Abstract
In spite of the substantial burden of atrial fibrillation and associated elevated ischemic stroke risk in patients undergoing hemodialysis, the role of warfarin in these high-risk patients remains uncertain. Our objective was to clarify the association between warfarin use and risk of stroke for patients with atrial fibrillation undergoing dialysis.
PubMed and Embase from January 1966 to January 2015 were searched to identify relevant studies. Inclusion criteria were cohort studies, patients with atrial fibrillation undergoing hemodialysis, and reported quantitative estimates of the multivariate adjusted relative risk (RR) and 95% confidence interval (CI) for future stroke associated with warfarin use. We identified 8 studies, with a total of 9539 participants and 706 stroke events. Three studies reported total stroke as primary endpoint and other studies reported ischemic stroke as primary endpoint. Pooling the results showed that warfarin use was associated with higher risk of any stroke (RR 1.50, 95% CI: 1.13–1.99). By stroke type, warfarin was not significantly linked to risk of ischemic stroke (RR 1.01, 95% CI: 0.65–1.57, P = 0.97), but was related to greater hemorrhagic stroke risk (RR 2.30, 95% CI: 1.62–3.27). Warfarin heightened overall bleeding risk (RR 1.27, 95% CI: 1.03–1.56), but not death (RR 0.67, 95% CI: 0.37–1.21).
Among patients with atrial fibrillation undergoing hemodialysis, use of warfarin is associated with a higher risk of hemorrhagic stroke, but did not increase overall mortality.
INTRODUCTION
Patients undergoing hemodialysis are at elevated risk of both ischemic and hemorrhagic stroke.1 Atrial fibrillation is the most common cardiac source of embolism and is associated with a 5-fold increased risk of stroke as compared with age-matched controls.2,3 About 1% of adults in general population have atrial fibrillation4 and among patients undergoing hemodialysis, the prevalence of atrial fibrillation is estimated to be 7% to 20%.5 Studies also show that atrial fibrillation confers an increased risk of ischemic stroke in hemodialysis patients.6,7
Anticoagulation therapies, such as warfarin, are recommended in patients with atrial fibrillation to prevent ischemic stroke.8,9 In spite of the substantial burden of atrial fibrillation and associated elevated ischemic stroke risk in patients undergoing hemodialysis, the role of warfarin in these high-risk patients remains uncertain. Hemodialysis patients have dysfunctional platelets and receive heparin during their dialysis treatment, thus warfarin use in dialysis patients may confer additional bleeding risk as compared to general population.10–12 Clinical trials testing the efficacy of anticoagulants for stroke prevention have largely excluded patients receiving hemodialysis. Thus it is not clear whether warfarin use is beneficial or harmful for these patients.
We therefore carried out a systematic review and meta-analysis of cohort studies to clarify the association of warfarin use and risk of stroke for patients with atrial fibrillation undergoing hemodialysis.
METHODS
Search Strategy
The search strategy was done according to the recommendations of the Meta-analysis Of Observational Studies in Epidemiology (MOOSE) consensus group.13 Ethical review was waived because this is a meta-analysis with the data extracted from published articles. We searched PubMed (January 1966 to January 3, 2014) and Embase (January 1966 to January 3, 2014), using the following search strategy: “glomerular filtration rate” or “renal disease” or “kidney dysfunction” or “chronic kidney disease” or “end stage renal disease” or “dialysis” and “warfarin” or “coumadin” or “anticoagulant” or “vitamin K antagonist” and “atrial fibrillation.” No search software was used. Our search was limited to studies in humans. We focused only on data in published papers. No language restrictions were applied. One investigator (ML) would be responsible for articles published only in Chinese while another investigator (KSH) would be responsible for articles published only in Korean. Further information was retrieved through a manual search of references from relevant published original studies and reviews. We did not contact authors for further information.
Selection Criteria
Inclusion criteria were prospective or retrospective cohort studies, patients with atrial fibrillation undergoing hemodialysis at baseline, assessed stroke as an endpoint during the follow-up period, intended follow-up of at least 1 year for all participants, and reported estimates of the multivariate adjusted, or propensity score matched, relative risk (RR) and 95% confidence interval (CI) for future stroke associated with warfarin use. Studies including small amounts (<20%) of patients receiving peritoneal dialysis were included. We excluded studies that only reported unadjusted RR.
