Abstract
Incidence of hepatocellular carcinoma (HCC) ranked the fifth in male and ninth in the female counterparts, and 50% of incidence HCC cases were occurred in China with high hepatitis B virus (HBV) prevalence. HCC has seriously compromised the health status of general population in China. A case–control study of 314 HCC cases and 346 controls was conducted in Xiamen, which is an epidemic area in China for both hepatitis B infection and HCC. Face-to-face interview was conducted to gather information on demographic characteristics as well as exposure of environmental factors. Commercial enzyme-linked immunosorbent assay kits were used to determine the status of serological markers of HBV infection. Odds ratios and 95% confidence intervals were estimated by using unconditional logistic regression. Multivariate unconditional logistic regression analysis was applied to evaluate the potential interactions of variables or confounders.
As expected, HBV and alcohol intake still are the major risk factors of HCC. Liver disease history and passive smoking are also associated with elevated HCC risk. Indoor air pollution and pesticide exposure have newly identified as risk factors of HCC. Fruit and tea intake can significantly lower the HCC risk.
The application of HBV vaccine and reduction on alcohol intake should be further promoted in high-risk population. Fruit and tea can be served as chemoprevention in daily life due to their high accessibility.
INTRODUCTION
Primary liver cancer can be qualified as the one of the most common malignancy in the world, and ∼80% of primary liver cancer cases are hepatocellular carcinoma (HCC). It has high mortality and with a mortality incidence ratio of 0.95, due to its high mortality, HCC has seriously compromised the health status of general population. According to statistics released by the World Health Organization, ∼6% of cancer incidence and 9% of cancer mortality can be attributed to HCC in the global range. There were 746,000 deceased HCC cases in worldwide, and HCC was the second death cause of cancer. The incidence of HCC cancer among male population ranked the fifth and ninth in the female counterparts. In general, ∼75% of HCC incidence cases was diagnosed in developing countries, and ∼50% of HCC incidence and mortality were occurred in China.1 Geographic characteristics of HCC can be found based on the historical incidence and mortality data which indicated that HCC has highest prevalence in Asia, and followed with Africa, Europe, Oceania, and America has the lowest prevalence.
Chronic hepatitis B virus infection has been generally accepted as the major risk factor of HCC and the prevalence of HBV infection largely reflects the HCC occurrence.2 The statistics suggested that HBV infection accounts for 60% of liver cancer cases in less developed regions but only 23% in more developed regions,3 and the proportion attributed to the HBV infection among HCC cases in China reached 80% to 90%. Other than HBV infection, including HCV infection and exposure to aflatoxin B14 has also been associated with the development of HCC in parts of Africa and Asia.5 According to the latest data, the positive rate of HBsAg among Chinese general population was 7.2%;6 the HBsAg was greatly diminished among the population aged <15 years which was strongly associated with national vaccination program. However, Xiamen, a high prevalence area both for chronic hepatitis B virus and HCC, maintains an HBsAg positive rate of 13% which ∼2-fold higher than national average level based on the census data acquired in 2008. Back in the 1970s, 3 major retrospective investigations showed that the mortality of HCC was ranging from 37.54 to 44.74 per 100,000 in 1973 to 1987, which also 2-fold higher than national average mortality in the same period. Recently, Wu et al7 conducted an analysis on the mortality of HCC, and results indicated the annual average mortality of HCC from 2002 to 2011 was 32.7 per 100,000, which ranked as the top death cause among local residents. Identifying the risk factor of HCC among population in the epidemic area would definitely help to reduce the incidence and providing evidence for the making of prevention strategy. Therefore, we performed a case–control study to explore the association between environmental factors, HBV infection, and the risk of developing HCC in Xiamen, which is the epidemic area in both HBV infection and HCC.
METHODS
Study Participants
Consecutive primary HCC cases (ICD9-155) were recruited from Xiamen Zhongshan Hospital and Xiamen Traditional Chinese Medicine Hospital between December 2011 and July 2014. All HCC patients were incidence patients with the confirmation of liver biopsy and were permanent residents who lived in Xiamen >10 years and aging from 20 to 79 years. Patients were excluded if any of the following conditions were met: (1) liver disease due to parasitosis, diabetes, fatty liver, metabolism disorders, or severe cardiovascular diseases; (2) presence of tumors other than HCC; (3) autoimmune hepatitis or toxic hepatitis; (4) refusal or inability to participate in the investigation because of critical status.
