Abstract
IMPORTANCE
The 2013 American College of Cardiology/American Heart Association (ACC/AHA) guidelines for cholesterol management defined new eligibility criteria for statin therapy. However, it is unclear whether this approach improves identification of adults at higher risk of cardiovascular events.
OBJECTIVE
To determine whether the ACC/AHA guidelines improve identification of individuals who develop incident cardiovascular disease (CVD) and/or have coronary artery calcification (CAC) compared with the National Cholesterol Education Program’s 2004 Updated Third Report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (ATP III) guidelines.
DESIGN, SETTING, AND PARTICIPANTS
Longitudinal community-based cohort study, with participants for this investigation drawn from the offspring and third-generation cohorts of the Framingham Heart Study. Participants underwent multidetector computed tomography for CAC between 2002 and 2005 and were followed up for a median of 9.4 years for incident CVD.
EXPOSURES
Statin eligibility was determined based on Framingham risk factors and low-density lipoprotein thresholds for ATP III, whereas the pooled cohort calculator was used for ACC/AHA.
MAIN OUTCOMES AND MEASURES
The primary outcome was incident CVD (myocardial infarction, death due to coronary heart disease [CHD], or ischemic stroke). Secondary outcomes were CHD and CAC (as measured by the Agatston score).
RESULTS
Among 2435 statin-naive participants (mean age, 51.3 [SD, 8.6] years; 56% female), 39% (941/2435) were statin eligible by ACC/AHA compared with 14% (348/2435) by ATP III (P < .001). There were 74 incident CVD events (40 nonfatal myocardial infarctions, 31 nonfatal ischemic strokes, and 3 fatal CHD events). Participants who were statin eligible by ACC/AHA had increased hazard ratios for incident CVD compared with those eligible by ATP III: 6.8 (95% CI, 3.8–11.9) vs 3.1 (95% CI, 1.9–5.0), respectively (P <.001). Similar results were seen for CVD in participants with intermediate Framingham Risk Scores and for CHD. Participants who were newly statin eligible (n = 593 [24%]) had an incident CVD rate of 5.7%, yielding a number needed to treat of 39 to 58. Participants with CAC were more likely to be statin eligible by ACC/AHA than by ATP III: CAC score >0 (n = 1015): 63% vs 23%; CAC score >100 (n = 376): 80% vs 32%; and CAC score >300 (n = 186): 85% vs 34% (all P < .001). A CAC score of 0 identified a low-risk group among ACC/AHA statin-eligible participants (306/941 [33%]) with a CVD rate of 1.6%.
CONCLUSIONS AND RELEVANCE
In this community-based primary prevention cohort, the ACC/AHA guidelines for determining statin eligibility, compared with the ATP III, were associated with greater accuracy and efficiency in identifying increased risk of incident CVD and subclinical coronary artery disease, particularly in intermediate-risk participants.
Efforts toward preventing cardiovascular disease (CVD) have focused on the treatment of traditional risk factors, including the management of blood cholesterol with preventive low-density lipoprotein cholesterol (LDL-C)–lowering statin therapy by using risk-based LDL-C cut points according to the National Cholesterol Education Program’s 2001 and 2004 Updated Third Report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (ATP III) cholesterol treatment guidelines.1–3
The recently released 2013 American College of Cardiology/American Heart Association (ACC/AHA) guidelines for the management of blood cholesterol4,5 represent a shift in the treatment approach for the primary prevention of CVD, focusing on absolute cardiovascular risk as estimated by the 10-year atherosclerotic CVD (ASCVD) score for statin treatment.
However, concerns about this more comprehensive approach to preventive therapy have been raised.6,7 A recent investigation based on extrapolation of the National Health and Nutrition Examination Survey cohort revealed that the new ACC/AHA guidelines would result in 12.8 million more adults being eligible for statin treatment compared with the ATP III guidelines.8 The proposition is that the new guidelines more accurately identify those who will experience cardiovascular events, that this constitutes an improvement over previous guidelines, and that the potential risks of providing statin therapy to more people are outweighed by these benefits.
Another marker to assess the new guidelines may be the alignment of statin eligibility with the presence and extent of subclinical coronary atherosclerosis, measured as coronary artery calcification (CAC), as asymptomatic adults who have high CAC (Agatston score >300) experience a nearly 10-fold higher incidence of coronary events.9
Hence, we compared the efficiency and accuracy of the ATP III and the ACC/AHA guidelines eligibility criteria for statin therapy to identify participants at higher risk of incident CVD in a large, prospective, community-based asymptomatic cohort in the Framingham Heart Study (FHS).
Methods
Details regarding the FHS population, selection criteria, and design of the Framingham multidetector computed tomography (MDCT) imaging study and the method of calcium measurement have been published and described elsewhere.10–13
Study Population
Participants in this study were drawn from the offspring and the third-generation cohorts of the FHS, who underwent MDCT between 2002 and 2005. Participants in the analysis attended the offspring seventh examination cycle (1998–2001) or third-generation first examination cycle (2002–2005). Inclusion in the MDCT study was weighted toward participants from larger FHS families and those residing in the greater New England area. We included men aged 35 years or older and women aged 40 years or older who were not pregnant. All participants weighed 350 lb (157.5 kg) or less. We excluded participants with prevalent CVD, defined as prior stroke, congestive heart failure, myocardial infarction, coronary insufficiency, coronary artery bypass graft surgery, valve replacement, or percutaneous coronary stent placement, as well as participants who were taking lipid-lowering therapy at baseline. Race and ethnicity were self-reported.