Data Extraction
We extracted the following information about the studies: study characteristics (first author's name, publication year, study country, population, follow-up years, number of participants, number of participants with warfarin use), participants’ characteristics (mean age, percentage of women, % of stroke history at baseline), reported end points (total stroke, ischemic stroke, hemorrhagic stroke, all-cause mortality, and bleeding), duration of warfarin use and the time spent in therapeutic range, duration of time spent on dialysis, diagnosis or definition of atrial fibrillation, use of concomitant medications (eg, aspirin and clopidogrel), neuroimaging mentioned as part of the stroke event ascertainment process, and adjusted covariates included in the models of analysis. Two investigators (ML and KSH) independently search the database and extracted data from eligible studies. Discrepancies were resolved by discussion with a third investigator (BO) and by referencing the original report.
Quality of Studies
Quality of studies was assessed with the following aspects: prospective design, maintenance of comparable groups, adjustment of CHADS2 scores or each CHADS2 component (congestive heart failure, hypertension, age, diabetes mellitus, and stroke), total stroke reported (not ischemic or fatal stroke only), and generalizability to other populations. Studies were graded as high quality if they met at least 3 of 5 criteria and low quality if they met fewer than 3.
Outcome Measures
The primary outcome was the association of warfarin therapy and risks of future stroke. Since some studies reported total stroke (ischemic plus hemorrhagic) while others only reported ischemic stroke as endpoints, the analyses were conducted with stratification of the studies by endpoints (any stroke vs ischemic stroke or thromboembolism). We did not pool endpoints of ischemic stroke and total stroke together since hemorrhagic stroke is a major concern in warfarin use among atrial fibrillation patients undergoing hemodialysis. The secondary endpoints were the association of warfarin therapy and risks of hemorrhagic stroke, death, and bleeding.
Data Synthesis
We combined log RR and standard errors using the inverse variance approach. We used a random effect model for primary analysis and a fixed effect model was also used for comparison. Heterogeneity was assessed by P-value of χ2 statistics and I2.14,15 We regarded heterogeneity as high when I2 more than 75%.16 We performed a sensitivity analysis by removing each study from the meta-analysis 1 at a time. Publication bias was estimated by funnel plots.17 Reported P values were two sided, with significance set at less than 0.05. We used RevMan 5.3 for this meta-analysis.
RESULTS
Literature Search
A total of 2174 reports were initially screened in title and abstract level, of which 39 were retrieved in full text for the detailed assessment. Among the 39 articles, 27 were excluded for not having appropriate RR and 95% CI for stroke or death among atrial fibrillation patients undergoing hemodialysis, 12 for not using warfarin. Finally 8 cohort studies fulfilled our prespecified inclusion criteria to be considered in our analysis (Figure 1).18–25
FIGURE 1.
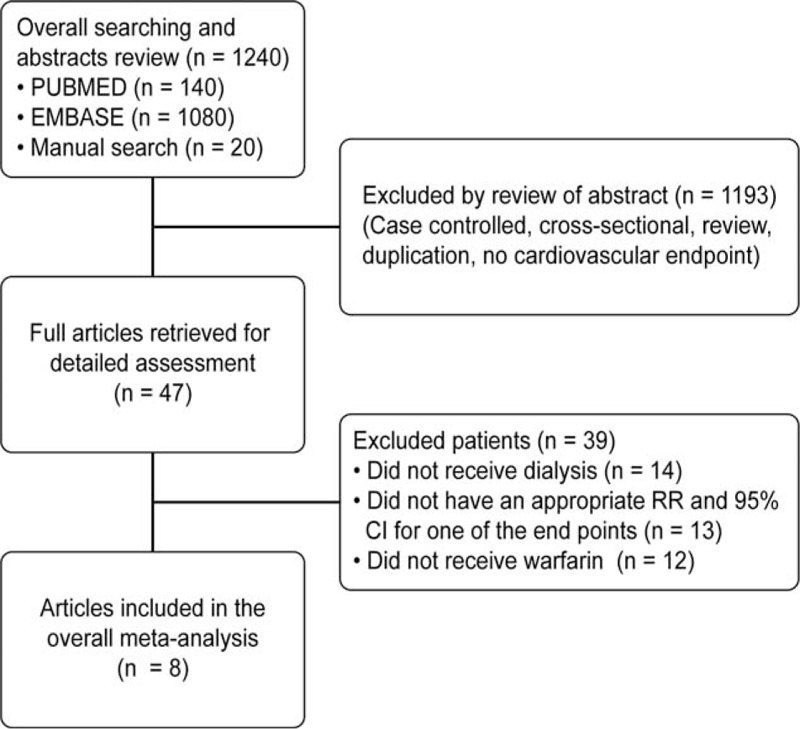
Flow of study selection.
