abnormal Pap smear. So just educating them on how it’s transmitted” and that the HPV vaccine is “one of the ways that we can prevent that…[then] they seem very, very interested.”
Related, HPs also indicated that they have few women proactively ask for the vaccine. HP8 said “I have very few patients that actually come in and ask for the vaccine; that is something that I bring up to the patients; they do not a lot of times mention that.” HP1 also said that her patients rarely bring up the vaccine and estimates that there are maybe “ten that is ever brought it up.” HP5 said that while “I do not think that most people refuse it when we offer it,” it is the HPs who must be proactive in offering the vaccine to the patient. In addition, she said that “most of them really take whatever they get for free…they do not ask a lot of questions.” She went on to say that “they may not even know, understand what it is but they will take it.” This implies that some women are receiving the HPV vaccine without fully understanding what it is for and how important it is to their health.
Inadequate region- and age-specific HPV vaccination education and promotion
HPs believed that increased patient education about the vaccine is needed, especially through more focused media efforts for rural Appalachian Kentucky that generates discussion throughout the community such as billboards, radio, and community events. HP1 commented that informational videos playing at pharmacies and clinic lobbies would help to educate a variety of people about the vaccine, including mothers and grandmothers, who according to half of the providers, still play an important role in young adult women’s health care decisions. She suggested a video because “a lot of people cannot read in this area…they need the hands-on education and visual” offered in a video format. This statement was countered by six other HPs who identified text-based pamphlets as important education tools they use with patients. In addition, several HPs believed that the current HPV media campaign (e.g., Merck’s “One Less” campaign) is not focused on these young adult women (HP3 said “it looks like it is for children”) and a separate campaign “to market [to] the older adolescent group” (HP1) is needed. HP5 argued that “probably not as many of them realize that they are candidates for the vaccine” because of the focus on younger girls. In addition, HP1 argued that the current HPV vaccine commercials “may be perceived as sex being ok if they obtain the vaccine and many religions in the area I know would have problems with that.” HP5 also commented that religion may play a role in Appalachian Kentucky “more so than other [areas] because we are still kind of the Bible Belt area.” As a result of the national campaign’s mismatch with this older age group and geographic region, HP4 stated that in turn it is the local HPs’ responsibility to promote the vaccine to this older age group. Related, HP1 went on to say that “the lack of health care in the area provides less patient education so we spend a lot of time trying to educate these patients.”
In addition to more targeted efforts for this young adult population in Appalachian Kentucky, several HPs advocated for a focus on genital warts which are also a sequelae of HPV infection. HP7 noted that one of the HPV vaccines (Gardasil) prevents “not just cervical cancer…but genital warts, which are something that as I tell the kids you know, when you get that, you have got it the rest of your life; you may never where you got it and you would not know his name.” HP6 said that many anti-smoking campaigns geared toward this age group are “geared toward how ugly it is and like visual things”, so for HPV, it might be effective “if you could have these big old warts.” HPs felt that a focus on genital warts would make the vaccine more relevant for this age group, thereby potentially increasing uptake.
Reasons for low HPV vaccination adherence
Complications of three-dose vaccine schedule
HPs identified two reasons why patients do not return for doses two and three of the HPV vaccine; current ACIP guidelines promote receipt of all three doses (CDC, 2010). First, they believed that many of the young women they see do not understand the importance of the full vaccine series and this is coupled with the inconvenience of coming back to the clinic for the two remaining shots. HP8 argued “I do not think in this age group, they do not value the importance of the immunization.” HP8 believed that it “looks like there is a breakdown in terms of stressing the importance of coming back” and HP2 said that “of course it needs to be stressed that it takes all three doses to be effective,” indicating that these HPs believe that some of the responsibility for vaccine adherence lies with the provider who administers the first dose. Several of the HPs said they inform their patients of the importance of and commitment to the three-dose regimen during the first visit because of the difficulty in getting them back for subsequent injections. HP8 said “that is the hard part. I usually start by saying you know there is no use in you taking the first dose if you are not going to come back.” She went on to say “…do not just take this because you are here today and I am looking at you and you feel obligated to take this…make the commitment to come back.” HP8 also recalled some patients commenting that because they have received dose one, they do not need to receive doses two and three. Similarly, HP2 stated, “maybe they think that after the first dose, maybe they are okay”. HP3 believed her patients think “I had one, why do I need three?” This is another example of these rural HPs’ perceptions that the young women they serve may not understand the value of preventive immunization and are not making fully informed decisions when initiating the vaccine series.
