Abstract
Lysosomal storage diseases (LSDs) are debilitating neurometabolic disorders for most of which long-term effective therapies have not been developed. Gene therapy is a potential treatment but a critical barrier to treating the brain is the need for global correction. We tested the efficacy of cisterna magna infusion of adeno-associated virus type 1 (AAV1) expressing feline alpha-mannosidase gene in the postsymptomatic alpha-mannosidosis (AMD) cat, a homologue of the human disease. Lysosomal alpha-mannosidase (MANB) activity in the cerebrospinal fluid (CSF) and serum were increased above the control values in untreated AMD cats. Clinical neurological signs were delayed in onset and reduced in severity. The lifespan of the treated cats was significantly extended. Postmortem histopathology showed resolution of lysosomal storage lesions throughout the brain. MANB activity in brain tissue was significantly above the levels of untreated tissues. The results demonstrate that a single cisterna magna injection of AAV1 into the CSF can mediate widespread neuronal transduction of the brain and meaningful clinical improvement. Thus, cisterna magna gene delivery by AAV1 appears to be a viable strategy for treatment of the whole brain in AMD and should be applicable to many of the neurotropic LSDs as well as other neurogenetic disorders.
Introduction
Lysosomal storage diseases (LSDs) are debilitating neurometabolic disorders for which long-term effective therapies have not been developed for most. A critical barrier to progress in the successful treatment of LSDs is an approach that will allow sustained delivery of the missing lysosomal enzyme to the brain in a quantity sufficient to prevent neuropathology. The nature of these diseases is that lesions are globally distributed in the brain due to the fundamental metabolic defect present in all cells, and treatment therefore requires widespread enzyme distribution to be effective.
In several different LSDs, delivery of the purified normal enzyme into the cerebrospinal fluid (CSF) by intrathecal or intraventricular injection (enzyme replacement therapy) has been shown to correct storage of the offending substrates in animal models1,2,3,4,5,6,7,8,9 and one human clinical trial has been reported.10 Enzyme delivered to the CSF may reach neuronal cells throughout the brain, a process aided by metabolic cross-correction.11,12 However, there are a number of limitations to the use of recombinant enzyme for long-term therapy. These include the relatively short half-lives of recombinant enzymes which necessitate weekly or monthly injections to sustain needed concentrations, the risks and inconvenience of repeated enzyme instillations, and the high cost of recombinant enzyme production.
Gene therapy provides an alternative means for delivery of genes encoding the missing lysosomal enzyme to the brain. Indeed, widespread gene transduction in the brain can be achieved with multiple intraparenchymal injections of adeno-associated virus (AAV) vectors and this has been shown to be effective in reducing neuropathology throughout the brain of large animal models of LSDs.13,14,15 CSF injection of AAV9, AAVrh.10, and AAV2.5 have also been shown to mediate transduction of glial and neuronal cells in the brain and spinal cord of large animals including dogs, cats, pigs, and monkeys.16,17,18,19,20,21,22,23
Here, we report that a single administration of AAV1 vector into the CSF via the cisterna magna provides sustained expression of a reporter gene in the cat brain, including widespread transduction of neurons in the cerebral cortex. We tested the efficacy of gene transfer to treat a neurotropic LSD in the alpha-mannosidosis (AMD) cat model, which has a genetic deficiency of lysosomal alpha-mannosidase (MANB). Neuronal cells were transduced in many areas of the brain and storage lesions were reversed throughout the brain. Even though the treatment was initiated after the onset of clinical signs, the lifespan of the treated cats was significantly extended and their condition was significantly improved compared to untreated cats. Thus, this appears to be a viable strategy for treatment of the whole brain in AMD and should be applicable to many of the neurotropic LSDs as well as other neurogenetic disorders. Taken together, the potential impact of these experiments on clinical practice is high since the largest current barrier to treating the brain in patients with LSDs would be circumvented.
Results
AAV1 injection into CSF of cats efficiently transduces neurons throughout the CNS
We compared AAV9 to AAV1 as we had found the latter to transduce multiple structures and regions of the cat brain after intraparenchymal injection.13,24 When injected at the same dose into the cisterna magna, AAV1 resulted in higher transduction in the cat brain than AAV9 (Figure 1), thus AAV1 was used for the rest of the experiments. Normal cats received cisterna magna injections of AAV1 vector encoding enhanced green fluorescent protein (eGFP). GFP expression in the CNS was examined using immunohistochemistry 4 weeks postinjection to analyze the distribution of gene transduction. Gene expression in the brain was analyzed in coronal sections taken at intervals along the rostral–caudal axis. A schematic of the location from which the samples were obtained is shown in Figure 2a. Extensive vector transduction was achieved throughout the brain, predominantly in cells with the morphology of pyramidal neurons of the cerebral cortex and granule cells of the hippocampus (Figure 2b–d). GFP expression was also observed in ependymal cells lining the ventricles, choroid plexus, trapezoid body cells in the pons, medium spiny neurons of the caudate nucleus, and spinal cord (Figure 2e–i). The vast majority of the transduced cells were neurons by morphology and transduction was almost exclusively confined to the gray matter. Very few glial cells were also transduced in the white matter.