Community-based healthy controls were frequency matched with HCC cases by age (±3 years) and gender, recruited from the people who attending physical examination in the community healthcare center. All control subjects were also permanent residents of Xiamen city without prior history of any cancer aging from 20 to 79 years old. In order to diminish possible risk of bias at maximum level, we have randomly selected these control subjects and confirmed that all study subjects were ethnically unrelated.
In total, 314 incidence HCC cases and 346 healthy controls were enrolled in our study. All study participants provided physically signed consent before the interview. Ethical approval for this study was obtained from the Ethics Committee of Xiamen Center for Disease Control and Prevention and all procedures within this study conformed to the Declaration of Helsinki.
Data Collection
Trained investigators interviewed all study participants face to face with a structured questionnaire containing demographic characteristics, social economic status, indoor air pollution, smoking habit, environmental tobacco smoking, alcohol consumption, tea consumption, food consumption, and general medical history. After the completion of interview of all study participants, data were recorded with double entry verification by using Epidata software version 3.1 (The Epidata Association, Odense, Denmark).
Determination of Hepatitis B Infection
All cases and healthy controls provided a 5-mL blood sample on the day of the interview. Blood samples were centrifuged at 4000 rpm for 10 min to separate plasma and blood cells and stored at −78°C prior to determination of serological markers for hepatitis B infection (including HBsAg, HBsAb, HBcAb, HBeAg, and HBeAb). The laboratory assay was performed in the plasma sample of each study participant by using commercial enzyme-linked immunosorbent assay kits (Wantai BioPharm, Beijing, China). All procedures were strictly conformed with manufacturer's manual; in addition, ∼5% of the samples were randomly selected and repeated for test as duplicated controls.
Statistical Analysis
The SPSS software (IBM, Chicago, IL) version 19 was used to perform all analyses in our study. The chi-squared test was used to examine the differences in demographic characteristics and potential confounders between HCC cases and healthy controls. Unconditional logistic regression was applied to determine the association between environmental factors, hepatitis B infection, and the risk of developing HCC, odd ratios (ORs), and 95% confidence intervals were calculated. Multivariate unconditional logistic regression was performed to evaluate the potential interactions of variables or confounders. After excluding the factors with high correlation, stepwise method was used to establish the multivariate equation. A 2-tailed P value of <0.05 was accepted as being statistically significant.
RESULTS
Demographic Characteristics
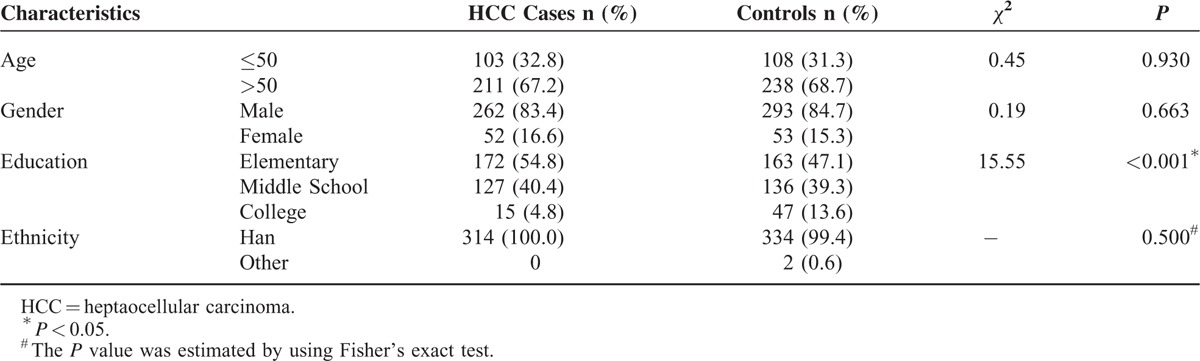
From 2 major hospitals, 314 HCC cases enrolled in this study and matched to 346 community-based healthy controls for age and gender during the study period. Demographic characteristics of the HCC cases and controls are presented in Table 1. As expected, we founded no significant difference among cases and controls in terms of age (P = 0.930) and gender (P = 0.663). However, we observed significant difference in education between cases and controls with a P value <0.001. As for the ethnicity, although we have enrolled 2 minority subjects in the control group while cases were consisted of all Han individuals, no significance was detected (P = 0.500).
TABLE 1.
