Summary
Introduction.
Alcohol is an important factor weighting towards global disease burden, premature death and Disability-Adjusted Life Years. This study examines the burden imposed on the Borgo Trento Verona Hospital Emergency Department (ED) Italy by patients with Acute Alcohol Intoxication (AAI).
Methods.
A 6-year retrospective study was performed by reviewing medical records in all patients (≥ 16 years old) diagnosed with AAI. Clinical criteria for inclusion in the sample followed those defined in the "Alcohol Intoxication Symptoms" section of DSM-IV-TR. Ambiguous cases presenting traumas potentially related to AAI were confirmed positive using a Blood Alcohol Level (BAL) test before inclusion in the sample. Socio-demographic data, case history, timing of admission/discharge and outcome were collected for each patient.
Results.
One thousand five hundred forty-seven patients (males:females = 6.6:1) were included in the study. With regard to marital status, the crude rate within the sample shows that single and married subjects have a significantly higher prevalence (p < 0.01). When demographic data of residents was taken into consideration, divorced/separated and single categories were significantly more represented (p < 0.05).
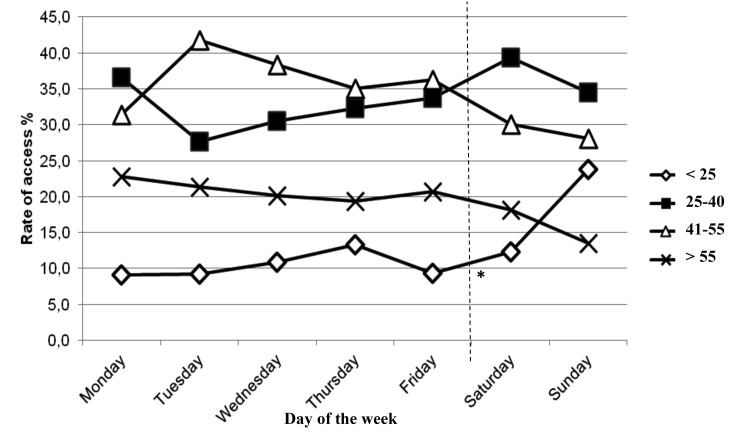
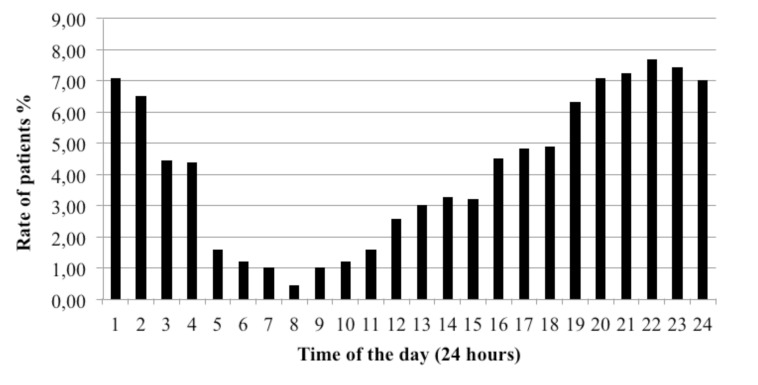
The admissions appeared fairly constant throughout the week with a higher prevalence of patients aged between 25-55 years, and a significant peak of the youngest age class on weekends. Higher rates of admission were recorded during the late afternoon and night.
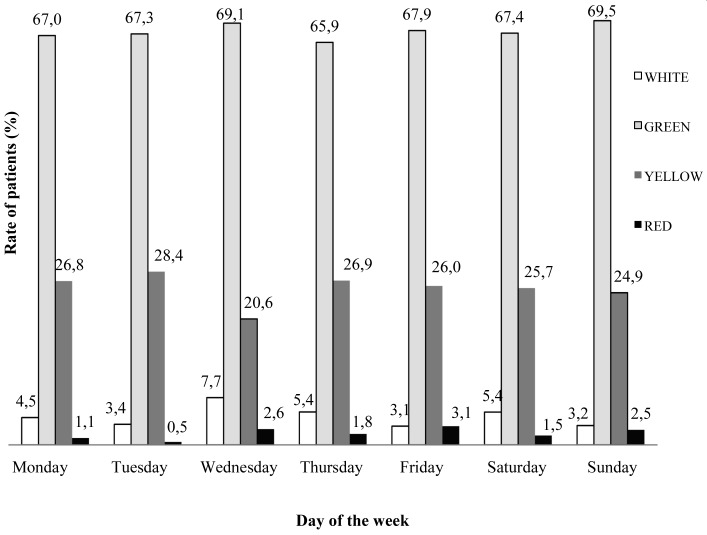
The triage code of admission appeared uniformly distributed along the week, with the highest prevalence of green code (67.7%), followed by yellow one (25.8%). The analysis of clinical symptoms and BAL highlights that moderate clinical severity concerns almost 50%, and clinically critical severity the 6.6% of cases of access.