Cholesterol levels in this article are reported in milligrams per deciliter. To convert to millimoles per liter, multiply by 0.0259.
The institutional review boards of Boston University Medical Center and Massachusetts General Hospital approved the study. All participants provided written informed consent.
Determination of Eligibility for Statin Therapy
Risk Factor Measurement
Adult-onset diabetes was defined as a fasting glucose level of 126 mg/dL (7 mmol/L) or higher or treatment with either insulin or a hypoglycemic agent. Participants were considered to be current smokers if they smoked 1 or more cigarettes per day for the last year. Blood pressure was measured in the left arm of the seated participant using a standardized protocol. Systolic and diastolic blood pressures were obtained using standardized protocols. Hypertension was defined as systolic blood pressure 140 mm Hg or higher, diastolic blood pressure 90 mm Hg or higher, or use of antihypertensive drug treatment. Total and high-density lipoprotein cholesterol measurements were obtained using standardized protocols as previously reported.
2004 ATP III Guidelines
To assess whether primary prevention statin treatment was indicated per the 2004 ATP III guidelines, we applied the algorithm based on risk factors, the Framingham Risk Score (FRS), and LDL-C cutoff levels.2,3 Specifically, participants were considered statin eligible if they met at least 1 of the following criteria: (1) LDL-C level 100 mg/dL or higher and diabetes mellitus or peripheral arterial disease or 10-year FRS for coronary heart disease (CHD) of 20% or higher; (2) LDL-C level 130 mg/dL or higher and FRS greater than 10% but less than 20% and 2 or more risk factors; (3) LDL-C level 160 mg/dL or higher and FRS of less than 10% and 2 or more risk factors; or (4) LDL-C level 190 mg/dL or higher and fewer than 2 risk factors. Risk factors in this algorithm included cigarette smoking, hypertension (blood pressure ≥140/90 mm Hg or taking antihypertensive medication), low high-density lipoprotein cholesterol (<40 mg/dL), family history of premature CHD (CHD in male first-degree relative <55 years of age; CHD in female first-degree relative <65 years of age), and age (men ≥45 years; women ≥55 years).
2013 ACC/AHA Guidelines
For the 2013 ACC/AHA guidelines, we identified candidates for statin treatment based on 4 delineated benefit groups outlined in the guidelines9: (1) clinical ASCVD; (2) LDL-C level 190 mg/dL or higher; (3) diabetes diagnosed between ages 40 and 75 years and LDL-C level of 70 to 189 mg/dL; or (4) no clinical ASCVD or diabetes, LDL-C level of 70 to 189 mg/dL, and estimated ASCVD risk of 7.5% or higher. Risk of ASCVD was determined using the pooled cohort calculator.4,5
Imaging for CAC
Participants under went electrocardiographically triggered non–contrast-enhanced cardiac CT on an 8-slice MDCT scanner (LightSpeed Ultra, General Electric) during a breath hold.14
The effective radiation exposure was 1.0 to 1.25 mSv. The amount of CAC was quantified independently by experienced readers using dedicated offline workstations (Aquarius, Terarecon) and expressed as the typical Agatston score.15
CVD Outcomes
In the FHS, CVD in previous risk algorithms was defined as CHD (ie, a fatal coronary event, myocardial infarction) or a cerebrovascular event (ie, ischemic stroke, hemorrhagic stroke).16 For the purpose of this study, incident CHD events included recognized myocardial infarction and death due to CHD, while incident CVD included incident CHD events and ischemic stroke, in accordance with the ASCVD end points defined in the 2013 ACC/AHA risk assessment guidelines.5
Participants were contacted annually for telephone follow-up. If a participant reported that he/she saw a physician, visited an emergency department, or was admitted to the hospital, all medical records from practitioners, hospitals, imaging centers, rehabilitation centers, and nursing homes were procured for review. This information included medical histories, physical examinations at the study clinic, hospitalization records, and communication with personal physicians. All suspected new events were reviewed by a panel of 3 experienced investigators who evaluated all pertinent medical records. The final date of follow-up was December 31, 2013, for both cohorts. A separate review committee including a panel of 3 investigators (at least 2 neurologists) adjudicated cerebrovascular events.
Statistical Analysis
Descriptive statistics are presented as means and standard deviations or percentages of participants; medians and quartiles are also presented for CAC. We compared the proportion of participants eligible for statin treatment using ATP III vs ACC/AHA guideline criteria using the McNemar test.
The primary end point was incident CVD. Secondary end points were incident CHD and CAC. The proportional hazards assumption for major CVD and CHD was tested using the Kolmogorov-type supremum test. Univariate Cox proportional hazards regression models to relate statin eligibility to time to events were carried out for each guideline. Our primary outcome was the difference between the 2 guidelines’ eligible vs noneligible hazard ratios (HRs) for incident CVD via comparison of the Cox β coefficients. Kaplan-Meier curves of cumulative CVD incidence are presented by eligibility status for each guideline; the curves were compared using the log-rank test. Cox analysis was repeated for subgroups of participants according to sex and intermediate CVD risk (FRS 6%–20%). We also assessed whether there were significant interactions of eligibility status with cohort (offspring [second generation] vs third generation) on time to events using separate Cox models with main effects for eligibility and cohort and with the eligibility-by-cohort interaction effect.