Demographic Characteristics of HCC Cases and Controls by Numbers (%)
The Association Between Serological Markers of Hepatitis B Infection and HCC Risk
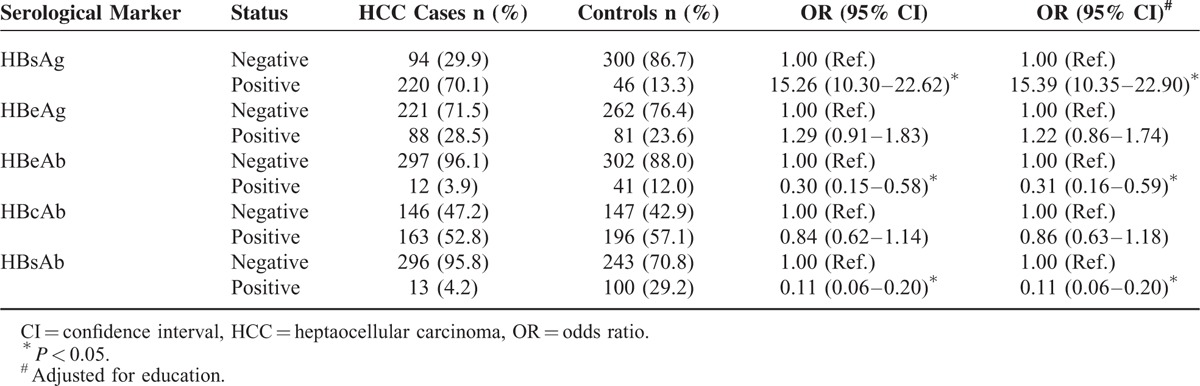
With regard to serological markers of hepatitis B infection, we observed a strong association between HBsAg positive and HCC risk with a crude OR of 15.26 (95% CI = 10.30–22.62). The unconditional logistic regression revealed that the both HBeAb positive and HBsAb positive were inversely associated with the risk of developing HCC, and the crude ORs were 0.30 (95% CI = 0.15–0.58) and 0.11 (95% CI = 0.06–0.20), respectively. Furthermore, the analysis showed the association between HBeAg positive and HBcAb positive was not significant. After the adjustment for education, the analysis demonstrated that the risk among population was 15.39-fold (95CI = 10.35–22.9) when comparing with those without HBsAg positive. Slightly affected by the adjustment, the AOR of population with the protection of HBsAb was 0.11 (95% CI = 0.06–0.20), which is exactly the same when comparing with the crude OR (data shown in Table 2).
TABLE 2.
The Association Between Serological Markers of Hepatitis B Infection and HCC Risk
The Association Between Environmental Factors and HCC Risk
Table 3 presents the association between environmental factors and HCC risk by using unconditional logistic regression. In the food consumption section, the consumption of smoked food (≥1 time/wk) and moldy food are identified as the risk factors of HCC, whereas use of refrigerator, high consumption of vegetable, fruit, and tea demonstrated protective effect against HCC risk. After adjustment, the consumption of smoked food maintained the highest risk among food section with an AOR of 4.80 (95% CI = 2.27–10.16), whereas the tea consumption has been identified as the top protective factor in this section, and the AOR for tea consumption was 0.18 (95CI = 0.12–0.28). However, we failed to observe any significant association between coffee intake and HCC risk.
TABLE 3.