Study Characteristics
Characteristics of the 8 included studies are shown in Table 1 and Supplemental Table 1. The total number of participants included in this meta-analysis was 9539 atrial fibrillation patients undergoing hemodialysis with 706 stroke events. The studies varied with regard to a stroke endpoint. Three studies reported total stroke endpoint,18,22,23 3 studies reported ischemic stroke endpoint,18,22,25 2 studies reported ischemic stroke or thromboembolism (eg, International Classification of Diseases 10th Revision: G458-G459, I63-I64, I74) endpoints,19,20 1 reported ischemic stroke and transient ischemic attack,24 and 1 study reported ischemic stroke, transient ischemic attack, and retinal infarct endpoints.21
TABLE 1.
Characteristics of Included Studies
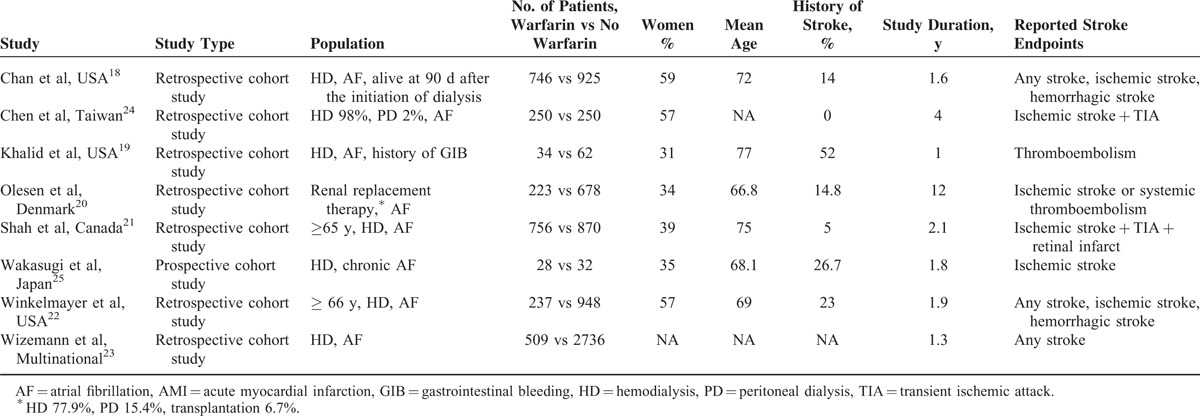
Among 8 included studies, 7 studies were retrospective studies18–24 and 1 study was a prospective cohort study.25 Six studies enrolled only patients receiving hemodialysis,18,19,21–23,25 while 2 included patients receiving peritoneal dialysis (15.4%20 and 2%,24 respectively) and 1 included patients receiving kidney transplantation (6.7%).20 Overall, 9233 (96.8%) patients received only hemodialysis, 214 (2.2%) received peritoneal dialysis, and 92 (1.0%) received renal transplantation.
Six studies were conducted in North America and Europe,18–23 1 study was conducted in Taiwan,24 and 1 study was conducted in Japan.25 The mean age ranged from 66.8 years20 to 77 years.19 The history of stroke at baseline ranged from 0%24 to 52%.19 The median follow-up duration was 1.8 years (ranging from 1 year19 to 12 years).20 On a scale of 5, the overall quality of studies was good (median score 3, range 2–4). The quality of each study with the result for each of the criteria of the quality score as well as the summary score was reported in Supplemental Table 2.