When women come back to the clinic for something else, the HPs often followed up on their completion of the vaccine series. HP5 said that she has “had a few of those where they came in; I am like, have you had your Gardasil? Yeah, yeah. I was like did you have all of it? No, I only had one dose and it was like 7 months ago so.” She said that for patients in similar situations, they have made the clinical decision to restart the vaccine series, which is costly and only adds to the discomfort a woman may experience (i.e., having to receive even more shots than the normal three-dose regimen). The medical decision to revaccinate is not taken lightly; if the woman received her initial shot(s) elsewhere, the provider may not have access to her immunization records, becoming solely reliant on potentially inaccurate patient self-report.
Clinic-centered communication deficiencies
HPs identified three key areas of communication that they believe would improve HPV vaccine adherence for the young adult women they serve. First, these HPs believed there were many missed opportunities for HPV vaccination in their clinic. They suggested simple policy changes which target women at varying interactions with the health care system such as adding a question about HPV vaccination status in primary care clinic “in-take” forms (HP3), making HPV vaccination a standing physician order (i.e., similar to influenza and pneumonia vaccinations) during routine primary care visits (HP3); inquiring about HPV vaccination status during OB/GYN and family planning visits (HP2, CP5, HP8), college physicals (HP4), and/or young mothers attending well-child visits (HP5). By questioning women about HPV vaccination at any these points, it increases the possibility of having higher vaccine adherence rates and thus providing the full protection from HPV afforded by this vaccine.
Second, the HPs in our study overwhelmingly believed a more effective clinic reminder system is needed to increase adherence rates. Several HPs identified reminder card systems, but as HP8 noted “you know, those get lost.” Instead, she believes something like “text messages would probably be right up there with that group.” HP2 also believes cell phones would be effective if used in a reminder system because these women always have their cell phone on their person and will “walk in texting and talking on the cell phone” even in the doctor’s office. Some HPs also suggested email as an effective means for reminders. However, while HP1 recognizes that technology is definitely an effective communication tool, she advocates communicating with the patient about her preferences for reminders as the best strategy for improving vaccine adherence: “ask the patient how she want[s] reminded.”
Third, HPs believed increased knowledge and awareness of the vaccine appointment protocol was important to improve vaccine adherence. HP8 said some women “generally associated coming to the clinic with a 2–3 hr process” when in reality women can “just pop in and get it done and you’re out the door” because they do not need to see a doctor when receiving the second and third dose. HP2 also said that the convenience of seeing only a nurse for doses two and three—without an appointment—needs to be clearly explained at the first dose. This was echoed by other HPs in the study, emphasizing the need for improved communication about clinic vaccine appointment protocol.
Discussion
The results from this study offer insight into rural health care providers’ perceptions of both barriers and facilitators to improving HPV vaccine uptake and adherence among young adult women. Among the many valuable suggestions provided by participants in this study, there are four specific recommendations for practice that are worth highlighting.