The Association Between Environmental Factors and HCC risk
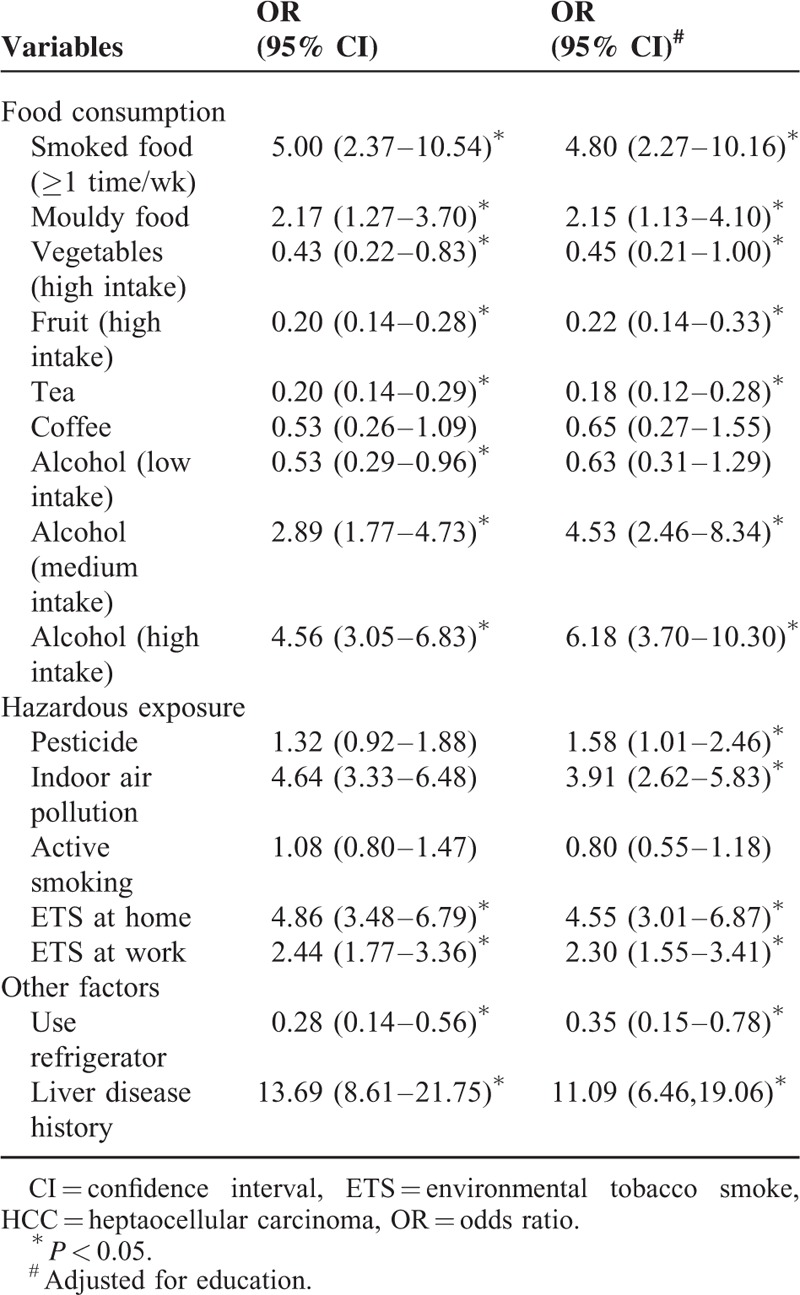
Indoor air pollution was also a risk factor of HCC, according to the results of analysis, the crude OR for indoor air pollution was 4.64 (95% CI = 3.33–6.48). After the adjustment, the association between exposure of pesticide and HCC became significant with an AOR of 1.58 (95% CI = 1.01–2.46) and the AOR for indoor air pollution was 3.91 (95% CI = 2.62–5.80).
According to the analysis of active and passive smoking, environmental tobacco smoke (ETS) at home and work were associated to the incidence of HCC significantly. In detail, ETS at home conferred a 4.86-fold risk (95% CI = 3.48–6.79) when comparing with those who without ETS at home. Similarly, ETS at work was positively correlated with HCC risk with an OR of 2.44 (95% CI = 1.77–3.36) without adjustment. After adjusted for education, the AORs for ETS at home and work were 4.58 (95% CI = 3.01–6.87) and 2.30 (95% CI = 1.55–3.41), respectively.
Alcohol consumption was also correlated with an elevated HCC risk and significant difference with regard to the frequency of alcohol consumption between the alcohol consumers of HCC cases and controls was observed. The AOR for medium and high consumption were 4.53 (95% CI = 2.46–8.34) and 6.18 (95% CI = 3.70–10.30), respectively, when comparing with those who intakes no alcohol. There was no significant association observed between the low consumption of alcohol and HCC risk. In addition, we also found that the liver disease history was correlated with HCC risk significantly. Population with liver disease history maintained an 11.09 fold (95% CI = 6.46–19.06) risk when being compared with the individuals without the factor after adjusted for education.
Multivariate Unconditional Logistic Regression
Multicollinearity diagnostics has been performed among those factors with significance after adjustment in the unconditional logistic regression, and no multicollinearity was observed (data not shown). Consequently, those factors were included in multivariate unconditional logistic regression analysis. The results regarding multivariate analysis were demonstrated in Table 4. As can be seen, HBsAg positive and liver disease history were the major risk factors of HCC. It also has been observed that exposure of pesticide, indoor air pollution, ETS at home and work, and high consumption of alcohol significantly increase the HCC risk. Declined HCC risk was detected among those study participants who have high consumption of fruit and tea (shown in Figure 1).
