Abstract
Background
Rheumatoid arthritis (RA) and metabolic syndrome (Mets) are considered to be diseases with common traits that can increase the risk of cardiovascular disease incidence; studies in other countries examined the relationship between these diseases. However, existing studies did not show consistent results. In the present study, the relationship between RA and Mets in Koreans was examined using the data of the 4th and 5th Korea National Health and Nutrition Examination Survey (KNHANES).
Methods
The present study used the data of the 4th and 5th KNHANES, conducted between 2007 and 2012. Among 25,812 adults aged over 40, 19,893 were selected as study subjects, excluding 5,919 who did not have variable information needed for the analysis. T-test and chi-square test were used for the analysis of related variables. To determine the relationship between diagnostic status of RA and Mets, multivariate logistic regression analysis was performed by controlling confounding variables, which were selected through literature review and statistical analysis.
Results
Multivariate logistic regression analysis was conducted to examine the relationship between diagnostic status of RA and Mets. When age, education level, average monthly household income, smoking, alcohol consumption, and level of physical activity were adjusted, the prevalence of Mets was lower in RA patients (adjusted odds ratio [aOR], 0.79; 95% confidence interval [CI], 0.65 to 0.96). Multivariate logistic regression analysis was performed to examine the relationship between treatment status of RA and Mets. When age, education level, average monthly household income, smoking, alcohol consumption, and level of physical activity were adjusted, there was a significant negative correlation in women (aOR, 0.65; 95% CI, 0.44 to 0.96).
Conclusion
The relationship between RA and Mets showed a significantly negative correlation in Korean women. The group that received RA treatment showed significantly lower prevalence of the Mets as compared to the untreated group in Korean RA women.
Keywords: Metabolic Syndrome, Rheumatoid Arthritis, Cardiovascular Diseases, Korea National Health and Nutrition Examination Survey
INTRODUCTION
Rheumatoid arthritis has a prevalence rate of approximately 0.5% to 1%, although it differs according to race and region, and occurs 5 times more frequently in women than in men.1) It is a chronic autoimmune disease causing pain, deformity, and impairment of certain joints, as well as concurrent systemic inflammatory responses. According to a study, rheumatoid arthritis is known to be a disease that does not simply target joints, but also causes a systemic inflammatory response in the lungs, heart, and kidneys.2) Cytokines such as tumor necrosis factor-α, interleukin (IL)-6, and IL-1 are produced in tissues within joints, the initial point of inflammation; these are secreted into the systemic circulation, and increase insulin resistance by acting on adipose tissue, skeletal muscles, the liver, and the endangium, and trigger dyslipidemia and inactivation and destruction of the endangium.3,4) Arteriosclerosis, among inflammatory responses acting systemically, increases the risk of cardiovascular diseases and largely affects the survival rate of patients. According to a study by Avina-Zubieta et al.,5) the mortality rate from cardiovascular disease was 1.5 times higher in rheumatoid arthritis patients than in the general population.
Metabolic syndrome is a group of risk factors for type 2 diabetes and cardiovascular diseases, including insulin resistance, abdominal obesity, dyslipidemia, hypertension, and impaired fasting glucose, incorporated into a single disease group, and is used as a predictor of life expectancy.6) Although there are slight differences depending on the criteria used by various authors, Ford et al.7) reported that the prevalence rate of metabolic syndrome in the USA is 34.3%, with mortality in patients with associated cardiovascular disease being 3 times higher than in those without metabolic syndrome.8)
A study conducted on Koreans showed that the prevalence rate of metabolic syndrome increased from 24.9% in 1998 to 31.3% in 2007. The causes of this increase are likely due to an increase in Western dietary habits and a decreased level of physical activity. Because the increased prevalence of metabolic syndrome threatens public health and increases medical costs, correcting lifestyle and metabolic syndrome indices in these patients is critical.9)
Rheumatoid arthritis and metabolic syndrome are considered to be diseases with common traits that can increase the risk of cardiovascular disease incidence; studies in other countries examined the relationship between these diseases.10) According to a meta-analysis by Zhang et al.,10) there was a correlation between rheumatoid arthritis and metabolic syndrome in 12 observational studies; when regionally examined, there was a positive correlation in studies using data from North America, but this was not significant when Asian research data were analyzed. In a study of a patient control group using domestic data by Lee et al.,11) the association between rheumatoid arthritis and metabolic syndrome showed no significant correlation (adjusted odds ratio [aOR], 1.22; 95% confidence interval [CI], 0.58 to 1.24).