First, health care providers may need to be more proactive about recommending the vaccine to all their eligible patients, especially considering providers in this study suggest that patient requests are minimal. Similarly, Keating et al. (2008) reported that almost 60% of a sample of rural North Carolina medical practices were concerned that too few patients wanted the vaccine. HPs in this study identified multiple time points when young women may interact with the health care system in their clinic, providing an opportunity to offer the initial HPV vaccination or subsequent doses. Unfortunately, research also reveals that pediatricians serving younger females in Appalachia are less likely to encourage HPV vaccination compared to non-Appalachian pediatricians (Krieger, Katz, Kam, & Roberto, 2012). This suggests that nursing professionals serving young adult female patients, like those in our study, may have an even heavier burden to bear when it comes to encouraging HPV vaccination for this patient group. Improvements in targeting all age-eligible patients for the vaccine, particularly young adult women, must be coupled with communication emphasizing the importance of the vaccine and the commitment to complete the three-dose series. The lack of understanding of the importance of this preventive health measure was pervasive in the providers’ perceptions of barriers to both HPV vaccine uptake and adherence. Our findings echo Teitelman et al. (2009) in suggesting health care providers, especially nursing professionals, have a role in not only helping patients make an informed decision about starting the HPV vaccine, but encouraging completion of the entire series.
Second, participants in our study believed more tailored, age-appropriate and region-specific promotional campaigns for young women are needed in Appalachian Kentucky. Merck’s “One Less” campaign was originally targeted to the mothers of young girls and may have failed to address women ages 18–26; this is echoed by the present findings. Subsequently, many of the providers felt like a different approach is needed to reach this young adult population. Several recommended more graphic campaigns showcasing genital warts caused by HPV as a prompt to vaccination, instead of the more common message of preventing cervical cancer. Furthermore, a heavier reliance on local media such as billboards, radio, and community events may emphasize the benefits of receiving the vaccine for this catch-up group of women and make the issue more salient for those young adult women who have little to no awareness of their eligibility to receive the vaccine.
Third, more synchronized and effective reminder systems may be needed. Many of the providers in our study mentioned an appointment card or phone call is used as a reminder for the next HPV vaccine dose; however, these remain ineffective as adherence is low. Perhaps the most important piece of a reminder system is the patient-centered approach. Simply asking women which reminder method is preferred could help increase adherence, especially with today’s variety of technology options. Several providers recommended cell phone (specifically, text message) reminders, which represents an effective communication system that clinics can easily implement (Head, Noar, Iannarino, & Harrington, 2012).
Fourth, providers in this study felt one of the reasons patients fail to return for doses two and three is because they do not want to make an appointment and wait at the clinic for the simple act of receiving an injection. This could imply poor communication of the clinic’s vaccination appointment protocol to patients; clinics should advertise that the subsequent doses may not require an actual physician appointment, but rather a nurse-only visit. This strategy may encourage young adult women to return to the clinic for the follow-up doses. In Appalachian Kentucky, this is particularly relevant because transportation to and from the health clinic may be difficult and therefore it is important to emphasize the convenience of a nurse-only visit.
There were several limitations of this study. First, there is limited generalizability as this study employed a small sample and focused only on rural health care providers serving young adult women in Appalachian Kentucky. Despite recruitment efforts, many factors may have contributed to the small sample size such as nurses’ and physicians’ busy schedules and time constraints. However, it should be noted that, though the sample size is small, these eight individuals—through the services of the FQHC where they are employed—actually provide a substantial portion of women’s and primary care-related health care in the eight-county vicinity. In addition, they were able to offer detailed and meaningful insight into the low vaccine uptake and adherence rates for the population of patients from the previous intervention study conducted at their FQHC. Second, the current research team shares an institutional affiliation with the FQHC; however, the researchers did not personally know any of the clinic staff prior to the interview. Regardless, there may have been undue bias with a university-based professor (second author) conducting the interviews. Third, the study sought to understand health care providers’ perspectives of low HPV vaccine uptake and adherence in their patient population. This represents a form of others’ reports that comes with its own limitations; for this study, that might include inaccurate observations and biased interpretations of patients’ behaviors and communication about HPV and cervical cancer prevention. Despite this, these providers offer a unique view into this group of young adult women who they serve on a daily basis. As noted earlier, this geographic area suffers from high cervical cancer rates and low vaccine uptake and adherence rates, and these providers’ previously unheard voices shed light on important issues that may help to address these public health problems.