To determine whether statin eligibility accurately identified participants with CAC, we used logistic regression to relate statin eligibility to outcomes of CAC Agatston scores greater than 0, greater than 100, and greater than 300. The logistic regression β coefficient for statin eligibility was exponentiated to obtain the odds ratio (OR) of statin eligibility vs noneligibility with respect to these CAC outcomes.
Analyses were performed with the use of SAS software, version 9.4 (SAS Institute Inc). Two-sided P <.05 was considered statistically significant.
Efficiency was evaluated as number needed to treat of newly statin-eligible participants to prevent 1 incident CVD event.
Results
Study Population
Of the 7634 participants in the offspring and third-generation FHS cohorts, 4105 were not included in the MDCT study. Of the 3529 participants undergoing MDCT, 3505 attended offspring examination 7 or third-generation examination 1, and 3496 of these had evaluable results for CAC. Of these, 3016 were between ages 40 and 75 years inclusive, of whom 2565 were not taking lipid-lowering therapy. Of these, 2477 were free of any CVD and 2435 of these had a complete risk factor profile. Thus, the study population consisted of 2435 participants.
Participants were aged a mean of 51.3 (SD, 8.6) years, 56% were women, and the mean FRS was 6.7% (Table 1). The mean LDL-C level was 121 mg/dL and the mean CAC score was 95 (median, 0; interquartile range, 0–30.4), with 42% of participants having a CAC score greater than 0. The population was overwhelmingly white.
Table 1.
Baseline Participant Characteristics
| Characteristics | Total (n = 2435) | No Incident Cardiovascular Disease (n = 2361) | Incident Cardiovascular Disease (n = 74) |
|---|---|---|---|
| Age, mean (SD), y | 51.3 (8.6) | 51.1 (8.5) | 57.7 (9.4) |
| Female, No. (%) | 1355 (55.6) | 1328 (56.2) | 27 (36.5) |
| Traditional risk factors, No. (%) | |||
| Hypertension | 616 (25.3) | 588 (24.9) | 28 (37.8) |
| Smoking | 318 (13.1) | 297 (12.6) | 21 (28.4) |
| Diabetes mellitus | 101 (4.1) | 92 (3.9) | 9 (12.2) |
| Family history of premature coronary heart diseasea | 424 (22.1) | 403 (21.7) | 21 (35.6) |
| Lipid levels, mean (SD), mg/dL | |||
| Total cholesterol | 199 (34) | 199 (35) | 204 (30) |
| Low-density lipoprotein cholesterol | 121 (32) | 120 (32) | 128 (30) |
| High-density lipoprotein cholesterol | 56 (17) | 56 (17) | 48 (14) |
| Antihypertensive medications, No. (%) | 353 (14.5) | 336 (14.2) | 17 (23.0) |
| Framingham Risk Score, mean (SD) | 6.6 (5.7) | 6.4 (5.5) | 12.7 (8.9) |
| Coronary artery calcification score | |||
| Mean (SD) | 93.3 (338) | 84.3 (324) | 380 (560) |
| Median (interquartile range) | 0 (0–28.8) | 0 (0–30.4) | 170 (3–500) |
| No. (%) with score >0 | 1015 (41.7) | 957 (40.5) | 58 (78.4) |
SI conversions: To convert total, low-density lipoprotein, and high-density lipoprotein cholesterol to mmol/L, multiply by 0.0259.
Family history status is based on a sample size of 1984 in whom definitive family history information was collected.
Outcomes
The median follow-up was 9.4 (interquartile range, 8.1–10.1) years. There were a total of 74 (3.0%) incident CVD events (40 nonfatal myocardial infarctions, 31 nonfatal strokes, and 3 with fatal CHD) and 43 (1.8%) incident CHD events (40 nonfatal myocardial infarctions and 3 with fatal CHD) (Table 2).
Table 2.
Identification of Incident CVD and Incident Major CHD by Statin Eligibility: Observed Event Rates and Hazards Ratios Stratified by Statin Allocation Recommendation According to 2004 ATP III vs 2013 ACC/AHA Guidelines
| Incident CVD
|
Incident Major CHD
|
|||||
|---|---|---|---|---|---|---|
| No. of Events/Sample Size (%) | Hazard Ratio (95% CI) | P Value | No. of Events/Sample Size (%) | Hazard Ratio (95% CI) | P Value | |
| Overalla | 74/2435 (3.0) | 43/2446 (1.8) | ||||
|
| ||||||
| 2004 ATP III guidelines | ||||||
|
| ||||||
| Statin eligible | 24/348 (6.9) | 3.1 (1.9–5.0) | <.001 | 15/355 (4.2) | 3.3 (1.8–6.2) | <.001 |
|
| ||||||
| Not statin eligible | 50/2087 (2.4) | 1 [Reference] | 28/2091 (1.3) | 1 [Reference] | ||
|
| ||||||
| 2013 ACC/AHA guidelines | ||||||
|
| ||||||
| Statin eligible | 59/941 (6.3) | 6.8 (3.8–11.9) | <.001 | 36/952 (3.8) | 8.6 (3.8–19.3) | <.001 |
|
| ||||||
| Not statin eligible | 15/1494 (1.0) | 1 [Reference] | 7/1494 (0.5) | 1 [Reference] | ||
|
| ||||||
| P value for ATP III vs ACC/AHA | <.001 | .004 | ||||
Abbreviations: ACC/AHA, American College of Cardiology/American Heart Association; ATP III, Updated Third Report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults; CHD, coronary heart disease; CVD, cardiovascular disease.