There have been no studies analyzing the relationship between these two diseases in Koreans using a large-scale database such as the Korea National Health and Nutrition Examination Survey (KNHANES). In the present study, the relationship between rheumatoid arthritis and metabolic syndrome in Koreans was examined using the data of the 4th and 5th KNHANES.
METHODS
The KNHANES extracts approximately 10,000 populations from 20 households in 192 regions using systematic sampling, and conducts examination, health questionnaire, and nutrition surveys. In the examination survey, the prevalence of chronic diseases such as obesity, hypertension, diabetes, and dyslipidemia is determined through physical and blood pressure measurement, and muscle strength, blood, and urine testing. The health questionnaire is divided into a survey conducted by examiners through individual interviews, and it is used to collect data on education level, economic activity, morbidity, medical use, and quality of life; and a self-administered health behavior survey on smoking, alcohol consumption, and mental health. A nutrition survey includes questions about food consumption one day before the survey.12)
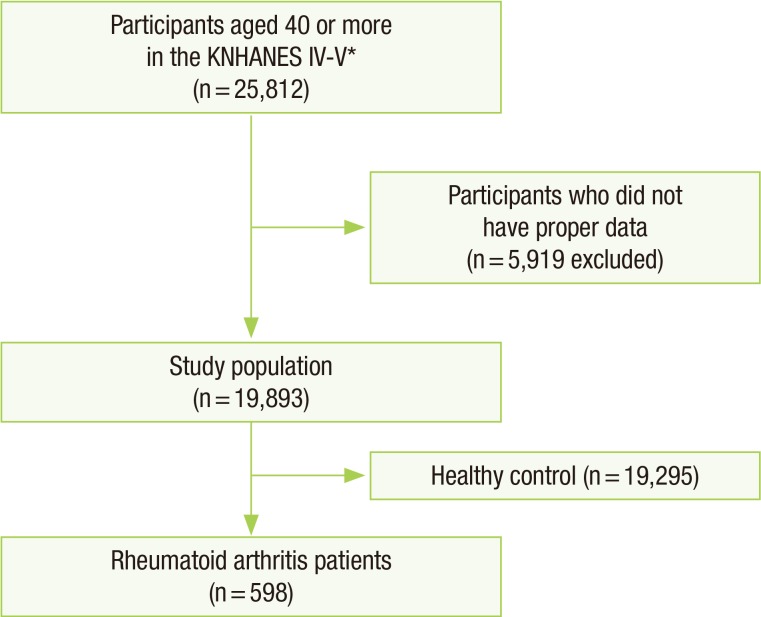
The present study used the data of the 4th and 5th KNHANES, conducted between 2007 and 2012. Among 25,812 adults aged over 40, 19,893 were selected as study subjects, excluding 5,919 who did not have variable information needed for the analysis. The 5,919 adults who were excluded from the study included 2,678 who did not have data for each component of the metabolic syndrome, 401 who did not report diagnostic status of rheumatoid arthritis, and 2,840 whose surveys for confounding variables such as education level, average monthly household income, physical activity, smoking, and alcohol consumption were missing (Figure 1).
Figure 1. Flow diagram of inclusion or exclusion of study participants. KNHANES, Korean National Health and Nutrition Examination Survey. *The 4th and 5th KNHANES 2007–2012.
1. Establishment of Related Variables
Among health behavior-related variables, physical activity was classified following the guideline of the 2005 International Physical Activity Questionnaire (2005 IPAQ guideline). Based on the guideline, the high-level physical activity group was defined as performing vigorous physical activity more than 3 days a week at an exercise level of 1,500 metabolic equivalent (MET) s, or more than 3,000 METs of exercise level including walking and moderate or vigorous-intensity exercise more than 7 days a week. The moderate-level physical activity group was defined as performing intense activity more than 20 minutes more than 3 days a week, performing moderate intensity exercise or walking for more than 30 minutes each time and more than 5 days a week, or achieving 600 MET of exercise level with walking or activity with moderate or vigorous intensity. The low-level physical activity group was defined as not belonging either of the two other groups.13)
The subjects were divided into nonsmokers, past smokers, and current smokers. Alcohol consumption was divided into 4 groups according to the average amount of alcohol (g/d) consumed daily by subjects through analysis of a self-administered survey from KNHANES: none (less than 1 g/d), light (1–14.99 g/d), moderate (15–29.99 g/d), and heavy (above 30 g/d).14)
Metabolic syndrome was defined as having 3 or more of the following, according to the definition of the American Heart Association/National Heart Lung and Blood Institute: waist circumference above 90 cm for men and above 85 cm for women; blood triglycerides higher than 150 mg/dL; high density lipoprotein cholesterol below 40 mg/dL for men and below 50 mg/dL for women; systolic blood pressure higher than 130 mm Hg or diastolic blood pressure higher than 85 mm Hg, or when diagnosed with hypertension; and fasting blood glucose higher than 100 mg/dL, or when diagnosed with diabetes.15,16) In the present study, the current diagnostic status of rheumatoid arthritis, as determined by a physician, was set as an outcome variable to minimize error due to self-reporting.