In summary, this qualitative follow-up study sought to understand health care providers’ perspectives on previously documented low HPV vaccine uptake and adherence rates in their young adult female patient population. The results offer important, practical implications from nursing professionals and a physician in a medically underserved region of the country recognized for cervical cancer disparities that can be readily applied to other communities. As articulated by these Appalachian Kentucky health care providers, nurses and physicians need to be proactive and creative in their efforts to educate young women about HPV, its related health consequences, and the value of the full vaccine series. In addition, messages about the HPV vaccine need tailoring to the unique characteristics of their patient population. The design, testing, and evaluation of region- and age-specific HPV vaccine education and promotion strategies, which are informed by health care provider input, is an area ripe for future research. Participants in this study also provided tangible examples of clinic-oriented strategies that could facilitate improved vaccine receipt and compliance, but these strategies deserve further research related to feasibility, implementation, and vaccination outcomes. Nursing professionals should serve as key stakeholders in developing and implementing such clinic-oriented interventions, which if proven successful, could be adopted by other health care providers in similar rural and underserved areas.
References
- Advisory Committee on Immunization Practices. Recommended adult immunization schedule: United States, 2010. Annals of Internal Medicine. 2010;152(1):36–39. doi: 10.7326/0003-4819-152-1-201001050-00008. [DOI] [PubMed] [Google Scholar]
- Appalachian Regional Commision (ARC) Underlying socioeconomic factors influencing health disparities in the Appalachian region final report. 2008 Retrieved from http://www.arc.gov/assets/research_reports/Socioeconomic-FactorsInfluencingHealthDisparitiesinAppalachianRegion5.pdf.
- Head KJ, Noar SM, Iannarino NT, Harrington NG. Efficacy of text messaging-based interventions for health promotion: A meta-analysis; Paper presented at the 98th Annual National Communication Association Conference; Orlando, FL. 2012. [Google Scholar]
- Behringer B, Friedell GH. Appalachia: Where place matters in health. Preventing Chronic Disease. 2006;3:1–4. [PMC free article] [PubMed] [Google Scholar]
- Brewer NT, Chapman GB, Gibbons FX, Gerrard M, McCaul KD, Weinstein ND. Meta-analysis of the relationship between risk perception and health behavior: The example of vaccination. Health Psychology. 2007;26:136–145. doi: 10.1037/0278-6133.26.2.136. [DOI] [PubMed] [Google Scholar]
- CDC. Human papillomavirus (HPV) 2010 Retrieved from http://www.cdc.gov/hpv/
- CDC. National, state, and local area vaccination coverage among adolescents aged 13–17 years – United States, 2011. Morbidity and Mortality Weekly Report. 2012b;61(32):671–677. [PubMed] [Google Scholar]
- Centers for Disease Control (CDC) Adult Vaccination Coverage - United States, 2010. Morbidity and Mortality Weekly Report. 2012a;61(4):66–72. [PubMed] [Google Scholar]
- Chao C, Velicer C, Slezak JM, Jacobsen SJ. Correlates for human papillomavirus vaccination of adolescent girls and young women in a managed care organization. American Journal of Epidemiology. 2010;171:357–367. doi: 10.1093/aje/kwp365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook RL, Zhang J, Mullins J, Kauf T, Brumback B, Steingraber H, et al. Factors associated with initiation and completion of human papillomavirus vaccine series among young women enrolled in Medicaid. Journal of Adolescent Health. 2010;47:596–599. doi: 10.1016/j.jadohealth.2010.09.015. [DOI] [PubMed] [Google Scholar]
- Couto RA, Simpson NK, Harris G, editors. Sowing seeds in the mountains, community based coalitions for cancer prevention and control. Bethesda: National Institutes of Health, National Cancer Institute; 1994. [Google Scholar]