Median follow-up was 9.4 (interquartile range, 8.1–10.1) years for both incident CVD and incident major CHD.
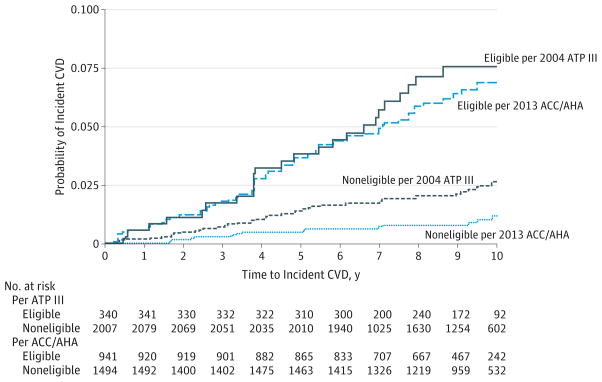
Guideline-Based Statin Eligibility and Incident CVD
Overall, more participants were eligible for statin treatment when applying the ACC/AHA guidelines compared with the ATP III guidelines (39% [941/2435] vs 14% [348/2435], respectively; P < .001). Among those eligible for statin treatment by the ATP III guidelines, 6.9% (24/348) developed incident CVD compared with 2.4% (50/2087) among noneligible participants (HR, 3.1; 95% CI, 1.9–5.0; P < .001). Applying the ACC/AHA guidelines, among those eligible for statin treatment, 6.3% (59/941) developed incident CVD compared with only 1.0% (15/1494) among those not eligible (HR, 6.8; 95% CI, 3.8–11.9; P < .001). Therefore, the HR of having incident CVD among statin-eligible vs noneligible participants was significantly higher when applying the ACC/AHA guidelines’ statin eligibility criteria compared with the ATP III guidelines (P < .001) (Figure 1). Adjustment for statin treatment at subsequent examinations as well as for aspirin and antihypertensive therapy did not attenuate these results. Also, excluding participants with LDL-C levels greater than 190 mg/dL and/or diabetes mellitus did not attenuate these results (eTable 1 in the Supplement). There were no significant interactions of eligibility status with cohort (offspring vs third generation), and eligibility trends were similar across cohorts (eTable 2 in the Supplement).
Figure 1. Kaplan-Meier Survival Curves for Incident CVD Stratified by Whether Participants Were Eligible for Statin Therapy per 2004 ATP III Guidelines and 2013 ACC/AHA Guidelines.
ACC/AHA, American College of Cardiology/American Heart Association; ATP III, Updated Third Report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults; CVD, cardiovascular disease. Log-rank P <.001 for statin eligible vs statin ineligible for both ATP III and ACC/AHA guidelines.
Statin Eligibility and Incident CVD in Subgroups
We further analyzed whether similar findings could be observed in specific subgroups including women and those traditionally considered at intermediate CVD risk (FRS 6%–20%)
Sex-Based Stratification
Among women, there was a total of 2.0% incident CVD (27/1355), whereas among men, there was a total of 4.4% incident CVD (47/1080). Using the ATP III guidelines, among women eligible for statin treatment, 3.5% (4/114) developed incident CVD compared with 1.9% (23/1241) of noneligible women (HR, 2.1; 95% CI, 0.7–6.0; P = .18). Applying the ACC/AHA guidelines, among women eligible for statin treatment, 5.8% (18/310) developed incident CVD compared with 0.9% (9/1045) among noneligible women (HR, 7.4; 95% CI, 3.3–16.5; P < .001).
Therefore, the risk of incident CVD among statin-eligible vs noneligible women was significantly higher when applying the ACC/AHA guidelines’ statin eligibility criteria compared with the ATP III guidelines (P < .001).
For men (n = 1080), using the ATP III guidelines, among those eligible for statin treatment, 8.5% (20/234) developed incident CVD compared with 3.2% (27/846) of noneligible men (HR, 2.8; 95% CI, 1.6–5.0; P < .001). Applying the ACC/AHA guidelines, among those eligible for statin treatment, 6.5% (41/631) developed incident CVD compared with 1.3% (6/449) among noneligible men (HR, 5.2; 95% CI, 2.2–12.2; P < .001). However, despite the large difference in HRs among men, the risk of incident CVD for statin-eligible vs noneligible participants was not significantly higher when applying the ACC/AHA guidelines’ statin eligibility criteria compared with the ATP III guidelines for men (P = .15), in part because of the smaller sample size.
