Abstract
Myocardial reinfarction is frequent after ST-elevation myocardial infarction (STEMI). The incidence of previous stroke in STEMI patients is also high. We aim to evaluate the risk factors for short-term myocardial reinfarction in STEMI patients in a multicenter study.
STEMI patients with chest pain onset within 12 hours in 247 hospitals in China were enrolled. Seven and 30-day follow-ups from admission to hospitals were performed. The primary outcome of our study was myocardial reinfarction at 30 days after STEMI. The study population was stratified into 2 groups: STEMI patients with mayocardial reinfarction and without mayocardial reinfarction. Survival curve was constructed using Kaplan–Meier survival methods with log-rank statistics. Multivariable Cox regression model was performed to determine the risk factors for myocardial reinfarction events in STEMI patients.
A total of 6876 STEMI patients were enrolled. The proportion of STEMI patients with previous stroke was 9.4%. Rate of 30-day myocardial reinfarction was 2.0% among all STEMI patients. Rate of 30-day myocardial reinfarction was 4.2% in STEMI patients with previous stroke which was statistically higher than that in STEMI patients without previous stroke (P < 0.001). Multivariable Cox regression analysis showed that previous stroke (HR, 3.673; 95% CI, 1.180–11.43) and statin use (HR, 0.230; 95% CI, 0.080–0.664) were independent predictors for 30-day myocardial reinfarction.
A large proportion of STEMI patients had previous stroke history. Short-term myocardial reinfarction after STEMI is not infrequent. STEMI patients with previous stroke confronted higher rates of short-term myocardial reinfarction and statin could decline the risk of short-term myocardial reinfarction.
INTRODUCTION
Change of people's lifestyle confers higher morbidity and mortality in cardiovascular athrosclerosis. Short-term Major Adverse Cardiovascular Events (MACE) rate of STEMI has declined with a greater use of primary percutaneous coronary interventions (PCI) and auxiliary antiplatelet and anticoagulant drugs.1 Myocardial reinfarction and the incident adverse events are the main components of short-term MACE. Identify the risk factors for myocardial reinfarction and appropriate intervention may further decline MACE rates of STEMI.
Several studies have evaluated the incidence, determinants, and clinical course of reinfarction of acute myocardial infarction. Donges et al2 found that in the era of thrombolysis therapy for acute myocardial infarction (AMI), previous AMI, age >70 years, diagnostic first electrocardiogram, and female sex are independent determinants for in-hospital reinfarction. White et al3 enrolled AMI patients within days 3 to 28 (>24 hours) from symptom onset and concluded that history of PCI before study entry, diabetes, and absence of new Q waves were independent predictors for 9-year myocardial reinfarction. However, it has been demonstrated that most of deaths after STEMI occurred within the first 30 days.4 Myocardial reinfarction was a powerful independent predictor of subsequent cardiac mortality.5 So far, limited evidence is available for evaluating the independent predictors for short-term myocardial reinfarction in STEMI patients in a multicenter and real-world study.
To solve the above question, we make a post hoc analysis of a prospective multicenter study which enrolled STEMI patients within 12 hours from chest pain onset in 247 hospitals in China. We aim to evaluate the independent predictors for short-term myocardial reinfarction in STEMI patients.
METHODS
Study Patients
A series of patients with STEMI admitted to 247 hospitals in China were enrolled in our study from June 2001 to July 2004. Each patient complained of angina pectoris within 12 hours from the symptom onset. The angina pectoris generally lasted more than 30 minutes. Electrocardiograms were performed for all patients and showed ST-segment elevation of >1 mm in contiguous leads. The diagnosis of STEMI abided by the Universal definition of myocardial infarction.6 STEMI patients who have previous myocardial infarction were excluded. All patients obtained written informed consents before enrollment. The study protocol was approved by the Ethics Committee of Beijing Fuwai Hospital.
