Abstract
We aimed to assess the short-term outcomes of per-oral endoscopic myotomy (POEM) compared with laparoscopic Heller myotomy (LHM) for achalasia through a meta-analysis of nonrandomized comparative studies.
We searched PubMed, Embase, Medline, Cochrane Library, and Google Scholar for studies that compared POEM and LHM for achalasia and were published between January 1, 2008 and December 31, 2014. The Methodological Index for Nonrandomized Studies (MINORS) was used to evaluate the quality of the studies. Random- and fixed-effects meta-analytical models were used, and between-study heterogeneity was assessed.
Four nonrandomized comparative studies that included 317 patients (125 in the POEM group and 192 in the LHM group) met our research criteria and were assessed. There were no differences between the POEM and LHM groups in terms of sex, preoperative Eckhart score, length of myotomy, operation time, length of hospital stay, and complications. The patients in the POEM group were older than those in the LHM group (MD =2.81, 95% CI 0.27–5.35; P = 0.03) with high between-study homogeneity (χ2 = 1.96, df = 2, I2 = 0%; P = 0.38). The patients in the POEM group had a lower Eckardt score after surgery compared with those in the LHM group (MD = −0.30, 95% CI −0.42 to −0.18; P < 0.001) with high between-study homogeneity (χ2 = 0.00, df = 1, I2 = 0%; P = 1.00).
The efficacy and safety of POEM appear to be comparable to those of LHM. Multicenter and randomized trials with larger sample size are needed to further compare the efficacy and safety of POEM and LHM for the treatment of achalasia.
INTRODUCTION
Achalasia is a motility disorder of the esophagus that presents with symptoms of dysphagia, regurgitation of undigested food, respiratory symptoms (nocturnal cough, recurrent aspiration, and pneumonia), chest pain, and weight loss.1,2 Treatments of achalasia include pharmacologic agents (nitrates and calcium-channel blockers), botulinum toxin injection (BTI), pneumatic dilatation (PD), laparoscopic Heller myotomy (LHM), per-oral endoscopic myotomy (POEM), and esophagectomy for end-stage achalasia.2 Pharmacologic agents are only suitable for those with mild symptoms, frail elderly patients, and those unable to receive other treatments. BTI should be limited to patients who are not candidates for more effective therapies because of a higher rate of recurrence of symptoms within 12 months.3 The Heller myotomy is a long-standing treatment for achalasia. It was first described in 1913 by German surgeon Ernst Heller and has been widely used with few technical changes.4 In 1991, with the advent of minimally invasive surgery, laparoscopic management was added.5 A growing body of evidence suggests that LHM offers better visualization of the distal esophageal muscle layers and the sling fibers of the gastric fundus, resulting in superior long-term efficacy and significantly less retreatment compared with PD, and the success rate of PD after 10 to 15 years is only 40% to 50%, even after several endoscopic sessions.6 Therefore, LHM is considered the first-line treatment and the gold standard for surgical therapy for achalasia.7–9
POEM was first performed on 17 patients by Inoue in 2008.10 Since then, the procedure has been increasingly utilized and has become a developed endoscopic technique for the treatment of achalasia. POEM incorporates concepts of natural orifice transluminal endoscopic surgery and expands upon the techniques used in endoscopic submucosal dissection to achieve a division of the esophageal circular muscle fibers across the esophagogastric junction and into the stomach.11,12 As a result, POEM integrates the theoretical advantages of both endoscopic dilation (no skin incisions, decreased pain, and less blood loss) and LHM (durable surgical myotomy and single procedure) and is a less invasive flexible endoscopic alternative. However, there is still no consensus as to whether LHM or POEM has greater efficacy and safety in the management of achalasia. Therefore, we compared the pre-, intra-, and postoperative outcomes using a meta-analysis based on several existing nonrandomized comparative studies (NRCS) published between 2008 and 2014.
METHODS
Data Sources
We systematically searched PubMed, Embase, Medline, Cochrane Library, and Google Scholar for relevant studies published from January 1, 2008 to December 31, 2014. The search strategy was (achalasia) AND (per oral endoscopic myotomy OR POEM) AND (laparoscopic Heller myotomy OR LHM). We also searched the reference lists of selected articles, conference proceedings, and personal files for relevant citations. The literature search was limited to the English language. Duplicate publications were excluded.