Admissions rates of foreign patients resulted to be 3 times higher compared to those of natives when adjusted to demographic data.
Discussion.
Social disadvantages such as foreign provenance and social difficulties as unemployment, low money intake, perception of loneliness, and dysfunction in family life were frequently identified in the sample. An exception was found within the youngest age group, where the AAI are mostly related to alcohol abuse during social outings over the weekend.
EDs play a crucial role in helping patients with AAI, but prevention of alcohol abuse though implementation of social and sanitary health policies on all ages (but especially among the youngest) is essential.
Key words: Alcohol, Acute intoxication, Emergency department
Introduction
Alcohol is the third risk factor for premature death and disability in the world: the WHO estimates that inappropriate use of alcohol causes approximatively 3.3 million deaths per year (about 6% of total world deaths) and over 5% of global disease burden (mainly cancer, vascular, and liver disease; traffic accidents, suicide, and violence), and represents an important cause of Disability- Adjusted Life Years (DALYs) [1, 2].
Europe appears to be a region in the world with recurrent heavy drinking, and stands out as the area with the most significant increase in patterns of alcohol consumption with a corresponding increase of cases of Acute Alcohol Intoxication (AAI) [3].
As a result, in this region alcohol consumption is an important and a growing public health problem: every year 195,000 people die for harmful use of alcohol (12% of all male and 2% of all female premature mortality cases), which represent about the 3.8% of all causes of death and the 4.6% of DALYs [4-6].
In Italy in 2010 were recorded 16,829 deaths (age > 15 years; rate M:F = 2.27) [7, 8] and the prevalence of atrisk alcohol consumers older than 11 years is estimated to be around 8,000,000 subjects (rate M:F = 1:3.27) [9]. The incidence of Acute Intoxications (AI) represents the 10.0/1000 of the total admittance to Emergency Departments (EDs) and among them about 57% were alcohol related, representing between the 0.6 and 40% of all the ED accesses as referred in various reports. [10-15]
As the ED play a crucial role for patients affected by acute Alcohol Use Disorders (AUDs), a study was performed to evaluate the burden imposed by patients with AAI to the Emergency Department of Borgo Trento Hospital in Verona (Italy).
Methods
This retrospective study involved a medical record review spanning a 6-year period (1 January 2009 - 31 December 2014) of all consecutive patients admitted to the ED due to alcohol intoxication. Admissions averaged approximately 98,800 patients per year.
The Italian "privacy" law and the Helsinki Declaration on human subjects testing were fully respected and the protocols were approved by the local ethical committee. All the patients included in the study were over 15 years old (patients under 16 years of age are served by a separate pediatric ED), and had a clinical criteria for inclusion following diagnosis of AAI as defined by the DSMIV- TR "Diagnostic Criteria for Alcohol Abuse and Dependence" [16, 17] which include "a) recent ingestion of alcohol; b) clinically significant maladaptive behavioral or psychological changes (e.g., inappropriate sexual or aggressive behavior, mood liability, impaired judgment, impaired social or occupational functioning) that developed during, or shortly after, alcohol ingestion; c) one (or more) of the following signs, developing during, or shortly after, alcohol use: slurred speech, incoordination, unsteady gait, nystagmus, impairment in attention or memory, stupor or coma."
All the samples were taken and coded with anonymous matching bar codes, non-specific to the patient, and all the information necessary for the study was associated.
To determine the presence and the level of alcohol intoxication of each patient a blood sample was obtained and analyzed at the central laboratory of the same hospital of the Emergency Department (ED) using a commercial enzymatic "alcohol dehydrogenate" method with the UV spectrophotometer as a blood alcohol level (BAL) test. The minimum measurable amount was of 0.1 g/L.