TABLE 4.
The Multivariate Unconditional Logistic Regression of Factors and HCC Risk
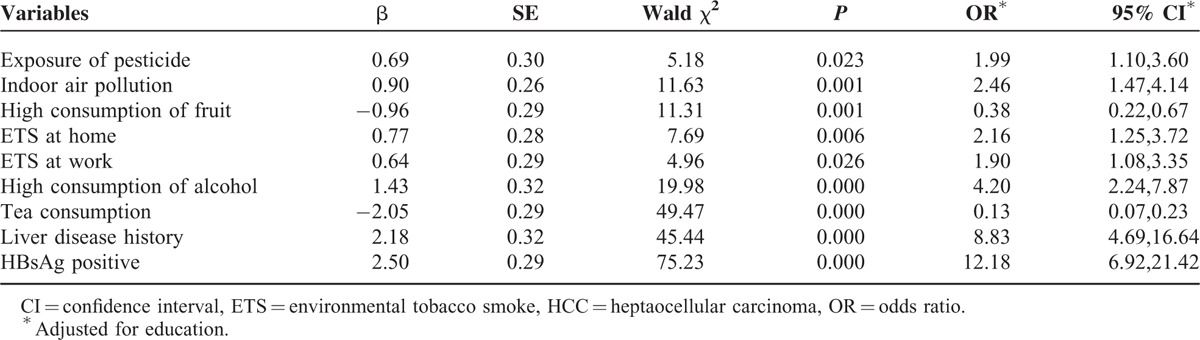
FIGURE 1.
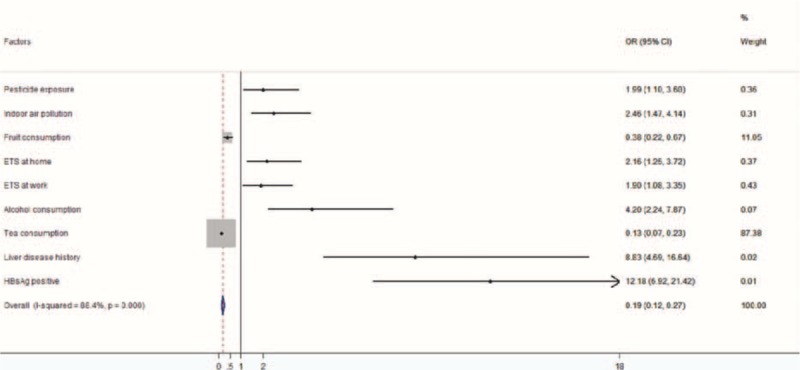
The forest plot of adjusted OR and 95% CI for the multivariate logistic regression. CI = confidence interval, OR = odds ratio.
DISCUSSION
Our investigation revealed that the individuals who exposed to indoor air pollution maintained 3.91-fold HCC risk (95% CI = 2.62–5.83) comparing the reference category after adjustment for education. As a matter of fact, the major component of indoor air pollutant includes formaldehyde, ammonia, benzene, radon, and other volatile organic compounds. Among them, formaldehyde has been classified as a human carcinogen and also can irritate skin and eyes. Due to its wide use in house decoration, the concentration of formaldehyde could be hazardous, and the natural emission of formaldehyde is a very slow process which will take ∼5 to 10 years to reach complete elimination inside a house. Previously, exposure to formaldehyde has been associated with increased risk of leukemia and death,8 and this link has also been confirmed by meta-analysis involving 2 large-scale studies with in total 38,000+ study subjects with a pooled RR of 1.53 (95% CI = 1.11–2.21).9 However, so far it has not yet been reported about elevating the HCC risk; therefore the investigation in future should focus on the formaldehyde and hepatocellular toxicity. Benzene is a colorless and highly flammable liquid with a sweet smell, and its carcinogenicity has been confirmed for long time. However, benzene mostly renders damage to nervous and respiratory systems; seldom studies which investigate the association between indoor air pollutant and HCC risk were conducted.
The results also gave a positive association between pesticide exposure and HCC risk with an OR of 1.58 (95% CI = 1.01–2.46). In contrast, a case–control study conducted in Egypt involving 236 HCC cases and the same number of controls showed no significant association between pesticide exposure and HCC risk.10 It has been generally acknowledged that organochlorine pesticides possess carcinogenicity, and organochlorine pesticides induced liver cancer has successfully observed among mice.11 Based on the epidemiological and biological evidence, we should raise concern about the occupational exposure and daily food residue, and on the other hand, this association must be further confirmed with more investigations.
