Supplemental Digital Content is available in the text
Abstract
Knee osteoarthritis (KOA) is a common disorder in elderly. There is no known cure for KOA, and thus therapeutic strategies of alleviating symptoms are increasingly emphasized. Moxibustion has been widely used to treat KOA; however, results are inconclusive. The aim of our study is to critically reassess the effects of moxibustion on KOA.
We searched PubMed, EMBASE, Cochrane Central Register of Controlled Trials (CENTRAL), and Chinese Biomedical Literature database (CBM) through 25 November 2015. Two independent reviewers selected studies and abstracted information, as well as assessed the risk of bias using Cochrane risk of bias tool. The random-effects meta-analyses were performed based on abstracted data.
We initially captured 163 citations and added 4 records through checking review. After critical appraisal, 13 RCTs were included. Meta-analyses indicated that moxibustion is not statistically different from oral drug in improving the response rate (MD = 1.09; 95% CI = 1.00, 1.20; P = 0.05), alleviating pain and improving physical function. Our meta-analysis also found that moxibustion is superior to usual care and sham moxibustion in reducing WOMAC score (MD = 7.56; 95% CI = 4.11, 11.00; P = 0.00), pain and function, as well as increasing QoL. Moreover, most AEs caused by moxibustion can heal without medical care.
We concluded that moxibustion treatment is equal to the oral drugs and intra-articular injections and may be an alternative in treating patients with KOA.
INTRODUCTION
Knee osteoarthritis (KOA) is a common chronic degenerative disease of knee joint in elderly,1 which significantly impairs the physical function and quality of life (QoL) of target population.2,3 Issued data illustrated that ∼10% of people aged >60 experience the KOA symptoms4 and the disability rate of KOA can reach 53%.5 With the increase in life expectancy and obesity population, the prevalence of symptomatic KOA is also increasing.1 There is no known cure for KOA, so the current regimes are primarily aimed at reliving symptom and recovering function.6,7 Pharmacological interventions are extensively adopted to treat KOA; however, numerous adverse events (AEs) related to agents limit the usage of these therapies.8 Consequently, researchers turn gradually their attention to nonpharmacological therapies, such as acupuncture and moxibustion.9
Moxibustion is a common noninvasive traditional Oriental intervention,10 which uses mainly the heat generated by burning herbal preparations containing moxa and mugwort (Artemisia vulgaris) to stimulate acupoints for alleviating the symptoms.11 This technique has been widely used to treat various conditions (eg rheumatic diseases and digestive dysfunction) in east Asia countries.6 Some randomized controlled trials (RCTs) concerning the effects of moxibustion on KOA have been published.6,12,13 Most studies demonstrated that moxibustion is benefit to KOA;10,14,15 however remaining studies do not support this conclusion.16,17
There is currently 1 systematic review18 which objectively assessed the effects of moxibustion on OA; however it is now outdated. And what's more, these authors just assessed response rate, pain, and AEs; other important outcomes such as physical function and QoL were not included. To address these issues and facilitate informed decision-making, the aim of our systematic review is to critically reassess the available evidence based on RCTs concerning the effects of moxibustion on KOA.
METHODS
We performed this article based on the methods recommended by Cochrane collobration19 and reported the summarized results according to Preferred Reporting Items for Systematic Review and Meta-analysis statemtent.20 Because our study was performed based on previous studies, so the ethical approval and informed consent were not required.
Selection Criteria
We predesigned following selection criteria with the PICOS principle (population, intervention, comparison, outcome, and study design): (1) P: adults diagnosed with KOA using definitive diagnostic criteria including American College of Rheumatology (ACR) and guiding principles of clinical research on new drugs (GPCRND)-KOA was included. (2) I and C: moxibustion alone versus conventional interventions including usual care, oral drug, intra-articular injection, and sham moxibustion. (3) O: we assessed the response rate, pain, physical function, AEs, and QoL. The response rate, pain, physical function, and AEs were regarded as primary outcomes and QoL were specified as secondary outcomes. All outcomes were assessed with definitive assessment instrument, such as the GPCRND, Western Ontario and McMaster Universities Questionnaire (WOMAC), numeric rating scale (NRS), and visual analogue scale (VAS). Because of the durations of treatment were different in all eligible studies, so we purposely analyzed it into 3 terms: short term (duration ≤ 6 weeks), midterm (7 weeks ≤ duration ≤ 13 weeks), and long term (duration ≥ 14 weeks). In our study, we calculated the change value between baseline and any specified endpoints to be as estimates using the method proposed by Davidson et al.21 (4) S: only randomized controlled trials (RCTs) were incorporated.
Identification of Literature
Two independent reviewers (G-MS and XT) to search potential citations in PubMed, Embase, Cochrane Register Central of Controlled Trials (CENTRAL), and Chinese Biomedical Literature database (CBM) through 25 November 2015 using following terms: moxibustion, osteoarthriti∗, degenerative arthriti∗, osteoarthros∗, osteoarthrosis deformans, random∗. We also customized search algorithms to update the research results weekly and manually checked the reference lists of eligible studies to include any potential studies. We did not restrict language and publication status. All search algorithms were documented in supplemental material-search algorithm (SM search algorithm).
Selection of Study
Two reviewers (G-MS and X-LP) independently selected studies. After removing duplicates, these reviewers screening the eligibility of remaining citations through reviewing title and abstract. The third step is to critically check eligibility of remaining citations based on the full text. Any disagreements concerning the eligibility of each study were resolved by consulting a third author (XT).
Abstraction of Essential Information
After screening literature, 2 independent investigators (G-MS and X-LP) to extract the following essential information with predesigned data extraction table (SM-Table 1): the first author, year of publication, diagnostic criteria, sample size, age of participants, details of intervention regimes, outcomes, and information of assessing the risk of bias. We will contact the corresponding author to obtain necessary information if the data were inadequate. A third reviewer (XT) will be consulted if discrepancies occurred.