Reperfusion Therapy
All hospitals adopted the uniform reperfusion strategy. If without contraindications, fibrinolytic therapy should be applied to these STEMI patients who were admitted to hospitals within 12 hours from the symptom onset and whose ECG showed ST elevation more than 0.1 mV in at least 2 contiguous precordial leads or at least 2 adjacent limb leads or new onset Left Bundle Branch Block in hospitals without intervention qualification or possible delayed reperfusion. Fibrinolytic agents used in our study included Streptokinase, Urokinase, and Alteplase. In hospitals that have the qualification for coronary intervention, primary PCI could be considered. Primary PCI was preferred on the following conditions: the duration from angina onset is within 12 hours; STEMI patients with severe heart failure, cardiac shock, and/or pulmonary edema regardless of the angina duration; STEMI patients with contraindication to fibrinolytic therapy. The index of reperfusion success includes 50% relief of angina pectoris, ahead of time of the peak cardiac troponin I level, occurrence of reperfusion arrhymia and a reduction of at least 50% of the initial ST-segment elevation leads on ECG 60 to 180 minutes after initiation of reperfusion therapy. The ancillary antiplatelet and anticoagulant therapy were also standardized. The ancillary antiplatelet drugs included Aspirin, Clopidogrel, and Ticlopidine.
Outcomes and Definitions
The primary endpoints events of the study were rate of 30-day myocardial reinfarction after AMI. Previous stroke was defined as sudden, nonconvulsive loss of neurological function due to brain ischemia or intracranial hemorrhages confirmed by computed tomography or magnetic resonance imaging. Myocardial reinfarction was defined as at least meeting 2 of the following criteria: new onset of angina pectoris during mild exercise or rest lasting more than 20 minutes or needing nitroglycerin; concentration of myocardial enzyme rising to above the 99th percentile upper reference limit or rising to greater than 50% of the lowest myocardial enzyme level during recovery of AMI, if enzymes have already been elevated; new or presumed new significant ST-segment–T-wave changes resulting from myocardial ischemia.
Clinical Follow-Up
In addition to the 7-day follow-up that was performed during the patient's hospitalization, a follow-up at 30 days from angina onset was also performed. Myocardial reinfarction events were recorded in detail.
Data Collection
Baseline clinical characteristics of all enrolled patients which include demographic data, previous disease histories, vital signs and laboratory tests on admission, and in-hospital management were well recorded. Thirty-day myocardial reinfarction events after acute AMI were collected in detail at the follow-up.
Statistical Analysis
Continuous variables were expressed as mean (±SD). Categorical variables were expressed as numbers and proportion. According to whether or not experiencing myocardial reinfarction, the study population was divided into 2 groups. Baseline characteristics of both groups were compared using the Pearson χ2 statistics for categorical variables and univariate ANOVA or Kruskal–Wallis test for continuous variables. According to previous stroke category, myocardial reinfarction events were compared with the Pearson χ2 statistics. Survival curve of myocardial reinfarction events by previous stroke category was constructed using Kaplan–Meier survival methods with log-rank statistics. Multivariable Cox regression model was performed to determine whether there was association between previous stroke and myocardial reinfarction events in patients after STEMI. Other covariates added into the Cox regression model included age, sex, ST segment elevation lead, heart rate, systolic blood pressure, Killip class, previous hypertension, previous stroke, previous diabetes mellitus, admission glucose, admission hemoglobin, in-hospital medications (aspirin, beta-blockers, angiotensin converting enzyme inhibitors (ACEI) and statins), target vascular, post percutaneous transluminal coronary angioplasty (PTCA) ADP-antagonists, reperfusion therapy (thrombolysis and PTCA). Variables with a P value <0.05 were entered by a forward stepwise manner, with retention set at a significance level of 0.10. All statistical analyses were performed using SPSS22.0. Statistical significance was indicated at a 2-side P value less than 0.05.
RESULTS
A total of 7468 STEMI patients were enrolled of whom 592 patients with previous myocardial infarction history were excluded. Finally, 6876 STEMI patients were included in our study for statistic analysis to evaluate the relationship between previous stroke and myocaidial reinfarction, among which 644 (9.4%) STEMI patients had previous stroke history, meanwhile 6232 (90.6%) STEMI patients had not.