2. Analytical Methods and Statistics
STATA ver. 13.1 for Windows (Stata Co., College Station, TX, USA) was used for statistical analysis. T-test and chi-square test were used for the analysis of related variables. To determine the relationship between diagnostic status of rheumatoid arthritis and metabolic syndrome, multivariate logistic regression analysis was performed by controlling confounding variables, which were selected through literature review and statistical analysis.
RESULTS
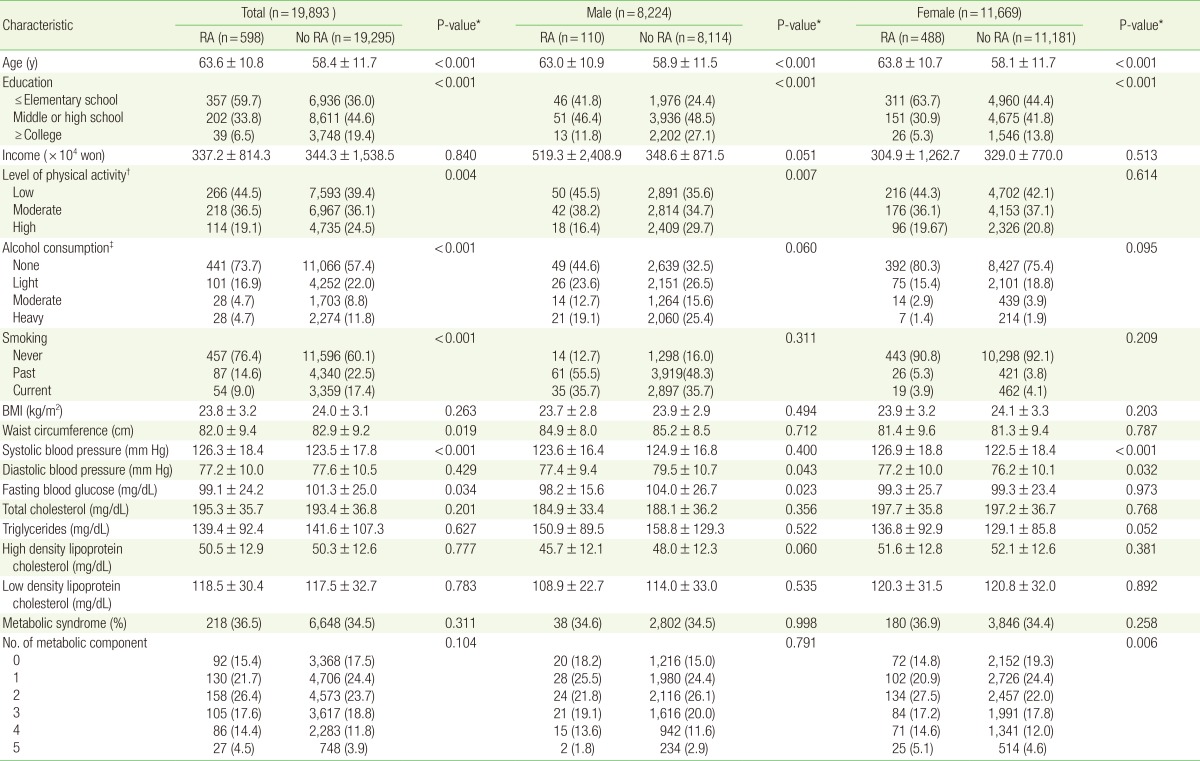
Of 19,893 study subjects, there were 8,224 men and 11,669 women; 1.4% (110) of men and 4.2% (488) of women had rheumatoid arthritis. The average age was 63.6 for patients with rheumatoid arthritis and 58.4 for the control group. Among sociodemographic variables and health risk factors, age, education level, physical activity, alcohol consumption, and smoking showed a significant difference, while among metabolic syndrome indices, waist circumference, systolic blood pressure, diastolic blood pressure, and fasting blood glucose showed a significant difference (Table 1).
