Abstract
Cervical intradural disc herniation (IDH) is an extremely rare condition, comprising only 0.27% of all disc herniations. Three percent of IDHs occur in the cervical, 5% in the thoracic, and over 92% in the lumbar spinal canal. There have been a total of 31 cervical IDHs reported in the literature. The pathogenesis and imaging characteristics of IDH are not fully understood. A preoperative diagnosis is key to facilitating prompt intradural exploration in patients with ambivalent findings, as well as in preventing reoperation. The purpose of reporting our case is to remind clinicians to consider the possibility of cervical IDH during spinal manipulation therapy in patient with chronic neck pain.
The patient signed informed consent for publication of this case report and any accompanying image. The ethical approval of this study was waived by the ethics committee of Chonbuk National University Hospital, because this study was case report and the number of patients was <3.
A 32-year-old man was transferred our emergency department with progressive quadriparesis. He had no history of trauma, but had received physical therapy with spinal manipulation for chronic neck pain over the course of a month. The day prior, he had noticed neck pain and tingling in the bilateral upper and lower extremities during the manipulation procedure. The following day, he presented with bilateral weakness of all 4 extremities, which rendered him unable to walk. Neurological examination demonstrated a positive Hoffmann sign and ankle clonus bilaterally, hypoesthesia below the C5 dermatome, 3/5 strength in the bilateral upper extremities, and 2/5 strength in the lower extremities. This motor weakness was progressive, and he further complained of voiding difficulty.
Urgent magnetic resonance imaging (MRI) of the cervical spine revealed large, central disc herniations at C4–C5 and C5–C6 that caused severe spinal cord compression and surrounding edema. We performed C4–C5–C6 anterior cervical discectomy and fusion.
The patient's limb weakness improved rapidly within 1 day postoperatively, and he was discharged 4 weeks later. At his 12-month follow-up, the patient had recovered nearly full muscle power.
We presented an extremely rare case of cervical IDH causing progressive quadriparesis after excessive spinal manipulation therapy. The presence of a “halo” and “Y-sign” were useful MRI markers for cervical IDH in this case.
INTRODUCTION
Intradural disc herniation (IDH) is an extremely rare condition, comprising only 0.27% of all disc herniations and there have been a total of 31 cervical IDHs reported in the literature.1–4 Because the pathogenesis and imaging characteristics of IDH are not fully understood, a preoperative diagnosis is key to facilitating prompt intradural exploration in patients with ambivalent findings, as well as in preventing reoperation.5 We provide 1 additional case report, along with a brief review of the literature.
CASE REPORT
A 32-year-old man was transferred our emergency department with rapidly progressive quadriparesis. He had no history of trauma, but had received physical therapy with spinal manipulation for chronic neck pain over the course of a month. The day prior, he had noticed neck pain and tingling in the bilateral upper and lower extremities during the manipulation procedure. The following day, he presented with bilateral weakness of all 4 extremities, which rendered him unable to walk. Neurological examination demonstrated a positive Hoffmann sign and ankle clonus bilaterally at that time, although these reflexes were not checked before. He complained hypoesthesia below the C5 dermatome, 3/5 strength in the bilateral upper extremities, and 2/5 strength in the lower extremities. This motor weakness was progressive, and he further complained of voiding difficulty.
Urgent magnetic resonance imaging (MRI) of the cervical spine revealed large, central disc herniations at C4–C5 and C5–C6 with severe spinal cord compression and surrounding edema (Figure 1). Furthermore, an area of increased intensity was seen in the spinal cord at C5–C6. The patient underwent anterior cervical discectomy and fusion at the C4/5/6 level. A large sequestrated disc had perforated through the posterior longitudinal ligament (PLL) into the intradural space, with an adhesion to the dura and PLL. We removed the extruded disc material, along with a small, longitudinal defect in the PLL and dura, under microscopic guidance. The dural tear was closed with Tachocomb, and an interbody cage filled with allograft and an anterior cervical plate was placed at C4/5/6. The patient's limb weakness improved rapidly within 1 day postoperatively, and he was discharged 4 weeks later. MRI taken 3 weeks postoperatively showed high signal intensity in the spinal cord at C4–C5 and C5–C6, as well as adhesions of the spinal cord to the PLL (Figure 2). At his 12-month follow-up, the patient had recovered nearly full muscle power.
FIGURE 1.