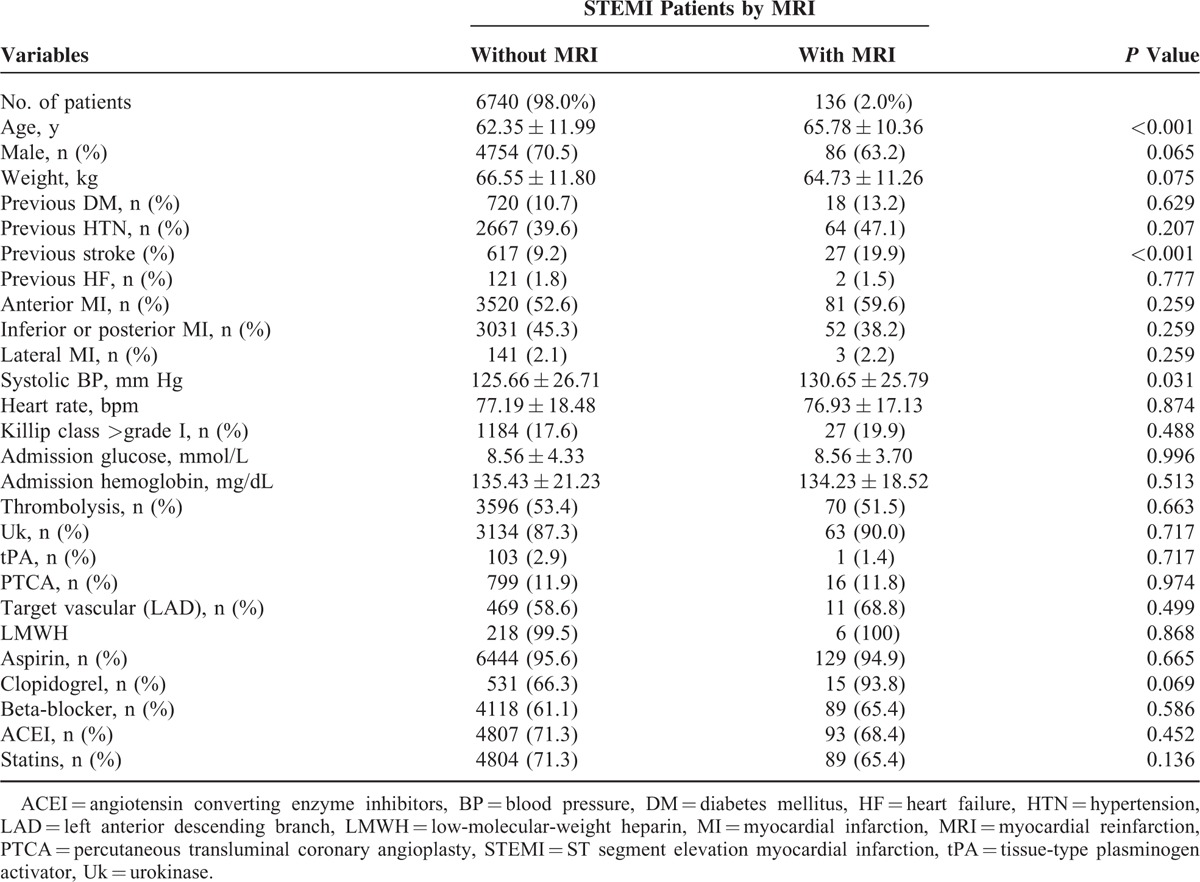
Table 1 lists clinical characteristics and in-hospital management of STEMI patients according to mayocardial reinfarction. STEMI patients with mayocardial reinfarction were often older and had high rates of previous stroke. Other variables between 2 groups did not differentiate significantly from each other. We have to state that the rates of thrombolysis therapy and primary PTCA in both groups were not relatively high.
TABLE 1.
Clinical Characteristics and In-Hospital Management of STEMI Patients
The 30-day follow-up was performed. Rate of 30-day myocardial reinfarction was 2.0% among all STEMI patients. Figure 1 shows rates of 30-day myocardial reinfarction according to previous stroke category. We could see from the figure that rate of 30-day myocardial reinfarction was 4.2% in STEMI patients with previous stroke which was statistically higher than that in STEMI patients without previous stroke (P < 0.001).
FIGURE 1.