Intermediate-Risk Participants
Approximately one-third of the overall population (38% [918/2435]) was at intermediate CVD risk (FRS 6%–20%), 36 (3.9%) of whom experienced incident CVD. Baseline characteristics of the intermediate-risk group were similarly distributed between those with and without future CVD events, although CAC was significantly higher in those experiencing events (eTable 3 in the Supplement). Most participants (80% [734/918]) at intermediate risk were eligible for statin treatment by the ACC/AHA guidelines compared with only 27% (251/918) by the ATP III guidelines (P < .001). For the ATP III guidelines, there was no significant difference between statin-eligible and noneligible participants for incident CVD (3.6% [9/251] among those eligible for statins vs 4.0% [27/667] among those not eligible; HR, 0.9; 95% CI, 0.4–1.9; P = .77). There was a significantly higher incidence of CVD among ACC/AHA statin-eligible than noneligible participants (4.8% [35/734] among those eligible for statins vs 0.5% [1/184] among those not eligible; HR, 9.3; 95% CI, 1.3–67.8; P = .03). Therefore, the risk of incident CVD among statin-eligible vs noneligible intermediate-risk participants was significantly higher when applying the ACC/AHA guidelines’ statin eligibility criteria compared with the ATP III guidelines (P = .02).
Guideline-Based Statin Eligibility and Incident CHD
Similar findings were noted for incident CHD. Using the ATP III guidelines, among those eligible for statin treatment, 4.2% (15/355) developed incident CHD, and among those not eligible, 1.3% (28/2091) developed incident CHD (HR, 3.3; 95% CI, 1.8–6.2; P < .001). In contrast, using the ACC/AHA guidelines, among those eligible for statin treatment, 3.8% (36/952) developed incident CHD, and among those not eligible, only 0.5% (7/1494) developed incident CHD (HR, 8.6; 95% CI, 3.8–19.3; P < .001). Therefore, the risk of incident CHD among statin-eligible vs noneligible participants was significantly higher when applying the ACC/AHA guidelines’ statin eligibility criteria compared with the ATP III guidelines (P = .004).
Efficiency of Treatment in Newly Statin-Eligible Participants
There were 593 newly statin-eligible participants per the 2013 ACC/AHA guidelines. These participants had an incident CVD rate of 5.7%. Assuming a relative risk reduction of 30% to 45%,17 this yields a number needed to treat of 39 to 58 newly eligible statin participants to prevent 1 CVD event over 9.4 years of follow-up.
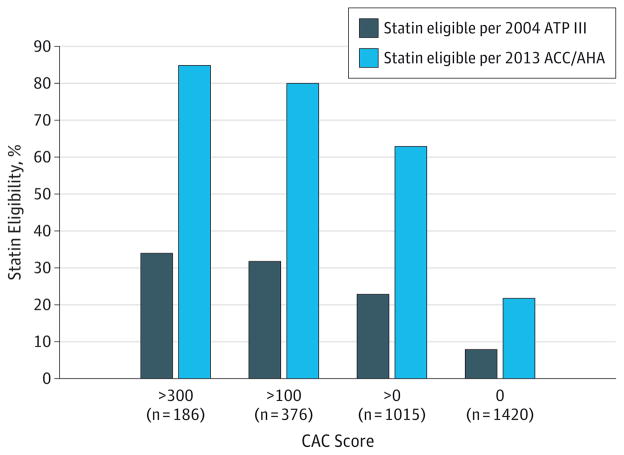
Statin Eligibility and Subclinical Coronary Artery Disease
Of the 2435 participants, 1015 (42%) had CAC scores greater than 0 and 186 (8%) had very high CAC scores (≥300). As shown in Figure 2, in those with CAC scores greater than 0, significantly more participants were eligible for statin treatment with the ACC/AHA guidelines compared with the ATP III guidelines (63% [635/1015] vs 23% [238/1015], respectively; P < .001). Among participants with CAC scores of 300 or greater (7.6% [186/2435]), who were at the highest risk of incident CVD (8.5% CVD event rate), most participants (85% [158/186]) were identified as eligible for statins with the ACC/AHA guidelines compared with only 34% (64/186) with the ATP III guidelines (P < .001). Similarly, among participants with CAC scores of greater than 100 (15% [376/2435]), most participants (80% [300/376]) were identified as eligible for statins with the ACC/AHA guideline compared with only 32% (122/376) with the ATP III guideline (P <.001). Among participants without CAC, 8% (110/1420) were eligible for statins with the ATP III guidelines vs 22% (306/1420) with the ACC/AHA guidelines (P < .001).
Figure 2. Prevalence of Coronary Artery Calcification Among Participants Identified as Candidates for Statin Therapy by the 2004 ATP III Guidelines vs the 2013 ACC/AHA Guidelines.
ACC/AHA, American College of Cardiology/American Heart Association; ATP III, Updated Third Report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults; CAC, coronary artery calcification.
CAC Scores Greater Than 0
Using the ATP III guidelines, among those eligible for statins, 68% (238/348) had CAC scores greater than 0 while among those not eligible, 37% (777/2087) had CAC scores greater than 0 (OR, 3.7; 95% CI, 2.9–4.7; P < .001) (Table 3). In contrast, using the ACC/AHA guidelines, among those eligible for statins, 68% (635/941) had CAC scores greater than 0 and among those not eligible, only 25% (380/1494) had CAC scores greater than 0 (OR, 6.1; 95% CI, 5.1–7.3; P < .001).