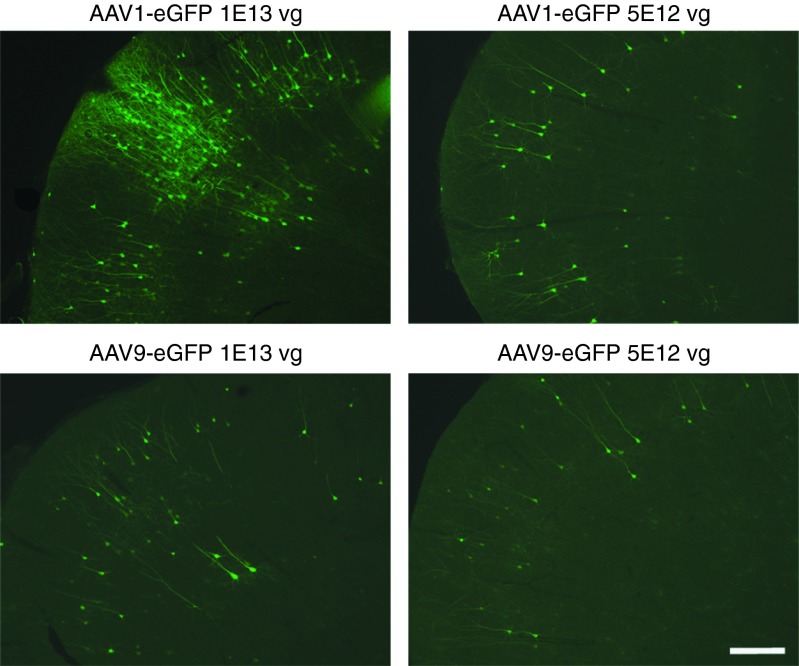
Figure 1.
GFP immunofluorescence in the cerebral cortex of normal cats following cisterna magna injection of AAV1 or AAV9 vector. Normal cats received cisterna magna injections of AAV1 (n = 3, 1013 GC; n = 1, 5 × 1012 GC) or AAV9 vector (n = 2, 1013 GC; n = 1, 5 × 1012 GC) encoding eGFP. Immunofluorescent staining with GFP antibody showed vector transduction in the cerebral cortex of cats 4 weeks postinjection. Bar = 300 µm. AAV, adeno-associated virus; eGFP, enhanced green fluorescent protein.
Figure 2.
Widespread gene transduction throughout the central nervous system (CNS) of normal cat following adeno-associated virus type 1 (AAV1) injection into cerebrospinal fluid. Normal cats (n = 3) received cisterna magna injections of AAV1 vector (1013 GC) encoding enhanced green fluorescent protein (eGFP), and GFP expression in the CNS was examined using immunohistochemistry 4 weeks postinjection. (a) The distribution of gene expression was analyzed in coronal sections taken at intervals along the rostral–caudal axis of the brain. (b–d) Extensive vector transduction was achieved throughout the brain, predominantly in cells with the morphology of pyramidal neurons of the cerebral cortex (b,c) and granule cells of the hippocampus (d). GFP expression was also observed in (e) ependymal cells lining the ventricles, (f) choroid plexus, (g) trapezoid body cells in the pons, (h) medium spiny neurons of the caudate nucleus, and (i) spinal cord. Bar = 300 µm (left columns) and 60 µm (right columns).
MANB activity in CSF and serum of AMD cats after cisterna magna delivery of AAV1-fMANB
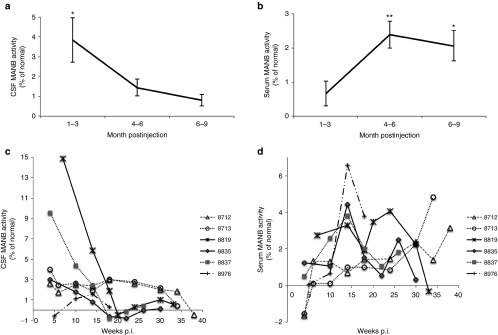
Six AMD cats were treated with a single injection of 1013 GC of AAV1 expressing feline alpha-mannosidase (MANB) into the CSF via the cisterna magna at 6 weeks of age, which is after the onset of clinical signs of the disease.13 CSF and serum samples were collected before and after injection and assayed for MANB enzyme activity in individual animals (Figure 3c,d). MANB activity in the CSF was significantly elevated above residual background activity at 1–3 months postinjection (Figure 3a; P < 0.05) but the activity was not statistically significant after 4–6 months. Serum MANB activity was statistically above background activity after 4 months postinjection (Figure 3b; P < 0.01 at 4–6 months and P < 0.05 at 6–9 months postinjection).