Study Selection
All relevant studies reporting comparisons between POEM and LHM to treat achalasia were considered for analysis. The studies presented the short-term outcomes of the intervention. If more than 1 article was published on the same cohort, only the study with the latest data was included. In the case of articles without sufficient data, we emailed the first author or corresponding author requesting more information. Ujiki provided original data, and Kumbhari et al13 provided updated data instead of the published data. All analyses in this meta-analysis were based on previously published studies, so no ethical approval or patient consent was required.
Data Extraction
Information, such as the summary of the study and items of pre-, intra-, and postoperative assessment, was extracted by 2 reviewers (YZ and XC) independently from each study into a structured dataset and compared. Summaries of studies included first author, year of publication, region, study design, time type, study period, and number of patients enrolled in POEM and LHM. The preoperative assessment consisted of age, sex, and Eckardt scores. Intraoperative indexes were the length of the myotomy and the operation time. Postoperative outcomes were Eckardt scores, length of stay, and complications, such as subcutaneous emphysema and perforation. Number, mean, and standard deviations were extracted from the articles. All disagreements were resolved by reaching consensus, and there was complete agreement on the extracted results in the final dataset.
Quality Assessment
All studies that met the selection criteria were assessed for methodological quality by 2 reviewers (HW and LL) independently. The quality of these nonrandomized trials was assessed using the Methodological Index for Nonrandomized Studies (MINORS).14 This index contains 12 items that are scored as 0 (not reported), 1 (reported but inadequate), or 2 (reported and adequate). The ideal total score is 24 for comparative studies. NRCS with a MINORS score higher than 12 were retained for analysis.
Statistical Analysis
The meta-analysis was performed in line with recommendations from the Cochrane Collaboration and the Quality of Reporting of Meta-analyses Guidelines.15,16 The odds ratio (OR) was used for dichotomous variables, and the mean difference (MD) was used for continuous variables. The OR and MD were considered to be statistically significant at a P value less than 0.05. We assessed heterogeneity using the Cochran Q test by the χ2 and I2. Higher χ2 and I2 indicate greater heterogeneity. The assumption of homogeneity between the groups was deemed invalid if the P value was less than 0.1, and the random-effects model was reported after exploring the causes of heterogeneity. Otherwise, the fixed-effects model was reported.17 Tests for funnel plot asymmetry are not appropriate for meta-analyses with 10 or fewer studies.18 Analyses were performed using Review Manager version 5.3.5 (The Nordic Cochrane Centre, The Cochrane Collaboration, 2014) and STATA IC version 13.1 (StataCorp, College Station, TX).
RESULTS
Characteristics of Included Studies
Using the predefined search strategy, 33 publications were identified, and 26 were excluded after title and abstract review. These included 1 animal study, 7 reviews, and 18 studies that were either irrelevant or noncomparative. The remaining 7 studies were fully reviewed, and 2 authors provided their original data upon request. Of these, 3 studies were excluded because of 1 lacked complete data and 2 had small sample sizes of the same patients from the same hospitals. The flow diagram is shown in Figure 1. Finally, 4 studies fulfilled the selection criteria and were included in the meta-analysis.19–22
FIGURE 1.
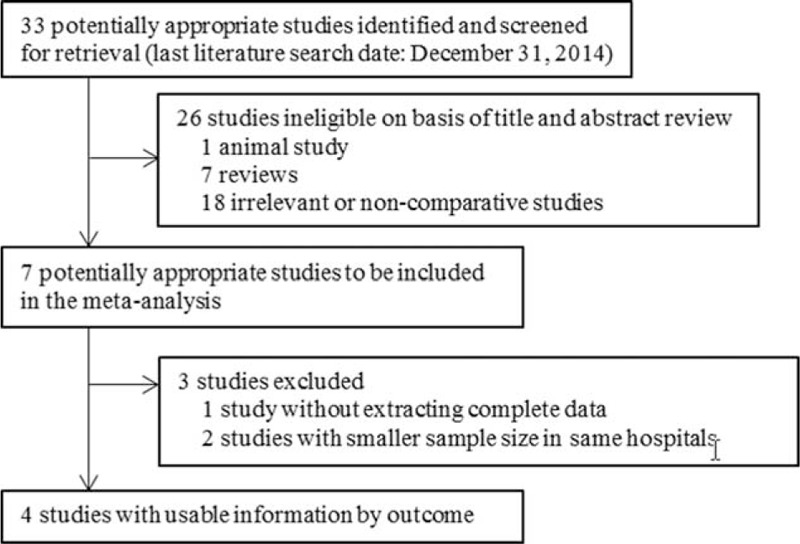
Study flow diagram for nonrandomized comparative studies of per-oral endoscopic myotomy versus laparoscopic Heller myotomy for achalasia.