Table 3.
Identification of CAC Scores Greater Than 0, 100, and 300 by Statin Eligibility: Observed Event Rates and Odds Ratios Stratified by Statin Allocation Recommendation According to 2004 ATP III vs 2013 ACC/AHA Guidelines
| CAC Score >0
|
CAC Score >100
|
CAC Score >300
|
|||||||
|---|---|---|---|---|---|---|---|---|---|
| No. of Events/Sample Size (%) | Odds Ratio (95% CI) | P Value | No. of Events/Sample Size (%) | Odds Ratio (95% CI) | P Value | No. of Events/Sample Size (%) | Odds Ratio (95% CI) | P Value | |
| Overall | 1015/2435 (42) | 376/2435 (15) | 186/2435 (7.6) | ||||||
|
| |||||||||
| 2004 ATP III guidelines | |||||||||
|
| |||||||||
| Statin eligible | 238/348 (68) | 3.7 (2.9–4.7) | <.001 | 122/348 (35) | 3.9 (3.0–5.0) | <.001 | 64/348 (18) | 3.6 (2.6–5.0) | <.001 |
|
| |||||||||
| Not statin eligible | 777/2087 (37) | 1 [Reference] | 254/2087 (12) | 1 [Reference] | 122/2087 (5.8) | 1 [Reference] | |||
|
| |||||||||
| 2013 ACC/AHA guidelines | |||||||||
|
| |||||||||
| Statin eligible | 635/941 (68) | 6.1 (5.1–7.3) | <.001 | 300/941 (32) | 8.7 (6.7–11) | <.001 | 158/941 (17) | 11 (7.0–16) | <.001 |
|
| |||||||||
| Not statin eligible | 380/1494 (25) | 1 [Reference] | 76/1494 (5.1) | 1 [Reference] | 28/1494 (1.9) | 1 [Reference] | |||
|
| |||||||||
| P value for ATP III vs ACC/AHA | <.001 | <.001 | <.001 | ||||||
Abbreviations: ACC/AHA, American College of Cardiology/American Heart Association; ATP III, Updated Third Report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults; CAC coronary artery calcification.
CAC Scores Greater Than 100
Using the ATP III guidelines, among those eligible for statins, 35% (122/348) had CAC scores greater than 100 while among those not eligible, 12% (254/2087) had CAC scores greater than 100 (OR, 3.9; 95% CI, 3.0–5.0; P < .001). In contrast, using the ACC/AHA guidelines, among those eligible for statins, 32% (300/941) had CAC scores greater than 100 and for those not eligible, only 5.1% (76/1494) had CAC scores greater than 100 (OR, 8.7; 95% CI, 6.7–11; P < .001).
CAC Scores Greater Than 300
Using the ATP III guidelines, among those eligible for statins, 18% (64/348) had CAC scores greater than 300 while among those not eligible, 5.8% (122/2087) had CAC scores greater than 300 (OR, 3.6; 95% CI, 2.6–5.0; P < .001). In contrast, using the ACC/AHA guidelines, among those eligible for statins, 17% (158/941) had CAC scores greater than 300 and among those not eligible, only 1.9% (28/1494) had CAC scores greater than 300 (OR, 11; 95% CI, 7.0–16; P < .001).
Therefore, the risk of having CAC scores greater than 0, 100, or 300 among statin-eligible vs noneligible participants was significantly higher when applying the ACC/AHA guidelines’ statin eligibility criteria compared with the ATP III guidelines (P < .001).
CAC Scores of 0
There were 348 statin-eligible participants by the ATP III guidelines and 941 statin-eligible participants by the ACC/AHA guidelines. Of these, 110 (32%) and 306 (33%), respectively, had CAC scores of 0, of whom 1.8% (2/110) and 1.6% (5/306) had incident CVD events. Importantly, adding CAC as a noneligibility criterion for statin therapy did not increase the incidence of CVD events in this group (ACC/AHA: 1.0% vs 1.1%; ATP III: 2.4% vs 2.4%) (eTable 4 in the Supplement).
Discussion
In this community-based primary prevention cohort, we demonstrate that the risk of incident CVD among statin-eligible vs noneligible participants is significantly higher when applying the ACC/AHA guidelines’ statin eligibility criteria compared with the ATP III guidelines. This finding is consistent across subgroups and particularly important in participants at intermediate CVD risk on the FRS, the most challenging group in clinical practice for whom to decide to initiate statin therapy.
Prior studies evaluating the ACC/AHA guidelines in various cohorts have focused on statin allocation, showing a substantial increase in the adult population eligible for statin therapy. For example, an analysis of the National Health and Nutrition Examination Survey cohort found that the new guidelines would increase the number of US adults between ages 40 and 75 years eligible for statin therapy from 43 million to 56 million because the vast majority of reclassification occurred toward new statin eligibility compared with the ATP-III guidelines.8 We extend these findings to an older white population and to important subgroups such as those at intermediate risk of events, in which risk factors are similar between those with and without future CVD events.
