Abstract
Metabolic acidosis could emerge from diseases disrupting acid-base equilibrium or from drugs that induce similar derangements. Occurrences are usually accompanied by comorbid conditions of drug-induced metabolic acidosis, and clinical outcomes may range from mild to fatal. It is imperative that clinicians not only are fully aware of the list of drugs that may lead to metabolic acidosis but also understand the underlying pathogenic mechanisms. In this review, we categorized drug-induced metabolic acidosis in terms of pathophysiological mechanisms, as well as individual drugs’ characteristics.
Keywords: metabolic, acidosis, drug-induced, MALA
Introduction
Metabolic acidosis is defined as an excessive accumulation of non-volatile acid manifested as a primary reduction in serum bicarbonate concentration in the body associated with low plasma pH. Certain conditions may exist with other acid-base disorders such as metabolic alkalosis and respiratory acidosis/alkalosis 1.
Humans possess homeostatic mechanisms that maintain acid-base balance ( Figure 1). One utilizes both bicarbonate and non-bicarbonate buffers in both the intracellular and the extracellular milieu in the immediate defense against volatile (mainly CO 2) and non-volatile (organic and inorganic) acids before excretion by the lungs and kidneys, respectively. Renal excretion of non-volatile acid is the definitive solution after temporary buffering. This is an intricate and highly efficient homeostatic system. Derangements in over-production, under-excretion, or both can potentially lead to accumulation of excess acid resulting in metabolic acidosis ( Figure 1).
Figure 1. Excretion of acid and ways to jeopardize the system.
1. A strong non-volatile acid HA dissociates to release H + and poses an immediate threat to plasma pH.
2. Bicarbonate buffers the H + and generates CO 2, which is expelled in the lungs and results in depletion of body HCO 3 -. Non-bicarbonate buffers (collectively referred to as B) carry the H + until the kidneys excrete it.
3. The kidneys split CO 2 into H + and HCO 3 - and selectively secrete H + into the lumen and HCO 3 - into the blood. In addition, any excess H + from the body fluid is also excreted.
4. Most H + excreted in the urine is carried by urinary buffers (UBs).
5. Some organic anions (A) (e.g. lactate, ketoanions) can be metabolized to regenerate the HCO 3 -. If A is not metabolizable (e.g. phosphate or sulfate), it is excreted in the urine.
* Two possible ways by which metabolic acidosis can occur.
Drug-induced metabolic acidosis is often mild, but in rare cases it can be severe or even fatal. Not only should physicians be keenly aware of this potential iatrogenic complication but they should also be fully engaged in understanding the pathophysiological mechanisms. Metabolic acidosis resulting from drugs and/or ingestion of toxic chemicals can be grouped into four general categories ( Figure 2):
Figure 2. Mechanisms of drug-induced metabolic acidosis.
1. Increased exogenous ingestion of acidic precursors that are converted into strong acids.
2. Loss of alkali from kidney or GI tract.
3. Increased endogenous production of strong organic acids.
4. Compromised renal net acid excretion by inhibition of the renin-angiotensin-aldosterone system (RAAS), impaired proximal tubule (PT), or distal tubule (DT) H + secretion.
-
1.
Drugs as exogenous acid loads
-
2.
Drugs leading to loss of bicarbonate in the gastrointestinal (GI) tract or kidney
-
3.
Drugs causing increased endogenous acid production
-
4.
Drugs that decrease renal acid excretion
Some medications cannot be placed into one single category, as they possess multiple mechanisms that can cause metabolic acidosis.
In suspected drug-induced metabolic acidosis, clinicians should establish the biochemical diagnosis of metabolic acidosis along with the evaluation of respiratory compensation and whether there is presence of mixed acid-based disorders 2, then convert the biochemical diagnosis into a clinical diagnosis with identification of the invading acid/drug 3. Next is to review the list of medications by history and record to determine whether any of the drugs are culprits in either the generation or the exacerbation of the disorder. Note that just because a patient has, for example, lactic acidosis and is on a drug that can potentially cause lactic acidosis does not mean that the two are causally related. Finally, if a drug is indeed causing some degree of metabolic acidosis, the clinician should make an appraisal of the benefits from the drug weighed against the severity of the metabolic complication to determine whether cessation of therapy is justified. For example, if a patient with problematic seizures is effectively controlled by topiramate, a mild degree of metabolic acidosis can be more tolerable than seizures.
Drugs resulting in exogenous acid precursors
Non-pharmaceutical agents: toxic alcohols, phenols, and ammonium chloride
Methanol 4, ethylene glycol 5, diethylene glycol 6, and isopropanol 7 are volatile alcohols that produce a high plasma osmolar gap (the alcohol itself and the aldehyde metabolite), pure high anion gap metabolic acidosis from their metabolism into strong carboxylic acids such as formic acid (from methanol), and a combination of oxalic, glyoxylic, and glycolic acid (from ethylene/diethylene glycol). Isopropanol alcohol, due to the absence of an alpha-carbon, could only be metabolized to a keto- group and contributes to an osmolar gap but not high anion gap metabolic acidosis in poisoning encounters. Toluene abuse with glue or paint thinner sniffing can cause hippuric metabolic acidosis that presents with a normal plasma anion gap but elevated urinary osmolar gap because of the rapid clearance of hippurate 8. Note that the time at which blood is sampled may reveal variable osmolar and anion gap. When the hydroxyl group is metabolized to carboxyl with a low pKa, there will not be an osmolar gap due to the contemporaneous consumption of bicarbonate; however, the metabolite between hydroxyl and carboxyl is an aldehyde, which still contributes to an osmolar gap but not an anion gap.
Ammonium chloride is not usually abused but is used extensively by investigators to study overproduction acidosis and used outside the laboratory 9. There is a rise in acid excretion and a fall in serum HCO 3 - concentration that remains constant after initial drop 10, 11.
Overproduction acidosis from pharmaceutical agents
The excessive use of amino acids with a net positive charge would result in liberation of H + during metabolism (arginine and lysine) in parenteral alimentation with inadequate concomitant administration of alkali 12. Another example in this category is propylene glycol (1,2-propanediol [PG]), a common hygroscopic and emulsifying agent that is metabolized to lactate 13. The U.S. Food and Drug Administration classified PG as GRAS (generally recognized as safe). The recommended maximum daily intake of PG should be less than 25 mg/kg/day (equivalent to 21 mmol/day for a 70 kg person) 14. Each drug injection may have very different amounts of PG. Clinically significant toxicity is seen only in rapid, massive, and protracted parenteral administration of high quantities, especially in patients with renal impairment. PG intoxication from intravenous vitamin therapy was reported in pediatric patients who developed stupor 15. Intoxication with lactic acidosis and hyperosmolality were found during treatment of schizophrenia 16, with the use of intravenous benzodiazepines 13, 17, etomidate 18, nitroglycerin 19, and barbiturates 20, all with PG as a vehicle. Approximately 55% of PG undergoes oxidation to propionaldehyde and pyruvic, acetic, and lactic acid, while the remainder is excreted unchanged in the urine 21, 22. Some studies have demonstrated PG-injured proximal tubular cells, leading to impaired renal acidification 20, 23. Patients with hepatic dysfunction, renal insufficiency, and diabetic ketoacidosis are more susceptible to PG toxicity and development of lactic acidosis 24.
Drugs causing external base loss
Renal loss of bicarbonate
Carbonic anhydrases (CAs) are critical enzymes for bicarbonate reabsorption. Acetazolamide is a commonly used CA inhibitor in the treatment of ocular and convulsive disorders. It causes bicarbonaturia and a mild degree of hyperchloremic metabolic acidosis 25. There have also been reports of symptomatic anion gap metabolic acidosis associated with acetazolamide therapy in elderly patients 26 and in those with impaired renal function 26, 27 and diabetes mellitus 28. Severe metabolic acidosis may result from inhibition of pyruvate carboxylase and mitochondrial damage 29. Ocular solution of CA inhibitor-induced acidosis is rare but has been reported 30.
Topiramate is approved for the treatment of seizure, as a migraine headache prophylaxis, and for weight loss, with off-label use for bipolar disorder, obesity, neuropathic pain, and smoking cessation 31. It inhibits CA II, IV, and XII 31. Topiramate generates a mild hyperchloremic metabolic acidosis 32, 33 but increases urinary pH and drastically lowers urinary citrate excretion, thus increasing the risk for calcium phosphate urolithiasis 34, 35.