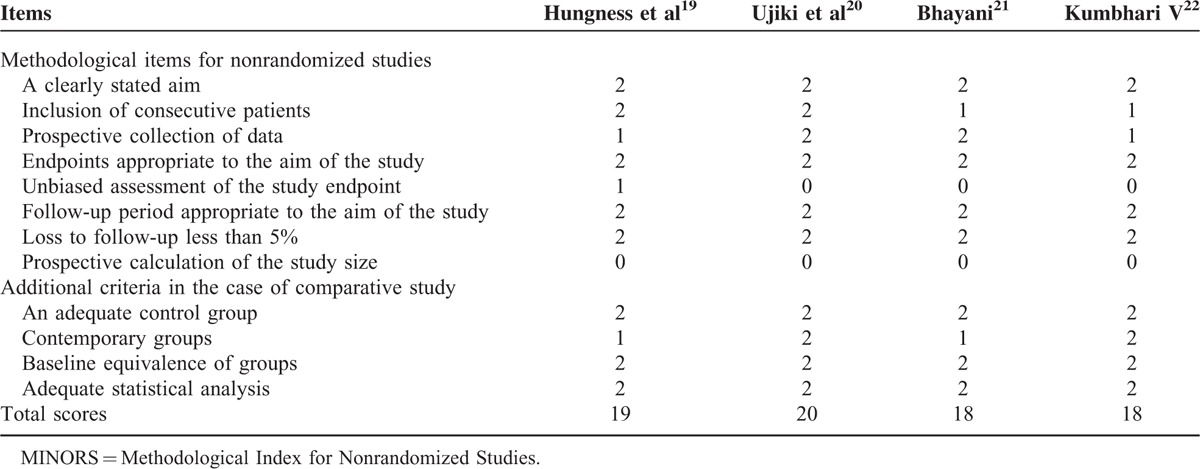
The 4 studies were of high quality, with scores of 18 to 20 under the evaluation of the Methodological Index for Nonrandomized Studies (MINORS). Quality scores for the 4 studies are shown in Table 1.
TABLE 1.
Quality Assessment Using MINORS
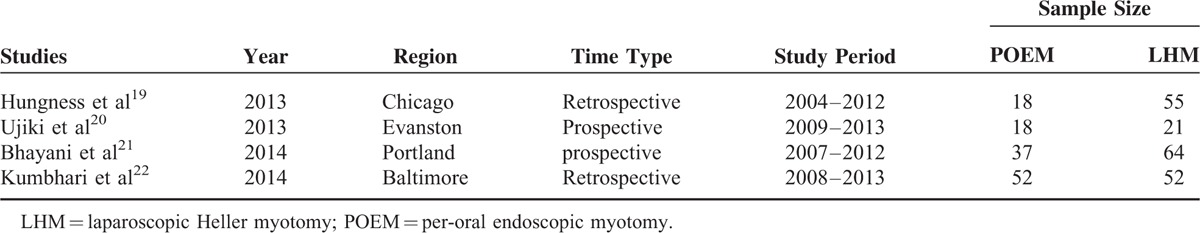
Analysis was performed on 125 patients in the POEM group and on 192 patients in the LHM group at US hospitals. The study characteristics are shown in Table 2. Pooling the data of 4 studies that assessed sex showed no significant difference (P > 0.05) between the 2 groups. The patients in the POEM group were older than those in the LHM group (MD = 2.81, 95% CI 0.27–5.35; P = 0.03) with high between-study homogeneity (χ2 = 1.96, df = 2, I2 = 0%; P = 0.38).
TABLE 2.
Demographic Characteristics of Included Studies
Meta-Analysis of Short-Term Efficacy and Safety
Length of Myotomy
Three studies19,20,22 assessed the length of myotomy in 216 patients and showed no significant difference (MD = 1.49, 95% CI 0.02–2.95; P = 0.05) with high between-study heterogeneity (χ2 = 12.88, df = 2, I2 = 84%; P < 0.001).