Figure 3.
MANB activity in CSF and serum of alpha-mannosidosis (AMD) cats following cisterna magna injection of adeno-associated virus type 1 (AAV1). AMD cats (n = 6) were treated with a single cisterna magna injection of AAV1 (1013 GC) expressing fMANB into the cisterna magna at 6 weeks of age. CSF and serum samples were collected before and after injection and assayed for MANB enzyme activity. (a) MANB activity in the CSF was significantly elevated above residual background activity at 1–3 months postinjection (p.i.). (b) MANB activity in the serum was significantly elevated after 4 months postinjection. (c,d) MANB activity in the CSF and serum of individual animals are shown. Bars represent means ± SEM. *P < 0.05; **P < 0.01. CSF, cerebrospinal fluid; fMANB, feline alpha-mannosidase; MANB, lysosomal alpha-mannosidase.
Extended lifespan and improvement in neurological signs in treated AMD cats
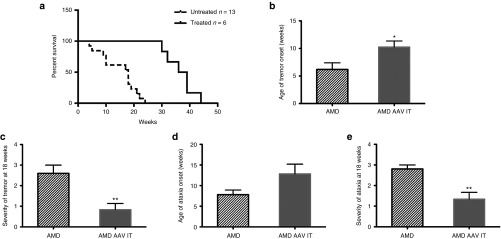
There were no vector-related toxicity or adverse events in the treated cats. The treated cats lived significantly longer than untreated cats and were euthanized at 30–44 weeks of age when they reached their humane endpoint (Figure 4a; log-rank test, P < 0.001). It is notable that untreated AMD cats do not live beyond 6 months of age.13,25 In our study, untreated AMD cats were euthanized between 4 and 6 months of age due to their deteriorating conditions. AMD cats were euthanized when they were unable to maintain weight or lost over 15% of body weight, neurological signs caused difficulty grooming and eating due to tremors/ataxia, required bathing two or more times a week, or had loss of appetite 2 days in a row. Neurological examinations were performed monthly from treatment to assess the therapeutic effects. Untreated AMD-affected cats show progressive worsening of neurological signs including whole body tremor, truncal ataxia, and dropped hocks starting at 5 weeks of age.13 The treated cats showed a significantly delayed onset of whole body tremor (Figure 4b; P < 0.05). Although the onset of ataxia did not reach statistical significance (Figure 4d), at 18 weeks of age, both the whole body tremor and truncal ataxia were significantly less severe in the treated cats (Figure 4c,e) compared to the untreated cats (P < 0.01).
Figure 4.
Extended lifespan and improvement in neurological signs in treated AMD cats. (a) The treated AMD cats (n = 6) lived significantly longer than untreated cats (n = 13) and were euthanized at 30–44 weeks of age due to disease progression (log-rank test, P < 0.001). Neurological examinations were performed monthly from treatment to assess the therapeutic effects. (b) The treated cats showed a significantly delayed onset of whole body tremor. (d) Onset of ataxia did not reach statistical significance. (c,e) At 18 weeks of age, both the whole body tremor and truncal ataxia were significantly less severe. Bars represent means ± SEM. *P < 0.05; **P < 0.01. AAV, adeno-associated virus; AMD, alpha-mannosidosis.