The sulfonamide class of drugs also has CA inhibitory activity. Topical application and absorption over large areas in burn patients can cause extremely high blood levels and systemic CA inhibition 36. This results in more than mere renal bicarbonate loss but rather a systemic disequilibrium syndrome.
Gastrointestinal loss of bicarbonate
Cholestyramine is an oral agent for treating hypertriglyceridemia and cholestasis by binding and sequestering bile acids from the entero-hepatic circulation; the non-absorbable complexes are eventually excreted in the stool 37. In the GI tract, cholestyramine also binds phosphate, sulfate, and bicarbonate, leading to potential loss of bicarbonate from the body. Under normal conditions, this is easily corrected by renal regeneration of bicarbonate. However, patients with impaired renal function are at risk of hyperchloremic acidosis 37– 39.
Sevelamer hydrochloride is a non-reabsorbable phosphate binder. Dialysis patients on sevelamer hydrochloride have lower mean serum bicarbonate concentration during and at the end of therapy compared to those treated with calcium acetate 40, 41. The chloride released upon phosphate stimulates bicarbonate secretion by the gut via chloride-bicarbonate exchange 40. This secretion coupled with defective ability to regenerate bicarbonate in renal patients leads to hyperchloremic acidosis. This complication is avoided by using sevelamer carbonate, which binds phosphate and releases carbonate instead 42, or by bixalomer, which contains no chloride, and seems to demonstrate equal efficacy of phosphate binding with no evidence of acidosis in clinical trials 43, 44. Laxative abuse, calcium chloride, and magnesium sulfate could also cause hyperchloremic acidosis because the secreted bicarbonate from the pancreas is trapped by calcium and magnesium 45– 47 and then excreted in stools.
Drugs causing increased endogenous acid production
Lactic acidosis
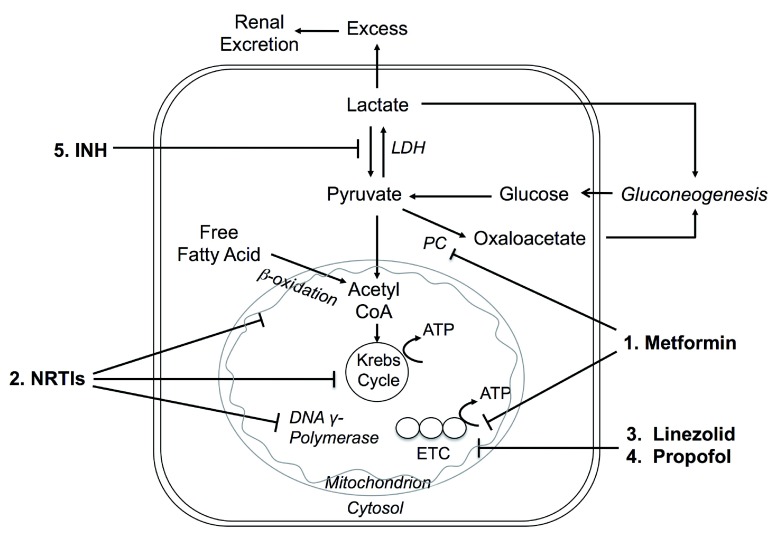
Lactic acid is produced under basal metabolic conditions and H + ions are released. Normally, an equivalent amount of H + ions is consumed when the liver and renal cortex utilize lactate for gluconeogenesis or oxidize it to water and CO 2 so that acid-base balance remains undisturbed ( Figure 3). Lactic acidosis is arbitrarily classified into overproduction of lactate (type A), underutilization of lactate (type B), or both 48. Type A lactic acidosis is associated with generalized or regional tissue hypoxia, while type B is seen in patients with metabolic abnormalities in malignancy, hepatic dysfunction, diabetes mellitus, congenital enzymatic deficiency, and drugs or toxins 45, 49. In 1995, metformin replaced phenformin, a notorious inducer of lactic acidosis, and became the primary biguanide used today 50. Post marketing safety surveillance revealed no cases of fatal lactic acidosis 51. There are still reports of metformin-associated lactic acidosis (MALA) 52, 53 with proposed mechanisms shown in Figure 3.
Figure 3. Mechanisms of drug-induced lactic acidosis.
1. Metformin inhibits pyruvate carboxylase (PC) → inhibits hepatic gluconeogenesis 146 → excess lactate 84. Metformin also inhibits complex I of the mitochondrial electron transport chain (ETC) 84 → increases NADH/NAD + ratio → blocks the entry of pyruvate into the tricarboxylic acid (TCA) cycle 147. LDH = lactate dehydrogenase
2. In vitro, nucleoside reverse transcriptase inhibitors (NRTIs) inhibit β-oxidation, the tricarboxylic acid (Krebs) cycle, and DNA γ-polymerase → mitochondrial dysfunction and loss of transcription of essential enzymes → hepatic steatosis (increased triglycerides), myopathy, pancreatitis, nephrotoxicity, and lactic acidosis 68.
3. Linezolid may cross-react with mammalian cellular processes → disrupts mitochondrial protein synthesis involved in ETC 75, 148.
4. Propofol may inhibit coenzyme Q and cytochrome C at Complex IV in ETC, and also inhibit mitochondrial fatty acid metabolism 88.
5. Isoniazid inhibits metabolism of lactate to pyruvate 82.
Most cases of MALA were associated with some underlying conditions such as acute renal failure induced by volume depletion, other potential nephrotoxic agents and concurrent use of radio-contrast media, or hepatic insufficiency 54– 58. Blood pH and lactate levels are not prognostic in MALA 59. Although the incidence of MALA is low, once developed, the mortality can be staggeringly high 52, particularly in the critical care setting, so discontinuation is advised in a patient with impending renal and multi-organ failure. Recently, a less restrictive guideline is proposed on metformin usage in patients of stable chronic kidney disease 60– 63. In general, the mortality of MALA decreased from 50% to 25% from the 1960s to the present 64.
Highly active antiretroviral therapy (HAART) has led to dramatic reductions in HIV-associated morbidity and mortality 65 ( Figure 3). However, lactic acidosis complicated this therapy, especially with the nucleoside and nucleotide reverse transcriptase inhibitor (NRTI)-based regimens: didanosine, stavudine, lamivudine, zidovudine, and abacavir 66– 71. Combined use of these drugs further increases the risk of lactic acidosis 72. Moreover, didanosine 73, cidofovir 74, lamivudine, and stavudine 75 could cause Fanconi syndrome with pan-proximal tubular dysfunction leading to exacerbation of the acidosis and reduction of the plasma anion gap. The mortality of HAART-induced lactic acidosis can be as high as 50% 76.
Linezolid is a long-term antibiotic against serious resistant Gram-positive organisms 77, 78 with adverse effects including bone marrow toxicity, optic/peripheral neuropathy, and lactic acidosis 77, 79, 80. Concurrent use of selective serotonin uptake inhibitors such as citalopram and sertraline may predispose patients to lactic acidosis 81, 82. The vast majority of lactic acidosis occurred in the elderly and those receiving prolonged treatment, and most resolved upon cessation of linezolid 80. Children receiving linezolid appeared to suffer lactic acidosis earlier during treatment 83 ( Figure 3).
Isoniazid is commonly used to treat tuberculosis 84. Dosing more than 300 mg/day can lead to refractory grand mal or localized seizure, coma, and lactic acidosis 84– 86. Some suggested acidosis stems from excessive muscle activity during refractory seizure 86, 87, and slow reversal was observed in the postictal period. One proposed mechanism is inhibition of conversion of lactate to pyruvate 84, 87– 89 ( Figure 3).
Propofol is commonly used for induction and maintenance of anesthesia, sedation, and interventional procedures. Two cases were reported on propofol-associated severe metabolic acidosis 90, 91. Risk factors include severe head injury, critical illness, prolonged administration (>48 hours) of large doses (>4 mg/kg/hour, equivalent to 1.6 mmol/hour for a 70 kg person), and inborn errors of fatty acid oxidation 90, 92 ( Figure 3).
Ketoacidosis
Ketosis develops when metabolism of fatty acid exceeds the removal of ketoacids (acetoacetic and β-hydroxybutyric). Typically there is insulin deficiency and/or resistance coupled with elevated glucagon and catecholamine. Glucose utilization is impaired and lipolysis is increased, augmenting the delivery of glycerol, alanine, and fatty acids for ketoacid generation 45, 93.