The severity of AAI in patients was classified by the ED into four categories considering both the severity of the clinical symptoms and the BAL: clinical symptoms (c.s.) less than slight and BAL < 17 mmol/L; c.s. slight and BAL between 17 and 53 mmol/L; c.s. moderate and BAL between 54 and 87 mmol/L; c.s. critical and BAL > 87 mmol/L.
Patients admitted for other clinical reasons such as various kind of traumas, burns, and mental disorders, and which could initially have led to a suspicion of excessive alcohol consumption, were only included if BAL tests resulted positive.
Day span was defined as beginning at 00:01 and ending at 24:00 h. The weekend started at 00:01 h on Saturday and finished at 24:00 h on Sunday.
For each admitted patient the following data were extracted from the database of the ED: identification code, sociodemographic data (sex, date of birth, age, nationality, place of residence, marital status), timing of admission/ discharge (day and hour of admittance, day and time of discharge, period of stay), and case history (triage category, anamnestic data, physical examination, BAL and severity of clinical symptoms, and diagnosis). The outcome was divided into "admission to a hospital ward", "sent to a general practitioner" (i.e. going to a family doctor for further treatment), "discharge" (i.e. returning back home), and "refusal of treatment" (i.e. decision of the patient not be treated).
Collected data were registered within a Microsoft Office Excel database.
STATISTICAL ANALYSIS
In order to report the results of the analysis, categorical variables were presented as numbers and percentages; the comparison between subgroups was carried out using Chi-square test for qualitative data. Linear trend was evaluated with the Cochran-Armitage test for linear trend.
P values were considered significant when < 0.05.
Results
The study included 1,547 patients, representing 0.26% of all ED visits occurred during the duration of the study. Males represented 85.2% of subjects, with a male-to-female ratio of 6.6:1. The age range was 16-92 years for males, 16-90 years for females, with a mean age of 42.6 and of 40.8 years respectively.
The crude distribution rate of marital status (Tab. I) highlights that single and married subjects show a significantly higher prevalence (p < 0.001). When demographic data of residents was taken into consideration, divorced/separated and single categories were significantly more represented (p < 0.05).
Tab. I.
Marital status: distribution in admitted patients to ED according to crude rate and to the respective distribution in resident population (Italian plus foreigner).
| Admitted patients | ||
|---|---|---|
| Marital status | Crude rate (%) |
Rate according to marital status of resident population (%) |
| Single | 38.1* | 0.5 & |
| Married | 22.2*, ** | 0.3 &, && |
| Divorced/separated | 5.7** | 0.6 && |
| Widow | 0.4 | 0.1 |
| Not declared | 33.6 | 0 |
p < 0.01;
p < 0.01;
p < 0.05
p < 0.05
Admissions appear fairly constant along the week (Fig. 1), with a predominance of patients aged between 25-55 years. On Saturday and Sunday admissions were respectively of 16.9% and 18.4% of the sample total, with exception of the youngest age class (< 25 years), which showed the largest and most significant increase (more than the 52%) during weekend compared to the other age classes (p < 0.001).
Fig. 1.
Weekly trend of admissions because of alcohol intoxication to ED according to age class and day of the week.
Admissions to the ED resulted mostly clustered (Fig. 2) around the late afternoon with a significantly (p < 0.001) increasing trend during the night (between hours 20 and 2). A remarkable reduction of patients was registered in the morning.
Fig. 2.
Distribution rate (%) of admissions to Emergency Department according to daytime.
The triage code distribution evaluated along the week (Fig. 3) shows a uniform and not significantly trend. Average Green Code pertained to 67.7% of the patients; Yellow to 25.8%; White to 4.6% and Red to 1.9%.
Fig. 3.
Distribution rate (%) of admissions according to day of attendance and triage.
The length of stay in the ED under medical observation was different according to the urgency level: < 1 hour for patients for White Codes, 1-2 hours with Green Code, 3-4 hours for Yellow Codes, and 5-7 hours for Red Codes.
The distribution of severity of clinical symptoms and BAL is reported in Tab. II. Notably, moderate severity was found in almost 50% of patients (prevalent age: 21- 50 years), and 6.6% resulted clinically critical (prevalent age: 31-50 years). Moderate clinical symptoms resulted significantly prevalent (p < 0.001) compared to other classifications of clinical classes.