Assessment of Risk of Bias
We adopted the Cochrane's risk of bias instrument to assess the methodological quality of eligible studies.19 Five domains including selection bias, performance bias, detection bias, attrition bias, and reporting bias were critically assessed accordingly in order to judge the level of risk of bias of each study. Each domain was rated as “high risk,” “unclear risk,” or “low risk” depending on the match degree between information extracted and assessment criteria.19
Statistical Analysis
All analyses were performed with Review Manager (RevMan) software (Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2013). The pooled effect size was expressed as relative risk (RR) with 95% confidence intervals (CIs) for dichotomous data and standard mean difference (SMD) or mean difference (MD) with 95% CIs for continuous data respectively. We also qualitatively evaluated heterogeneity across studies using Cochran's Q statistic with P value. The degree of heterogeneity was quantified using I2 statistic, which is defined as the variation degree can be explained by heterogeneity. I2 < 50% and P > 0.1 indicate homogeneous in all studies.19 All meta-analyses were performed via random-model which considered the variation among included studies. Subgroup analysis was conducted according to duration of measurement and various control interventions. A qualitative analysis was used to describe the studies with insufficient data and substantial heterogeneity or inadequate numbers of studies. We eliminated studies with high risk to perform sensitive analysis. Owing to the limited number (below 10) of studies included in each analysis, publication bias was not assessed.
RESULTS
Selection of Studies
We initially captured 263 citations and eliminated 61 duplicate with EndNote software. After reviewing the title and abstract of remaining records, 166 were excluded. We accessed full texts of remaining 36 records and 24 studies were excluded due to various reasons (Figure 1). Finally, 13 eligible RCTs6,9,10,12–15,17,22–25 were included.
FIGURE 1.
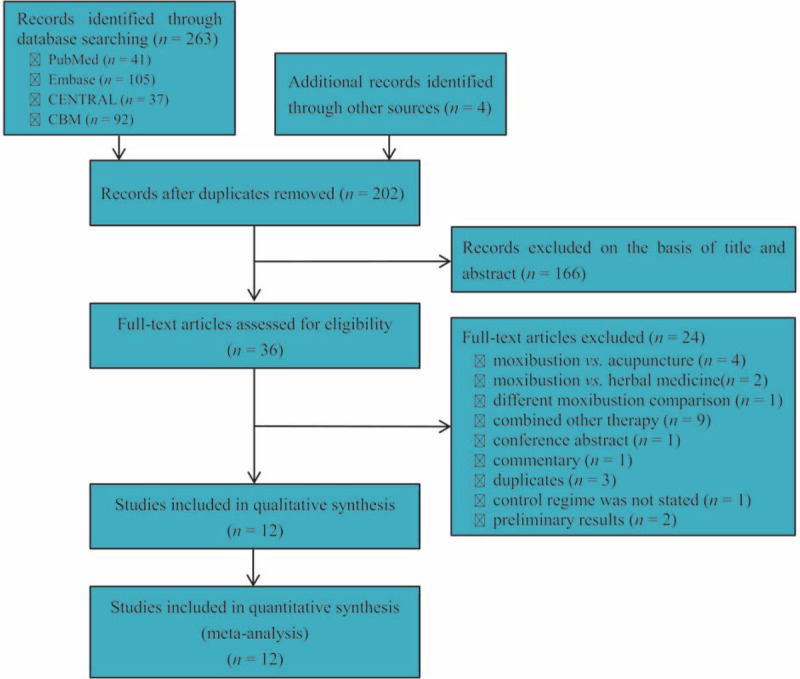
Flow diagram of literature retrieval and selection: 263 potential citations and additional 4 records were initially captured and eventually 12 eligible studies including 13 RCTs were incorporated into our systematic review and meta-analysis. RCTs = randomized controlled trials.
Basic Characteristics of Eligible RCTs
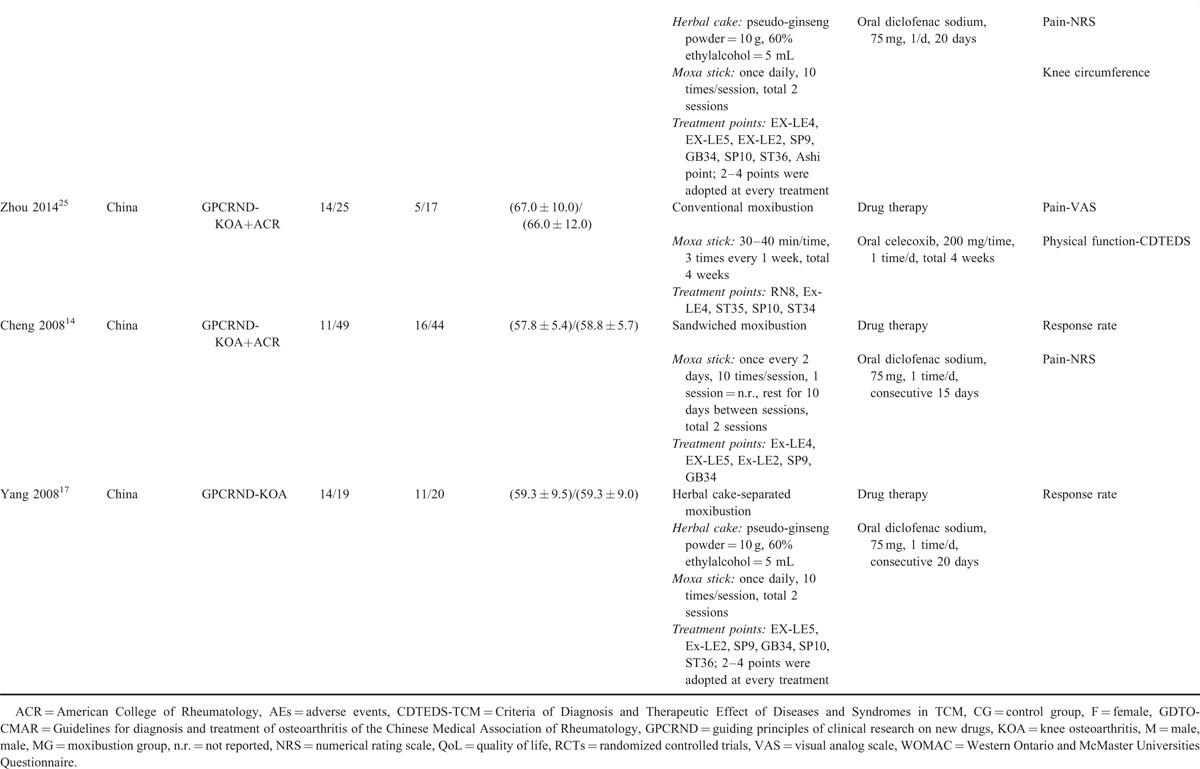
Table 1 documented the characteristics of all eligible RCTs. All studies were published between 2008 and 2015 and 110 was performed in Korea. One9 study was a 3-arm design which included heat-sensitive moxibustion (HSM), conventional moxibustion, and intra-articular injection, so we divided it into 2 RCTs. Consequently, sample size of each RCT was varied from 50 to 288 and the sum was 1309. Three RCTs9,17,25 adopted GPCRND scale to assess the response rate. Two RCTs8,10 used WOMAC scale to assess the pain and physical function. Four RCTs12,14,15,24 selected criteria of diagnosis and therapeutic effect of diseases and syndromes in TCM (CDTEDS) to assess pain and response rate. Two RCTs6,10 adopted Short-Form 36 Health Survey (SF-36) to assess QoL. Two RCTs selected VAS23 and Jane Scott method25 to assess pain respectively.