Operation Time
Operation time was available for 216 patients across 3 studies.19,20,22 There was no significant difference in operation time (MD = −55.62, 95% CI −145.96–34.71; P = 0.23) with high between-study heterogeneity (χ2 = 203.46, df = 2, I2 = 99%; P < 0.001).
Length of Stay
Length of stay was reported in 4 studies.19–22 There was no difference between the POEM and LHM groups (MD = −0.42, 95% CI −1.26–0.43; P = 0.33) with high between-study heterogeneity (χ2 = 15.22, df = 3, I2 = 80%; P < 0.001).
Eckardt Scores
Data on preoperative Eckardt scores were extracted from 3 studies assessing 244 patients.20–22 The scores had no significant difference (MD = 0.24, 95% CI −0.61–1.08; P = 0.58) with high between-study heterogeneity (χ2 = 27.47, df = 2, I2 = 93%; P < 0.001).
Only 2 studies20,22 reported postoperative Eckardt scores. There was difference significantly between the 2 groups (MD = −0.30, 95% CI −0.42 to −0.18; P < 0.001) with high between-study homogeneity (χ2 = 0.00, df = 1, I2 = 0%; P = 1.00). The patients in the POEM group had lower Eckardt scores after surgery compared with the LHM group.
Complications
Three studies19,20,22 reported adverse events, including subcutaneous emphysema, perforation, atrial fibrillation, and urinary retention. These complications did not differ between the POEM and LHM groups (OR 1.53, 95% CI 0.65–3.59; P = 0.33) with high between-study homogeneity (χ2 = 1.06, df = 2, I2 = 0.0%; P = 0.59)
Study outcomes are shown in Table 3 and Figure 2.
TABLE 3.
Results of Meta-Analysis Comparing POEM Versus LHM for Achalasia
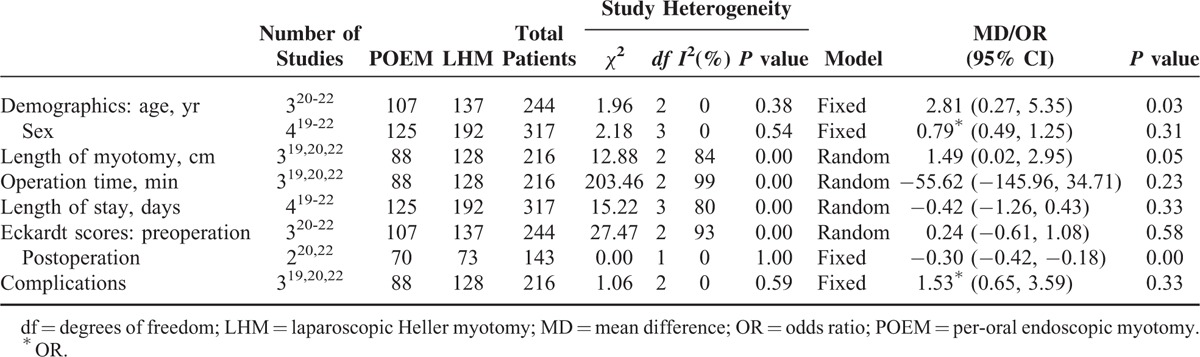
FIGURE 2.
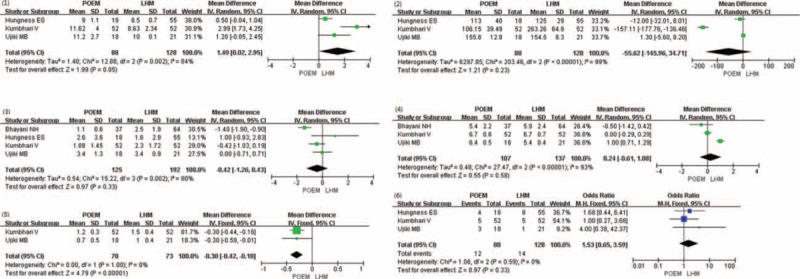
Outcomes of POEM versus LHM for achalasia in terms of length of myotomy (1), operation time (2), length of stay (3), preoperative Eckardt scores (4), postoperative Eckardt scores (5), and complications (6). Squares are the point estimates of the treatment effect (MD/OR) with 95% CI indicated by horizontal bars. Diamonds are the summary estimate from the pooled studies with 95% CI.