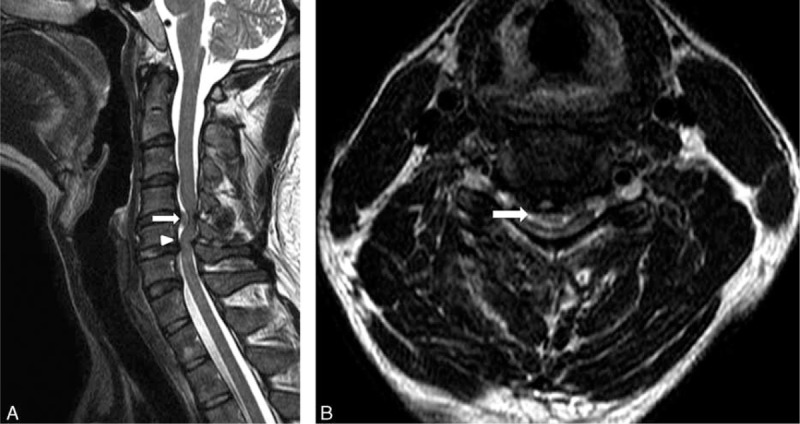
Preoperative MRI. (A) Sagittal T2-weighted image of the cervical spine revealed large disc herniation at C4–C5 (arrow) and C5–C6 with severe spinal cord compression. The “Y-sign” (arrow head) was found. (B) Axial T2-weighted image of the cervical spine revealed large, central disc herniation at C4–C5 with severe spinal cord compression and surrounding edema. A “halo” of CSF isointensity surrounding the herniated disc was also demonstrated (arrow). CSF = cerebrospinal fluid, MRI = magnetic resonance imaging.
FIGURE 2.
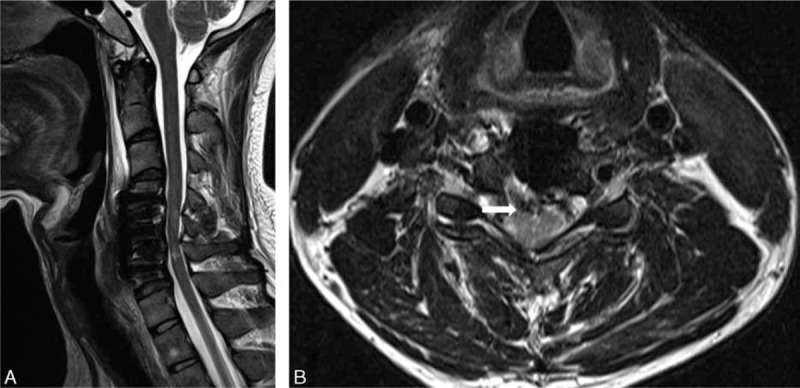
MRI taken 3 weeks postoperatively showed high signal intensity in the spinal cord at C4–C5 and C5–C6 (A), as well as adhesions of the spinal cord to the PLL (arrow) (B). MRI = magnetic resonance imaging, PLL = posterior longitudinal ligament.
DISCUSSION
Since Marega6 reported the first case of intradural cervical disc rupture, 31 cases of this rare condition have since occurred in the literature. In our review of these 32 cases, including our new case, we found a male predominance (19 of 32 cases) in IDH incidence, and the mean age at presentation was 45.2 years. The lower cervical spine, a site of increased spinal mobility, was the most frequently affected, particularly at C5–C6 and C6–C7.2 The most common clinical manifestations of cervical IDH were Brown–Sequard syndrome, transverse myelopathy, and rarely radiculopathy.4 In our new case, the patient presented with rapidly progressive quadriparesis after spinal manipulation therapy.
Pathogenesis of Cervical IDH
The mechanism of cervical IDH remains unclear. Trauma has been considered the most important inciting factor in previous studies,2,7 suggesting that traumatic injury may cause chronic adhesions between the ligaments and dura; indeed, these adhesions were found intraoperatively in most cervical IDH cases. In our patient, disc protrusion and repeated spinal manipulation caused chronic inflammation and mechanical irritation of the adjacent dura, creating adhesions between the PLL and the dura. We posit that the spinal manipulation procedures caused transdural disc herniation that compressed the spinal cord. Furthermore, we found evidence of adhesions between the dura and PLL in our patient intraoperatively.
Yildizhan et al8 performed a cadaveric study that found the dura to be firmly attached to the PLL in some cases. They hypothesized that congenital factors may have a role in the pathogenesis of cervical disc herniation.
Some authors have reported cases of cervical IDH in patients with ossification of PLL.9,10 They suggested that PLL hypertrophy and ossification can cause chronic mechanical irritation to the dura, particularly if it is already congenitally attached to the ligament.