Main Outcome
Pooling the results from the random-effects model showed that warfarin use was associated with higher risk of any stroke among atrial fibrillation patients undergoing hemodialysis (3 studies, RR 1.50, 95% CI: 1.13–1.99, P = 0.01) (Figure 2). There was no obvious heterogeneity among studies with an I2 = 59% (P = 0.05). The estimates were similar between the fixed-effects model (RR 1.46, 95% CI: 1.23–1.74, P < 0.001) and random-effects model. Warfarin use had a neutral effect upon ischemic stroke or thromboembolism among patients with atrial fibrillation patients undergoing hemodialysis (7 studies, RR 1.01, 95% CI: 0.65–1.57, P = 0.9) (Figure 2). There was obvious heterogeneity among studies with an I2 = 90% (P < 0.001). The estimates were similar between the fixed-effects model (RR 0.95, 95% CI: 0.83–1.09, P = 0.46) and random-effects model. The exclusion of any single study from the analysis did not alter the overall finding in a sensitivity test. There was no substantial asymmetrical appearance on the funnel plot (Supplemental Figure 1).
FIGURE 2.
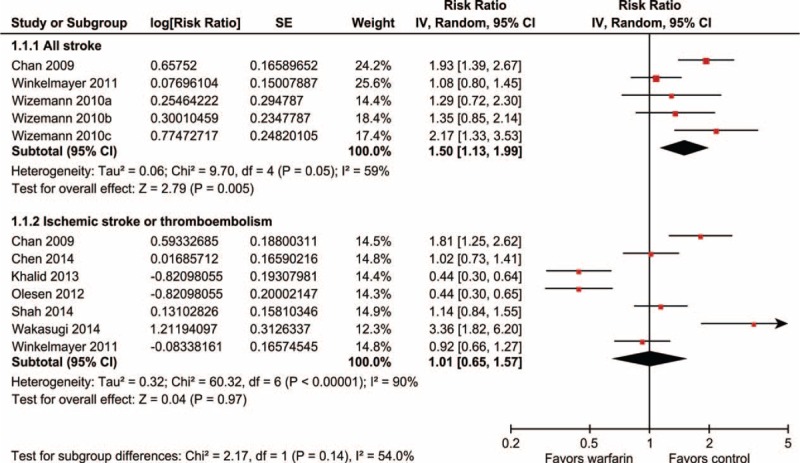
Risk ratio for association of warfarin use and risk of stroke and ischemic stroke in atrial fibrillation patients undergoing hemodialysis. (A) ≤65 years, (B) 66 to 75 years, (C) >75 years.
For additional end points, warfarin use was associated with a higher risk of hemorrhagic stroke and bleeding and was associated with neutral effects on death (Figure 3).
FIGURE 3.
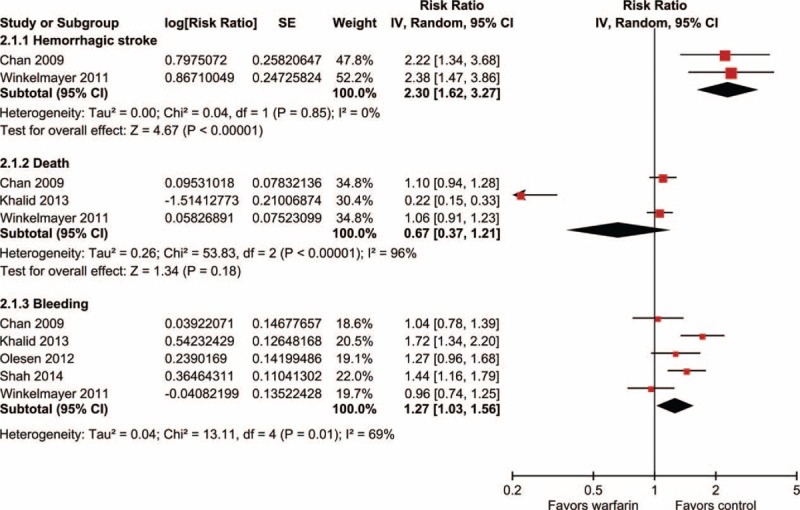
Risk ratio for association of warfarin use and risk of hemorrhagic stroke, death, and bleeding in atrial fibrillation patients undergoing hemodialysis.