TABLE 1.
Basic Characteristics of 13 RCTs Included into this Systematic Review and Meta-Analysis
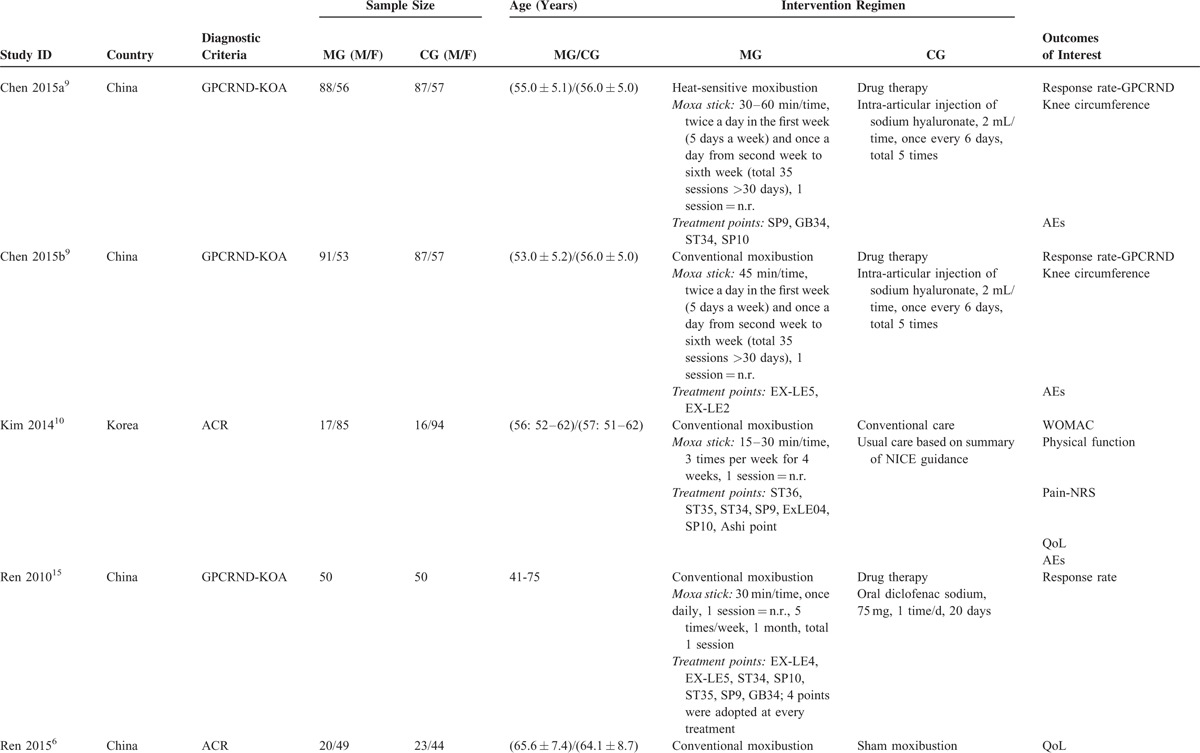
TABLE 1 (Continued).