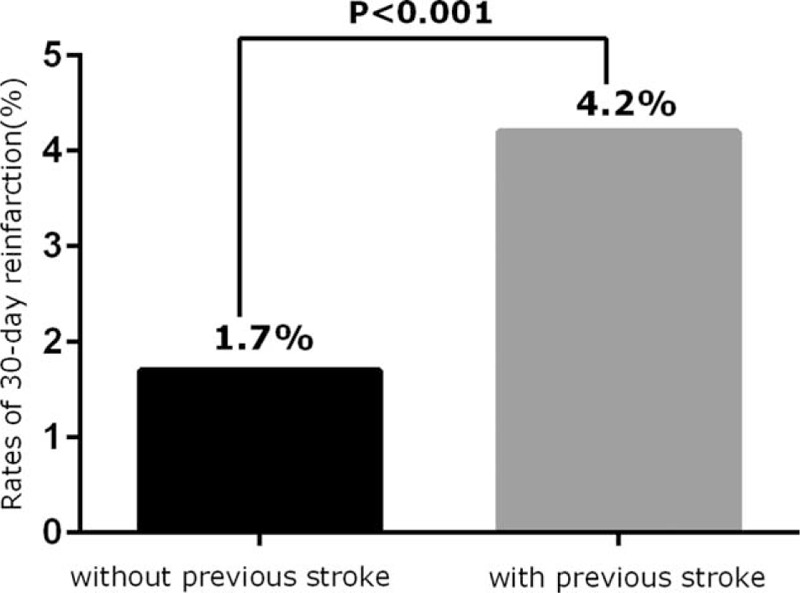
Rates of 30-day myocardial reinfarction according to previous stroke category.
Figure 2 shows Kaplan–Meier curves for 30-day myocardial reinfarction by previous stroke category. Log-rank statistics indicated freedom from myocardial reinfarction survival curves of STEMI patients with previous stroke was significantly lower than that of STEMI patients without previous stroke (log rank, P < 0.001).
FIGURE 2.
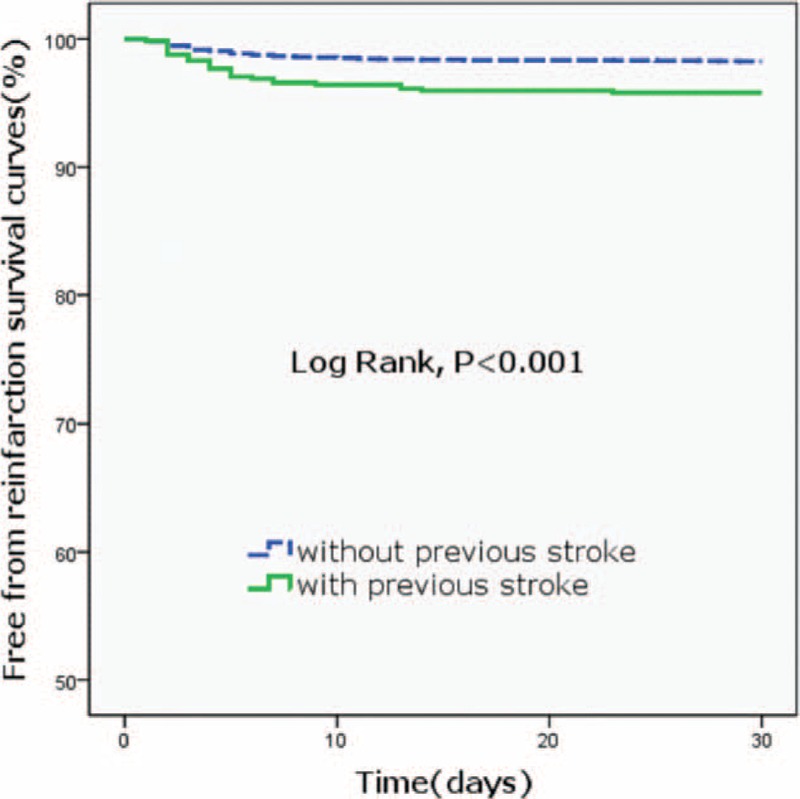
Kaplan–Meier curves for 30-day myocardial reinfarction by previous stroke category.