Widespread distribution of MANB mRNA transcripts and MANB enzymatic activity in the treated AMD cat brain
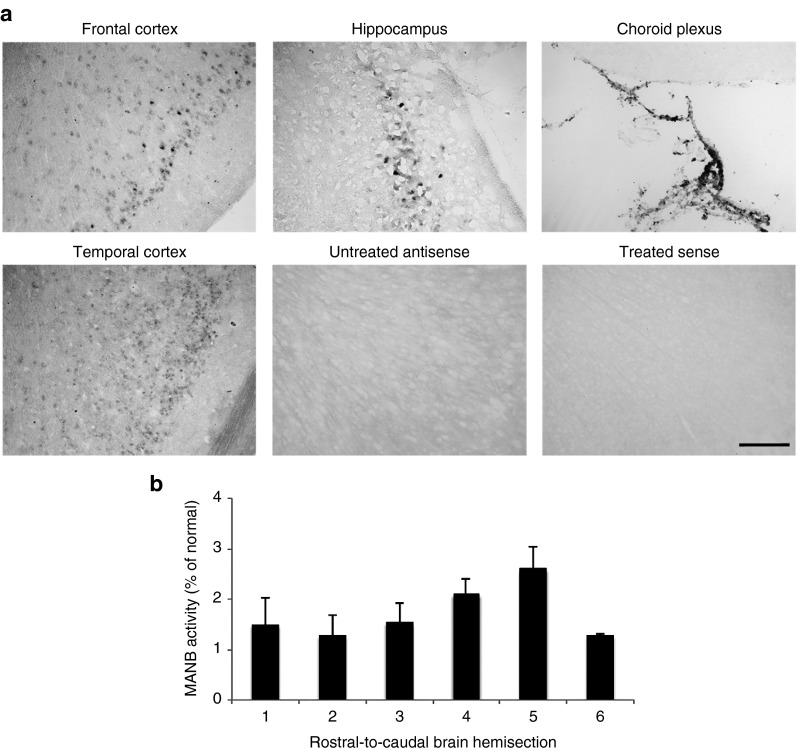
The postmortem analysis was performed when the treated cats were euthanized at 30–44 weeks of age. Since there is no suitable antibody to show expression of alpha-mannosidase by immunohistochemistry, we used in situ hybridization against the fMANB mRNA expressed from the vector to assess distribution of gene expression in the treated AMD cats. The background is negative due to the 4 bp deletion in the feline MANB gene that causes a translational frame shift and premature termination resulting in nonsense-mediated mRNA decay.26 Part of the cerebral cortex is shown in Figure 5a, which shows extensive transduction. The pattern of cells transduced was similar to the transduction by AAV1-eGFP vector in the normal cat brain (Figure 2) but the two methods look visually different because in situ hybridization is localized to the nucleus, whereas the GFP immunohistochemistry reacts with the whole cell since the GFP is a cytosolic protein. A strong in situ hybridization signal to the vector-encoded MANB mRNA was detected in the cerebral cortex, hippocampus, and choroid plexus epithelial cells within the lateral ventricle (Figure 5a). Brains from uninjected animals were negative for MANB mRNA and the sense probe, used as a control in a treated animal, also detected no signal.
Figure 5.
Widespread distribution of feline alpha-mannosidase (fMANB) mRNA transcripts and MANB enzymatic activity in treated alpha-mannosidosis (AMD) cat brain. (a) In situ hybridization (ISH) against the vector-encoded fMANB mRNA demonstrated a strong ISH signal in the cerebral cortex, hippocampus, and choroid plexus epithelial cells of the treated AMD cat brain. Brains from uninjected animals were negative for fMANB mRNA and the sense probe, used as a control in a treated animal, also detected no signal. The amount of MANB enzymatic activity was measured in coronal sections taken at intervals along the rostral–caudal axis as shown in Figure 2a. (b) The mean activity values for treated AMD cats (n = 4) in transverse slices along the rostral–caudal axis show the wide spatial distribution within the cat brain. Bars represent means ± SEM. Bar = 200 µm. MANB, lysosomal alpha-mannosidase.
The distribution of gene transfer after cisterna magna injection was evident throughout the cat brain. To evaluate this further, we measured the amount of MANB enzymatic activity in coronal sections taken at intervals along the rostral–caudal axis as shown in Figure 2a. The MANB enzymatic activities in the treated brains were calculated as the percentage between untreated AMD brain sections (0%) and normal cat brain sections (100%). The mean activity values for four treated AMD cats in transverse slices spaced along the rostral–caudal axis of the brain show the long-term wide spatial distribution within the cat brain after cisterna magna injection (Figure 5b).
Correction of lysosomal storage lesions in treated AMD cat brains
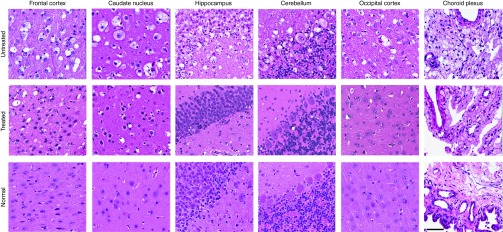
To assess whether the low levels of MANB activity could mediate a therapeutic benefit, histopathology of hematoxylin and eosin–stained brain sections were evaluated. Hematoxylin and eosin–stained sections showed resolution of lysosomal storage vacuoles throughout the brain, including in the cerebral cortex, caudate nucleus, hippocampus, cerebellum, and choroid plexus (Figure 6).
Figure 6.
Correction of lysosomal storage lesions on hematoxylin and eosin (H&E)-stained brain tissue of treated alpha-mannosidosis cats. H&E-stained brain sections of treated cats showed resolution of lysosomal storage vacuoles throughout the brain, including in the cerebral cortex, caudate nucleus, hippocampus, cerebellum, and choroid plexus. Bar = 60 µm.