Fruits are rich source of antioxidants, including retinol, carotenoids, and vitamin C, which are considered possess protective effects against cancer.12 Flow cytometric analysis indicated that a novel triterpenoid isolated from fruit is capable of arresting the cell cycle and inducing apoptosis in human hepatocarcinoma cells.13 Animal experiment also observed the anticancer effect of fruit extract which capable of reducing the tumor incidence, tumor yield, and tumor burden among Swiss Albino Mice with chemical-induced HCC.14 Although biological evidence has been obtained, a latest meta-analysis including 1,290,045 subjects and 19 studies showed no significant association between fruit consumption and reduced HCC risk; however, vegetable intake can significantly lower the HCC risk with a summary RR of 0.72 (95% CI = 0.63–0.83).15 Similarly, the multicenter cohort study conducted in Europe also obtained no evidence for the protective effect of fruit intake but further confirmed the anti-HCC risk caused by vegetable consumption.16 Inconsistent with previous epidemiological studies, but we still consider fruit consumption as an universal, accessible prevention against HCC and should be promoted.
Tea consumption is a part of traditional life style among Xiamen residents, our analysis showed that 80.9% of controls intakes tea regularly. As expected, the logistic regression demonstrated a strong protective effect against HCC risk caused by tea intake with an OR of 0.18 (95% CI = 0.12–0.28). Extract from camellia ptilophylla which is a kind of tea commonly consumed in southern China has been confirmed that capable of inhibiting HepG2 cells growth through inducing apoptosis.17 Aside of the inducing cancer cell apoptosis, cell assay also revealed that tea extract Epigallocatechin-3-gallate (EGCG) can enhance the sensitivity of HCC cells to 5-FU antitumor activity which is commonly used as chemotherapeutic drug.18 The prospective study with a median follow-up of 11 years showed a significant reduced HCC risk of tea intake with a RR of 0.41 (95% CI = 0.22–0.78).19 Given the prospective design and large sample size, the result was solid and appropriate; therefore, we suggested that tea intake can serve as a daily chemoprevention in the HCC epidemic area such as Xiamen.
Excessive alcohol consumption has been universally classified as the major risk factor of HCC, especially in European and American population in which HBV is less prevalent. The ORs we estimated in our study participants for medium and high consumption of alcohol were 4.53 (95% CI = 2.46–8.34) and 6.18 (95% CI = 3.70–10.3), respectively. Among Danish cohort study involving 15,258 males and 3552 female individuals, researchers observed significant elevated standardize incidence rate (SIR) of cancer in both genders, but the SIR was higher in women when being compared with their male counterparts.20 Biologically speaking, after absorption, alcohol is then metabolized by enzymes, which are body chemicals that breakdown other chemicals. In the liver, an enzyme called alcohol dehydrogenase (ADH) mediates the conversion of alcohol to acetaldehyde. Acetaldehyde is rapidly converted to acetate by other enzymes and is eventually metabolized to carbon dioxide and water. The genetic polymorphism on aldehyde dehydrogenase 2 (ALDH2) has been associated with the development of HCC, due to the mutant triggered inactive isoenzyme and elevated acute alcohol intoxication. It has been reported that the mutant is more prevalent among Asian than Caucasian; therefore the association studies regarded with the ALDH2 mutant and HCC risk were mostly conducted among Asian, although there is no conclusion yet. A case–control study conducted among Japanese population and results indicated that ALDH2 mutant can modify HCC risk among light to moderate consumers but not heavy drinkers.21 In Chinese population, no significant association was observed between ALDH2 genotype and HCC risk, and various genetic models were applied to calculate the OR.22 We infer that the genotyping assay of ALDH2 should be performed to further confirm or rule out the association.
The association studies between smoking and HCC have been conducted in both domestic and abroad; however, the results were inconsistent. Our study failed to observe the positive association between active smoking and HCC risk. However, significance was found among ETS at home and work with ORs of 4.58 (95% CI = 3.01–6.87) and 2.43 (95% CI = 1.55–3.41), respectively. As a matter of fact, the latest evidence has shown that the chemical compounds observed in sidestream smoke appear to have more unsaturated and less oxygenated components than those observed in mainstream smoke,23 and sidestream smoke is inhaled mainly by passive smokers. These findings confirmed that our assumption about passive smoking and HCC risk.