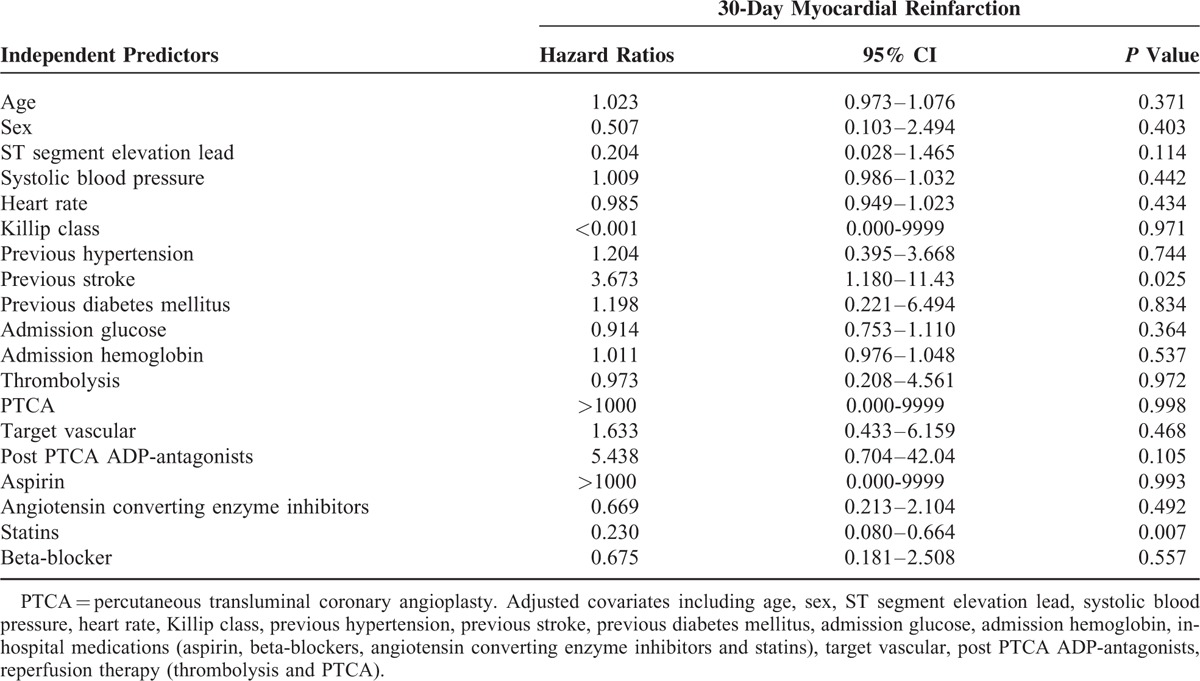
Table 2 shows hazards ratios for 30-day myocardial reinfarction by Cox regression analysis. Adjusted covariates included age, sex, ST segment elevation lead, heart rate, systolic blood pressure, Killip class, previous hypertension, previous stroke, previous DM, admission glucose, admission hemoglobin, in-hospital medications (aspirin, beta-blockers, ACEI, and statins), target vascular, post-PTCA ADP-antagonists, reperfusion therapy (thrombolysis and PTCA). After adjusting the confounding factors, multivariable Cox regression analysis showed that previous stroke (HR, 3.673; 95% CI, 1.180–11.43) and statin use (HR, 0.230; 95% CI, 0.080–0.664) were independent predictors for 30-day myocardial reinfarction. However, thrombolysis therapy, PTCA, target vascular, Clopidogrel and beta-blocker use did not correlate with short-term myocardial reinfarction.
TABLE 2.
Hazards Ratios for 30-Day Myocardial Reinfarction by Cox Regression Analysis
DISCUSSION
First 30 days after acute STEMI is the critical period because of higher rate of MACE. The present study showed that myocardial reinfarction after STEMI is not infrequent, besides STEMI patients with previous stroke confronted higher rates of short-term myocardial reinfarction and statin use could decline the risk of short-term myocardial reinfarction.
Several studies evaluated the incidence of myocardial reinfarction in AMI patients. In thrombolysis era for AMI, Donges et al2 found that the incidence of in-hospital repeat acute myocardial infarction was 4.7%. In 2009, Fokkema et al7 indicated reinfarction was observed in 3.4% STEMI patients within 1 year after primary PCI. In our study, although not all STEMI patients were managed with reperfusion therapy and the contemporary triple antiplatelet therapy, the rate of 30-day myocardial reinfarction among all STEMI patients was 2.0%. Similarly to our study, in 2014, in the contemporary era, Stone et al5 assessed 3202 STEMI patients and indicated the cumulative incidence of reinfarction was 1.8% at 30 days. Compared with the above study, although our study performed in thrombolysis era for AMI, the results were credible. Given our multicenter design, it may reflect situation of STEMI treatment in real world.