Overdose with salicylates in children commonly produces high anion gap acidosis, while adults exhibit a mixed respiratory alkalosis and metabolic acidosis. Metabolic acidosis occurs during salicylate toxicity due to uncoupling of oxidative phosphorylation and interfering with the Krebs cycle 45, 86, resulting in accumulation of lactic acid and ketoacids in as many as 40% of adult patients with salicylate poisoning 45, 94, 95. The anion gap is mainly composed of ketoanions and lactate, while salicylate anion seldom exceeds 3 mEq/L.
Alcoholic ketoacidosis occurs when ethanol is abused chronically in the setting of poor carbohydrate intake and volume contraction. Ketosis resolves when the ethanol intake is interrupted and the patient is provided with nutrients and fluid, which stimulates insulin secretion and promotes the regeneration of bicarbonate from the metabolism of ketoacid anions 45.
Pyroglutamic acidosis
The γ-glutamyl cycle produces glutathione, which is involved in the inactivation of free radicals, detoxification of many compounds, and amino acid transport 45, 96, 97. Acetaminophen can deplete glutathione, leading to increased formation of γ-glutamyl cysteine, which is converted and accumulated as pyroglutamic acid (5-oxoproline) 45, 97. Patients at risk include those with malnutrition, sepsis, alcohol abuse, underlying liver disease, and/or renal insufficiency 96. Acetaminophen ingestion alone may not cause pyroglutamic acidosis, but synergistic interaction between acetaminophen and the other factors as noted above 96 can. Concomitant use of other drugs such as aminoglycoside and β-lactam penicillin is reported to increase the risk 98.
Drugs causing decreased renal acid excretion
Syndromes of hyper-hypokalemia and reduced distal hydrogen secretion
Both angiotensin II and aldosterone are stimulators of the H +-ATPase α-intercalated cells in the cortical collecting tubule 99, 100, adding H + into the urinary luminal. Inhibition of the renin-angiotensin-aldosterone system (RAAS), which leads to secondary inhibition of the H +-ATPase, can lead to decreased H + secretion and metabolic acidosis. Additionally, inhibition of the RAAS reduces Na + reabsorption, which reduces the luminal electronegativity and reduces H + excretion by the H +-ATPase 100. The same mechanisms can cause hyperkalemia, which can in turn reduce stimulation of the H +/K +-ATPase 101. Hyperkalemia suppresses ammoniagenesis in the proximal tubule, impairs NH 4 + transport in the medullary thick ascending limb, and reduces medullary interstitial ammonium concentration, all of which can lower urine acid excretion 45, 102. Therefore, any drug that affects the RAAS or causes hyperkalemia can increase the risk of metabolic acidosis. These drugs include the following ( Figure 4):
Figure 4. Mechanisms of drug-induced distal H + secretion.
1. Cyclooxygenase (COX) inhibitors and β-blockers interfere with release of renin, leading to hyperkalemia with metabolic acidosis 43, 101.
2. Angiotensin-converting enzyme inhibitors (ACEIs), aldosterone receptor blockers (ARBs), and renin inhibitors all interfere with the renin-angiotensin-aldosterone system (RAAS), causing hyperkalemia with hyperchloremic metabolic acidosis 102– 104.
3. Heparin 105 and ketoconazole 106, 107 interfere with aldosterone synthesis.
4. Spironolactone and eplerenone block aldosterone receptors 43, 108.
5. Na + channel blockers lead to reduced net negative charge in lumen in cortical collecting ducts (CCD), which reduces K + and H + excretion and causes hyperkalemia and acidosis 43, 108– 111.
6. Calcineurin inhibitors interfere with Na, K-ATPase in the principal cell decreasing transepithelial K secretion and H + secretion, cause vasoconstriction of afferent glomerular arterioles, and decrease glomerular filtration rate and alter filtration fraction 112, 113.
7. Lithium causes a voltage-dependent defect for H + secretion and decreases H +-ATPase activity 114– 116.
8. Amphotericin B binds to sterol in mammalian cell membranes 106, 107 forming intramembranous pores which increase permeability and back diffusion of H +.
- -
- -
-
-
Angiotensin-converting enzyme inhibitors (ACEIs), angiotensin II receptor blockers (ARBs), and direct renin inhibitors 104– 106
- -
- -
-
-
Potassium-sparing diuretics: amiloride and triamterene 45, 110
- -
-
-
Calcineurin inhibitors: cyclosporine and tacrolimus 114, 115
When these drugs are administered in combination, there is increased risk for hyperkalemia and metabolic acidosis, especially in patients with diabetes, chronic kidney disease, and liver disease 45.
In contrast, patients with classic distal renal tubular acidosis (dRTA) generally have hypokalemic hyperchloremic metabolic acidosis. The metabolic acidosis results from the inability to acidify urine in the distal nephron and impaired excretion of NH4 + 100. Inherited forms of dRTA have defects in the basolateral HCO 3 -/Cl - exchanger, B1 or A4 subunits of the H +-ATPase, or CA. Some medications can mimic these defects by altering membrane permeability and causing leaky pathways 45. Amphotericin B 108, 109, lithium 116– 118, and foscarnet 119 are known to cause leak and lead to hypokalemic hyperchloremic metabolic acidosis ( Figure 4).
Drugs causing Fanconi syndrome and proximal renal tubular acidosis
The proximal tubule is the initial step in renal acidification and is essential in maintaining acid-base homeostasis by reclaiming 80% of filtered bicarbonate (HCO 3 -) ( Figure 5). Bicarbonate reabsorption occurs by luminal H + excretion and HCO 3 - extrusion back into the blood at the basolateral membrane 100. CAs catalyze the reaction: CO 2 + H 2O → HCO 3 -+ H +. If proximal HCO 3 - reclamation is impaired, more HCO 3 - is delivered to the distal tubule, which has limited capacity for HCO 3 - reabsorption. Bicarbonaturia ensues and net acid excretion decreases, which eventually leads to metabolic acidosis 45, 120. Generalized proximal tubule dysfunction is termed Fanconi syndrome. Potential drugs that could induce Fanconi syndrome include the following ( Figure 5):
Figure 5. Mechanisms of proximal tubule (PT) and drug-induced Fanconi syndrome.
1. CA inhibitors 25 cause bicarbonaturia and hyperchloremic metabolic acidosis in the elderly 26 and patients with renal failure 27 and diabetes 28.
2. Antineoplastic platinum-containing agents 126, 127 and DNA-alkylating agents 128– 130 damage proximal tubule cells through accumulation and induced cell apoptosis.
3. Anti-viral/HIV drugs 75, 121– 124, valproic acid (VPA) 131– 133, and outdated tetracycline 134– 136 interfere with mitochondrial function within proximal tubule cells, leading to tubular dysfunction.
4. Aminoglycosides 137, 148, 149 induce acidosis with unclear mechanisms 150.
5. Deferasirox 139– 143 increases hemodynamic iron removal, causes vacuolization of proximal tubular epithelial cells 142, and elevates iron absorption in various organs. All could lead to acidosis.
-
-
CA inhibitors (e.g. acetazolamide) 25.
-
-
Anti-viral/HIV drugs (e.g. lamivudine, stavudine 75 and tenofovir 121– 124). Most tenofovir-induced cases are subclinical 125
-
-
Platinum-containing agents (e.g. cisplatin 126, 127) and DNA alkylating agents (e.g. ifosfamide 128– 130) are common proximal tubule toxins. Note that cyclophosphamide, structural isomer of ifosfamide, can also cause hemorrhagic cystitis but is not nephrotoxic by producing less chloroacetaldehyde 128
- -
- -
-
-
Aminoglycoside 137 accumulation in proximal tubule would lead to nephrotoxicity with an unclear mechanism; however, incidence decreased recently due to a better monitoring strategy 138
- -
Many other agents such as fumaric acid 144, suramin 145, and imatinib 146 have also been associated with Fanconi syndrome in case reports. This field remained to be further explored as proximal tubule toxicity is common due to the existence of multiple drug transporters at the surface membrane, leading to very high uptake of drugs by this segment 147.