Basic Characteristics of 13 RCTs Included into this Systematic Review and Meta-Analysis
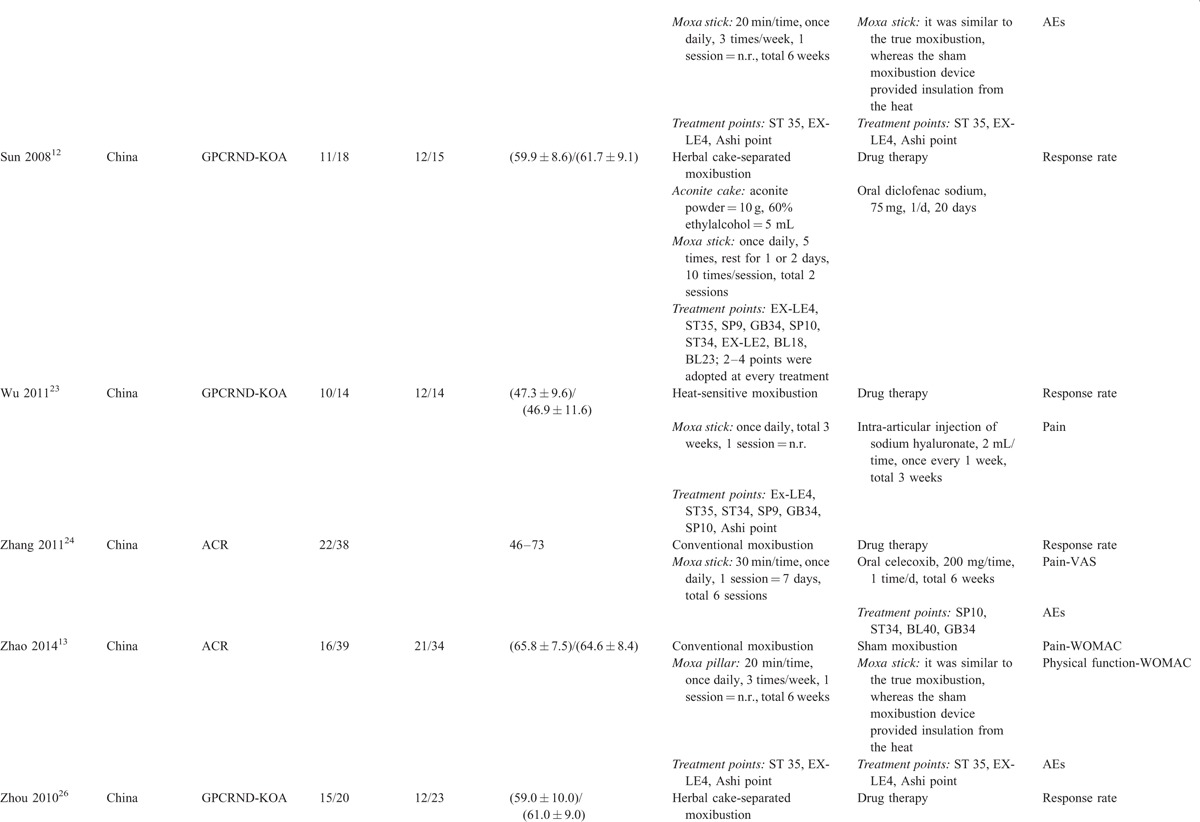
TABLE 1 (Continued).
Basic Characteristics of 13 RCTs Included into this Systematic Review and Meta-Analysis
Assessment of Risk of Bias
Figure 2 graphically delineated the result of assessment of risk of bias. Nine RCTs generated appropriately random sequence with computer-generated randomization table or random number table.6,8–10,12,22,24,25 For remaining RCTs, 214,17 generated inappropriately random sequence and 25,23 did not state details of generating random sequence. Five RCTs6,8–10 performed appropriately concealment of allocation using the central randomization system, sealed envelopes, or letter codes. 56,8–10 and 46,8,9 RCTs performed blinding participants and personnel and conducted blinding to outcomes assessor respectively. All RCTs reported the number and reasons of dropout or withdrawal. Seven RCTs8,9,14,17,22,24 used the intention-to-treat (ITT) method to analyze data. All eligible studies reported the anticipated outcomes.
FIGURE 2.
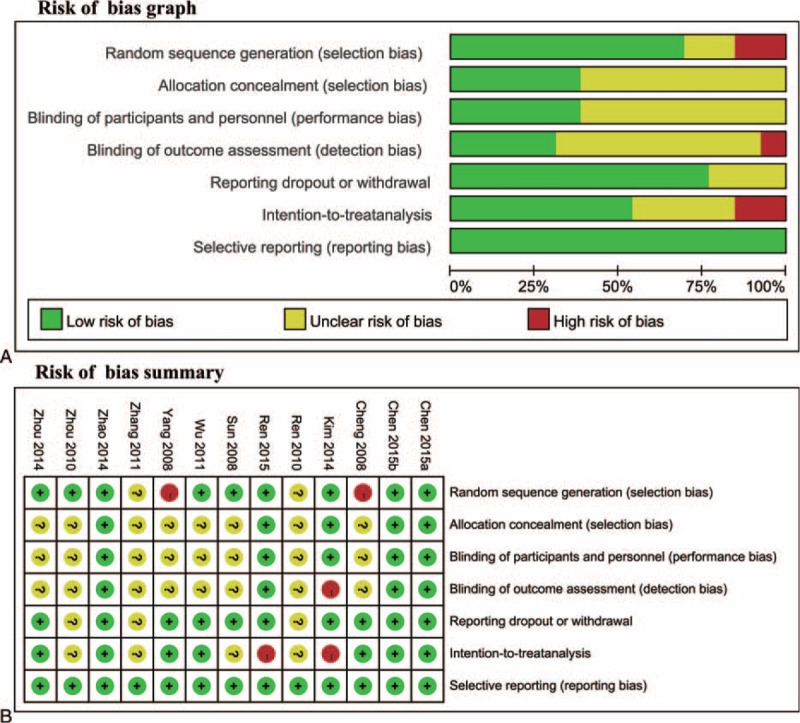
Assessment of risk of bias: (A) risk of bias graph, (B) risk of bias summary.
Response Rate: Results of Meta-Analyses
Of all eligible RCTs, 712,14,15,17,22,23,25 reported the response rate and control regimens included intra-articular injection and oral drug. These data were expressed as dichotomous. Moreover, although results were not transformed into response rate, 3 RCTs9,10 reported the GPCRND and WOMAC scores, respectively.
Because all 7 RCTs reported the short-term response rate and 2 types of control regimes were designed, we performed subgroup to analyze these data. Meta-analysis suggested that moxibustion increased the response rate compared with oral drug (RR = 1.09; 95% CI = 1.03, 1.17; P = 0.00; heterogeneity: I2 = 9%, P = 0.36; Figure 3A). Compared with intra-articular injection, the result did not indicate statistically different (RR = 0.96; 95% CI = 0.86, 1.07; P = 0.45; Figure 3A). We performed sensitive analysis through eliminating 2 RCTs with high risk to test robustness of pooled result and indicated that moxibustion was not statistically different from oral drug (MD = 1.09; 95% CI = 1.00, 1.20; P = 0.05; heterogeneity: I2 = 19%, P = 0.29).
FIGURE 3.