Discussion
Achieving widespread gene transfer throughout the entire brain, especially in humans, is a major challenge. It is a critical barrier in the treatment of neurogenetic diseases because the pathology is usually distributed globally. Cisterna magna delivery of an AAV vector results in transduction of ependymal and choroid plexus cells, which can then continuously secrete vector-encoded proteins into the CSF. In addition, our data show that AAV1 also transduces many cells in the brain parenchyma itself, particularly cortical neurons.
This route of vector delivery is simple and not as invasive as injecting vectors along multiple injection tracks throughout the brain, for which a very large number of injections will be needed to achieve widespread gene transfer in a human brain.13,27,28 Cisterna magna vector injection is also more specific to the CNS compared to systemic i.v. administration of vector.28 Injecting the vector directly into the CSF circumvents the blood–brain barrier and a lower total dose can be used than with i.v. delivery.
This study shows that a single injection of AAV1 results not only in sustained expression and improvement in pathology within the CNS but is also sufficient to moderate neurologic signs. A striking result in our study was that cisterna magna delivery of AAV1 resulted in predominantly neuronal transduction throughout the whole brain. Although choroid plexus and ependymal cells were transduced, many cells in the brain parenchyma were transduced and not only in regions proximal to the ventricular system. CSF injections of AAV9, AAVrh.10, and AAV2.5 have also shown variable degrees of transduction in the brains of large animals, albeit in normal animals (cats, dogs, and monkeys).16,17,18,19,20,21,22,23
Domestic animals with essentially the same disease as human patients serve as a critical test of the potential for effective treatment of the human disease. Dog and cat brains are more similar in organization to the human brain than rodent brains; most prominently they have a gyrencephalic cerebral cortex. They also are much closer in size to the human brain, with a 1-year-old human brain being ~2,000 times larger than a mouse brain but only 25 times larger than a cat's. CSF-directed delivery of AAV vectors has been studied in two large animal disease models, both using AAV9 in cats: (i) one found transduction of motor neurons and oligodendrocytes in the spinal cord but expression of a trophic factor failed to improve lower motor neuron pathology29 and (ii) another showed correction of histopathology in the Hurler disease brain but no clinical improvement was seen,22 although Hurler disease has severe symptoms in skeletal and other non-neurological organs which may mask neurological signs. Our results with cisterna magna AAV1 delivery in the AMD cat demonstrate that widespread correction of the storage lesions in the brain can improve the neurological clinical syndrome as well as extend the lifespan of treated animals.
Low levels of normal enzymatic activity from somatic gene transfer can mediate substantial amounts of tissue correction in LSD models.13,30 In the present study, the enzymatic activity values of MANB as a percentage of normal was initially high in the CSF then dropped, but low in serum and then increased. The values appeared to equilibrate in the 1–2% range in both compartments after 3 months. Lysosomal enzymes can be transported from brain transduction into peripheral tissues, probably via the bulk transport from CSF to the venous system.31 Although the serum values of individual AMD cats varied at specific time points, measuring serum MANB activity over time could be useful as a minimally invasive procedure for monitoring the presence of the therapeutic enzyme in patients treated by cisterna magna infusion of AAV1.
Human AMD is characterized by severe-to-mild psychomotor retardation but also includes hearing loss, dysostosis multiplex, hepatosplenomegaly, and ocular impairment. Animals with AMD have essentially the same genetic, biochemical, and clinical abnormalities as human patients.32 The most prominent clinical symptoms of AMD are related to the neurological disease and some neurological signs were improved. Lifespan was significantly increased but the cats eventually succumbed to the disease. Thus, while the AAV gene infusion into the CSF resulted in significant clinical benefit, it was not curative. Small amounts of storage lesions were still visible in some cells of the brain thus some remaining neurological dysfunction may contribute to the eventual demise. Another potential contributor would be that disease which was present before the initiation of therapy also contributed. However, this is the situation with most human LSD patients who need to be treated postsymptomatically because they are not diagnosed until they manifest clinical signs. Nevertheless, the treatment did mediate great reduction of storage lesions throughout the brain after a single infusion of AAV1 vector via the cistern magna, improvement in clinical signs, and extended lifespan. Thus, the single cisterna magna infusion of the AAV1 vector has strong translational potential for the treatment of AMD and other LSDs, as well as for widespread targeting of gene transfer to neurons in other CNS disorders.