Conclusion
In summary, metabolic acidosis can occur as a side effect of therapy. Instead of memorizing the catalogue of drugs, clinicians should classify these agents based on their pathophysiologic mechanisms to facilitate the recognition of potential causal relationships. Some of these side effects are inferred from empirical observations, but some have undergone extensive studies to determine the pathogenesis of metabolic acidosis. We hope that this review will intrigue our readers to experience that eureka moment identifying unrecognized explanations for metabolic acidosis in patients or to partake in extending clinical observations to clinical investigations.
Abbreviations
ACEI, Angiotensin-converting enzyme inhibitor; ARB, Aldosterone receptor blocker; CA, Carbonic anhydrase; COX, Cyclooxygenase; dRTA, Distal renal tubular acidosis; FDA, Food & Drug Administration; GRAS, Generally recognized as safe; GI, Gastrointestinal; HAART, Highly active antiretroviral therapy; MALA, Metformin-associated lactic acidosis; NAD, Nicotinamide Adenine Dinucleotide; PG, Propylene glycol; RAAS, Renin-angiotensin-aldosterone system; VPA, Valproic acid.
Editorial Note on the Review Process
F1000 Faculty Reviews are commissioned from members of the prestigious F1000 Faculty and are edited as a service to readers. In order to make these reviews as comprehensive and accessible as possible, the referees provide input before publication and only the final, revised version is published. The referees who approved the final version are listed with their names and affiliations but without their reports on earlier versions (any comments will already have been addressed in the published version).
The referees who approved this article are:
Pierluigi Brazzola, Regional Hospital of Bellinzona and valleys, Bellinzona, Switzerland
Mitchell Halperin, Faculty of Medicine, University of Toronto, Toronto, Ontario, Canada
Jeffrey Kraut, Department of Medicine, David Geffen School of Medicine, Los Angeles, CA, USA
Funding Statement
The authors are supported by the National Institutes of Health (R01-DK092461, R01 DK081423, R01DK091392, U01-HL111146), the O’Brien Kidney Research Center (P30 DK-079328), and the Charles and Jane Pak Foundation.
[version 1; referees: 3 approved]
References
- 1. Moe OW, Fuster D, Alpern RJ: Common acid-base disorders. In: Goldman L, Wachter RM, Hollander H, editors. Hosp Med 2nd ed. Philadelphia: Lippincott, William & Wilkins;2005;1055–65. [Google Scholar]
- 2. Wiederkehr MR, Moe OW: Treatment of metabolic acidosis. In: Massry SG, Suki WK, editors. Therapy of Renal Diseases and Related Disorders 4th ed: Springer; In press,2011. [Google Scholar]
- 3. Moe OW, Fuster D: Clinical acid-base pathophysiology: disorders of plasma anion gap. Best Pract Res Clin Endocrinol Metab. 2003;17(4):559–74. 10.1016/S1521-690X(03)00054-X [DOI] [PubMed] [Google Scholar]
- 4. McMartin KE, Ambre JJ, Tephly TR: Methanol poisoning in human subjects. Role for formic acid accumulation in the metabolic acidosis. Am J Med. 1980;68(3):414–8. 10.1016/0002-9343(80)90113-8 [DOI] [PubMed] [Google Scholar]
- 5. Jacobsen D, Hewlett TP, Webb R, et al. : Ethylene glycol intoxication: evaluation of kinetics and crystalluria. Am J Med. 1988;84(1):145–52. 10.1016/0002-9343(88)90024-1 [DOI] [PubMed] [Google Scholar]
- 6. Vale JA, Buckley BM: Metabolic acidosis in diethylene glycol poisoning. Lancet. 1985;2(8451):394. 10.1016/S0140-6736(85)92538-3 [DOI] [PubMed] [Google Scholar]
- 7. Slaughter RJ, Mason RW, Beasley DM, et al. : Isopropanol poisoning. Clin Toxicol (Phila). 2014;52(5):470–8. 10.3109/15563650.2014.914527 [DOI] [PubMed] [Google Scholar]
- 8. Carlisle EJ, Donnelly SM, Vasuvattakul S, et al. : Glue-sniffing and distal renal tubular acidosis: sticking to the facts. J Am Soc Nephrol. 1991;1(8):1019–27. [DOI] [PubMed] [Google Scholar]
- 9. Relman AS, Shelburne PF, Talman A: Profound acidosis resulting from excessive ammonium chloride in previously healthy subjects. A study of two cases. N Engl J Med. 1961;264:848–52. 10.1056/NEJM196104272641703 [DOI] [PubMed] [Google Scholar]
- 10. Lemann J, Jr, Lennon EJ, Goodman AD, et al. : The net balance of acid in subjects given large loads of acid or alkali. J Clin Invest. 1965;44(4):507–17. 10.1172/JCI105164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lemann J, Jr, Lennon EJ, Goodman AD, et al. : The role of fixed tissue buffers in acid-base regulation. Trans Assoc Am Physicians. 1964;77:188–95. [PubMed] [Google Scholar]
- 12. Tsai IC, Huang JW, Chu TS, et al. : Factors associated with metabolic acidosis in patients receiving parenteral nutrition. Nephrology (Carlton). 2007;12(1):3–7. 10.1111/j.1440-1797.2006.00748.x [DOI] [PubMed] [Google Scholar]
- 13. Wilson KC, Reardon C, Theodore AC, et al. : Propylene glycol toxicity: a severe iatrogenic illness in ICU patients receiving IV benzodiazepines: a case series and prospective, observational pilot study. Chest. 2005;128(3):1674–81. 10.1378/chest.128.3.1674 [DOI] [PubMed] [Google Scholar]
- 14. Toxicological evaluation of certain food additives with a review of general principles and of specifications. Seventeenth report of the joint FAO-WHO Expert Committee on Food Additives. World Health Organ Tech Rep Ser. 1974;539:1–40. [PubMed] [Google Scholar]
- 15. Martin G, Finberg L: Propylene glycol: a potentially toxic vehicle in liquid dosage form. J Pediatr. 1970;77(5):877–8. 10.1016/S0022-3476(70)80253-0 [DOI] [PubMed] [Google Scholar]
- 16. Cate JC, 4th, Hedrick R: Propylene glycol intoxication and lactic acidosis. N Engl J Med. 1980;303(21):1237. 10.1056/NEJM198011203032116 [DOI] [PubMed] [Google Scholar]
- 17. Wilson KC, Reardon C, Farber HW: Propylene glycol toxicity in a patient receiving intravenous diazepam. N Engl J Med. 2000;343(11):815. 10.1056/NEJM200009143431115 [DOI] [PubMed] [Google Scholar]
- 18. Bedichek E, Kirschbaum B: A case of propylene glycol toxic reaction associated with etomidate infusion. Arch Intern Med. 1991;151(11):2297–8. 10.1001/archinte.1991.00400110137026 [DOI] [PubMed] [Google Scholar]
- 19. Demey HE, Daelemans RA, Verpooten GA, et al. : Propylene glycol-induced side effects during intravenous nitroglycerin therapy. Intensive Care Med. 1988;14(3):221–6. 10.1007/BF00717993 [DOI] [PubMed] [Google Scholar]
- 20. Yorgin PD, Theodorou AA, Al-Uzri A, et al. : Propylene glycol-induced proximal renal tubular cell injury. Am J Kidney Dis. 1997;30(1):134–9. 10.1016/S0272-6386(97)90577-1 [DOI] [PubMed] [Google Scholar]
- 21. Ruddick JA: Toxicology, metabolism, and biochemistry of 1,2-propanediol. Toxicol Appl Pharmacol. 1972;21(1):102–11. 10.1016/0041-008X(72)90032-4 [DOI] [PubMed] [Google Scholar]
- 22. Speth PA, Vree TB, Neilen NF, et al. : Propylene glycol pharmacokinetics and effects after intravenous infusion in humans. Ther Drug Monit. 1987;9(3):255–8. 10.1097/00007691-198709000-00001 [DOI] [PubMed] [Google Scholar]