Tab. II.
Distribution rate (%) of patients with AAI according to clinical symptoms, (BAL) and age class.
| Severity of clinical symptoms and level of BAL in Acute Alcohol Intoxication (AAI) | |||||
|---|---|---|---|---|---|
| Clinical Symptomps BAL |
Non Relevant (< 17 mmol/L) |
Slight (17-53 mmol/L) |
Moderate (54-87 mmol/L) |
Critical (> 87 mmol/L) |
Total results |
| AGE CLASS | & | & | |||
| < 20 | 1.5% | 4.7% | 2.1% *, ** | 0.3% | 8.6 % |
| 21-30 | 5.3% | 5.1% | 8.8% *, ** | 0.6% | 19.8% |
| 31-40 | 4.7% | 1.9% | 10.1% *, ** | 1.7% +, ++ | 18.4% |
| 41-50 | 9.2% | 2.6% | 13.3% *, ** | 2.8% +, ++ | 27.9% £ |
| 51-60 | 2.6% | 2.3% | 4.9% *, ** | 0.8% | 10.6 % |
| >60 | 3.2 % | 1.9% | 9.2% *, ** | 0.4% | 14.7% |
| TOTAL | 26.5 % | 18.5% | 48.4 % °° | 6.6% | 100% |
Chi-square test among age classes (from < 20 to > 60) among non relevant and among slight clinical symptoms: p = n.s.
Total results: Age 41-50 vs all other age classes: p < 0.05 (Chi-square test);
Moderate clinical symptoms: evaluation of age classes 31-40 and of 41-50 and other age classes: p < 0.05 (Chi-square test)
Moderate clinical symptoms: evaluation of age classes 31-40 and of 41-50 and other age classes: p < 0.05 (Chi-square test)
Critical clinical symptoms: p < 0.05 (Chi-square test)
Critical clinical symptoms: p < 0.05 (Chi-square test)
Moderate clinical symptoms vs other clinical classes: p < 0.001 (Chi-square test)
The majority of admissions are represented by subjects aged between 21-50 (p: n.s.) with a significantly predominance among ages 41-50 (27.9% of cases) (p < 0.05). Analysis based on clinical symptoms and BAL shows that distribution of admissions by age is different according to clinical condition: younger subjects generally had a non-relevant or a moderate AAI, while patients aged 31-50 resulted experiencing prevalently and significantly moderate (p < 0.05) or critical (p < 0.05) BAL levels.
The majority of patients (crude rate: 68.6%) admitted to the ED were native Italian subjects.
However, when the analysis of these data was evaluated proportionally to demographic information (local municipal data), the admission rate of foreign patients results in 123.2/105 inhabitants, which is almost three times greater than rate for the Italian patients (46.4/105 inhabitants).
Among foreign patients African and Asian subjects show the greatest admission rate, being collectively responsible for 32.7% of admissions, followed by Eastern European (26.1%) and Western European (3.9%) subjects.
The main distributions of foreign country provenance of the most prevalent patients (first ten countries) admitted to the ED and the proportion, according to nationality, relative to the respective resident foreign population are reported in Table III. The data highlight that the majority of admitted patients came from Morocco and Sri Lanka, but that the demographically highest proportion came from India.
Tab. III.
Foreign patients: countries of provenance (first ten countries), crude rate of admission to ED and rate of foreign patients according to the respective resident foreign population in Verona.
| Country of origin | Crude rate of admission to ED for foreign patients according to nationality out of total admitted foreigners (%) | Rate of foreign patients according to nationality in relation to the respective resident foreign population in Verona (%) |
|---|---|---|
| Morocco | 20.9 | 4.8 |
| Sri Lanka | 17.0 | 1.1 |
| India | 14.5 | 11.0 |
| Romania | 13.6 | 0.7 |
| Poland | 4.1 | 4.9 |
| Moldavia | 3.6 | 0.5 |
| Ghana | 3.6 | 1.2 |
| Senegal | 2.3 | 2.8 |
| Algeria | 1.6 | 2.5 |
| Albania | 1.1 | 0.3 |
Slightly more than half of the patients (59.3%) left the ED before concluding of all checks and the final visits. Among the remaining patients, one in three was discharged and sent to his GP and 0.4% was sent directly to Community Psychiatric Services.