Table 1. Baseline characteristics of the subjects.
Values are presented as mean±standard deviation or number (%). BMI was calculated as weight in kilograms divided by height in meters squared.
RA, rheumatoid arthritis; BMI, body mass index; MET, metabolic equivalent.
*From a T-test for continuous outcomes and chi-square test for binary outcomes comparing a difference between any of the 2 study groups. †Categorical variable from the International Physical Activity Questionnaire Research Committee: low, no activity is reported or some activity is reported but not enough to meet categories 2 or 3; moderate, either of the following 3 criteria (3 or more days of vigorous activity of at least 20 minutes per day; 5 or more days of moderate-intensity activity and/or walking of at least 30 minutes per day; 5 or more days of any combination of walking, moderate-intensity, or vigorous intensity activities achieving a minimum of at least 600 MET-minutes/wk); high, any one of the following 2 criteria (vigorous-intensity activity on at least 3 days and accumulating at least 1,500 MET-minutes/wk; 7 or more days of any combination of walking, moderate- or vigorous-intensity activities accumulating at least 3,000 MET-minutes/wk). ‡None<1, light 1–14.99, moderate 15–29.99, and heavy ≥30 g/d.
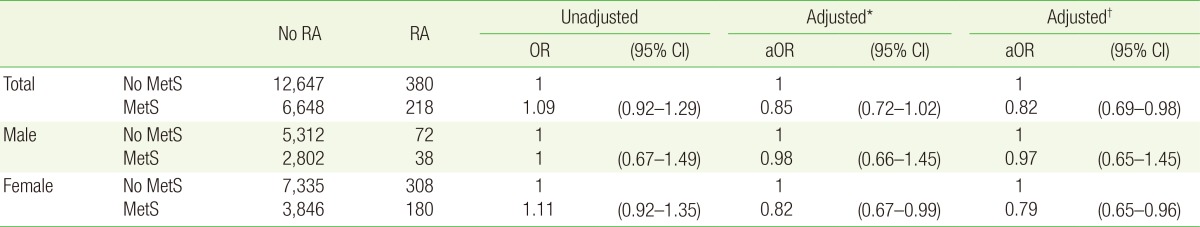
Multivariate logistic regression analysis was conducted to examine the relationship between diagnostic status of rheumatoid arthritis and metabolic syndrome. When age was adjusted in women, there was a negative correlation (aOR, 0.82; 95% CI, 0.67 to 0.99) When age, education level, average monthly household income, smoking, alcohol consumption, and level of physical activity were adjusted, the prevalence of metabolic syndrome was lower in rheumatoid arthritis patients (aOR, 0.79; 95% CI, 0.65 to 0.96). No significant correlation was observed in men (Table 2).
Table 2. Multiple logistic regression to assess the relationship between MetS and RA.
MetS, metabolic syndrome; RA, rheumatoid arthritis; OR, odds ratio; CI, confidence interval; aOR, adjusted odds ratio.
*Adjusted for age and sex in total; adjusted for age in male and female. †Adjusted for age, sex, education level, household income, smoking status, alcohol consumption, and level of physical activity in total; adjusted for age, education level, household income, smoking status, alcohol consumption, and level of physical activity in male and female.