- 23. Morshed KM, Jain SK, McMartin KE: Propylene glycol-mediated cell injury in a primary culture of human proximal tubule cells. Toxicol Sci. 1998;46(2):410–7. 10.1006/toxs.1998.2521 [DOI] [PubMed] [Google Scholar]
- 24. Lu J, Zello GA, Randell E, et al. : Closing the anion gap: contribution of D-lactate to diabetic ketoacidosis. Clin Chim Acta. 2011;412(3–4):286–91. 10.1016/j.cca.2010.10.020 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 25. Hanley T, Platts MM: Observations on the metabolic effects of the carbonic anhydrase inhibitor diamox: mode and rate of recovery from the drug's action. J Clin Invest. 1956;35(1):20–30. 10.1172/JCI103248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Chapron DJ, Gomolin IH, Sweeney KR: Acetazolamide blood concentrations are excessive in the elderly: propensity for acidosis and relationship to renal function. J Clin Pharmacol. 1989;29(4):348–53. 10.1002/j.1552-4604.1989.tb03340.x [DOI] [PubMed] [Google Scholar]
- 27. De Marchi S, Cecchin E: Severe metabolic acidosis and disturbances of calcium metabolism induced by acetazolamide in patients on haemodialysis. Clin Sci (Lond). 1990;78(3):295–302. 10.1042/cs0780295 [DOI] [PubMed] [Google Scholar]
- 28. Siklos P, Henderson RG: Severe acidosis from acetazolamide in a diabetic patient. Curr Med Res Opin. 1979;6(4):284–6. 10.1185/03007997909109439 [DOI] [PubMed] [Google Scholar]
- 29. Filippi L, Bagnoli F, Margollicci M, et al. : Pathogenic mechanism, prophylaxis, and therapy of symptomatic acidosis induced by acetazolamide. J Investig Med. 2002;50(2):125–32. 10.2310/6650.2002.31297 [DOI] [PubMed] [Google Scholar]
- 30. Menon GJ, Vernon SA: Topical brinzolamide and metabolic acidosis. Br J Ophthalmol. 2006;90(2):247–8. 10.1136/bjo.2005.075622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Mirza N, Marson AG, Pirmohamed M: Effect of topiramate on acid-base balance: extent, mechanism and effects. Br J Clin Pharmacol. 2009;68(5):655–61. 10.1111/j.1365-2125.2009.03521.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Wilner A, Raymond K, Pollard R: Topiramate and metabolic acidosis. Epilepsia. 1999;40(6):792–5. 10.1111/j.1528-1157.1999.tb00781.x [DOI] [PubMed] [Google Scholar]
- 33. Stowe CD, Bollinger T, James LP, et al. : Acute mental status changes and hyperchloremic metabolic acidosis with long-term topiramate therapy. Pharmacotherapy. 2000;20(1):105–9. 10.1592/phco.20.1.105.34662 [DOI] [PubMed] [Google Scholar]
- 34. Welch BJ, Graybeal D, Moe OW, et al. : Biochemical and stone-risk profiles with topiramate treatment. Am J Kidney Dis. 2006;48(4):555–63. 10.1053/j.ajkd.2006.07.003 [DOI] [PubMed] [Google Scholar]
- 35. Maalouf NM, Langston JP, van Ness PC, et al. : Nephrolithiasis in topiramate users. Urol Res. 2011;39(4):303–307. In press. 10.1007/s00240-010-0347-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Petroff PA, Hander EW, Mason AD, Jr: Ventilatory patterns following burn injury and effect of sulfamylon. J Trauma. 1975;15(8):650–6. 10.1097/00005373-197508000-00005 [DOI] [PubMed] [Google Scholar]
- 37. Scheel PJ, Jr, Whelton A, Rossiter K, et al. : Cholestyramine-induced hyperchloremic metabolic acidosis. J Clin Pharmacol. 1992;32(6):536–8. 10.1177/009127009203200608 [DOI] [PubMed] [Google Scholar]
- 38. Kleinman PK: Letter: Cholestyramine and metabolic acidosis. N Engl J Med. 1974;290(15):861. 10.1056/NEJM197404112901519 [DOI] [PubMed] [Google Scholar]
- 39. Eaves ER, Korman MG: Cholestyramine induced hyperchloremic metabolic acidosis. Aust N Z J Med. 1984;14(5):670–2. 10.1111/j.1445-5994.1984.tb05023.x [DOI] [PubMed] [Google Scholar]
- 40. Brezina B, Qunibi WY, Nolan CR: Acid loading during treatment with sevelamer hydrochloride: mechanisms and clinical implications. Kidney Int Suppl. 2004;66(90):S39–45. 10.1111/j.1523-1755.2004.09007.x [DOI] [PubMed] [Google Scholar]
- 41. Qunibi WY, Hootkins RE, McDowell LL, et al. : Treatment of hyperphosphatemia in hemodialysis patients: The Calcium Acetate Renagel Evaluation (CARE Study). Kidney Int. 2004;65(5):1914–26. 10.1111/j.1523-1755.2004.00590.x [DOI] [PubMed] [Google Scholar]
- 42. Biggar P, Ketteler M: Sevelamer carbonate for the treatment of hyperphosphatemia in patients with kidney failure (CKD III - V). Expert Opin Pharmacother. 2010;11(16):2739–50. 10.1517/14656566.2010.526107 [DOI] [PubMed] [Google Scholar]
- 43. Akizawa T, Origasa H, Kameoka C, et al. : Randomized controlled trial of bixalomer versus sevelamer hydrochloride in hemodialysis patients with hyperphosphatemia. Ther Apher Dial. 2014;18(2):122–31. 10.1111/1744-9987.12068 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 44. Hatakeyama S, Murasawa H, Narita T, et al. : Switching hemodialysis patients from sevelamer hydrochloride to bixalomer: a single-center, non-randomized analysis of efficacy and effects on gastrointestinal symptoms and metabolic acidosis. BMC Nephrol. 2013;14:222. 10.1186/1471-2369-14-222 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 45. DuBose TD: Disorder of Acid-Base Balance. In: Brenner BM editor. Brenner and Rector's The Kidney.8th ed. Philadelphia: Saunders;2007;505–46. [Google Scholar]
- 46. Gennari FJ, Weise WJ: Acid-base disturbances in gastrointestinal disease. Clin J Am Soc Nephrol. 2008;3(6):1861–8. 10.2215/CJN.02450508 [DOI] [PubMed] [Google Scholar]
- 47. Haldane JB, Hill R, Luck JM: Calcium chloride acidosis. J Physiol. 1923;57(5):301–6. 10.1113/jphysiol.1923.sp002067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Madias NE: Lactic acidosis. Kidney Int. 1986;29(3):752–74. 10.1038/ki.1986.62 [DOI] [PubMed] [Google Scholar]
- 49. Melvin L, Wesson D: Lactic Acidosis. In: Dubose TD, Hamm L. Lee, editor. Acid-Base and Electrolyte Disorders: A Companion to Brenner and Rector's The Kidney.Philadelphia: WB Saunders;2002;83–5. [Google Scholar]
- 50. Lalau JD: Lactic acidosis induced by metformin: incidence, management and prevention. Drug Saf. 2010;33(9):727–40. 10.2165/11536790-000000000-00000 [DOI] [PubMed] [Google Scholar]
- 51. Salpeter SR, Greyber E, Pasternak GA, et al. : Risk of fatal and nonfatal lactic acidosis with metformin use in type 2 diabetes mellitus. Cochrane Database Syst Rev. 2010; (4):CD002967. 10.1002/14651858.CD002967.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 52. Peters N, Jay N, Barraud D, et al. : Metformin-associated lactic acidosis in an intensive care unit. Crit Care. 2008;12(6):R149. 10.1186/cc7137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Almaleki N, Ashraf M, Hussein MM, et al. : Metformin-associated lactic acidosis in a peritoneal dialysis patient. Saudi J Kidney Dis Transpl. 2015;26(2):325–8. 10.4103/1319-2442.152498 [DOI] [PubMed] [Google Scholar]
- 54. Nyirenda MJ, Sandeep T, Grant I, et al. : Severe acidosis in patients taking metformin--rapid reversal and survival despite high APACHE score. Diabet Med. 2006;23(4):432–5. 10.1111/j.1464-5491.2006.01813.x [DOI] [PubMed] [Google Scholar]