In addition, this study complements other studies that suggest that the application of the ACC/AHA guidelines will have a favorable effect on ASCVD prevention with reasonable efficiency of statin use compared with the prior ATP III recommendations.17 Extrapolating our findings to the approximately 10 million US adults who are newly eligible for statins, we estimate that between 41 000 and 63 000 incident CVD events would be prevented over a 10-year period by adopting the ACC/AHA guidelines.
By demonstrating a simultaneously improved matching of statin-eligible participants with the presence and extent of subclinical atherosclerosis (CAC), we provide a mechanistic link between absolute cardiovascular risk, expressed as 10-year ASCVD risk score, and subsequent incident CVD. These findings support prior cohort studies that have found that general cardiovascular risk, much more than LDL-C levels, is associated with CAC.18–20 The improvement with the new ACC/AHA guidelines in identifying subclinical atherosclerosis is consistent with a recent study of 3076 participants in which the ACC/AHA guidelines provided better discrimination of those with significant coronary artery plaque on cardiac CT angiography.21 Analogous to their finding that participants with 50% or greater coronary stenosis were more frequently assigned statin therapy with the ACC/AHA guidelines than the ATP III guidelines (90% vs 60%, respectively), we show that those with high-risk CAC scores (>300) are more frequently allocated statin therapy with the ACC/AHA guidelines compared with the ATP III guidelines (85% vs 34%, respectively), and the HR among those with CAC scores greater than 300 for being statin eligible vs noneligible with the ACC/AHA guidelines is considerably higher than with the ATP III guidelines (HRs, 11 vs 3.6, respectively).
Although our analyses suggest that adherence to new ACC/AHA statin eligibility guidelines may prove beneficial for the reduction of future cardiovascular events compared with using the ATP III guidelines, the absolute event risk of statin-noneligible adults is not much lower with the ACC/AHA guidelines (1.0%) compared with the ATP III guidelines (2.4%), and the larger benefit may be that the ACC/AHA guidelines identify many more statin-eligible participants with a similarly high event rate as the ATP III guidelines (6.3% vs 6.9%). In addition, a risk-benefit analysis considering costs and potential adverse effects of statins, especially in patients with prediabetes and in lower-risk patients, is needed to provide a complete assessment of the effects of the change in statin eligibility guidelines on the health care system.
Our study has limitations. The relatively small number of events is a limitation. Results in white Americans may not be generalizable to other ethnic groups; it should be noted that the reported significant differences in associations among risk factors, CAC, and outcomes in whites compared with other ethnic groups suggest that ethnic group specific prediction rules may be required.22,23 In addition, complete family history of premature coronary artery disease was available in 78% of participants. However, analyses of statin eligibility were conservative and assumed no family history if complete data were not available. Furthermore, sensitivity analyses examining only the cohort with complete family history data yielded nearly identical results (eTable 5 in the Supplement).
Conclusions
In this community-based primary prevention cohort, the ACC/AHA guidelines for determining statin eligibility, compared with the ATP III guidelines, were associated with greater accuracy and efficiency in identifying increased risk of incident CVD events and presence of subclinical coronary artery disease, particularly in those at intermediate risk.
Supplementary Material
Acknowledgments
Funding/Support: This work was supported by the National Heart, Lung, and Blood Institute’s Framingham Heart Study (contracts N01-HC-25195, HL076784, AG028321, HL070100, HL060040, HL080124, HL071039, HL077447, and HL107385). Dr Pursnani was supported by National Institutes of Health grant T32 HL076136.
Glossary
- ASCVD
atherosclerotic cardiovascular disease
- CAC
coronary artery calcification
- CHD
coronary heart disease
- FRS
Framingham Risk Score
- LDL-C
low-density lipoprotein cholesterol
- MDCT
multidetector computed tomography
Footnotes
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Dr Hoffmann reports receipt of grants from HeartFlow Inc, Siemens Healthcare, Genentech, and the American College of Radiology Imaging Network and personal fees from the American Heart Association. No other disclosures were reported.
Role of the Funder/Sponsor: The National Institutes of Health had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Author Contributions: Dr Hoffmann had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Pursnani, O’Donnell, Hoffmann.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Pursnani, O’Donnell, Hoffmann.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Pursnani, Massaro, D’Agostino.
Obtained funding: D’Agostino, O’Donnell, Hoffmann.
Administrative, technical, or material support: Hoffmann.
Study supervision: Pursnani, O’Donnell, Hoffmann.