DISCUSSION
In this meta-analysis of 8 cohort studies of generally good quality, among almost 10,000 people with atrial fibrillation undergoing hemodialysis, we found that patients who received warfarin had a risk of future stroke that was 50% greater than those who did not receive warfarin. Warfarin use had a neutral effect on ischemic stroke risk, but was associated with an increased risk of hemorrhagic stroke and bleeding among these patients. Our findings may be of clinical importance since warfarin is broadly used to prevent future stroke in patients with atrial fibrillation, but these analyses suggest that in the subset of atrial fibrillation patients undergoing hemodialysis, warfarin use may not be as effective in preventing ischemic stroke and may even be associated with a rise in combined ischemic and hemorrhagic stroke. Still, the association between warfarin use and increased stroke risk in atrial fibrillation patients undergoing hemodialysis does not necessarily imply causality given the observational nature of the included studies.
Potential reasons for the absence of an effect of warfarin in reducing ischemic stroke risk are several. An important first consideration is that this finding may be due to confounding by indication. Most studies were retrospective in design, and so we really do not know enough about the cases enrolled, and those who were on warfarin already. The treating physicians are clearly aware of the increased bleeding risks of hemodialysis, so there is likely a reason for continued warfarin use in some of these cases based on perceived risks. Although all studies included in our meta-analysis reported a multivariate adjusted relative risk, which minimizes the influence of known confounding on our results, residual confounding from measured and unmeasured variables remains possible.
Additional potential causes include that, while warfarin is likely to reduce cardiac emboli among atrial fibrillation patients, regardless of kidney function, the attributable risk of atrial fibrillation to ischemic stroke among hemodialysis patients might not be as high as for the general population.3,6 Also, warfarin use in hemodialysis patients can inhibit Matrix Gla protein and Gas-6, accelerating vascular calcification, and thereby increasing risk for ischemic stroke.26,27
Risk-benefit assessment with respect to warfarin use for stroke prevention in patients with atrial fibrillation is crucially dependent on the magnitude of stroke risk, as well as the effectiveness and safety of warfarin use.28 With respect to the effectiveness and safety of warfarin use, the risk of elevated hemorrhagic stroke in hemodialysis patients needs be taken into consideration.29 In addition to various platelet and coagulation abnormalities, hemodialysis patients routinely receive heparin during dialysis procedures, which also increases the risk for bleeding.12 Furthermore, over-anticoagulation (international normalized ratio >4) is more frequently encountered among patients with severe chronic kidney disease taking warfarin, as compared with patients without chronic kidney disease.30 All of the aforementioned factors probably contributed to the greater risk of hemorrhagic stroke and overall bleeding seen among atrial fibrillation patients on hemodialysis receiving warfarin therapy.
There are limitations to this meta-analysis. First, most included studies were retrospective cohort studies and the precise reasons for using or not using warfarin are not well known. Furthermore, the history of stroke at baseline ranged from 0% to 52% which means it was a combination of primary and secondary prevention. This is a critical aspect to understand the potential confounding by indication, which is hard to control for using the available study methods. Individual-level pooled analyses of relevant studies are warranted and may provide additional insights. Second, only 3 studies provided a total stroke endpoint and there was moderate heterogeneity with I2 = 59%. Meta-regression analysis with baseline variables might be helpful to examine the reason for the heterogeneity. However, each study provided different items of baseline variables, which prevented us from exploring further. Third, substantial heterogeneity existed among studies with an ischemic stroke endpoint. Warfarin use seems to be beneficial in studies using ischemic stroke or systemic thromboembolism as an endpoint19,20 while associated with neutral effect in studies using ischemic stroke as an endpoint.21,22,24,25 One plausible explanation might be the benefit of warfarin use in reducing cardiac emboli could be amplified if the studies counts all the possible systemic thromboembolic events. Fourth, hemorrhagic stroke data were provided from only 2 studies and confidence interval was wide for hemorrhagic stroke outcome. Fifth, neuroimaging was explicitly mentioned as part of the stroke event ascertainment process in only 1 study.25 Finally, the included studies did not provide the information on the concomitant use of heparin, time since end stage renal disease, duration of warfarin use and the time spent in therapeutic range, and how warfarin was initiated in these patients since the period at risk for both ischemic and hemorrhagic events are the first 3 months of treatment.31
In conclusion, this meta-analysis of cohort studies showed that warfarin use may be associated with higher risk of future stroke among atrial fibrillation patients undergoing hemodialysis. Still, the results should be interpreted cautiously in the light of the several limitations as described above. Large randomized controlled trials are warranted to clarify this issue and to guide atrial fibrillation management guideline among hemodialysis patients.