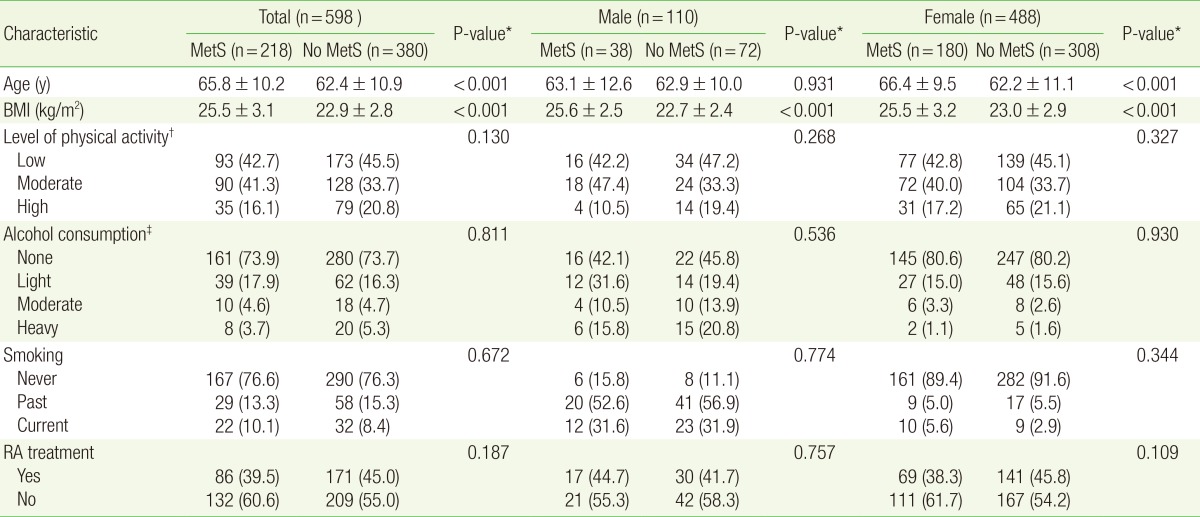
Of 598 patients diagnosed with rheumatoid arthritis, the average age was 65.8 for 218 patients with metabolic syndrome and 62.4 for 380 patients without metabolic syndrome. There were differences in age, body mass index (BMI), level of physical activity, alcohol consumption, smoking, and treatment status of rheumatoid arthritis; differences were especially significant according to age and BMI (Table 3).
Table 3. Characteristics of RA patient.
Values are presented as mean±standard deviation or number (%). BMI was calculated as weight in kilograms divided by height in meters squared.
RA, rheumatoid arthritis; MetS, metabolic syndrome; BMI, body mass index; MET, metabolic equivalent.
*From a T-test for continuous outcomes and chi-square test for binary outcomes comparing a difference between any of the 2 study groups. †Categorical variable from the International Physical Activity Questionnaire Research Committee: low, no activity is reported or some activity is reported but not enough to meet categories 2 or 3; moderate, either of the following 3 criteria (3 or more days of vigorous activity of at least 20 minutes per day; 5 or more days of moderate-intensity activity and/or walking of at least 30 minutes per day; 5 or more days of any combination of walking, moderate-intensity, or vigorous intensity activities achieving a minimum of at least 600 MET-minutes/wk); high, any one of the following 2 criteria (vigorous-intensity activity on at least 3 days and accumulating at least 1,00 MET-minutes/wk; 7 or more days of any combination of walking, moderate- or vigorous-intensity activities accumulating at least 3,000 MET-minutes/wk. ‡None <1, light 1–14.99, moderate 15–29.99, and heavy ≥30 g/d.
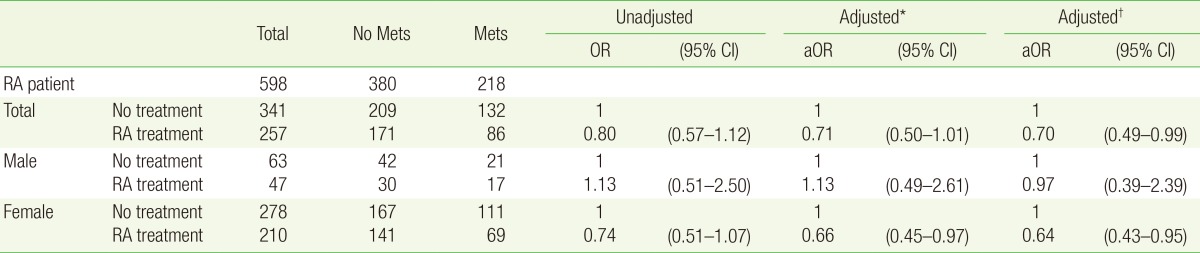
Multivariate logistic regression analysis was performed to examine the relationship between treatment status of rheumatoid arthritis and metabolic syndrome. When age was adjusted in women, there was a negative correlation (odds ratio [OR], 0.66; 95% CI, 0.45 to 0.97); when age, education level, average monthly household income, smoking, alcohol consumption, and level of physical activity were adjusted, there was a significant negative correlation in women (aOR, 0.65; 95% CI, 0.44 to 0.96). No significant correlation was observed in men (Table 4).
Table 4. Multiple logistic regression to assess the relationship between Mets and RA treatment.
Mets, metabolic syndrome; RA, rheumatoid arthritis; OR, odds ratio; CI, confidence interval; aOR, adjusted odds ratio.
*Adjusted for age and sex in total; adjusted for age in male and female. †Adjusted for age, sex, education level, household income, smoking status, alcohol consumption, and level of physical activity in total; adjusted for age, education level, household income, smoking status, alcohol consumption, and level of physical activity in male and female.