Only 4.4% of patients were transferred to a hospital ward: 39.7% was admitted to the ED ward, 35.3% to the Medical Ward, 17.6% to the Surgical Ward, and 7.34% to the Psychiatric ward.
Discussion
By examining the population served by the Borgo Trento ED, this study sheds a different light onto the prevalence of AAI, which has otherwise only been appreciated within the contexts of mortality rate or hospitalization statistics.
During the six years studied 0.26% of all ED admittances were due to AAI. Among them the crude rate shows that almost 70% of admitted patients were native Italians. However, when the data were compared to the proportion of nationalities of Verona residents, it became apparent that this phenomenon concerns foreigners almost tree times more severely than native Italians (123.2/105 vs 46.4/105, respectively).
Recent Italian data report harmful uses of alcohol in 6.3% of Italians [18] and a higher rate (13.2%) in foreigners [19], which may explain the greater prevalence of AAI among foreign people found in this report.
Foreigners show diversified behaviors of alcohol consumption depending on their country of provenance, all of which are styles that differ from the Italian traditional one [20, 21]. This fact could be related to a general and widespread greater social disadvantage in comparison with the indigenous population, to difficulties with integration (language, racism), to socio-economic difficulties (finding a job, food, housing, and obtaining documents), to a need to decrease anxiety, to increased availability of alcohol compared to countries of origin (due to legal, religious, or economic reasons). All of these reasons can facilitate alcohol use and abuse, leading to episodes of acute intoxication and/or to chronic alcoholism [22].
In comparison to the Epicentro Italian study [23], in which a greater prevalence of AAI was found among Romanian, Albanian, and Polish people, our data reports a higher prevalence, as crude rate, in patients coming from Morocco, Sri Lanka, India, and Romania.
From the analysis of age groups, a constant higher prevalence along the week emerged in patients aged 21 to 55. A significant peak was observed over the weekend only among younger patients (aged < 21 years), who instead show the lowest prevalence between Monday and Friday. According to National data (Istat, 2013) [7, 18], this weekend peak, as well as the higher prevalence during evenings and nights, could reflect the predominant lifestyle adopted by young people during recent years, which includes an increase in socially shared and emulated transgressions and risky behaviors [24].
Furthermore, it is necessary to consider that both occasional and chronic alcohol abuse may be a sign of social and personal difficulties, such as those related to work, social, or personal problems, all of which appear to have increased in the past few years [25].
Data are in accordance with what has emerged from the BALs calculated for accesses during the week relative to age: the majority of younger patients (< 20 years) were classified into the lower level category, and had probably resorted to ED care either because they were less experienced and more disconcerted by their symptoms, or perhaps due to a rising tendency among younger generations to seek professional care no matter the extent of symptomatic distress.In accordance with national data regarding the higher prevalence of alcohol consumption [24], alcohol intoxication with clinical symptoms (moderate and critical and BALs) is mostly found among 31- to 40-year-olds, and even more among 41- to 50-year-olds, probably, as above discussed, mainly due to social, economic, and personal causes. It was within these age groups, as a matter of fact, that we found the majority of divorced/separated and single patients with AAI, which might consequentially have a greater perception of loneliness, and of economic and social difficulties. On the other hand we must also consider the reverse hypothesis, i.e. that alcohol abuse may lead to break-ups and dysfunction within family life, resulting in a deterioration of the psychological and living situation of the patient. Thirdly, a two way process with both factors influencing each other may be at play, making it hard to discern a clear cause-and-effect relationship. An exception is found in the youngest age group over the weekend, which represents the moment of the week when social gatherings, and hence the tendency to abuse alcohol, are more frequent [26]. Although a small number of patients were classified and treated with Code Red (1.9%), which is certainly the most challenging and expensive in sanitary terms, the higher prevalence of Green (67.7%) and Yellow (25.8%) Codes are still responsible for the largest portion of healthcare costs for the ED in terms of space, personnel involved, and specific therapeutic interventions [27].
Conclusions
Access to the ED is only the tip of the iceberg of the acute and chronic alcohol abuse that represents a major health and social problem among the population [28-30].
The significantly high costs encountered are related to a number of factors: medical interventions (use of emergency services and medical specialists, and diagnostic and therapeutic care); social burden (due to road, occupational, and domestic accidents, risky sexual behaviors, fetal alcohol spectrum disorders, criminal acts, social problems and psychiatric distress, and increase in alcohol-related diseases); and years of life lost due to premature mortality and disability attributable to alcohol (DALYs) [25, 31, 32].