- Crosby RA, Casey BR, Vanderpool RC, Collins T, Moore GR. Uptake of free HPV vaccination among young women: A comparison of rural versus urban rates. Journal of Rural Health. 2011 doi: 10.1111/j.1748-0361.2010.00354.x. Advanced online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duval B, Gilca V, Boulianne N, Pielak K, Halperin B, Simpson MA, et al. Cervical cancer prevention by vaccination: Nurses’ knowledge, attitudes, and intentions. Journal of Advanced Nursing. 2008;65(3):499–508. doi: 10.1111/j.1365-2648.2008.04900.x. [DOI] [PubMed] [Google Scholar]
- Fazekas KI, Brewer NT, Smith JS. HPV vaccine acceptability in a rural southern area. Journal of Women’s Health. 2008;17:539–548. doi: 10.1089/jwh.2007.0489. [DOI] [PubMed] [Google Scholar]
- Fitzgerald JT, Stansfield RB, Tang T, Oh M, Frohna A, Armbruster B, et al. Patient and provider perceptions of diabetes: Measuring and evaluating differences. Patient Education and Counseling. 2008;70:118–125. doi: 10.1016/j.pec.2007.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gamm L, Castillo G, Pittman S. Rural Healthy People 2010: A companion document to Rural Healthy People 2010. Vol. 2. College Station, TX: The Texas A&M University System Health Science Center, School of Rural Public Health, Southwest Research Center; 2003. Access to quality health services in rural areas-primary care: A literature review. [Google Scholar]
- Hall B, Howard K, McCaffery K. Do cervical cancer screening patient information leaflets meet the HPV information needs of women? Patient Education and Counseling. 2008;72:78–87. doi: 10.1016/j.pec.2008.01.024. [DOI] [PubMed] [Google Scholar]
- Hopenhayn C, King JB, Christian A, Huang B, Christian WJ. Variability of cervical cancer rates accross 5 Appalachian states, 1998–2003. Cancer. 2008;113:2974–2980. doi: 10.1002/cncr.23749. [DOI] [PubMed] [Google Scholar]
- Huang B, Wyatt S, Tucker T, Bottorff D, Lengerich E, Hall H. Cancer death rates – Appalachia, 1994–1998. Morbidity and Mortaity Weekly Report. 2002;51:527–529. [PubMed] [Google Scholar]
- Katz ML, Reiter PL, Heaner S, Ruffin MT, Post DM, Paskett ED. Acceptance of the HPV vaccine among women, parents, community leaders, and healthcare providers in Ohio Appalachia. Vaccine. 2009;27:3945–3952. doi: 10.1016/j.vaccine.2009.04.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz ML, Reiter PL, Kennedy S, Schoenberg N, Johnson A, Ely G, et al. Human papillomavirus (HPV) vaccine availability, recommendations, cost and policies among health disparities in seven Appalachian states. Vaccine. 2009;27:3195–3200. doi: 10.1016/j.vaccine.2009.03.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keating KM, Brewer NT, Gottlieb SL, Liddon N, Ludema C, Smith JS. Potential barriers to HPV vaccine provision among medical practices in an area with high rates of cervical cancer. The Journal of Adolescent Health. 2008;43:S61–S67. doi: 10.1016/j.jadohealth.2008.06.015. [DOI] [PubMed] [Google Scholar]
- Krieger JL, Katz ML, Kam JA, Roberto A. Appalachian and Non-Appalachian pediatricians’ encouragement of the human papillomavirus vaccine: Implications for health disparities. Women’s Health Issues. 2012;22:e19–e26. doi: 10.1016/j.whi.2011.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lengerich E, Tucker T, Powell R, Colsher P, Lehman E, Ward A, et al. Cancer incidence in Kentucky, Pennsylvania, and West Virginia: Disparities in Appalachia. Journal of Rural Health. 2005;21:39–47. doi: 10.1111/j.1748-0361.2005.tb00060.x. [DOI] [PubMed] [Google Scholar]
- Lindlof TR, Taylor BC. Qualitative communication research methods. Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- Long KA, Weinert C. Rural nursing: Developing the theory base. In: Winters CA, Lee HJ, editors. Rural nursing concepts, theory and practice. 3rd. New York, NY: Springer; 2010. pp. 3–18. [Google Scholar]
- Markowitz L, Dunne EF, Saraiya M, Lawson H, Chesson H, Unger E. Quadrivalent human papillomavirus vaccine: Recommendations of the ACIP. Moridity and Mortaity Weekly Report. 2007;56(RR02):1–24. [PubMed] [Google Scholar]
- National Cancer Institute (NCI) Human papillomavirus (HPV) vaccines. 2009 Retrieved from http://www.cancer.gov/cancertopics/factsheet/Prevention/HPV-vaccine.