- 55. Audia P, Feinfeld DA, Dubrow A, et al. : Metformin-induced lactic acidosis and acute pancreatitis precipitated by diuretic, celecoxib, and candesartan-associated acute kidney dysfunction. Clin Toxicol (Phila). 2008;46(2):164–6. 10.1080/15563650701355314 [DOI] [PubMed] [Google Scholar]
- 56. El-Hennawy AS, Jacob S, Mahmood AK: Metformin-associated lactic acidosis precipitated by diarrhea. Am J Ther. 2007;14(4):403–5. 10.1097/01.pap.0000249953.92311.23 [DOI] [PubMed] [Google Scholar]
- 57. Renda F, Mura P, Finco G, et al. : Metformin-associated lactic acidosis requiring hospitalization. A national 10 year survey and a systematic literature review. Eur Rev Med Pharmacol Sci. 2013;17(Suppl 1):45–9. [PubMed] [Google Scholar]; F1000 Recommendation
- 58. Scheen AJ, Paquot N: Metformin revisited: a critical review of the benefit-risk balance in at-risk patients with type 2 diabetes. Diabetes Metab. 2013;39(3):179–90. 10.1016/j.diabet.2013.02.006 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 59. Kajbaf F, Lalau JD: The prognostic value of blood pH and lactate and metformin concentrations in severe metformin-associated lactic acidosis. BMC Pharmacol Toxicol. 2013;14:22. 10.1186/2050-6511-14-22 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 60. Adam WR, O'Brien RC: A justification for less restrictive guidelines on the use of metformin in stable chronic renal failure. Diabet Med. 2014;31(9):1032–8. 10.1111/dme.12515 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 61. Inzucchi SE, Lipska KJ, Mayo H, et al. : Metformin in patients with type 2 diabetes and kidney disease: a systematic review. JAMA. 2014;312(24):2668–75. 10.1001/jama.2014.15298 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 62. Venos ES, Sigal RJ: My patient's diabetic kidney disease has progressed to stage 4; should I discontinue metformin? Can J Diabetes. 2014;38(5):296–9. 10.1016/j.jcjd.2014.07.225 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 63. Heaf J: Metformin in chronic kidney disease: time for a rethink. Perit Dial Int. 2014;34(4):353–7. 10.3747/pdi.2013.00344 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 64. Kajbaf F, Lalau JD: Mortality rate in so-called "metformin-associated lactic acidosis": a review of the data since the 1960s. Pharmacoepidemiol Drug Saf. 2014;23(11):1123–7. 10.1002/pds.3689 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 65. Palella FJ, Delaney KM, Moorman AC, et al. : Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. HIV Outpatient Study Investigators. N Engl J Med. 1998;338(13):853–60. 10.1056/NEJM199803263381301 [DOI] [PubMed] [Google Scholar]
- 66. Gérard Y, Maulin L, Yazdanpanah Y, et al. : Symptomatic hyperlactataemia: an emerging complication of antiretroviral therapy. AIDS. 2000;14(17):2723–30. [DOI] [PubMed] [Google Scholar]
- 67. Sundar K, Suarez M, Banogon PE, et al. : Zidovudine-induced fatal lactic acidosis and hepatic failure in patients with acquired immunodeficiency syndrome: report of two patients and review of the literature. Crit Care Med. 1997;25(8):1425–30. 10.1097/00003246-199708000-00034 [DOI] [PubMed] [Google Scholar]
- 68. Bissuel F, Bruneel F, Habersetzer F, et al. : Fulminant hepatitis with severe lactate acidosis in HIV-infected patients on didanosine therapy. J Intern Med. 1994;235(4):367–71. 10.1111/j.1365-2796.1994.tb01088.x [DOI] [PubMed] [Google Scholar]
- 69. Goldfarb-Rumyantzev AS, Jeyakumar A, Gumpeni R, et al. : Lactic acidosis associated with nucleoside analog therapy in an HIV-positive patient. AIDS Patient Care STDS. 2000;14(7):339–42. 10.1089/108729100413194 [DOI] [PubMed] [Google Scholar]
- 70. Kakuda TN: Pharmacology of nucleoside and nucleotide reverse transcriptase inhibitor-induced mitochondrial toxicity. Clin Ther. 2000;22(6):685–708. 10.1016/S0149-2918(00)90004-3 [DOI] [PubMed] [Google Scholar]
- 71. Margolis AM, Heverling H, Pham PA, et al. : A review of the toxicity of HIV medications. J Med Toxicol. 2014;10(1):26–39. 10.1007/s13181-013-0325-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Bonnet F, Balestre E, Bernardin E, et al. : Risk factors for hyperlactataemia in HIV-infected patients, Aquitaine Cohort, 1999--2003. Antivir Chem Chemother. 2005;16(1):63–7. [DOI] [PubMed] [Google Scholar]
- 73. Crowther MA, Callaghan W, Hodsman AB, et al. : Dideoxyinosine-associated nephrotoxicity. AIDS. 1993;7(1):131–2. [PubMed] [Google Scholar]
- 74. Vittecoq D, Dumitrescu L, Beaufils H, et al. : Fanconi syndrome associated with cidofovir therapy. Antimicrob Agents Chemother. 1997;41(8):1846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Nelson M, Azwa A, Sokwala A, et al. : Fanconi syndrome and lactic acidosis associated with stavudine and lamivudine therapy. AIDS. 2008;22(11):1374–6. 10.1097/QAD.0b013e328303be50 [DOI] [PubMed] [Google Scholar]
- 76. Falcó V, Rodríguez D, Ribera E, et al. : Severe nucleoside-associated lactic acidosis in human immunodeficiency virus-infected patients: report of 12 cases and review of the literature. Clin Infect Dis. 2002;34(6):838–46. 10.1086/339041 [DOI] [PubMed] [Google Scholar]
- 77. De Vriese AS, Coster RV, Smet J, et al. : Linezolid-induced inhibition of mitochondrial protein synthesis. Clin Infect Dis. 2006;42(8):1111–7. 10.1086/501356 [DOI] [PubMed] [Google Scholar]
- 78. Diekema DJ, Jones RN: Oxazolidinone antibiotics. Lancet. 2001;358(9297):1975–82. 10.1016/S0140-6736(01)06964-1 [DOI] [PubMed] [Google Scholar]
- 79. Apodaca AA, Rakita RM: Linezolid-induced lactic acidosis. N Engl J Med. 2003;348(1):86–7. 10.1056/NEJM200301023480123 [DOI] [PubMed] [Google Scholar]
- 80. Wiener M, Guo Y, Patel G, et al. : Lactic acidosis after treatment with linezolid. Infection. 2007;35(4):278–81. 10.1007/s15010-007-6302-x [DOI] [PubMed] [Google Scholar]
- 81. Bernard L, Stern R, Lew D, et al. : Serotonin syndrome after concomitant treatment with linezolid and citalopram. Clin Infect Dis. 2003;36(9):1197. 10.1086/374558 [DOI] [PubMed] [Google Scholar]
- 82. Pea F, Scudeller L, Lugano M, et al. : Hyperlactacidemia potentially due to linezolid overexposure in a liver transplant recipient. Clin Infect Dis. 2006;42(3):434–5. 10.1086/499533 [DOI] [PubMed] [Google Scholar]
- 83. Ozkaya-Parlakay A, Kara A, Celik M, et al. : Early lactic acidosis associated with linezolid therapy in paediatric patients. Int J Antimicrob Agents. 2014;44(4):334–6. 10.1016/j.ijantimicag.2014.06.017 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 84. Neff TA: Isoniazid toxicity: reports of lactic acidosis and keratitis. Chest. 1971;59(3):245–8. 10.1378/chest.59.3.245 [DOI] [PubMed] [Google Scholar]
- 85. Hankins DG, Saxena K, Faville RJ, Jr, et al. : Profound acidosis caused by isoniazid ingestion. Am J Emerg Med. 1987;5(2):165–6. 10.1016/0735-6757(87)90098-2 [DOI] [PubMed] [Google Scholar]
- 86. Kreisberg RA, Wood BC: Drug and chemical-induced metabolic acidosis. Clin Endocrinol Metab. 1983;12(2):391–411. 10.1016/S0300-595X(83)80048-6 [DOI] [PubMed] [Google Scholar]
- 87. Alvarez FG, Guntupalli KK: Isoniazid overdose: four case reports and review of the literature. Intensive Care Med. 1995;21(8):641–4. 10.1007/BF01711541 [DOI] [PubMed] [Google Scholar]