Our study has extensively investigated the association between serological markers of HBV infection and HCC risk. With no surprise, the population with HBsAg maintains 15.39-fold (95% CI = 10.35–22.90) HCC risk when being compared with the HBsAg negative, and HBsAb also demonstrates a strong protective effect against HCC with an OR of 0.11 (95% CI = 0.06–0.20). Additionally, HBeAb was also identified as the protective factor. Hepatocellular carcinoma currently has become the second death cause among population aged from 35 to 54 years old. According to the data released in 2012, the incidence and mortality of HCC in China were 22.27 per 100,000 and 21.41 per 100,000, respectively. Comparing with the corresponding indicators of USA, the figures in China were 3.6-fold and 4.7-fold, respectively. As for the incidence and mortality of HCC in Japan, the figures in China were 2.4-fold and 2.8-fold, respectively. China takes the highest death toll of HCC among 20 top HCC epidemic countries, in accurate, China has the 20% population of global range but >50% of HCC incidence and mortality occur in China. There will be ∼ 800,000 incidence of HCC cases in worldwide range annually, among them, 85% of cases are of chronic HBV infection, and 10% of HCV infection. Before the implementation of HBV vaccination program, 10% of Chinese population was HBsAg positive, and with the natural progress of HBV infection, these individuals would possibly advance to liver cirrhosis and liver cancer. Without effective intervention, there will be 8 to 10 million death toll due to HCC, and China will have to face the substantial pressure and disease burden caused by HBV- and HCV-induced HCC.
In summary, we managed to conduct a case–control study to identify possible protective and risk factors of HCC in an HBV and HCC epidemic area. As can be seen in the analysis results, HBV and alcohol intake still are the major risk factors of HCC; therefore, the application of HBV vaccine should be further promoted among not only children but also adults without the protection of HBsAb. The reduction of alcohol intake should also be promoted, especially among the high-risk population, for example, people with chronic HBV infection. Indoor air pollution and exposure to pesticide have been newly identified as the risk factor of HCC which required further investigation. Fruit and tea can be served as chemoprevention in daily life due to their high accessibility.
Acknowledgments
The authors would like to express gratitude to the Dr. Qianguo Mao of Xiamen Traditional Medicine Hospital and Ms. Jianhui Wu of Xiamen Zhongshan Hospital for their great efforts in sample collection.
Footnotes
Abbreviations: ALDH2 = aldehyde dehydrogenase 2, ETS = environmental tobacco smoke, HBV = hepatitis B virus, HCC = heptaocellular carcinoma, HCV = hepatitis C virus.
JN and YL are equally contributed to this study.
Funding: this study has been financially supported by grants from the Social Development Program (No. 3502Z20124023) of the Xiamen Bureau of Science and Technology.
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Chen JG, Zhu J, Zhang YH. Incidence trend of liver cancer; an analysis of 40 year's data from Qidong population-based cancer registry. China Cancer 2014; 23:621–628. [Google Scholar]
- 2.Raza SA, Clifford GM, Franceschi S. Worldwide variation in the relative importance of hepatitis B and hepatitis C viruses in hepatocellular carcinoma: a systematic review. Br J Cancer 2007; 96:1127–1134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Parkin DM. The global health burden of infection-associated cancers in the year 2002. Int J Cancer 2006; 118:3030–3044. [DOI] [PubMed] [Google Scholar]
- 4.Villar S, Oritz-Cuaran S, Abedi-Ardekani B, et al. Aflatoxin-induced TP53 R249S mutation in hepatocellular carcinoma in Thailand: association with tumors developing in the absence of liver cirrhosis. PLoS One 2012; 7:e37707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kumar V, Kato N, Urabe Y, et al. Genome-wide association study identifies a susceptibility locus for HCV-induced hepatocellular carcinoma. Nat Genet 2011; 43:455–458. [DOI] [PubMed] [Google Scholar]