Materials and Methods
Plasmid and rAAV production. eGFP and fMANB gene were cloned into the AAV packaging plasmid pZac2.1, provided by the Vector Core of the University of Pennsylvania (Philadelphia, PA). The vector genome contained AAV2 terminal repeats, a human GUSB promoter, simian virus 40 splice donor/acceptor signal, and bovine growth hormone polyadenylation signal. Recombinant AAV1 vectors were produced by the University of Pennsylvania Vector Core using triple transfection of HEK293 cells with AAV cis-plasmid, AAV trans-plasmid containing AAV rep and cap genes, and adenovirus helper plasmid. Vectors were purified using iodixanol gradient ultracentrifugation and the titers were determined by real-time PCR.33
Animals and vector injections. All animal care and procedures were in accordance with the Institutional Animal Care and Use Committee at the University of Pennsylvania, and all studies were conducted in accordance with the US Public Health Service's Policy on Humane Care and Use of Laboratory Animals. Normal and AMD-affected cats (4–6 weeks old) produced in the breeding colony of the University of Pennsylvania veterinary school were used for cat experiments. Cats were anesthetized with i.v. propofol (up to 6 mg/kg). Using sterile techniques, ~0.5 ml of CSF was collected using a 22-gauge spinal needle from the cerebellomedullary cistern. After collecting the CSF, AAV1-eGFP or AAV1-fMANB (1 × 1013 GC) was injected. Cats were monitored after procedure until fully recovered.
Neurological examinations. Neurological examinations were performed monthly from treatment by the same blind observer who was unaware of whether cats were treated or not. The onset and progression as well as the severity of signs of neurologic dysfunction were identified. Tremor was graded on a 0–3 scale (0: none; +1: mild; +2: moderate; +3: severe). Ataxia was graded on a 0–4 scale (0: none; +1: mild ataxia; +2: moderate ataxia resulting in falling when running; +3: severe ataxia resulting in falling when walking; +4: no longer able to stand).
MANB enzymatic activity assay. MANB enzymatic activity was measured in CSF, serum, or brain tissue homogenized in saline containing 0.2% Triton X-100. Enzyme activity was determined using 5 mmol/l 4-methylumbelliferyl α-d-mannopyranoside in 0.1 mol/l sodium citrate buffer (pH 4.4) at 37 °C for 1 hour. Protein was quantified using bicinchoninic acid assay.
Tissue collection. Cats were euthanized by using an overdose of i.v. barbiturates. After sacrifice, cats were transcardially perfused with 700 ml of 0.9% cold saline and tissues were drop-fixed in 4% paraformaldehyde for 48 hours. Tissues were embedded in 2% agarose and sectioned coronally at 50 µm on a vibratome (Leica VT1000S; Leica, Buffalo Grove, IL) for subsequent immunohistochemical staining. For cryosectioning, brains were cryoprotected in 30% sucrose, embedded in optimum cutting temperature solution (Sakura, Torrance, CA), and then cryosectioned at 20 µm thickness using a cryostat (Leica Microsystems, Wetzlar, Germany) for in situ hybridization. For histology, tissues were paraffin embedded and stained with hematoxylin and eosin. For serum collection, the whole blood was incubated for 30 minutes at room temperature followed by centrifugation at 1,000g for 15 minutes. The supernatant was then aspirated and stored at −80 °C.
Immunohistochemistry. GFP-positive cells were labeled using standard immunohistochemistry. Free-floating sections were permeabilized and immunoblocked for 30 minutes in 4% goat or donkey serum in PBS-T (phosphate-buffered saline containing 0.3% Triton X-100). The sections were then incubated overnight at 4 °C with the rabbit anti-GFP (1:1,000; Molecular Probes, Grand Island, NY) antibody. After three washes in PBS-T, sections were washed in PBS-T and incubated with the appropriate biotinylated secondary antibodies (goat anti-rabbit, 1:250; Vector Laboratories, Burlingame, CA) for 45 minutes followed by PBS-T washes. The antibody binding was visualized using VECTASTAIN Elite ABC reagent and 3,3′-diaminobenzidine substrate kit for peroxidase (Vector Laboratories, Burlingame, CA). Sections were then mounted onto glass slides, dehydrated, and mounted in Cytoseal 60 mounting medium (Richard Allen Scientific, Kalamazoo, MI) with glass coverslips. Images were visualized using a Leica AF6000 LX microscope (Leica, Heerbrugg, Switzerland) and acquired using a DFC 425 digital camera (Leica).
In situ hybridization. Sense and antisense DNA templates for RNA transcription were synthesized by PCR using fMANB sequence in the pZac2.1 plasmid as the template with primers containing T7 or T3 RNA polymerase promoters upstream. Digoxigenin (DIG)-labeled RNA probes were produced using the DNA templates with the DIG RNA labeling kit (Roche Applied Science, Indianapolis, IN). The integrity and size of the labeled RNA probes were verified on a nondenaturing agarose gel and compared to the control RNA of the same length. Frozen sections were hybridized with DIG-labeled riboprobes specific for vector fMANB sequence, and DIG-positive cells were visualized by anti-DIG–alkaline phosphatase antibody (Roche Applied Science, Indianapolis, IN) followed by NBT–BCIP substrate (Roche Applied Science) for colorimetric detection of alkaline phosphatase. Whole slides were scanned using the Aperio scanscope (Aperio, Vista, CA).