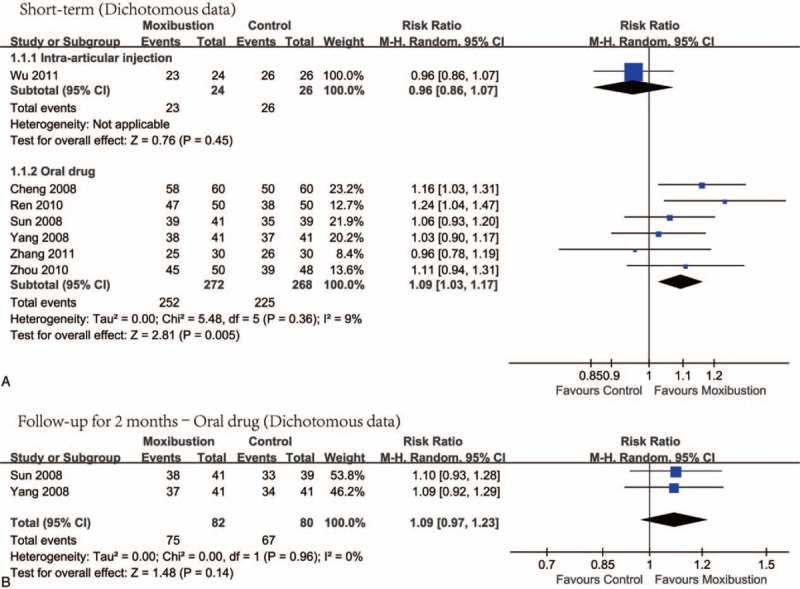
Meta-analysis on the response rate: (A) moxibustion relative to intra-articular injection and oral drug short term and (B) moxibustion versus oral drug follow-up 2 months: random-effects analysis.
Two RCTs12,17 reported the response rate after follow-up 2 months. Meta-analysis revealed that the moxibustion was not superior to oral drug (RR = 1.09; 95% CI = 0.97, 1.23; P = 0.14; heterogeneity: I2 = 0%, P = 0.96; Figure 3B).
Three RCTs9,10 reported GPCRND or WOMAC scores, in which various control regimes and durations of treatment were designed, so we performed separate meta-analysis using subgroup analysis. Meta-analysis suggested that, compared with intra-articular injection, moxibustion did not significantly reduce the GPCRND score at short-term (MD = 0.91; 95% CI = −0.75, 2.87; P = 0.36; heterogeneity: I2 = 95%, P = 0.00; ESM-3a) and after follow-up 7 months (MD = 1.15; 95% CI = -1.50, 3.79; P = 0.39; heterogeneity: I2 = 97%, P = 0.00; SM-Figure 1A). Compared with usual care, the moxibustion effectively decreased the WOMAC score at short-term (MD = 8.19, 95% CI = 3.32, 13.06, P = 0.00; SM-Figure 1B) and midterm (MD = 6.92, 95% CI = 2.04, 11.80, P = 0.00; SM-Figure 1B).
Pain: Results of Meta-Analysis
Total 6 RCTs8,10,14,23–25 reported pain, in which oral drug, usual care or sham moxibustion was used in the control group. Meta-analyses indicated that, compared with oral drug, moxibustion did not significantly alleviate pain (SMD = -0.17; 95% CI = -0.39, 0.05; P = 0.12; heterogeneity: I2 = 1%, P = 0.39; Figure 4A), whereas it significantly relieved pain compared to usual care and sham moxibustion at short-term (Figure 4A), mid-term (Figure 4B) and long-term (Figure 4C).
FIGURE 4.
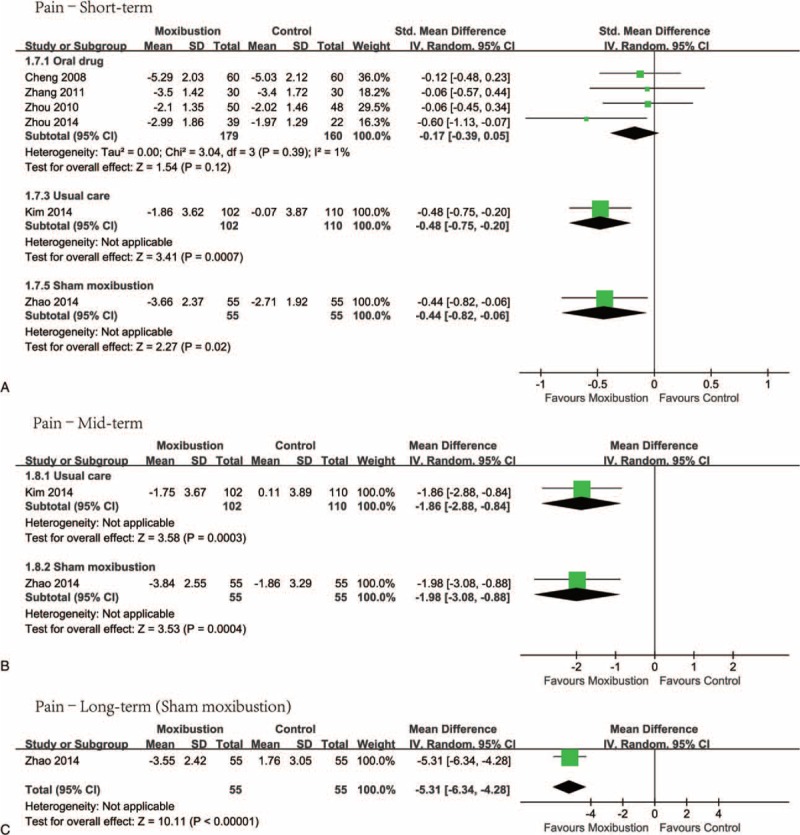
Meta-analysis on pain: (A) comparing moxibustion with oral drug, usual care, and sham moxibustion at short term, (B) moxibustion relative to usual care and sham moxibustion at midterm, and (C) active moxibustion versus sham moxibustion at long term.
Physical Function
Physical function was presented in 3 eligible RCTs.8,10,24 We did not perform meta-analysis due to insufficient numbers of studies. Nevertheless, we used RevMan software to graphically displayed results (SM-Figure 2). These findings suggested that moxibustion effectively improved physical function of KOA patients relative to usual care and sham moxibustion. However, it was not statistically superior to oral drug.