DISCUSSION
Achalasia is a neurodegenerative motility disorder of the esophagus resulting in deranged esophageal peristalsis and function loss of the lower esophageal sphincter (LES). It is a rare disease with an incidence of approximately 1/100,000 per year.23 Its most common form is idiopathic achalasia, which usually occurs sporadically. Achalasia results from the disappearance of the myenteric neurons that coordinate esophageal peristalsis and relaxation of the LES.24 Although the exact etiology remains unknown, the most widely accepted theory is that environmental or viral exposures result in inflammation of the esophageal myenteric plexus, which elicits an autoimmune attack in individuals with a genetic predisposition.23 Patients often have a long medical history of suffering before the diagnosis is made and adequate therapy is provided. The current gold standard for treatment is LHM. The muscle layer of the distal esophagus and LES is known as the Heller. LHM is performed to cut the Heller that joins the esophagus and stomach. This limits the activity of the muscle and allows food to pass more easily into the stomach, relieving most patients of their symptoms. Both Dor and Toupet partial fundoplication provide comparable control of reflux after LHM.2,25 It is preferentially performed via the laparoscopic route and combined with partial fundoplication. POEM, an alternative to a Heller myotomy via the endoscopic route per oral, is under intensive investigation in several centers worldwide.26 POEM is performed by creating a submucosal tunnel through a natural body orifice. An endoscopic myotomy of circular muscle bundles is then performed, maintaining the integrity of the longitudinal muscle.10 Smooth passage of an endoscope through the gastroesophageal junction is confirmed at the end of the procedure.27 In our experience, the patients with repeated balloon dilatation, indeed, have the problem of the adhesion of LES muscle layer, and this condition makes the operation of POEM more difficult. POEM was forbidden to patients who with severe fibrosis and whose tunnel was not successfully established.
To date, few reports have compared POEM and LHM prospectively and randomly. One recent article28 on POEM with a review and meta-analysis states that POEM has similar outcomes as LHM. However, the 5 studies included in that meta-analysis have some limitations, including overlapping case within the same period between the studies of Teitelbaum et al29 and Hungness et al,19 and overlapping case in the absence or presence of prior achalasia treatment between the studies of Vigneswaran et al30 and Ujiki et al.20 Therefore, the study of Teitelbaum et al29 with a sample size and the study of Vigneswaran et al30 after prior LHM may affect the final results. Based on the above considerations, we ultimately included 4 articles from 4 different institutions. Moreover, Kumbhari et al22 provided their updated data to us with more patients than were included in the article, which was published in 2014.13 This was precisely the advantage of our meta-analysis, with a larger sample size of patients and more stringent inclusive and exclusive criteria for searching the literature. This guaranteed a high quality of results. From the short-term efficacy of our research, we found that POEM was similar to LHM. There were no differences between the POEM and LHM groups in terms of sex, preoperative Eckardt score, length of myotomy, operation time, or length of hospital stay. The patients in the POEM group were older than those in the LHM group (MD = 2.81, 95% CI 0.27–5.35; P = 0.03) with high between-study homogeneity (χ2 = 1.96, df = 2, I2 = 0%; P = 0.38). However, the patients in the POEM group had lower Eckardt scores after surgery compared with the LHM group (MD = −0.30, 95% CI −0.42 to −0.18; P < 0.001) with high between-study homogeneity (χ2 = 0.00, df = 1, I2 = 0%; P = 1.00). Fundoplication was not performed after POEM. In the LHM group, antireflux surgery consisted of 27 (42%) Toupet fundoplications and 37 (58%) Dor fundoplications.21 The efficacy of LHM is also associated with the type of achalasia, and poor efficiency is always associated with a sigmoid esophagus. However, Inoue and colleagues report successful POEM in 16 of 105 patients with sigmoid achalasia.31 Regarding short-term safety, there were no differences between the POEM and LHM groups in terms of complications. Esophageal perforation is the major complication of these 2 operations and is partly due to personal reasons, such as not following the doctor's advice regarding eating. If the postoperative surgical site does not restore, and the patients do not eat properly, surgical incision damage (iatrogenic) will be increased. That leads to perforation, but surgery is not a direct result of perforation. Imaging of digestive tract with oral meglumine diatrizoate will be used. If the contrast agent spilles out of the esophagus, perforation will be confirmed. Minor complications include subcutaneous emphysema, atrial fibrillation, urinary retention, anterior vagus nerve division, and splenic capsule tear.19 A relatively rare complication is mediastinal sepsis, which has a POEM mortality of approximately 1/900,31 similar to or even lower than that of LHM. Complications of Heller include dysphagia, inability to belch, and early satiety because of esophageal wrap.21
Apart from the above outcomes analyzed in the meta-analysis, short-term prognosis also includes recovery time, postoperative pain, time until the patient can start eating, and length of complications. Cost should be taken into account. In our study, only Kumbhari et al22 mentioned cost. POEM incurred significantly lower total charges than LHM ($14,481 vs. $17,782, P = 0.017). POEM in-room charges were significantly less than those for LHM ($5070 vs. $7616, P < 0.001). When the charges incurred due to the procedure itself (in-room, supplies, drugs) were compared, POEM was associated with cost savings compared with LHM ($9756 vs. $11,136, P = 0.015). In addition, the charges incurred due to the inpatient hospital stay were significantly less with POEM than with LHM ($2771 vs. $5206, P = 0.006).