The findings highlighted by this study concern only ED accesses, but in fact the phenomenon is much more serious when one considers that in Italy official statistics report a minimum of 30,000 hospitalizations and 800 deaths per year due to AAI [15].
EDs undoubtedly play a very important role when it comes to providing relief to the phenomenon of AAI.
The worrisome entity of the impact of alcohol abuse, however, calls for an improved implementation of public health activities on a national scale, in order to prevent excessive alcohol use throughout the country and across all the ages. Policies should include a substantial involvement of the school system, of pediatricians and family doctors, of Local Health Departments, and of mass communication platforms (including e-channels).
References
- 1.Global status report on alcohol and health – 2014ed. WHO Library Cataloguing-in-Publication Data. http://apps.who.int/iris/bitstream/10665/112736/1/9789240692763_eng.pdf.
- 2.Management of substance abuse. Alcohol (WHO). http://www.who.int/substance_abuse/facts/alcohol/en/
- 3.Rehm J, Mathers C, Popova S, et al. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet. 2009;373:2223–2233. doi: 10.1016/S0140-6736(09)60746-7. [DOI] [PubMed] [Google Scholar]
- 4. ISTISAN ALCOOL 2014/1 http://www.iss.it/binary/alco4/cont/Rapporto_Istisan.pdf.
- 5.Anderson P., Møller L., Galea G. Alcohol in the European Union Consumption. Harm and policy approaches (WHO, 2012) http://www.euro.who.int/__data/assets/pdf_file/0003/160680/e96457.pdf. [Google Scholar]
- 6. Alcol e patologie correlate. Dipartimento delle dipendenze– Regione del Veneto, AULSS 20. http://alcol.dronet.org/epidemiologia/europa.html.
- 7. ISTAT. Uso e abuso da alcol in Italia, ed. 2012. http://www.istat.it/it/archivio/59033.
- 8.Scafato E, Ghirini S, Gandin C, et al. La mortalità alcol-attribuibile in Italia e nelle Regioni. Analisi delle cause di morte nei contesti territoriali e nelle differenti generazioni. Istituto Superiore Di Sanità. Osservatorio Nazionale Alcol (ONA) – CNESPS. Reparto Salute della Popolazione e suoi Determinanti. Rapporto 2014 http://www.epicentro.iss.it/alcol/apd2014/OK%20SCAFATO%20REVISIONE%20FACSHEET%20mortalit%C3%A0%20alcol%20attribuibile.pdf.
- 9.Gandin C, Galluzzo L, Martire S, et al. Epidemiologia e monitoraggio alcol-correlato in Italia e nelle Regioni. Valutazione dell'Osservatorio Nazionale Alcol-CNESPS sull'impatto del consumo di alcol ai fini dell'implementazione delle attività del Piano Nazionale Alcol e Salute. Rapporto 2014. http://www.iss.it/binary/publ/cont/14_1web.pdf.
- 10. DSM-IV-TR. Criteria for Alcohol Intoxication. http://www.hamsnetwork.org/dsm_intoxication/
- 11. National Institute on Alcohol Abuse and Alcoholism , author. Alcohol Use Disorder: A Comparison Between DSM-IV and DSM-5. http://pubs.niaaa.nih.gov/publications/dsmfactsheet/dsmfact.pdf.
- 12.Pirmohamed M, Brown C, Owens L, et al. The burden of alcohol misuse on an inner-city general hospital. QJM. 2000;93:291–295. doi: 10.1093/qjmed/93.5.291. [DOI] [PubMed] [Google Scholar]
- 13.Charalambous MP. Alcohol and the accident and Emergency Department: a current review. Alcohol. 2002;37:307–312. doi: 10.1093/alcalc/37.4.307. [DOI] [PubMed] [Google Scholar]
- 14.Pletcher MJ, Maselli J, Gonzales R. Uncomplicated alcohol intoxication in the Emergency Department: an analysis of the National Hospital Ambulatory Medical Care Survey. Am J Med. 2004;117:863–867. doi: 10.1016/j.amjmed.2004.07.042. [DOI] [PubMed] [Google Scholar]
- 15.Botti P, Cipriani F, Dannaoui B, et al. Acute intoxications and poisonings in Italian Emergency Rooms. Ann Ist Super Sanita. 2006;42:287–297. [PubMed] [Google Scholar]
- 16. The Surgeon General's Call to Action To Prevent and Reduce Underage Drinking. Appendix B: DSM-IV-TR Diagnostic Criteria for Alcohol Abuse and Dependence. http://www.ncbi.nlm.nih.gov/books/NBK44358/
- 17. Alcohol Dependence and Alcohol Abuse/Harmful Use: DSM-IV and ICD-10 Diagnostic Criteria. http://www.estreatment.org/wordpress/wp-content/uploads/2012/10/adc.pdf.