QoL
Two RCTs6,10 reported the information of QoL, in which 2 various control regimes were designed. We adopted the qualitative method was used to analyze the information of QoL due to the available data were insufficient to perform quantitative synthesis. Kim et al10 reported that, compared with usual care, the moxibustion improved the status of physical function (PF) and social function (SF) but remaining indices did not at short term. Moreover, their study revealed that moxibustion improved body pain (BP) at midterm. Ren et al6 suggested that KOA patients in the active moxibustion group experienced statistically greater improvement in mental health (MH) than sham moxibustion at short term. Meanwhile, they also found better MH and vitality (VT) status in the true moxibustion group at short-term and midterm.
AEs
Six RCTs6,8–10,23 reported AEs after treatment; however, meta-analysis was not conducted due to insufficient data. Chen et al9 reported no AEs in all participants. Kim et al10 enrolled 102 KOA patients in the moxibustion group, of which 48 and 7 patients experienced AEs at least once and >5 times respectively. In Ren et al's study,6 although 22 KOA patients receiving moxibustion experienced blisters which healed after 1 week, most patients regarded moxibustion as a safe procedure. Zhang et al23 found no AEs in the moxibustion group; however acid reflux (n = 1), nausea (n = 1), and epigastric pain (n = 1) were observed in the oral celecoxib group. Zhao et al8 reported that, in the active moxibustion group, 10 patients experienced skin flushing of ∼5 mm in diameter at treatment sites but the flushing disappeared within 3 days without medical care.
DISCUSSION
KOA characterized mainly by pain and dysfunction is a common health problem in elderly.26,27 It has been regarded as the important contributor to disability and reduced QoL of target population.2,3,6 There is no known cure for KOA, consequently the therapeutic strategy of mitigating pain and recovering function are currently emphasized,7,18 of which moxibustion is widely used.12,18
Our meta-analyses suggested that moxibustion was not statistically different from oral drug in alleviating pain, improving function, and increasing response rate. The pooled result of pain and function was supported by most eligible studies.14,23,25 However, the response rate was inconsistent with that of Choi et al's study.18 It must be noted that 2 RCTs with high risk14,17 were incorporated in Choi et al's study to calculate summarized estimate. Two RCTs8,10 compared moxibustion with usual care and sham moxibustion in mitigating pain respectively. Summarized results suggested that KOA patients receiving moxibustion experienced statistically greater improvement in pain than patients receiving usual care and sham moxibustion. These findings revealed that the effect of moxibustion in alleviating pain is different from the effect of placebo. Qualitative analyses revealed that KOA patients receiving moxibustion experienced statistically greater improvement in function than patients receiving usual care and sham moxibustion. One RCT22 suggested that moxibustion was not statistically different from intra-articular injection in the response rate. WOMAC questionnaire10 and GPCRND scale9 have been validated and widely used in assessment of symptoms and signs of KOA and the lower scores represent better status. Two RCTs9 reported the GPCRND score and pooled results did not generate favorable effect for moxibustion. One RCT10 presented the WOMAC score and indicated reduced WOMAC score in the moxibustion group. Pooled result based on dichotomous data was consistent with results generated from the GPCRND score, and thus the conclusion that the moxibustion was equal to intra-articular injection was supported.
Moxibustion treat various disorders mainly based on temperature and infrared radiation generated from burning moxa or mugwort.6 KOA is categorized into arthromyodynia in traditional Chinese medicine theory.28 Moxibustion can produce hemostatic, analgesic and desiccant effects, as well as alleviate abdominal pain through decreasing the contents of interlukin-1β (TL-1β),29–31 tumor necrosis factor-α (TNF-α),31,32 matrix metalloproteinase-1 (MMP-1),29,33 MMP-13,33 MMP-1/matrix metalloproteinase inhibitor-1 (TIMP-1),34 prostaglandin-E2 (PGE2),30 nitric oxide (ON),30,35 and simultaneously increasing proteoglycan, type 2 collagen29 after stimulating acupoints.36,37 These effects may effectively alleviate pain, improve function, and increase QoL, as well as increase the response rate eventually. These mechanisms that moxibustion treating KOA are similar with that of conventional drugs.29,32,34 Consequently, these are not statistically different in alleviating pain, recovering function, and increasing response rate between both methods.
Although moxibustion have a positive effect on KOA, those factors promoting moxibustion to produce treatment effects also are primarily contributor to various AEs, such as burn wounds and pruritus when moxa lit on or above the acupoints. In our study, 3 RCTs9,23 found that patients receiving moxibustion did not experience AEs. Remaining 3 RCTs6,8,10 reported the occurrence of burn wounds, pruritus, fatigue, blisters, and skin flushing in moxibustion. These findings were supported by Park et al's systematic review.38 Must be noted is that all AEs can heal without medical care8 and most patients regarded moxibustion as a safe procedure.6 Moreover, 1 RCT23 found that oral celecoxib caused acid reflux, nausea, and epigastric pain and results also reported in a Cochrane systematic review.36 Future studies should exam this outcome so that researchers can objectively evaluate and select interventions.
QOL is a key factor to evaluate effectiveness and safety of interventions.6 Kim et al found that moxibustion statistically improved the PF, BP, and SF relative to usual care, and the same favorable effect of moxibustion on QoL was also detected compared to sham moxibustion. However, we found that in Kim's study,10 outcome assessor was not blinded and the ITT method was also not used. Meanwhile, Ren et al's6 did not perform the ITT method. Hence, RCTs with rigorous design are required to further investigate the effects of moxibustion on QoL.