- 88. Peters JH, Miller KS, Brown P: Studies on the metabolic basis for the genetically determined capacities for isoniazid inactivation in man. J Pharmacol Exp Ther. 1965;150(2):298–304. [PubMed] [Google Scholar]
- 89. Patiala J: The amount of pyridine nucleotides (coenzymes I and II) in blood in experimental tuberculosis before and during isoniazid treatment. Am Rev Tuberc. 1954;70(3):453–64. [DOI] [PubMed] [Google Scholar]
- 90. Kam PC, Cardone D: Propofol infusion syndrome. Anaesthesia. 2007;62(7):690–701. 10.1111/j.1365-2044.2007.05055.x [DOI] [PubMed] [Google Scholar]
- 91. Marinella MA: Lactic acidosis associated with propofol. Chest. 1996;109(1):292. 10.1378/chest.109.1.292 [DOI] [PubMed] [Google Scholar]
- 92. Bray RJ: Propofol infusion syndrome in children. Paediatr Anaesth. 1998;8(6):491–9. 10.1046/j.1460-9592.1998.00282.x [DOI] [PubMed] [Google Scholar]
- 93. Bidani A, Tuazon DM, Heming TA: Regulation of Whole Body Acid-Base Balance. In: Dubose TD, Hamm L. Lee, editor. Acid-Base and Electrolyte Disorders: A Companion to Brenner and Rector's The Kidney Philadelphia: WB Saunders;2002;1–21. [Google Scholar]
- 94. Arena FP, Dugowson C, Saudek CD: Salicylate-induced hypoglycemia and ketoacidosis in a nondiabetic adult. Arch Intern Med. 1978;138(7):1153–4. 10.1001/archinte.1978.03630320085031 [DOI] [PubMed] [Google Scholar]
- 95. Proudfoot AT, Krenzelok EP, Brent J, et al. : Does urine alkalinization increase salicylate elimination? If so, why? Toxicol Rev. 2003;22(3):129–36. 10.2165/00139709-200322030-00001 [DOI] [PubMed] [Google Scholar]
- 96. Fenves AZ, Kirkpatrick HM 3rd, Patel VV, et al. : Increased anion gap metabolic acidosis as a result of 5-oxoproline (pyroglutamic acid): a role for acetaminophen. Clin J Am Soc Nephrol. 2006;1(3):441–7. 10.2215/CJN.01411005 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 97. Emmett M: Acetaminophen toxicity and 5-oxoproline (pyroglutamic acid): a tale of two cycles, one an ATP-depleting futile cycle and the other a useful cycle. Clin J Am Soc Nephrol. 2014;9(1):191–200. 10.2215/CJN.07730713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Croal BL, Glen AC, Kelly CJ, et al. : Transient 5-oxoprolinuria (pyroglutamic aciduria) with systemic acidosis in an adult receiving antibiotic therapy. Clin Chem. 1998;44(2):336–40. [PubMed] [Google Scholar]
- 99. Wagner CA, Devuyst O, Bourgeois S, et al. : Regulated acid-base transport in the collecting duct. Pflugers Arch. 2009;458(1):137–56. 10.1007/s00424-009-0657-z [DOI] [PubMed] [Google Scholar]
- 100. Rodríguez-Soriano J: New insights into the pathogenesis of renal tubular acidosis--from functional to molecular studies. Pediatr Nephrol. 2000;14(12):1121–36. 10.1007/s004670000407 [DOI] [PubMed] [Google Scholar]
- 101. Eiam-Ong S, Kurtzman NA, Sabatini S: Regulation of collecting tubule adenosine triphosphatases by aldosterone and potassium. J Clin Invest. 1993;91(6):2385–92. 10.1172/JCI116471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. DuBose TD, Jr: Molecular and pathophysiologic mechanisms of hyperkalemic metabolic acidosis. Trans Am Clin Climatol Assoc. 2000;111:122–33; discussion 133–4. [PMC free article] [PubMed] [Google Scholar]
- 103. Cheng HF, Harris RC: Cyclooxygenases, the kidney, and hypertension. Hypertension. 2004;43(3):525–30. 10.1161/01.HYP.0000116221.27079.ea [DOI] [PubMed] [Google Scholar]
- 104. Weinberg JM, Appel LJ, Bakris G, et al. : Risk of hyperkalemia in nondiabetic patients with chronic kidney disease receiving antihypertensive therapy. Arch Intern Med. 2009;169(17):1587–94. 10.1001/archinternmed.2009.284 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 105. White WB, Bresalier R, Kaplan AP, et al. : Safety and tolerability of the direct renin inhibitor aliskiren in combination with angiotensin receptor blockers and thiazide diuretics: a pooled analysis of clinical experience of 12,942 patients. J Clin Hypertens (Greenwich). 2011;13(7):506–16. 10.1111/j.1751-7176.2011.00438.x [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 106. Sakallı H, Baskın E, Bayrakcı US, et al. : Acidosis and hyperkalemia caused by losartan and enalapril in pediatric kidney transplant recipients. Exp Clin Transplant. 2014;12(4):310–3. 10.6002/ect.2013.0172 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 107. Preston RA, Hirsh MJ MD, Oster MD, Jr, et al. : University of Miami Division of Clinical Pharmacology therapeutic rounds: drug-induced hyperkalemia. Am J Ther. 1998;5(2):125–32. 10.1097/00045391-199803000-00013 [DOI] [PubMed] [Google Scholar]
- 108. Ayub M, Levell MJ: Inhibition of human adrenal steroidogenic enzymes in vitro by imidazole drugs including ketoconazole. J Steroid Biochem. 1989;32(4):515–24. 10.1016/0022-4731(89)90384-1 [DOI] [PubMed] [Google Scholar]
- 109. Ohlsson A, Cedergreen N, Oskarsson A, et al. : Mixture effects of imidazole fungicides on cortisol and aldosterone secretion in human adrenocortical H295R cells. Toxicology. 2010;275(1–3):21–8. 10.1016/j.tox.2010.05.013 [DOI] [PubMed] [Google Scholar]
- 110. Davies DL, Wilson GM: Diuretics: mechanism of action and clinical application. Drugs. 1975;9(3):178–226. 10.2165/00003495-197509030-00003 [DOI] [PubMed] [Google Scholar]
- 111. Kleyman TR, Roberts C, Ling BN: A mechanism for pentamidine-induced hyperkalemia: inhibition of distal nephron sodium transport. Ann Intern Med. 1995;122(2):103–6. 10.7326/0003-4819-122-2-199501150-00004 [DOI] [PubMed] [Google Scholar]
- 112. Schlanger LE, Kleyman TR, Ling BN: K +-sparing diuretic actions of trimethoprim: inhibition of Na + channels in A6 distal nephron cells. Kidney Int. 1994;45(4):1070–6. 10.1038/ki.1994.143 [DOI] [PubMed] [Google Scholar]
- 113. Velázquez H, Perazella MA, Wright FS, et al. : Renal mechanism of trimethoprim-induced hyperkalemia. Ann Intern Med. 1993;119(4):296–301. 10.7326/0003-4819-119-4-199308150-00008 [DOI] [PubMed] [Google Scholar]
- 114. Caliskan Y, Kalayoglu-Besisik S, Sargin D, et al. : Cyclosporine-associated hyperkalemia: report of four allogeneic blood stem-cell transplant cases. Transplantation. 2003;75(7):1069–72. 10.1097/01.TP.0000057241.69355.59 [DOI] [PubMed] [Google Scholar]
- 115. Lea JP, Sands JM, McMahon SJ, et al. : Evidence that the inhibition of Na +/K +-ATPase activity by FK506 involves calcineurin. Kidney Int. 1994;46(3):647–52. 10.1038/ki.1994.317 [DOI] [PubMed] [Google Scholar]
- 116. Kim YH, Kwon TH, Christensen BM, et al. : Altered expression of renal acid-base transporters in rats with lithium-induced NDI. Am J Physiol Renal Physiol. 2003;285(6):F1244–57. 10.1152/ajprenal.00176.2003 [DOI] [PubMed] [Google Scholar]
- 117. Roscoe JM, Goldstein MB, Halperin ML, et al. : Lithium-induced impairment of urine acidification. Kidney Int. 1976;9(4):344–50. 10.1038/ki.1976.40 [DOI] [PubMed] [Google Scholar]
- 118. Grünfeld JP, Rossier BC: Lithium nephrotoxicity revisited. Nat Rev Nephrol. 2009;5(5):270–6. 10.1038/nrneph.2009.43 [DOI] [PubMed] [Google Scholar]