There is currently intense research comparing POEM and LHM for achalasia, but information on the long-term efficacy of POEM is lacking. Whether POEM diminishes in efficacy with time is a concern, so more studies of its long-term effects are needed.32 Currently, the array of follow-up evaluation systems from different studies is overwhelming. We recommend that studies should include symptom evaluations and objective parameters at the 1-month, 3-month, 6-month, and 1-year postoperative clinical visits. Symptoms can be easily evaluated by Eckardt scores. The evaluation was as follows:33 depending on whether weight loss, dysphagia, retrosternal pain, and regurgitation occurred occasionally, daily, or several times during the day, a symptom score ranging from 0 to 3 could be determined. A completely asymptomatic patient would have a symptom score of 0, whereas a severely affected patient could have a symptom score of up to 12. Patients are considered to have reached clinical remission if symptoms have totally disappeared or if they did not exceed a score of 3 over a period of at least 6 months after therapy. Objective follow-up should include the percent of emptying after timed barium swallow, esophagitis through gastroscopy, high-resolution manometry, 24-hour pH probe, and complications (eg, iatrogenic gastroesophageal reflux).34,35
Based on the literature, POEM is indeed a promising procedure. The potential specific advantages of POEM may include the following:31 easy extension of the myotomy to any length, permitting long myotomies that may be optimal for patients with diffuse esophageal spasm or other disorders with long hypercontractile esophageal segments. Less risk of injury to the vagus nerve. POEM is performed under endoscopy without needing laparoscopy and entering the abdominal cavity. So the risk of damaging to the vagus nerve will be much lower than LHM. Less reflux because attachments of the esophagus, such as the phrenoesophageal membrane, are not disrupted. Less pain than in LHM. However, some concerns on this new technique were raised by Allaix and Patti6 and should be considered: POEM is a very demanding technique that requires great skill, and the learning curve is quite long. Most surgeons worldwide have not yet mastered it. Although several studies have reported a significant reduction in pressure in the LES, the pressure did not reach the effective long-term pressure standard. Revisional surgery in patients with recurrent dysphagia after POEM can be challenging. The presence of adhesions between the submucosa and the longitudinal muscle layer after POEM could make dissection very difficult in this area.
Our study also had some limitations. Because the comparative research about efficacy and safety of POEM versus LHM for achalasia was a relatively new research field, the published literatures were not so much. Only 4 studies fulfilled the selection criteria and were included in the meta-analysis. And none of these 4 studies was randomized controlled trials (RCTs). Analysis of publication bias was not performed because of the limited number of studies. There was heterogeneity among operation time, length of stay, and Eckardt scores. The majority of the studies only provided short-term follow-up data. And lacking data of analyzing long-term effects was the limitation of the current studies. The cost analysis of POEM and LHM should be taken into account, but only 1 study addressed this.22 Although these are relatively limited and retrospective data, they appear to suggest at least equivalence between the 2 procedures in terms of operation time, length of hospital stay, and complications. The lower Eckardt scores after surgery, with POEM being at a nascent stage and LHM at a very mature and fully developed stage, likely portend dominance of POEM in the not too distant future.31 Therefore, although achalasia is a very rare disease, RCTs to compare POEM with LHM should be performed, and longer follow-up is needed before accepting POEM as a more mature treatment option for achalasia.