In the contemporary era, Stone et al5 indicated that current smoking, Killip class >=2, baseline thrombocytosis, multivessel disease, symptom onset-to-balloon time, and total stent length were independent predictors of reinfarction. Many STEMI patients had the previous stroke history. Abtahian et al8 found the incidence of previous stroke was 5.1% in patients with STEMI and those with previous stroke were less likely to receive evidence-based therapies. In our study, we found that previous stroke was independent predictor of short-term myocardial reinfarction in STEMI patients. Similarly to our study, Kornowski et al9 concluded prior stroke was a predictor of recurrent myocardial infarction for men. Some explanations can interpret this phenomenon: on the one hand, STEMI patients with previous stroke, despite hemorrhagic or ischemic stroke, have widely existed atherosclerosis in the whole artery tree including coronary artery. On the other hand, when meeting STEMI patients with previous stroke who need reperfusion therapy, clinicians were confronted with too many worries. However, our result should be further verified in the contemporary era for STEMI. At last, for STEMI patients with previous stroke primary PCI was the preferred reperfusion therapy.
Statin agents have been established as standard therapy for acute coronary syndrome (ACS) patients. The beneficial effects attribute to the pleiotropic actions of statin agents, of which low-density lipoprotein cholesterol (LDL-C) lowering effects are the most important.10 But for ACS patients with low LDL-C level, statin therapy can benefit similarly. Kanadasi et al11 found for ACS patients with a low LDL level, atorvastatin can lower the hsCRP and plasma amyloid A values on the 5th day and in the 6th month. Accordingly, Tsai et al12 included statin therapy can significantly lower the incidence of death, reinfarction, or stroke at 6 months. Beyond LDL-C lowering effects such as anti-inflammation, protection of endothelial cells, reduction of platelet activation and reactivity13 and stabilization of atheroscerosis plaque can interpret the above beneficial effect. Bybee et al14 indicated that early statin treatment significantly decreases the risk of in-hospital mortality and in-hospital reinfarction in acute myocardial infarction. In our study, statin therapy was an independent predictor for 30-day myocardial reinfarction in STEMI patients. Leone et al15 concluded an intensive statin treatment after primary or rescue PCI can increase the endothelial progenitor cells count at follow-up. Zhao et al16 indentified pretreatment with statins could attenuate no-reflow after AMI in patients with acute hyperglycemia. So statin is the key drug to decrease the risk of myocardial reinfarction.
The main strength of our study lies in its design as a multicenter registry and relatively larger study population of patients with STEMI. And we for the first time found the correlation of previous stroke and myocardial reinfarction. However, limitation still existed. The study was retrospective and conducted 1 decade ago in the era of thrombolysis therapy for AMI.
In conclusion, STEMI patients with previous stroke confronted higher rates of short-term myocardial reinfarction. Statin could decline the risk of short-term myocardial reinfarction. Primary PCI was the preferred reperfusion therapy for these STEMI patients.
Acknowledgment
The authors wish to thank the study participants for their consent and time and the staff of the participating hospitals for their dedication and careful efforts to provide data for this multicenter study. The authors are also grateful to the administrators of the patient record database for their conscientious work.
Footnotes
Abbreviations: ACEI = angiotensin converting enzyme inhibitors, ACS = acute coronary syndrome, AMI = acute myocardial infarction, LDL-C = low-density lipoprotein cholesterol, MACE = Major Adverse Cardiovascular Events, PCI = percutaneous coronary intervention, PTCA = percutaneous transluminal coronary angioplasty, STEMI = ST-elevation myocardial infarction.
The authors have no funding and conflicts of interest to disclose.