MRI Findings in Cervical IDH
Because it is difficult to identify dural sac perforation on MRI, there have been few reports on the imaging features of IDH. In 1998, Hidalgo-Ovejero et al11 suggested that the presence of epidural gas on computed tomography could be an indicator. Choi et al5 designated an abrupt discontinuity in the PLL “hawk-beak sign” on MRI. Recently, Borm et al12 described a “Halo” of cerebrospinal fluid (CSF) isointensity surrounding a herniated mass on sagittal T2-weighted imaging that could indicate intradural extension into the cervical spine. Similarly, Sasaji et al13 described a “Y-sign” in the lumbar spine. Because intradural extra-arachnoid disc herniation occurs between the dura and arachnoid, the arachnoid was peeled from the dura by the disc herniation. One line of the dura and arachnoid was divided into 2 lines of the dura and the arachnoid. The branch of the ventral dural lines appeared as “Y,” and they called it the “Y sign.” In our case, a “halo” of CSF isointensity surrounding the herniated disc was demonstrated in axial MR images (Figure 1B), and the “Y-sign” was found in sagittal MR images (Figure 1A). We found that the CSF isointensity around the herniated area appeared not only as a “halo” in axial images, but also as “Y-sign” on sagittal images. We therefore suggest that both the “halo” and “Y-sign” are strong indicators of IDH on MRI.
Surgical Treatment of Cervical IDH
Surgical intervention is the definitive treatment for cervical IDH, and all patients in the literature underwent surgery. According to previous reports, anterior cervical discectomy and fusion is superior to posterior decompression in terms of operative procedure and outcome.1,10,14 Since the anterior approach directly accesses the affected disc, it facilitates removal of extruded disc material and dura repair.
CONCLUSION
We presented an extremely rare case of cervical IDH causing progressive quadriparesis after excessive spinal manipulation therapy. The presence of a “halo” and “Y-sign” were useful MRI markers for cervical IDH in this case.
Footnotes
Abbreviations: CSF = cerebrospinal fluid, CT = computed tomography, IDH = intradural disc herniation, MRI = magnetic resonance imaging, PLL = posterior longitudinal ligament.
The authors have no funding and conflicts of interest to disclose.
REFERENCES
- 1.Epstein NE, Syrquin MS, Epstein JA, et al. Intradural disc herniations in the cervical, thoracic, and lumbar spine: report of three cases and review of the literature. J Spinal Disord 1990; 3:396–403. [PubMed] [Google Scholar]
- 2.Pan J, Li L, Qian L, et al. Intradural cervical disc herniation: report of two cases and review of the literature. Spine 2011; 36:E1033–E1037. [DOI] [PubMed] [Google Scholar]
- 3.Kansal R, Mahore A, Kukreja S. Cervical intradural disc herniation and cerebrospinal fluid leak. Neurol India 2011; 59:447–450. [DOI] [PubMed] [Google Scholar]
- 4.Warade AG, Misra BK. Spontaneous cervical intradural disc herniation. J Clin Neurosci 2014; 21:872–873. [DOI] [PubMed] [Google Scholar]
- 5.Choi JY, Lee WS, Sung KH. Intradural lumbar disc herniation—is it predictable preoperatively? A report of two cases. Spine J 2007; 7:111–117. [DOI] [PubMed] [Google Scholar]
- 6.Marega T. Ernia del disco cervicale espulsa nel sacco durale. Arch Putti Chir Organi Mov 1959; 12:425–430. [PubMed] [Google Scholar]
- 7.Eisenberg RA, Bremer AM, Northup HM. Intradural herniated cervical disk—a case-report and review of the literature. Am J Neuroradiol 1986; 7:492–494. [PMC free article] [PubMed] [Google Scholar]
- 8.Yildizhan A, Pasaoglu A, Okten T, et al. Intradural disc herniations pathogenesis, clinical picture, diagnosis and treatment. Acta Neurochir 1991; 110:160–165. [DOI] [PubMed] [Google Scholar]
- 9.Iwamura Y, Onari K, Kondo S, et al. Cervical intradural disc herniation. Spine 2001; 26:698–702. [DOI] [PubMed] [Google Scholar]
- 10.Wang D, Wang H, Shen WJ. Spontaneous cervical intradural disc herniation associated with ossification of posterior longitudinal ligament. Case Rep Orthop 2014; 2014:256207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hidalgo-Ovejero AM, Garcia-Mata S, Izco-Cabezon T, et al. Intradural disc herniation associated with epidural gas. Spine 1998; 23:281–283. [DOI] [PubMed] [Google Scholar]
- 12.Borm W, Bohnstedt T. Intradural cervical disc herniation. Case report and review of the literature. J Neurosurg 2000; 92 (Suppl):221–224. [PubMed] [Google Scholar]
- 13.Sasaji T, Horaguchi K, Yamada N, et al. The specific sagittal magnetic resonance imaging of intradural extra-arachnoid lumbar disc herniation. Case Rep Med 2012; 2012:383451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee JK, Kim YS, Kim SH. Brown–Sequard syndrome produced by cervical disc herniation with complete neurologic recovery: report of three cases and review of the literature. Spinal Cord 2007; 45:744–748. [DOI] [PubMed] [Google Scholar]