DISCUSSION
This study is the first to examine the relationship between rheumatoid arthritis and metabolic syndrome in Koreans using data from KNHANES. Our study showed that prevalence of metabolic syndrome was significantly lower in female patients with rheumatoid arthritis than in the control group, when age, education level, average monthly household income, smoking, alcohol consumption, and level of physical activity were adjusted. This is in contrast with a study result by da Cunha et al.17) (OR, 2.01; 95% CI, 1.36 to 2.98), and study results conducted in the USA and Europe, in which the prevalence of metabolic syndrome was higher in patients with rheumatoid arthritis. However, in a comparison with 5 studies conducted in Asia (OR, 0.99; 95% CI, 0.80 to 1.24), the prevalence of metabolic syndrome was not significant in patients with rheumatoid arthritis in some studies, because of inconsistently reported results. 11,18,19,20,21) Therefore, the results of this study, the relationship between the two diseases in Koreans, was close to the results of studies were performed in Asia.
The relationship between the treatment status of rheumatoid arthritis and metabolic syndrome was analyzed as a subcategory, and multivariate logistic regression analysis after adjusting for age, education level, average monthly household income, smoking, alcohol consumption, and level of physical activity showed a significant negative correlation in women (aOR, 0.65; 95% CI, 0.44 to 0.96). This result is consistent with the study result by Toms et al.,22) which showed that the prevalence of metabolic syndrome was lower in a group of patients with rheumatoid arthritis who used methotrexate (MTX; OR, 0.52; 95% CI, 0.33 to 0.81). MTX causes changes in extracellular concentration of adenosine, and the subsequent anti-inflammatory action of adenosine increases the effect of insulin, which affects glucose transport and metabolism, and alters lipid metabolism. It was also hypothesized that activity of adenosine would prevent arteriosclerosis.22) However, this is still controversial, as another study claims that administration of MTX does not reduce the incidence of metabolic syndrome in patients with rheumatoid arthritis.23)
As previously stated, the inflammatory response initiated in joint tissues in rheumatoid arthritis patients is known to act on adipose tissue, skeletal muscle, the liver, and the endangium through the systemic circulation, and increases the prevalence of cardiovascular disease through increased insulin resistance, dyslipidemia, and destruction/transformation of the endangium. Therefore, efforts to prevent cardiovascular disease are crucial in patients with rheumatoid arthritis. When the level of physical activity was compared in the present study, the percentage of exercise higher than moderate level according to the IPAQ classification was 55.5% in patients with rheumatoid arthritis and 60.6% in the control group, showing that the level of physical activity was significantly lower in patients with rheumatoid arthritis (P=0.004). Although the level of physical activity plays an important role in the life expectancy for all adults, a decrease in physical activity in patients with rheumatoid arthritis is an especially important risk factor that can lead to increased mortality from cardiovascular disease, and intervention is deemed necessary from a treatment perspective.1,24)
The BMI was 23.8 kg/m2 in the patient group with rheumatoid arthritis and 24.0 kg/m2 in the control group, showing no significant difference; however, waist circumference was 82.0 cm in the patient group with rheumatoid arthritis, showing a significant decrease compared to 82.9 cm in the control group (P=0.019). According to Kerekes et al.,25) BMI as well as the amounts of subcutaneous and visceral fat show a tendency to increase at an early stage in rheumatoid arthritis; however, the BMI and the amount of subcutaneous fat decrease, and only the amount of visceral fat increases, which leads to 'skinny obesity' at a stage when activity of disease becomes higher and resistance to treatment develops.26,27) Based on this, it is believed that abdominal circumference and blood pressure decrease depending on the severity of rheumatoid arthritis, and therefore, it may show a negative correlation in the relationship with metabolic syndrome.
The present study has a limitation as an observational study, in that a causal relationship between variables cannot be determined. In addition to independent variables such as rheumatoid arthritis and metabolic syndrome, whether the confounding variables used for the analysis of health behavior in study subjects, such as smoking, alcohol consumption, and level of physical activity, were preexisting health behaviors or changes that occurred after morbidity of disease, could not be determined. Furthermore, as the type of treatment was not clearly described, it was difficult to analyze the correlation between metabolic syndrome and the treatment status with a particular therapeutic agent. Because the severity of rheumatoid arthritis in each patient could not be determined from the KNHANES data alone, it was unclear in the analysis of physical activity in patients with rheumatoid arthritis which factors affected the decrease in physical activity.