- 18. Tavole Istat, http://www.istat.it/it/archivio/117897.
- 19. http://www.epicentro.iss.it/alcol/apd2014/APD2014_perez_last1.pdf.
- 20.Pelliccia A. Alcol e immigrazione. Uno sguardo transculturale. Istituto di Fisiologia Clinica Sezione di Epidemiologia e Ricerca sui Servizi Sanitari CNR 2006. https://www.epid.ifc.cnr.it/AreaDownload/Pubblicazioni/ALCOL_E_IMMIGRAZIONE_%20Uno_sguardo_transculturale.pdf.
- 21.Salvioni P, Soria A, Feltrin R. Tossicodipendenza e immigrazione: analisi sociodemografica degli utenti di un servizio a bassa soglia d'accesso a Milano. Boll Farmacodip e Alcoolis 2002;XXV. http://www.unicri.it/min.san.bollettino/bulletin_it/2002-1%202/p101.pdf.
- 22.Carta MG, Bernal M, Hardoy MC, et al. Migration and mental health in Europe (the state of the mental health in Europe working group: appendix 1. Clin Pract Epidemiol Ment Health. 2005;1:13–18. doi: 10.1186/1745-0179-1-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dota F, Giorgio G, Perez M, et al. Il consumo di alcol tra i cittadini stranieri. Istat. Alcol Prevention Day, Roma, 9 Aprile 2014. http://www.epicentro.iss.it/alcol/apd2014/APD2014_perez_last1.pdf.
- 24.Mancinelli R, Fidente RM, Draisci R, et al. Donna e alcol: aggiornamenti in tema di ricerca clinica e preclinica. Rapporti ISTISAN 13/36 http://www.iss.it/binary/alco4/cont/Rapporto_Istisan.pdf.
- 25. Separazioni e divorzi in Italia. Anno 2012. Statistiche Istat. http://www.axerta.it/news/124/statistiche_separazioni_divorzi_italia.htm.
- 26.Cherpitel CJ. Emergency room and primary care services utilization and associated alcohol and drug use in the United States general population. Alcohol. 1999;34:581–589. doi: 10.1093/alcalc/34.4.581. [DOI] [PubMed] [Google Scholar]
- 27.Corser WD, Huebner M, Zhu Q. Predictors of 2010-2011 Michigan Medicaid Beneficiary Predictors of 2010-2011. Michigan Medicaid Beneficiary Adverse E-Code Health Care Encounters. J Patient Saf. 2015:215–219. doi: 10.1097/PTS.0000000000000206. [DOI] [PubMed] [Google Scholar]
- 28.Cherpitel CJ, Ye Y. Risky Drinking, Alcohol Use Disorders, and Health Services Utilization in the U.S. General Population: Data from the 2005 and 2010 National Alcohol Surveys. Alcohol Clin Exp Res. 2015:305–310. doi: 10.1111/acer.12801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cherpitel CJ, Ye Y. Drug use and problem drinking associated with primary care and emergency roomutilization in the US general population: data from the 2005 national alcohol survey. Drug Alcohol Depend. 2008;97:226–230. doi: 10.1016/j.drugalcdep.2008.03.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cherpitel CJ. Changes in substance use associated with emergency room and primary care services utilization in the United States general population: 1995-2000. Am J Drug Alcohol Abuse. 2003;29:789–802. doi: 10.1081/ada-120026261. [DOI] [PubMed] [Google Scholar]
- 31. Alcohol. Media Centre. Fact sheet. January 2015 http://www.who.int/mediacentre/factsheets/fs349/en/
- 32. Alcol. Informazioni generali. EpiCentro. http://www.epicentro.iss.it/alcol/alcol.asp.