CONCLUSIONS
The short-term efficacy and safety of POEM appears to be comparable to LHM. Multicenter RCTs with larger samples are needed to further compare the short-term role of POEM and LHM with fundoplication for the treatment of achalasia.
Footnotes
Abbreviations: BTI = botulinum toxin injection, LES = lower esophageal sphincter, LHM = laparoscopic Heller myotomy, MD = mean difference, MINORS = Methodological Index for Nonrandomized Studies, NRCS = nonrandomized comparative studies, OR = odds ratio, PD = pneumatic dilatation, POEM = per-oral endoscopic myotomy, RCT = randomized controlled trial.
This study was supported by the Seed Fund of the 2nd Hospital of Shandong University (S2015010023).
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Richter JE, Boeckxstaens GE. Management of achalasia: surgery or pneumatic dilation. Gut 2011; 60:869–876. [DOI] [PubMed] [Google Scholar]
- 2.Boeckxstaens GE, Zaninotto G, Richter JE. Achalasia. Lancet 2014; 383:83–93. [DOI] [PubMed] [Google Scholar]
- 3.Vaezi MF, Richter JE, Wilcox CM, et al. Botulinum toxin versus pneumatic dilatation in the treatment of achalasia: a randomised trial. Gut 1999; 44:231–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Heller E. Extramucosal cardioplasty for chronic cardiospasm with esophageal dilation. Mitt Greenzgeb Med Chir 1913; 27:8. [Google Scholar]
- 5.Shimi S, Nathanson LK, Cuschieri A. Laparoscopic cardiomyotomy for achalasia. J R Coll Surg Edinb 1991; 36:152–154. [PubMed] [Google Scholar]
- 6.Allaix ME, Patti MG. New trends and concepts in diagnosis and treatment of achalasia. Cir Esp 2013; 91:352–357. [DOI] [PubMed] [Google Scholar]
- 7.Yaghoobi M, Mayrand S, Martel M, et al. Laparoscopic Heller's myotomy versus pneumatic dilation in the treatment of idiopathic achalasia: a meta-analysis of randomized, controlled trials. Gastrointest Endosc 2013; 78:468–475. [DOI] [PubMed] [Google Scholar]
- 8.Schoenberg MB, Marx S, Kersten JF, et al. Laparoscopic Heller myotomy versus endoscopic balloon dilatation for the treatment of achalasia: a network meta-analysis. Ann Surg 2013; 258:943–952. [DOI] [PubMed] [Google Scholar]
- 9.Schoenberg MB, Vassiliou MC, von Renteln D. Achalasia: advances in treatment. Expert Rev Gastroenterol Hepatol 2014; 8:767–773. [DOI] [PubMed] [Google Scholar]
- 10.Inoue H, Minami H, Kobayashi Y, et al. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy 2010; 42:265–271. [DOI] [PubMed] [Google Scholar]
- 11.Rattner D, Kalloo A. ASGE/SAGES Working Group. ASGE/SAGES Working Group on Natural Orifice Translumenal Endoscopic Surgery. October 2005. Surg Endosc 2006; 20:329–333. [DOI] [PubMed] [Google Scholar]
- 12.Othman MO, Wallace MB. Endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD) in 2011, a Western perspective. Clin Res Hepatol Gastroenterol 2011; 35:288–294. [DOI] [PubMed] [Google Scholar]
- 13.Kumbhari V, Tieu A, Azola A, et al. Tu1354 PerOral Endoscopic Myotomy (POEM) is equivalent to laparoscopic Heller myotomy (Lhm) for the treatment of achalasia. Gastrointestinal Endoscopy 2014; 79:AB509–AB510. [Google Scholar]
- 14.Slim K, Nini E, Forestier D, et al. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 2003; 73:712–716. [DOI] [PubMed] [Google Scholar]
- 15.Clarke M, Horton R. Bringing it all together: Lancet-Cochrane collaborate on systematic reviews. Lancet 2001; 357:1728. [DOI] [PubMed] [Google Scholar]
- 16.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 2009; 62:1006–1012. [DOI] [PubMed] [Google Scholar]
- 17.Lau J, Ioannidis JP, Schmid CH. Quantitative synthesis in systematic reviews. Ann Intern Med 1997; 127:820–826. [DOI] [PubMed] [Google Scholar]