If instruments that can objectively evaluate the severity of rheumatoid arthritis, such as DAS28 (Disease Activity Score 28) or HAQ-DI (Health Assessment Questionnaire-Disability Index for rheumatoid arthritis) are included in a future study, determining the relationship of metabolic syndrome with severity of disease, level of physical activity, and morbidity may be possible.17)
Despite these limitations, the prevention of cardiovascular disease and removal of risk factors are as important as studies on the relationship between metabolic syndrome and rheumatoid arthritis in extending the life span of patients with rheumatoid arthritis. The present study investigated an association between the two diseases using the KNHANES data, which has not previously been reported. We confirmed that the prevalence of metabolic syndrome among patients with rheumatoid arthritis was lower in the group who received treatment than in those who did not. In the future, through studies of patient control groups and cohort studies, the effects of specific therapeutic agents such as MTX on the incidence of metabolic syndrome in rheumatoid arthritis need to be examined.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Tierney M, Fraser A, Kennedy N. Physical activity in rheumatoid arthritis: a systematic review. J Phys Act Health. 2012;9:1036–1048. doi: 10.1123/jpah.9.7.1036. [DOI] [PubMed] [Google Scholar]
- 2.Kinder BW, Collard HR, Koth L, Daikh DI, Wolters PJ, Elicker B, et al. Idiopathic nonspecific interstitial pneumonia: lung manifestation of undifferentiated connective tissue disease? Am J Respir Crit Care Med. 2007;176:691–697. doi: 10.1164/rccm.200702-220OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sattar N, McCarey DW, Capell H, McInnes IB. Explaining how "high-grade" systemic inflammation accelerates vascular risk in rheumatoid arthritis. Circulation. 2003;108:2957–2963. doi: 10.1161/01.CIR.0000099844.31524.05. [DOI] [PubMed] [Google Scholar]
- 4.Del Rincon I, Freeman GL, Haas RW, O'Leary DH, Escalante A. Relative contribution of cardiovascular risk factors and rheumatoid arthritis clinical manifestations to atherosclerosis. Arthritis Rheum. 2005;52:3413–3423. doi: 10.1002/art.21397. [DOI] [PubMed] [Google Scholar]
- 5.Avina-Zubieta JA, Choi HK, Sadatsafavi M, Etminan M, Esdaile JM, Lacaille D. Risk of cardiovascular mortality in patients with rheumatoid arthritis: a meta-analysis of observational studies. Arthritis Rheum. 2008;59:1690–1697. doi: 10.1002/art.24092. [DOI] [PubMed] [Google Scholar]
- 6.Sidiropoulos PI, Karvounaris SA, Boumpas DT. Metabolic syndrome in rheumatic diseases: epidemiology, pathophysiology, and clinical implications. Arthritis Res Ther. 2008;10:207. doi: 10.1186/ar2397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ford ES, Li C, Zhao G. Prevalence and correlates of metabolic syndrome based on a harmonious definition among adults in the US. J Diabetes. 2010;2:180–193. doi: 10.1111/j.1753-0407.2010.00078.x. [DOI] [PubMed] [Google Scholar]
- 8.Isomaa B, Almgren P, Tuomi T, Forsen B, Lahti K, Nissen M, et al. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care. 2001;24:683–689. doi: 10.2337/diacare.24.4.683. [DOI] [PubMed] [Google Scholar]
- 9.Lim S, Shin H, Song JH, Kwak SH, Kang SM, Won Yoon J, et al. Increasing prevalence of metabolic syndrome in Korea: the Korean National Health and Nutrition Examination Survey for 1998-2007. Diabetes Care. 2011;34:1323–1328. doi: 10.2337/dc10-2109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang J, Fu L, Shi J, Chen X, Li Y, Ma B, et al. The risk of metabolic syndrome in patients with rheumatoid arthritis: a meta-analysis of observational studies. PLoS One. 2013;8:e78151. doi: 10.1371/journal.pone.0078151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee SG, Kim JM, Lee SH, Kim KH, Kim JH, Yi JW, et al. Is the frequency of metabolic syndrome higher in South Korean women with rheumatoid arthritis than in healthy subjects? Korean J Intern Med. 2013;28:206–215. doi: 10.3904/kjim.2013.28.2.206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kweon S, Kim Y, Jang MJ, Kim Y, Kim K, Choi S, et al. Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES) Int J Epidemiol. 2014;43:69–77. doi: 10.1093/ije/dyt228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.International Physical Activity Questionnaire Research Committee. Guidelines for data processing and analysis of the International Physical Activity Questionnaire (IPAQ): short and long forms [Internet] [place unknown]: International Physical Activity Questionnaire Research Committee; 2005. [cited 2015 Feb 20]. Available from: http://www.ipaq.ki.se. [Google Scholar]