Statistical analysis. Unpaired two-tailed Student's t-test and one-way analysis of variance were used, where applicable, to determine whether mean differences between groups were different and were considered significant when P <0.05. Log-rank (Mantel–Cox) test was used to demonstrate difference in survival between the treated and untreated cats. Data are reported as means ± SEM unless otherwise stated.
Acknowledgments
We thank E. Cabacungan and A. Polesky for excellent technical assistance, all of the veterinary students who assisted in clinical care of animals, and S. Kaler of the NICHD for the helpful discussions. This work was supported by NIH grants R01-DK063973, a Bench-to-Bedside Award attached to R01-NS038690, U01-HD079066, P40-OD010939, and UL1-TR000003. S.Y.Y. was supported in part by NIH training grant T32-NS007180.
References
- Auclair, D, Finnie, J, White, J, Nielsen, T, Fuller, M, Kakkis, E et al. (2010). Repeated intrathecal injections of recombinant human 4-sulphatase remove dural storage in mature mucopolysaccharidosis VI cats primed with a short-course tolerisation regimen. Mol Genet Metab 99: 132–141. [DOI] [PubMed] [Google Scholar]
- Chang, M, Cooper, JD, Sleat, DE, Cheng, SH, Dodge, JC, Passini, MA et al. (2008). Intraventricular enzyme replacement improves disease phenotypes in a mouse model of late infantile neuronal ceroid lipofuscinosis. Mol Ther 16: 649–656. [DOI] [PubMed] [Google Scholar]
- Crawley, AC, Marshall, N, Beard, H, Hassiotis, S, Walsh, V, King, B et al. (2011). Enzyme replacement reduces neuropathology in MPS IIIA dogs. Neurobiol Dis 43: 422–434. [DOI] [PubMed] [Google Scholar]
- Dierenfeld, AD, McEntee, MF, Vogler, CA, Vite, CH, Chen, AH, Passage, M et al. (2010). Replacing the enzyme alpha-L-iduronidase at birth ameliorates symptoms in the brain and periphery of dogs with mucopolysaccharidosis type I. Sci Transl Med 2: 60ra89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodge, JC, Clarke, J, Treleaven, CM, Taksir, TV, Griffiths, DA, Yang, W et al. (2009). Intracerebroventricular infusion of acid sphingomyelinase corrects CNS manifestations in a mouse model of Niemann-Pick A disease. Exp Neurol 215: 349–357. [DOI] [PubMed] [Google Scholar]
- Hemsley, KM and Hopwood, JJ (2009). Delivery of recombinant proteins via the cerebrospinal fluid as a therapy option for neurodegenerative lysosomal storage diseases. Int J Clin Pharmacol Ther 47 (suppl. 1): S118–S123. [DOI] [PubMed] [Google Scholar]
- Hemsley, KM, King, B and Hopwood, JJ (2007). Injection of recombinant human sulfamidase into the CSF via the cerebellomedullary cistern in MPS IIIA mice. Mol Genet Metab 90: 313–328. [DOI] [PubMed] [Google Scholar]
- Kakkis, E, McEntee, M, Vogler, C, Le, S, Levy, B, Belichenko, P et al. (2004). Intrathecal enzyme replacement therapy reduces lysosomal storage in the brain and meninges of the canine model of MPS I. Mol Genet Metab 83: 163–174. [DOI] [PubMed] [Google Scholar]
- Lee, WC, Tsoi, YK, Troendle, FJ, DeLucia, MW, Ahmed, Z, Dicky, CA et al. (2007). Single-dose intracerebroventricular administration of galactocerebrosidase improves survival in a mouse model of globoid cell leukodystrophy. FASEB J 21: 2520–2527. [DOI] [PubMed] [Google Scholar]
- Vera, M, Le, S, Kan, SH, Garban, H, Naylor, D, Mlikotic, A et al. (2013). Immune response to intrathecal enzyme replacement therapy in mucopolysaccharidosis I patients. Pediatr Res 74: 712–720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fratantoni, JC, Hall, CW and Neufeld, EF (1968). Hurler and Hunter syndromes: mutual correction of the defect in cultured fibroblasts. Science 162: 570–572. [DOI] [PubMed] [Google Scholar]
- Liu, G, Martins, I, Wemmie, JA, Chiorini, JA and Davidson, BL (2005). Functional correction of CNS phenotypes in a lysosomal storage disease model using adeno-associated virus type 4 vectors. J Neurosci 25: 9321–9327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vite, CH, McGowan, JC, Niogi, SN, Passini, MA, Drobatz, KJ, Haskins, ME et al. (2005). Effective gene therapy for an inherited CNS disease in a large animal model. Ann Neurol 57: 355–364. [DOI] [PubMed] [Google Scholar]
- Ciron, C, Desmaris, N, Colle, MA, Raoul, S, Joussemet, B, Vérot, L et al. (2006). Gene therapy of the brain in the dog model of Hurler's syndrome. Ann Neurol 60: 204–213. [DOI] [PubMed] [Google Scholar]