- 119. Navarro JF, Quereda C, Quereda C, et al. : Nephrogenic diabetes insipidus and renal tubular acidosis secondary to foscarnet therapy. Am J Kidney Dis. 1996;27(3):431–4. 10.1016/S0272-6386(96)90369-8 [DOI] [PubMed] [Google Scholar]
- 120. Hamm LL, Nakhoul N: Renal Acidification. In: Brenner BM, editor. Brenner and Rector's The Kidney Philadelphia: Saunders;2007;248–69. [Google Scholar]
- 121. Malik A, Abraham P, Malik N: Acute renal failure and Fanconi syndrome in an AIDS patient on tenofovir treatment--case report and review of literature. J Infect. 2005;51(2):E61–5. 10.1016/j.jinf.2004.08.031 [DOI] [PubMed] [Google Scholar]
- 122. Hall AM, Hendry BM, Nitsch D, et al. : Tenofovir-associated kidney toxicity in HIV-infected patients: a review of the evidence. Am J Kidney Dis. 2011;57(5):773–80. 10.1053/j.ajkd.2011.01.022 [DOI] [PubMed] [Google Scholar]
- 123. Herlitz LC, Mohan S, Stokes MB, et al. : Tenofovir nephrotoxicity: acute tubular necrosis with distinctive clinical, pathological, and mitochondrial abnormalities. Kidney Int. 2010;78(11):1171–7. 10.1038/ki.2010.318 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 124. Lucey JM, Hsu P, Ziegler JB: Tenofovir-related Fanconi's syndrome and osteomalacia in a teenager with HIV. BMJ Case Rep. 2013;2013: pii: bcr2013008674. 10.1136/bcr-2013-008674 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 125. Hall AM, Edwards SG, Lapsley M, et al. : Subclinical tubular injury in HIV-infected individuals on antiretroviral therapy: a cross-sectional analysis. Am J Kidney Dis. 2009;54(6):1034–42. 10.1053/j.ajkd.2009.07.012 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 126. Cachat F, Nenadov-Beck M, Guignard JP: Occurrence of an acute Fanconi syndrome following cisplatin chemotherapy. Med Pediatr Oncol. 1998;31(1):40–1. [DOI] [PubMed] [Google Scholar]
- 127. Sahni V, Choudhury D, Ahmed Z: Chemotherapy-associated renal dysfunction. Nat Rev Nephrol. 2009;5(8):450–62. 10.1038/nrneph.2009.97 [DOI] [PubMed] [Google Scholar]
- 128. Zamlauski-Tucker MJ, Morris ME, Springate JE: Ifosfamide metabolite chloroacetaldehyde causes Fanconi syndrome in the perfused rat kidney. Toxicol Appl Pharmacol. 1994;129(1):170–5. 10.1006/taap.1994.1241 [DOI] [PubMed] [Google Scholar]
- 129. Stöhr W, Paulides M, Bielack S, et al. : Ifosfamide-induced nephrotoxicity in 593 sarcoma patients: a report from the Late Effects Surveillance System. Pediatr Blood Cancer. 2007;48(4):447–52. 10.1002/pbc.20858 [DOI] [PubMed] [Google Scholar]
- 130. Leem AY, Kim HS, Yoo BW, et al. : Ifosfamide-induced Fanconi syndrome with diabetes insipidus. Korean J Intern Med. 2014;29(2):246–9. 10.3904/kjim.2014.29.2.246 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 131. Watanabe T, Yoshikawa H, Yamazaki S, et al. : Secondary renal Fanconi syndrome caused by valproate therapy. Pediatr Nephrol. 2005;20(6):814–7. 10.1007/s00467-005-1827-7 [DOI] [PubMed] [Google Scholar]
- 132. Knorr M, Schaper J, Harjes M, et al. : Fanconi syndrome caused by antiepileptic therapy with valproic Acid. Epilepsia. 2004;45(7):868–71. 10.1111/j.0013-9580.2004.05504.x [DOI] [PubMed] [Google Scholar]
- 133. Endo A, Fujita Y, Fuchigami T, et al. : Fanconi syndrome caused by valproic acid. Pediatr Neurol. 2010;42(4):287–90. 10.1016/j.pediatrneurol.2009.12.003 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 134. Wegienka LC, Weller JM: Renal tubular acidosis caused by degraded tetracycline. Arch Intern Med. 1964;114(2):232–5. 10.1001/archinte.1964.03860080082007 [DOI] [PubMed] [Google Scholar]
- 135. Cleveland WW, Adams WC, Mann JB, et al. : Acquired Fanconi syndrome following degraded tetracycline. J Pediatr. 1965;66(2):333–42. 10.1016/S0022-3476(65)80190-1 [DOI] [PubMed] [Google Scholar]
- 136. Montoliu J, Carrera M, Darnell A, et al. : Lactic acidosis and Fanconi's syndrome due to degraded tetracycline. Br Med J (Clin Res Ed). 1981;283(6306):1576–7. 10.1136/bmj.283.6306.1576-a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. Izzedine H, Launay-Vacher V, Isnard-Bagnis C, et al. : Drug-induced Fanconi's syndrome. Am J Kidney Dis. 2003;41(2):292–309. 10.1053/ajkd.2003.50037 [DOI] [PubMed] [Google Scholar]
- 138. Banerjee S, Narayanan M, Gould K: Monitoring aminoglycoside level. BMJ. 2012;345:e6354. 10.1136/bmj.e6354 [DOI] [PubMed] [Google Scholar]
- 139. Grangé S, Bertrand DM, Guerrot D, et al. : Acute renal failure and Fanconi syndrome due to deferasirox. Nephrol Dial Transplant. 2010;25(7):2376–8. 10.1093/ndt/gfq224 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 140. Papadopoulos N, Vasiliki A, Aloizos G, et al. : Hyperchloremic metabolic acidosis due to deferasirox in a patient with beta thalassemia major. Ann Pharmacother. 2010;44(1):219–21. 10.1345/aph.1M440 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 141. Rafat C, Fakhouri F, Ribeil JA, et al. : Fanconi syndrome due to deferasirox. Am J Kidney Dis. 2009;54(5):931–4. 10.1053/j.ajkd.2009.03.013 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 142. Murphy N, Elramah M, Vats H, et al. : A case report of deferasirox-induced kidney injury and Fanconi syndrome. WMJ. 2013;112(1):177–80. [PubMed] [Google Scholar]; F1000 Recommendation
- 143. Dell'Orto VG, Bianchetti MG, Brazzola P: Hyperchloraemic metabolic acidosis induced by the iron chelator deferasirox: a case report and review of the literature. J Clin Pharm Ther. 2013;38(6):526–7. 10.1111/jcpt.12095 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 144. Häring N, Mähr HS, Mündle M, et al. : Early detection of renal damage caused by fumaric acid ester therapy by determination of urinary β2-microglobulin. Br J Dermatol. 2011;164(3):648–51. 10.1111/j.1365-2133.2010.10171.x [DOI] [PubMed] [Google Scholar]
- 145. Rago RP, Miles JM, Sufit RL, et al. : Suramin-induced weakness from hypophosphatemia and mitochondrial myopathy. Association of suramin with mitochondrial toxicity in humans. Cancer. 1994;73(7):1954–9. [DOI] [PubMed] [Google Scholar]
- 146. François H, Coppo P, Hayman JP, et al. : Partial fanconi syndrome induced by imatinib therapy: a novel cause of urinary phosphate loss. Am J Kidney Dis. 2008;51(2):298–301. 10.1053/j.ajkd.2007.10.039 [DOI] [PubMed] [Google Scholar]
- 147. Launay-Vacher V, Izzedine H, Karie S, et al. : Renal tubular drug transporters. Nephron Physiol. 2006;103(3):p97–106. 10.1159/000092212 [DOI] [PubMed] [Google Scholar]
- 148. Ghiculescu RA, Kubler PA: Aminoglycoside-associated Fanconi syndrome. Am J Kidney Dis. 2006;48(6):e89–93. 10.1053/j.ajkd.2006.08.009 [DOI] [PubMed] [Google Scholar]
- 149. Gainza FJ, Minguela JI, Lampreabe I: Aminoglycoside-associated Fanconi's syndrome: an underrecognized entity. Nephron. 1997;77(2):205–11. 10.1159/000190274 [DOI] [PubMed] [Google Scholar]
- 150. Lopez-Novoa JM, Quiros Y, Vicente L, et al. : New insights into the mechanism of aminoglycoside nephrotoxicity: an integrative point of view. Kidney Int. 2011;79(1):33–45. 10.1038/ki.2010.337 [DOI] [PubMed] [Google Scholar]