- 14.Baik I, Shin C. Prospective study of alcohol consumption and metabolic syndrome. Am J Clin Nutr. 2008;87:1455–1463. doi: 10.1093/ajcn/87.5.1455. [DOI] [PubMed] [Google Scholar]
- 15.Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112:2735–2752. doi: 10.1161/CIRCULATIONAHA.105.169404. [DOI] [PubMed] [Google Scholar]
- 16.Lee SY, Park HS, Kim DJ, Han JH, Kim SM, Cho GJ, et al. Appropriate waist circumference cutoff points for central obesity in Korean adults. Diabetes Res Clin Pract. 2007;75:72–80. doi: 10.1016/j.diabres.2006.04.013. [DOI] [PubMed] [Google Scholar]
- 17.Da Cunha VR, Brenol CV, Brenol JC, Fuchs SC, Arlindo EM, Melo IM, et al. Metabolic syndrome prevalence is increased in rheumatoid arthritis patients and is associated with disease activity. Scand J Rheumatol. 2012;41:186–191. doi: 10.3109/03009742.2011.626443. [DOI] [PubMed] [Google Scholar]
- 18.Sahebari M, Goshayeshi L, Mirfeizi Z, Rezaieyazdi Z, Hatef MR, Ghayour-Mobarhan M, et al. Investigation of the association between metabolic syndrome and disease activity in rheumatoid arthritis. ScientificWorldJournal. 2011;11:1195–1205. doi: 10.1100/tsw.2011.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mok CC, Ko GT, Ho LY, Yu KL, Chan PT, To CH. Prevalence of atherosclerotic risk factors and the metabolic syndrome in patients with chronic inflammatory arthritis. Arthritis Care Res (Hoboken) 2011;63:195–202. doi: 10.1002/acr.20363. [DOI] [PubMed] [Google Scholar]
- 20.Karimi M, Mazloomzadeh S, Kafan S, Amirmoghadami H. The frequency of metabolic syndrome in women with rheumatoid arthritis and in controls. Int J Rheum Dis. 2011;14:248–254. doi: 10.1111/j.1756-185X.2011.01595.x. [DOI] [PubMed] [Google Scholar]
- 21.Dao HH, Do QT, Sakamoto J. Increased frequency of metabolic syndrome among Vietnamese women with early rheumatoid arthritis: a cross-sectional study. Arthritis Res Ther. 2010;12:R218. doi: 10.1186/ar3203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Toms TE, Panoulas VF, John H, Douglas KM, Kitas GD. Methotrexate therapy associates with reduced prevalence of the metabolic syndrome in rheumatoid arthritis patients over the age of 60- more than just an anti-inflammatory effect?: a cross sectional study. Arthritis Res Ther. 2009;11:R110. doi: 10.1186/ar2765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Raterman HG, Voskuyl AE, Dijkmans BA, Nurmohamed MT. Use of methotrexate therapy is not associated with decreased prevalence of metabolic syndrome. Arthritis Res Ther. 2009;11:413. doi: 10.1186/ar2805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Larkin L, Kennedy N. Correlates of physical activity in adults with rheumatoid arthritis: a systematic review. J Phys Act Health. 2014;11:1248–1261. doi: 10.1123/jpah.2012-0194. [DOI] [PubMed] [Google Scholar]
- 25.Kerekes G, Nurmohamed MT, Gonzalez-Gay MA, Seres I, Paragh G, Kardos Z, et al. Rheumatoid arthritis and metabolic syndrome. Nat Rev Rheumatol. 2014;10:691–696. doi: 10.1038/nrrheum.2014.121. [DOI] [PubMed] [Google Scholar]
- 26.Giles JT, Allison M, Blumenthal RS, Post W, Gelber AC, Petri M, et al. Abdominal adiposity in rheumatoid arthritis: association with cardiometabolic risk factors and disease characteristics. Arthritis Rheum. 2010;62:3173–3182. doi: 10.1002/art.27629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lombard LA, du Plessis LM, Visser J. Body composition of rheumatoid arthritis patients in the City of Cape Town, South Africa. Clin Rheumatol. 2014;33:467–476. doi: 10.1007/s10067-013-2414-0. [DOI] [PubMed] [Google Scholar]