- Reiter PL, Katz ML, Paskett ED. HPV vaccination among adolescent females from Appalachia: Implications for cervical cancer disparities. Cancer Epidemiology Biomarkers & Prevention. 2012;21:2220–2230. doi: 10.1158/1055-9965.EPI-12-0850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal SL, Weiss TW, Zimet GD, Ma L, Good MB, Vichnin MD. Predictors of HPV vaccine uptake among women aged 19–26: Importance of a physician’s recommendation. Vaccine. 2010;29:890–895. doi: 10.1016/j.vaccine.2009.12.063. [DOI] [PubMed] [Google Scholar]
- Schoenberg NE, Hatcher J, Dignan MB. Appalachian women’s perceptions of their community’s health threats. Journal of Rural Health. 2008;24(1):75–83. doi: 10.1111/j.1748-0361.2008.00140.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Short MB, Rosenthal SL, Sturm L, Black L, Loza M, Breitkopf D, et al. Adult women’s attitudes toward the HPV vaccine. Journal of Women’s Health. 2010;19:1305–1311. doi: 10.1089/jwh.2009.1471. [DOI] [PubMed] [Google Scholar]
- Strauss A, Corbin JM. Basics of qualitative research: Grounded theory procedures and techniques. Thousand Oaks, CA: Sage; 1990. [Google Scholar]
- Tan W, Viera AJ, Rowe-West B, Grimshaw A, Quinn B, Walter EB. The HPV vaccine: Are dosing recommendations being followed? Vaccine. 2011;29:2548–2554. doi: 10.1016/j.vaccine.2011.01.066. [DOI] [PubMed] [Google Scholar]
- Teitelman AM, Stringer M, Averbuch T, Witkoski A. Human papillomavirus, current vaccines, and cervical cancer prevention. Journal of Obstetric, Gynecologic, & Neonatal Nursing. 2009;38:69–80. doi: 10.1111/j.1552-6909.2008.00304.x. [DOI] [PubMed] [Google Scholar]
- Wang JF, Simoni PS, Wu Y. Human papillomavirus (HPV) in rural adolescent females: Knowledge, protected sex, and sexual risk behaviors. Online Journal of Rural Nursing and Health Care. 2006;6:74–88. [Google Scholar]
- Wingo PA, Tucker TC, Jamison PM, Martin H, McLaughlin C, Bayakly R, et al. Cancer in Appalachia, 2001–2003. Cancer. 2008;112(1):181–192. doi: 10.1002/cncr.23132. [DOI] [PubMed] [Google Scholar]
- Yabroff K, Lawrence W, King J, Mangan P, Washington K, Yi B, et al. Geographic disparities in cervical cancer mortality: What are the roles of risk factor prevalence, screening, and use of recommended treatment? Journal of Rural Health. 2005;21(2):149–157. doi: 10.1111/j.1748-0361.2005.tb00075.x. [DOI] [PubMed] [Google Scholar]