References
- 1.Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) JAMA. 2001;285(19):2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 2.National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106(25):3143–3421. [PubMed] [Google Scholar]
- 3.Grundy SM, Cleeman JI, Merz CN, et al. Coordinating Committee of the National Cholesterol Education Program. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. J Am Coll Cardiol. 2004;44(3):720–732. doi: 10.1016/j.jacc.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 4.Stone NJ, Robinson J, Lichtenstein AH, et al. American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25 pt B):2889–2934. doi: 10.1016/j.jacc.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 5.Goff DC, Jr, Lloyd-Jones DM, Bennett G, et al. American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25 pt B):2935–2959. doi: 10.1016/j.jacc.2013.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guallar E, Laine C. Controversy over clinical guidelines: listen to the evidence, not the noise. Ann Intern Med. 2014;160(5):361–362. doi: 10.7326/M14-0112. [DOI] [PubMed] [Google Scholar]
- 7.Martin SS, Blumenthal RS. Concepts and controversies: the 2013 American College of Cardiology/American Heart Association risk assessment and cholesterol treatment guidelines. Ann Intern Med. 2014;160(5):356–358. doi: 10.7326/M13-2805. [DOI] [PubMed] [Google Scholar]
- 8.Pencina MJ, Navar-Boggan AM, D’Agostino RB, Sr, et al. Application of new cholesterol guidelines to a population-based sample. N Engl J Med. 2014;370(15):1422–1431. doi: 10.1056/NEJMoa1315665. [DOI] [PubMed] [Google Scholar]
- 9.Detrano R, Guerci AD, Carr JJ, et al. Coronary calcium as a predictor of coronary events in 4 racial or ethnic groups. N Engl J Med. 2008;358(13):1336–1345. doi: 10.1056/NEJMoa072100. [DOI] [PubMed] [Google Scholar]
- 10.Hoffmann U, Massaro JM, Fox CS, Manders E, O’Donnell CJ. Defining normal distributions of coronary artery calcium in women and men (from the Framingham Heart Study) Am J Cardiol. 2008;102(9):1136–1141. doi: 10.1016/j.amjcard.2008.06.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lehman SJ, Massaro JM, Schlett CL, O’Donnell CJ, Hoffmann U, Fox CS. Periaortic fat, cardiovascular disease risk factors, and aortic calcification: the Framingham Heart Study. Atherosclerosis. 2010;210(2):656–661. doi: 10.1016/j.atherosclerosis.2010.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Preis SR, Hwang SJ, Fox CS, et al. Eligibility of individuals with subclinical coronary artery calcium and intermediate coronary heart disease risk for reclassification (from the Framingham Heart Study) Am J Cardiol. 2009;103(12):1710–1715. doi: 10.1016/j.amjcard.2009.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thanassoulis G, Massaro JM, Cury R, et al. Associations of long-term and early adult atherosclerosis risk factors with aortic and mitral valve calcium. J Am Coll Cardiol. 2010;55(22):2491–2498. doi: 10.1016/j.jacc.2010.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hong C, Bae KT, Pilgram TK. Coronary artery calcium: accuracy and reproducibility of measurements with multi-detector row CT—assessment of effects of different thresholds and quantification methods. Radiology. 2003;227(3):795–801. doi: 10.1148/radiol.2273020369. [DOI] [PubMed] [Google Scholar]
- 15.Hoffmann U, Siebert U, Bull-Stewart A, et al. Evidence for lower variability of coronary artery calcium mineral mass measurements by multi-detector computed tomography in a community-based cohort—consequences for progression studies. Eur J Radiol. 2006;57(3):396–402. doi: 10.1016/j.ejrad.2005.12.027. [DOI] [PubMed] [Google Scholar]
- 16.D’Agostino RB, Sr, Vasan RS, Pencina MJ, et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117(6):743–753. doi: 10.1161/CIRCULATIONAHA.107.699579. [DOI] [PubMed] [Google Scholar]
- 17.Paixao AR, Ayers CR, Berry JD, de Lemos JA, Khera A. Atherosclerotic cardiovascular disease prevention: a comparison between the third Adult Treatment Panel and the new 2013 treatment of blood cholesterol guidelines. Circ Cardiovasc Qual Outcomes. 2014;7(5):778–779. doi: 10.1161/CIRCOUTCOMES.114.001139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Allison MA, Wright M, Tiefenbrun J. The predictive power of low-density lipoprotein cholesterol for coronary calcification. Int J Cardiol. 2003;90(2–3):281–289. doi: 10.1016/s0167-5273(02)00571-5. [DOI] [PubMed] [Google Scholar]
- 19.Paramsothy P, Katz R, Owens DS, Burke GL, Probstfield JL, O’Brien KD. Age-modification of lipoprotein, lipid, and lipoprotein ratio-associated risk for coronary artery calcium (from the Multi-Ethnic Study of Atherosclerosis [MESA]) Am J Cardiol. 2010;105(3):352–358. doi: 10.1016/j.amjcard.2009.09.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wong ND, Kawakubo M, LaBree L, Azen SP, Xiang M, Detrano R. Relation of coronary calcium progression and control of lipids according to National Cholesterol Education Program guidelines. Am J Cardiol. 2004;94(4):431–436. doi: 10.1016/j.amjcard.2004.05.003. [DOI] [PubMed] [Google Scholar]
- 21.Johnson KM, Dowe DA. Accuracy of statin assignment using the 2013 AHA/ACC cholesterol guideline vs the 2001 NCEP ATP III guideline: correlation with atherosclerotic plaque imaging. J Am Coll Cardiol. 2014;64(9):910–919. doi: 10.1016/j.jacc.2014.05.056. [DOI] [PubMed] [Google Scholar]
- 22.Polonsky TS, McClelland RL, Jorgensen NW, et al. Coronary artery calcium score and risk classification for coronary heart disease prediction. JAMA. 2010;303(16):1610–1616. doi: 10.1001/jama.2010.461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Safford MM, Brown TM, Muntner PM, et al. REGARDS Investigators. Association of race and sex with risk of incident acute coronary heart disease events. JAMA. 2012;308(17):1768–1774. doi: 10.1001/jama.2012.14306. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.