More accurate pooled results were generated from our study due to comprehensive literature search and critical appraisals of studies were performed. However, we must acknowledge some limitations, which may impair the power of our findings. First, we just searched PubMed, Embase, CENTRAL, and CBM. More potential studies might be captured if search was expanded. Second, 4 RCTs with high risk were included to calculate summarized estimates, and thus some findings in our study may be exaggerated. Third, we did not investigate the effects of various active moxibustion treatments on KOA and also did not perform subgroup analysis according to various moxibustion treatments. This may also negatively affect our findings. Fourth, the various oral drugs with different pharmacological functions were used in control groups; however we did not perform subgroup analysis due to the inadequate number of eligible studies. Various control oral drugs will play a contributor to heterogeneity and further the power of our pooled results. Fifth, the participants enrolled each eligible trial were small and thus small sample size effects may be generated. The power of our review based on small sample size effects may be exaggerated. Sixth, all eligible selected treatment acupoints to perform moxibustion; however, we did not design subgroup analysis according to different acupoints which may generate different treatment effects, and thus our result has increased risk of exaggerating effects. Finally, our study did not perform the publication bias test owing to the insufficient number of eligible studies on each outcome. So robustness of our findings may be impaired if publication bias existed.
CONCLUSION
For the treatment of KOA, moxibustion is superior to usual care and sham moxibustion, but the effects of moxibustion on target population are nearly equal to oral drug and intra-articular injection. Consequently, we concluded that moxibustion is an alternative of treating KOA; however more studies with well-designed are warranted in order to further determine the effect of moxibustion on QoL.
Supplementary Material
Acknowledgments
The authors would like to appreciate the editor and all staff working in editorial office of Medicine. They also appreciate all anonymous referees who spent their golden time to review our manuscript.
Footnotes
Abbreviations: ACR = American College of Rheumatology, AEs = adverse events, CBM = Chinese Biomedical Literature database, CDTEDS-TCM = Criteria of Diagnosis and Therapeutic Effect of Diseases and Syndromes in TCM, CENTRAL = Cochrane Central Register of Controlled Trials, CIs = confidence intervals, CRC = colorectal cancer, GDTO-CMAR = Guidelines for diagnosis and treatment of osteoarthritis of the Chinese Medical Association of Rheumatology, GPCRND = guiding principles of clinical research on new drugs, ITT = intention-to-treat, KOA = knee osteoarthritis, NRS = numerical rating scale, PRISMA = Preferred Reporting Items for Systematic Review and Meta-analysis, QoL = quality of life, RCTs = randomized controlled trials, RR = relative risk, SMD = standardized mean difference, VAS = visual analog scale, WOMAC = Western Ontario and McMaster Universities Questionnaire.
G-MS, XT, and Y-HJ contributed equally to this study.
Contributors—conceived and designed the protocol: G-MS and XT; searched potential citations: G-MS and XT; selected studies and collected information: G-MS and X-LP; assessed the methodological quality: JGZ and Y-HD; performed the meta-analyses: G-MS and HZ; prepared and reported manuscript: G-MS and XT; checked the manuscript and authorship: all authors.
Disclosure: all authors have read the whole manuscript and approved the authorship and current version to be considered for publication in Medicine®.
The authors have no funding and conflicts of interest to disclose.
REFERENCES
- 1.Felson DT, Lawrence RC, Dieppe PA, et al. Osteoarthritis: new insights. Part 1: the disease and its risk factors. Ann Intern Med 2000; 133:635–646. [DOI] [PubMed] [Google Scholar]
- 2.Dawson J, Linsell L, Zondervan K, et al. Impact of persistent hip or knee pain on overall health status in elderly people: a longitudinal population study. Arthrit Rheum-Arthr 2005; 53:368–374. [DOI] [PubMed] [Google Scholar]
- 3.Palmer KT, Reading I, Calnan M, et al. Does knee pain in the community behave like a regional pain syndrome? Prospective cohort study of incidence and persistence. Ann Rheum Dis 2007; 66:1190–1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Heidari B. Knee osteoarthritis prevalence, risk factors, pathogenesis and features: part I. Caspian J Intern Med 2011; 2:205–212. [PMC free article] [PubMed] [Google Scholar]
- 5.Ren XM, Cao JJ, Shen XY, et al. Knee osteoarthritis treated with moxibustion: a randomized controlled trial. Zhongguo zhen jiu = Chin Acupunct Moxibustion 2011; 31:1057–1061. [PubMed] [Google Scholar]
- 6.Ren X, Yao C, Wu F, et al. Effectiveness of moxibustion treatment in quality of life in patients with knee osteoarthritis: a randomized, double-blinded, placebo-controlled trial. Evidence-based Complementary Alternative Med: eCAM 2015; 2015:569523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang W, Moskowitz RW, Nuki G, et al. OARSI recommendations for the management of hip and knee osteoarthritis, Part II: OARSI evidence-based, expert consensus guidelines. Osteoarthritis Cartilage 2008; 16:137–162. [DOI] [PubMed] [Google Scholar]
- 8.Zhao L, Cheng K, Wang L, et al. Effectiveness of moxibustion treatment as adjunctive therapy in osteoarthritis of the knee: a randomized, double-blinded, placebo-controlled clinical trial. Arthritis Res Tther 2014; 16:R133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen R, Chen M, Su T, et al. Heat-sensitive moxibustion in patients with osteoarthritis of the knee: a three-armed multicentre randomised active control trial. Acupunct Med 2015; 33:262–269. [DOI] [PubMed] [Google Scholar]