- 6.Liang X, Bi S, Yang W, et al. Reprint of: Epidemiological serosurvey of Hepatitis B in China—declining HBV prevalence due to Hepatitis B vaccination. Vaccine 2013; 31 Suppl 9:J21–J28. [DOI] [PubMed] [Google Scholar]
- 7.Wu XQ, Mi HF, Rong B, et al. Analysis on death causes of liver cancer of inhabitants in Xiamen City from 2002 to 2011 Article in Chinese. Chin J Dis Control Prev 2014; 18:613–616. [Google Scholar]
- 8.Dreyfuss JH. Occupational formaldehyde exposure linked to increased risk of myeloid leukemia and death. CA Cancer J Clin 2010; 60:135–136. [DOI] [PubMed] [Google Scholar]
- 9.Schwilk E, Zhang L, Smith MT, et al. Formaldehyde and leukemia: an updated meta-analysis and evaluation of bias. J Occup Environ Med 2010; 52:878–886. [DOI] [PubMed] [Google Scholar]
- 10.Ezzat S, Abdel-Hamid M, Eissa SA, et al. Associations of pesticides, HCV, HBV, and hepatocellular carcinoma in Egypt. Int J Hyg Environ Health 2005; 208:329–339. [DOI] [PubMed] [Google Scholar]
- 11.Reuber MD. Carcinogenicity testing of chemicals with particular reference to organochlorine pesticides. Sci Total Environ 1978; 10:105–115. [DOI] [PubMed] [Google Scholar]
- 12.Stanner SA, Hughes J, Kelly CN, et al. A review of the epidemiological evidence for the antioxidant hypothesis. Public Health Nutr 2004; 7:407–422. [DOI] [PubMed] [Google Scholar]
- 13.Hong J, Min HY, Xu GH, et al. Growth inhibition and G1 cell cycle arrest mediated by 25-methoxyhispidol A, a novel triterpenoid, isolated from the fruit of Poncirus trifoliata in human hepatocellular carcinoma cells. Planta Med 2008; 74:151–155. [DOI] [PubMed] [Google Scholar]
- 14.Singh R, Sharma J, Goyal PK. Prophylactic role of Averrhoa carambola (star fruit) extract against chemically induced hepatocellular carcinoma in Swiss albino mice. Adv Pharmacol Sci 2014; 2014:158936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yang Y, Zhang D, Feng N, et al. Increased intake of vegetables, but not fruit, reduces risk for hepatocellular carcinoma: a meta-analysis. Gastroenterology 2014; 147:1031–1042. [DOI] [PubMed] [Google Scholar]
- 16.Bamia C, Lagiou P, Jenab M, et al. Fruit and vegetable consumption in relation to hepatocellular carcinoma in a multi-centre, European cohort study. Br J Cancer 2015; 112:1273–1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yang XR, Wang YY, La KK, et al. Inhibitory effects of cocoa tea (Camellia ptilophylla) in human hepatocellular carcinoma HepG2 in vitro and in vivo through apoptosis. J Nutr Biochem 2012; 23:1051–1057. [DOI] [PubMed] [Google Scholar]
- 18.Yang XW, Wang XL, Cao LQ, et al. Green tea polyphenol epigallocatechin-3-gallate enhances 5-fluorouracil-induced cell growth inhibition of hepatocellular carcinoma cells. Hepatol Res 2012; 42:494–501. [DOI] [PubMed] [Google Scholar]
- 19.Bamia C, Lagiou P, Jenab M, et al. Coffee, tea and decaffeinated coffee in relation to hepatocellular carcinoma in a European population: multicentre, prospective cohort study. Int J Cancer 2015; 136:1899–1908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thygesen LC, Mikkelsen P, Andersen TV, et al. Cancer incidence among patients with alcohol use disorders—long-term follow-up. Alcohol Alcohol 2009; 44:387–391. [DOI] [PubMed] [Google Scholar]
- 21.Sakamoto T, Hara M, Higaki Y, et al. Influence of alcohol consumption and gene polymorphisms of ADH2 and ALDH2 on hepatocellular carcinoma in a Japanese population. Int J Cancer 2006; 118:1501–1507. [DOI] [PubMed] [Google Scholar]
- 22.Zhou D, Xiao L, Zhang Y, et al. Genetic polymorphisms of ALDH2 and ADH2 are not associated with risk of hepatocellular carcinoma among East Asians. Tumour Biol 2012; 33:841–846. [DOI] [PubMed] [Google Scholar]
- 23.Schramm S, Carré V, Scheffler JL, et al. Analysis of mainstream and sidestream cigarette smoke particulate matter by laser desorption mass spectrometry. Anal Chem 2011; 83:133–142. [DOI] [PubMed] [Google Scholar]