- 18.Rothstein HR, Sutton AJ, Borenstein M. Publication Bias in Meta-Analysis: Prevention, Assessment and Adjustments. 376: WILEY; ISBN: 978-0-470-87014-3; 2005. [Google Scholar]
- 19.Hungness ES, Teitelbaum EN, Santos BF, et al. Comparison of perioperative outcomes between peroral esophageal myotomy (POEM) and laparoscopic Heller myotomy. J Gastrointest Surg 2013; 17:228–235. [DOI] [PubMed] [Google Scholar]
- 20.Ujiki MB, Yetasook AK, Zapf M, et al. Peroral endoscopic myotomy: a short-term comparison with the standard laparoscopic approach. Surgery 2013; 154:893–900. [DOI] [PubMed] [Google Scholar]
- 21.Bhayani NH, Kurian AA, Dunst CM, et al. A comparative study on comprehensive, objective outcomes of laparoscopic Heller myotomy with per-oral endoscopic myotomy (POEM) for achalasia. Ann Surg 2014; 259:1098–1103. [DOI] [PubMed] [Google Scholar]
- 22.Kumbhari V, Tieu AH, El Zein MH, et al. Peroral endoscopic myotomy (POEM) achieves similar clinical response but incurs lesser charges compared to Heller myotomy (HM) for the treatment of achalasia. 2015; Washington, DC: Digestive Disease Week, 2014 updated data. [Google Scholar]
- 23.O’Neill OM, Johnston BT, Coleman HG. Achalasia: a review of clinical diagnosis, epidemiology, treatment and outcomes. World J Gastroenterol 2013; 19:5806–5812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Boeckxstaens GE. The lower oesophageal sphincter. Neurogastroenterol Motil 2005; 17:13–21. [DOI] [PubMed] [Google Scholar]
- 25.Achalasia. Available at: http://www.uchospitals.edu/specialties/gi/esophageal/achalasia/, Accessed January 2015. [Google Scholar]
- 26.von Rahden BH, Filser J, Seyfried F, et al. Diagnostics and therapy of achalasia. Chirurg 2014; 85:1055–1063. [DOI] [PubMed] [Google Scholar]
- 27.Katada N, Sakuramoto S, Yamashita K, et al. Recent trends in the management of achalasia. Ann Thorac Cardiovasc Surg 2012; 18:420–428. [DOI] [PubMed] [Google Scholar]
- 28.Talukdar R, Inoue H, Reddy DN. Efficacy of peroral endoscopic myotomy (POEM) in the treatment of achalasia: a systematic review and meta-analysis. Surg Endosc 2015; 29:3030–3046. [DOI] [PubMed] [Google Scholar]
- 29.Teitelbaum EN, Rajeswaran S, Zhang R, et al. Peroral esophageal myotomy (POEM) and laparoscopic Heller myotomy produce a similar short-term anatomic and functional effect. Surgery 2013; 154:885–892. [DOI] [PubMed] [Google Scholar]
- 30.Vigneswaran Y, Yetasook AK, Zhao JC, et al. Peroral endoscopic myotomy (POEM): feasible as reoperation following Heller myotomy. J Gastrointest Surg 2014; 18:1071–1076. [DOI] [PubMed] [Google Scholar]
- 31.Stavropoulos SN, Friedel D, Modayil R, et al. Endoscopic approaches to treatment of achalasia. Therap Adv Gastroenterol 2013; 6:115–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Friedel D, Modayil R, Stavropoulos SN. Per-oral endoscopic myotomy: major advance in achalasia treatment and in endoscopic surgery. World J Gastroenterol 2014; 20:17746–17755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Eckardt VF, Gockel I, Bernhard G. Pneumatic dilation for achalasia: late results of a prospective follow up investigation. Gut 2004; 53:629–633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Swanstrom LL, Kurian A, Dunst CM, et al. Long-term outcomes of an endoscopic myotomy for achalasia: the POEM procedure. Ann Surg 2012; 256:659–667. [DOI] [PubMed] [Google Scholar]
- 35.Pescarus R, Shlomovitz E, Swanstrom LL. Per-oral endoscopic myotomy (POEM) for esophageal achalasia. Curr Gastroenterol Rep 2014; 16:369. [DOI] [PubMed] [Google Scholar]