Footnotes
Abbreviations: CI = confidence interval, RR = relative risk.
The authors have no conflicts of interest to disclose.
This work was supported by grants from Ministry of Science and Technology Taiwan (NSC 102-2628-B-182-012 and MOST103-2314-B-182-056). The sponsors played no role in the study design, data collection and analysis, or decision to submit the article for publication.
REFERENCES
- 1.Wang HH, Hung SY, Sung JM, et al. Risk of stroke in long-term dialysis patients compared with the general population. Am J Kidney Dis 2014; 63:604–611. [DOI] [PubMed] [Google Scholar]
- 2.Fuster V, Ryden LE, Cannom DS, et al. 2011 ACCF/AHA/HRS focused updates incorporated into the ACC/AHA/ESC 2006 Guidelines for the management of patients with atrial fibrillation: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines developed in partnership with the European Society of Cardiology and in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. J Am Coll Cardiol 2011; 57:e101–e198. [DOI] [PubMed] [Google Scholar]
- 3.Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke 1991; 22:983–988. [DOI] [PubMed] [Google Scholar]
- 4.Lip GY, Brechin CM, Lane DA. The global burden of atrial fibrillation and stroke: a systematic review of the epidemiology of atrial fibrillation in regions outside North America and Europe. Chest 2012; 142:1489–1498. [DOI] [PubMed] [Google Scholar]
- 5.Wetmore JB, Mahnken JD, Rigler SK, et al. The prevalence of and factors associated with chronic atrial fibrillation in Medicare/Medicaid-eligible dialysis patients. Kidney Int 2012; 81:469–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Toyoda K, Fujii K, Fujimi S, et al. Stroke in patients on maintenance hemodialysis: a 22-year single-center study. Am J Kidney Dis 2005; 45:1058–1066. [DOI] [PubMed] [Google Scholar]
- 7.Vazquez E, Sanchez-Perales C, Garcia-Garcia F, et al. Atrial fibrillation in incident dialysis patients. Kidney Int 2009; 76:324–330. [DOI] [PubMed] [Google Scholar]
- 8.Alberts MJ, Eikelboom JW, Hankey GJ. Antithrombotic therapy for stroke prevention in non-valvular atrial fibrillation. Lancet Neurol 2012; 11:1066–1081. [DOI] [PubMed] [Google Scholar]
- 9.January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: Executive Summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol 2014; 64:2246–2280. [DOI] [PubMed] [Google Scholar]
- 10.Sreedhara R, Itagaki I, Lynn B, et al. Defective platelet aggregation in uremia is transiently worsened by hemodialysis. Am J Kidney Dis 1995; 25:555–563. [DOI] [PubMed] [Google Scholar]
- 11.Boccardo P, Remuzzi G, Galbusera M. Platelet dysfunction in renal failure. Semin Thromb Hemost 2004; 30:579–589. [DOI] [PubMed] [Google Scholar]
- 12.Marinigh R, Lane DA, Lip GY. Severe renal impairment and stroke prevention in atrial fibrillation: implications for thromboprophylaxis and bleeding risk. J Am Coll Cardiol 2011; 57:1339–1348. [DOI] [PubMed] [Google Scholar]
- 13.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 2000; 283:2008–2012. [DOI] [PubMed] [Google Scholar]
- 14.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002; 21:1539–1558. [DOI] [PubMed] [Google Scholar]
- 15.Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ 2003; 327:557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions. West Sussex: Cochrane Collaboration and John Wiley & Sons Ltd; 2008. [Google Scholar]