- 10.Kim TH, Kim KH, Kang JW, et al. Moxibustion treatment for knee osteoarthritis: a multi-centre, non-blinded, randomised controlled trial on the effectiveness and safety of the moxibustion treatment versus usual care in knee osteoarthritis patients. PLoS One 2014; 9:e101973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Deng H, Shen X. The mechanism of moxibustion: ancient theory and modern research. Evidence-Based Complementary Alternative Med 2013; 2013:379291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sun K, Yang J, Shen DK. Clinical observation on treatment of primary knee osteoarthritis of liver and kidney deficiency type with Aconite cake-separated moxibustion. Zhongguo zhen jiu = Chin Acupunct Moxibustion 2008; 28:87–90. [PubMed] [Google Scholar]
- 13.Zhao L, Cheng K, Wang LZ, et al. Effectiveness of moxibustion treatment as adjunctive therapy in osteoarthritis of the knee: a randomized, double-blinded, placebo-controlled clinical trial. Arthritis Res Ther 2014; 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cheng HL, Han W, Hu PJ, et al. Clinical study of differential selection of objects separated moxibustion for treatment of knee osteoarthritis. Clin J Tradit Chin Med 2008; 20:114–116.[Chinese]. [Google Scholar]
- 15.Ren XM, Song SL, Shi Y. Observations on the therapeutic effect of herbal cake-separated moderate moxibustion on knee osteoarthritis of 50 cases. Zhejiang J Tradit Chin Med 2010; 45:759.[Chinese]. [Google Scholar]
- 16.Sun K, Yang YH, Zhou ZL. Clinical observations on the treatment of primary genual osteoarthritis of liver-kidney depletion type by aconite cake-separated moxibustion. Shanghai J Acup Moxi 2008; 27:9–10.[Chinese]. [Google Scholar]
- 17.Yang YH, Sun K, Su GH, et al. Clinical study panax notoginsengs cake separated moxibustion treatment of qi stagnation blood stasis type for primary knee osteoarthritis. Clin J Tradit Chin Med 2008; 20:53–55.[Chinese]. [Google Scholar]
- 18.Choi TY, Choi J, Kim KH, et al. Moxibustion for the treatment of osteoarthritis: a systematic review and meta-analysis. Rheumatol Int 2012; 32:2969–2978. [DOI] [PubMed] [Google Scholar]
- 19.Higgins JPT, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration; 2008. Available from http://www.Chochrane-handbook.Org. [Google Scholar]
- 20.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 2009; 151:264–269.W264. [DOI] [PubMed] [Google Scholar]
- 21.Davidson MB, Castellanos M, Kain D, et al. The effect of self monitoring of blood glucose concentrations on glycated hemoglobin levels in diabetic patients not taking insulin: a blinded, randomized trial. Am J Med 2005; 118:422–425. [DOI] [PubMed] [Google Scholar]
- 22.Wu F, Xiong P. Moxibustion on heat-sensitive acupoints in the treatment of KOA (Swelling Type). J Clin Acup Moxi 2011; 27:1–4.[Chinese]. [Google Scholar]
- 23.Zhang QJ, Cao LH, Li ZD, et al. The clinical effects and safety of moxibustion and celecoxib for obteoarthritis of knee. Chin J Tradit Med Trauma Orthop 2011; 19:13–15.[Chinese]. [Google Scholar]
- 24.Zhou YL, Li J, Hou WG, et al. Clinical observation of moxibustion in treatment of knee osteoarthritis. Shanghai J Acup Moxi 2014; 33:1086–1087.[Chinese]. [Google Scholar]
- 25.Zhou ZL, Sun K, Cheng HL, et al. Observations on the therapeutic effect of herbal cake-separated moxibustion on knee osteoarthritis of blood stasis type. Shanghai J Acup Moxi 2010; 29:45–47.[Chinese]. [Google Scholar]
- 26.Peat G, McCarney R, Croft P. Knee pain and osteoarthritis in older adults: a review of community burden and current use of primary health care. Ann Rheumatic Dis 2001; 60:91–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Xiang YJ, Dai SM. Prevalence of rheumatic diseases and disability in China. Rheumatol Int 2009; 29:481–490. [DOI] [PubMed] [Google Scholar]
- 28.Xu MF, Xiao XH, Yu Q. Observations on the efficacies of moxibustion plus drug injection in treating knee osteoarthritis. Shanghai J Acup Moxi 2011; 30:318–320.[Chinese]. [Google Scholar]
- 29.Zheng SG, Chen B, Ma SB, et al. Regulative effect of moxibustion on experimental knee osteoarthritis in rabbit. J Beijing Univ Trad Chin Med 2008; 31:358–360.[Chinese]. [Google Scholar]
- 30.Huang XY, Lin YK, Lu JD, et al. Effect of moxibustion at Zusanli (ST36) and Shensu (BL23) PGE2, NO and IL-1 ( in osteoarthritis rat model. Prog Vete Med 2014; 35:75–78.[Chinese]. [Google Scholar]
- 31.Xiong Y, Peng R, Xia SS. Effect of moxibustion on the expressions of interleukin-1 beta and tumor necrosis factor alpha in joint synovial fluid of rabbits with knee osteoarthritis. J Clin Reha Tiss Engi Res 2010; 14:7700–7703.[Chinese]. [Google Scholar]
- 32.Chen B, Xie XM, Li JL. Effects of moxibustion on cartilage injury, expression of TNF-(, TGF-(1 and IGF-1 in knee osteoarthritis rabbit model: an experimental study. Jiangsu J Trad Chin Med 2009; 41:69–71.[Chinese]. [Google Scholar]
- 33.Wu YL, Ma XX, Liu D, et al. Effects of the Hui nationality megical of Zhen Shamazhunjiu on cartilage MMP-1, MMP-13 level in the knee osteoarthritis of rabbits. Ningxia Med J 2015; 37:595–598.[Chinese]. [Google Scholar]
- 34.CHen B, Zheng SG, Ma SB. Eeffcts of moxibustion on cartilage injury, expression of MMP-1 and TIMP-1 in knee osteoarthritis rabbit model: an experimental study. Shanxi J Trad Chin Med 2009; 30:502–504.[Chinese]. [Google Scholar]
- 35.Wang S, Shen L, Xiao L. Effect of moxibustion therapy on articular chondrocyte apoptosis of osteoarthritis rabbits. Chin J Clin Rehab 2006; 10:55–58.[Chinese]. [Google Scholar]
- 36.Towheed TE, Maxwell L, Judd MG, et al. Acetaminophen for osteoarthritis. Cochrane Database Syst Rev 2006; CD004257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Qu Y, Zeng R, Liu Y. General situation of the studies of Chinese mugwort (artemisia argyi) leaves. J Southwest Univ Nation (Natural Sci Edition) 2005; 31:254–256.[Chinese]. [Google Scholar]
- 38.Park JE, Lee SS, Lee MS, et al. Adverse events of moxibustion: a systematic review. Complement Ther Med 2010; 18:215–223. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