REFERENCES
- 1.De Servi S, Mariani G, Mariani M, et al. How to reduce mortality in ST-elevation myocardial infarction patients treated with primary percutaneous coronary interventions: cut the bleeding. Curr Med Res Opin 2013; 29:189–194. [DOI] [PubMed] [Google Scholar]
- 2.Donges K, Schiele R, Gitt A, et al. Incidence, determinants, and clinical course of reinfarction in-hospital after index acute myocardial infarction (results from the pooled data of the maximal individual therapy in acute myocardial infarction [MITRA], and the myocardial infarction registry [MIR]). Am J Cardiol 2001; 87:1039–1044. [DOI] [PubMed] [Google Scholar]
- 3.White HD, Reynolds HR, Carvalho AC, et al. Reinfarction after percutaneous coronary intervention or medical management using the universal definition in patients with total occlusion after myocardial infarction: results from long-term follow-up of the Occluded Artery Trial (OAT) cohort. Am Heart J 2012; 163:563–571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kadri Z, Danchin N, Vaur L, et al. Major impact of admission glycaemia on 30 day and one year mortality in non-diabetic patients admitted for myocardial infarction: results from the nationwide French USIC 2000 study. Heart 2006; 92:910–915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stone SG, Serrao GW, Mehran R, et al. Incidence, predictors, and implications of reinfarction after primary percutaneous coronary intervention in ST-segment-elevation myocardial infarction: the Harmonizing Outcomes with Revascularization and Stents in Acute Myocardial Infarction Trial. Circ Cardiovasc Interv 2014; 7:543–551. [DOI] [PubMed] [Google Scholar]
- 6.Myocardial infarction redefined: a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. Eur Heart J 2000; 21:1502–1513. [DOI] [PubMed] [Google Scholar]
- 7.Fokkema ML, van der Vleuten PA, Vlaar PJ, et al. Incidence, predictors, and outcome of reinfarction and stent thrombosis within one year after primary percutaneous coronary intervention for ST-elevation myocardial infarction. Catheter Cardiovasc Interv 2009; 73:627–634. [DOI] [PubMed] [Google Scholar]
- 8.Abtahian F, Olenchock B, Ou FS, et al. Effect of prior stroke on the use of evidence-based therapies and in-hospital outcomes in patients with myocardial infarction (from the NCDR ACTION GWTG registry). Am J Cardiol 2011; 107:1441–1446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kornowski R, Goldbourt U, Boyko V, et al. Clinical predictors of reinfarction among men and women after a first myocardial infarction. SPRINT Study Group. Secondary Prevention Reinfarction Israeli Nifedipine Trial. Cardiology 1995; 86:163–168. [DOI] [PubMed] [Google Scholar]
- 10.Gencer B, Auer R, Nanchen D, et al. Expected impact of applying new 2013 AHA/ACC cholesterol guidelines criteria on the recommended lipid target achievement after acute coronary syndromes. Atherosclerosis 2015; 239:118–124. [DOI] [PubMed] [Google Scholar]
- 11.Kanadasi M, Cayli M, Demirtas M, et al. The effect of early statin treatment on inflammation and cardiac events in acute coronary syndrome patients with low-density lipoprotein cholesterol. Heart Vessels 2006; 21:291–297. [DOI] [PubMed] [Google Scholar]
- 12.Tsai TT, Nallamothu BK, Mukherjee D, et al. Effect of statin use in patients with acute coronary syndromes and a serum low-density lipoprotein <or=80 mg/dl. Am J Cardiol 2005; 96:1491–1493. [DOI] [PubMed] [Google Scholar]
- 13.Pawelczyk M, Chmielewski H, Kaczorowska B, et al. The influence of statin therapy on platelet activity markers in hyperlipidemic patients after ischemic stroke. Arch Med Sci 2015; 11:115–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bybee KA, Wright RS, Williams BA, et al. Effect of concomitant or very early statin administration on in-hospital mortality and reinfarction in patients with acute myocardial infarction. Am J Cardiol 2001; 87:771–774. [DOI] [PubMed] [Google Scholar]
- 15.Leone AM, Rutella S, Giannico MB, et al. Effect of intensive vs standard statin therapy on endothelial progenitor cells and left ventricular function in patients with acute myocardial infarction: statins for regeneration after acute myocardial infarction and PCI (STRAP) trial. Int J Cardiol 2008; 130:457–462. [DOI] [PubMed] [Google Scholar]
- 16.Zhao JL, Yang YJ, Pei WD, et al. The effect of statins on the no-reflow phenomenon: an observational study in patients with hyperglycemia before primary angioplasty. Am J Cardiovasc Drugs 2009; 9:81–89. [DOI] [PubMed] [Google Scholar]