- 17.Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997; 315:629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chan KE, Lazarus JM, Thadhani R, et al. Warfarin use associates with increased risk for stroke in hemodialysis patients with atrial fibrillation. J Am Soc Nephrol 2009; 20:2223–2233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Khalid F, Qureshi W, Qureshi S, et al. Impact of restarting warfarin therapy in renal disease anticoagulated patients with gastrointestinal hemorrhage. Ren Fail 2013; 35:1228–1235. [DOI] [PubMed] [Google Scholar]
- 20.Olesen JB, Lip GY, Kamper AL, et al. Stroke and bleeding in atrial fibrillation with chronic kidney disease. N Engl J Med 2012; 367:625–635. [DOI] [PubMed] [Google Scholar]
- 21.Shah M, Avgil Tsadok M, Jackevicius CA, et al. Warfarin use and the risk for stroke and bleeding in patients with atrial fibrillation undergoing dialysis. Circulation 2014; 129:1196–1203. [DOI] [PubMed] [Google Scholar]
- 22.Winkelmayer WC, Liu J, Setoguchi S, et al. Effectiveness and safety of warfarin initiation in older hemodialysis patients with incident atrial fibrillation. Clin J Am Soc Nephrol 2011; 6:2662–2668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wizemann V, Tong L, Satayathum S, et al. Atrial fibrillation in hemodialysis patients: clinical features and associations with anticoagulant therapy. Kidney Int 2010; 77:1098–1106. [DOI] [PubMed] [Google Scholar]
- 24.Chen JJ, Lin LY, Yang YH, et al. Anti-platelet or anti-coagulant agent for the prevention of ischemic stroke in patients with end-stage renal disease and atrial fibrillation—a nation-wide database analyses. Int J Cardiol 2014; 177:1008–1011. [DOI] [PubMed] [Google Scholar]
- 25.Wakasugi M, Kazama JJ, Tokumoto A, et al. Association between warfarin use and incidence of ischemic stroke in Japanese hemodialysis patients with chronic sustained atrial fibrillation: a prospective cohort study. Clin Exp Nephrol 2014; 18:662–669. [DOI] [PubMed] [Google Scholar]
- 26.Clase CM, Holden RM, Sood MM, et al. Should patients with advanced chronic kidney disease and atrial fibrillation receive chronic anticoagulation? Nephrol Dial Transplant 2012; 27:3719–3724. [DOI] [PubMed] [Google Scholar]
- 27.Reynolds JL, Joannides AJ, Skepper JN, et al. Human vascular smooth muscle cells undergo vesicle-mediated calcification in response to changes in extracellular calcium and phosphate concentrations: a potential mechanism for accelerated vascular calcification in ESRD. J Am Soc Nephrol 2004; 15:2857–2867. [DOI] [PubMed] [Google Scholar]
- 28.Gage BF, van Walraven C, Pearce L, et al. Selecting patients with atrial fibrillation for anticoagulation: stroke risk stratification in patients taking aspirin. Circulation 2004; 110:2287–2292. [DOI] [PubMed] [Google Scholar]
- 29.Seliger SL, Gillen DL, Longstreth WT, Jr, et al. Elevated risk of stroke among patients with end-stage renal disease. Kidney Int 2003; 64:603–609. [DOI] [PubMed] [Google Scholar]
- 30.Limdi NA, Beasley TM, Baird MF, et al. Kidney function influences warfarin responsiveness and hemorrhagic complications. J Am Soc Nephrol 2009; 20:912–921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wetmore JB, Phadnis MA, Ellerbeck EF, et al. Relationship between Stroke and Mortality in Dialysis Patients. Clin J Am Soc Nephrol 2015; 10:80–89. [DOI] [PMC free article] [PubMed] [Google Scholar]