- McCurdy, VJ, Johnson, AK, Gray-Edwards, HL, Randle, AN, Brunson, BL, Morrison, NE et al. (2014). Sustained normalization of neurological disease after intracranial gene therapy in a feline model. Sci Transl Med 6: 231ra48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haurigot, V, Marco, S, Ribera, A, Garcia, M, Ruzo, A, Villacampa, P et al. (2013). Whole body correction of mucopolysaccharidosis IIIA by intracerebrospinal fluid gene therapy. J Clin Invest 123: 3254–3271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bevan, AK, Duque, S, Foust, KD, Morales, PR, Braun, L, Schmelzer, L et al. (2011). Systemic gene delivery in large species for targeting spinal cord, brain, and peripheral tissues for pediatric disorders. Mol Ther 19: 1971–1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samaranch, L, Salegio, EA, San Sebastian, W, Kells, AP, Foust, KD, Bringas, JR et al. (2012). Adeno-associated virus serotype 9 transduction in the central nervous system of nonhuman primates. Hum Gene Ther 23: 382–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray, SJ, Nagabhushan Kalburgi, S, McCown, TJ and Jude Samulski, R (2013). Global CNS gene delivery and evasion of anti-AAV-neutralizing antibodies by intrathecal AAV administration in non-human primates. Gene Ther 20: 450–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bucher, T, Dubreil, L, Colle, MA, Maquigneau, M, Deniaud, J, Ledevin, M et al. (2014). Intracisternal delivery of AAV9 results in oligodendrocyte and motor neuron transduction in the whole central nervous system of cats. Gene Ther 21: 522–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer, K, Ferraiuolo, L, Schmelzer, L, Braun, L, McGovern, V, Likhite, S et al. (2015). Improving single injection CSF delivery of AAV9-mediated gene therapy for SMA: a dose-response study in mice and nonhuman primates. Mol Ther 23: 477–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinderer, C, Bell, P, Gurda, BL, Wang, Q, Louboutin, JP, Zhu, Y et al. (2014). Intrathecal gene therapy corrects CNS pathology in a feline model of mucopolysaccharidosis I. Mol Ther 22: 2018–2027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, H, Yang, B, Qiu, L, Yang, C, Kramer, J, Su, Q et al. (2014). Widespread spinal cord transduction by intrathecal injection of rAAV delivers efficacious RNAi therapy for amyotrophic lateral sclerosis. Hum Mol Genet 23: 668–681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vite, CH, Passini, MA, Haskins, ME and Wolfe, JH (2003). Adeno-associated virus vector-mediated transduction in the cat brain. Gene Ther 10: 1874–1881. [DOI] [PubMed] [Google Scholar]
- Vite, CH, McGowan, JC, Braund, KG, Drobatz, KJ, Glickson, JD, Wolfe, JH et al. (2001). Histopathology, electrodiagnostic testing, and magnetic resonance imaging show significant peripheral and central nervous system myelin abnormalities in the cat model of alpha-mannosidosis. J Neuropathol Exp Neurol 60: 817–828. [DOI] [PubMed] [Google Scholar]
- Berg, T, Tollersrud, OK, Walkley, SU, Siegel, D and Nilssen, O (1997). Purification of feline lysosomal alpha-mannosidase, determination of its cDNA sequence and identification of a mutation causing alpha-mannosidosis in Persian cats. Biochem J 328 (Pt 3): 863–870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sondhi, D, Johnson, L, Purpura, K, Monette, S, Souweidane, MM, Kaplitt, MG et al. (2012). Long-term expression and safety of administration of AAVrh.10hCLN2 to the brain of rats and nonhuman primates for the treatment of late infantile neuronal ceroid lipofuscinosis. Hum Gene Ther Methods 23: 324–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simonato, M, Bennett, J, Boulis, NM, Castro, MG, Fink, DJ, Goins, WF et al. (2013). Progress in gene therapy for neurological disorders. Nat Rev Neurol 9: 277–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bucher, T, Colle, MA, Wakeling, E, Dubreil, L, Fyfe, J, Briot-Nivard, D et al. (2013). scAAV9 intracisternal delivery results in efficient gene transfer to the central nervous system of a feline model of motor neuron disease. Hum Gene Ther : 670–682. [DOI] [PubMed]
- Wolfe, JH, Sands, MS, Barker, JE, Gwynn, B, Rowe, LB, Vogler, CA et al. (1992). Reversal of pathology in murine mucopolysaccharidosis type VII by somatic cell gene transfer. Nature 360: 749–753. [DOI] [PubMed] [Google Scholar]
- Karolewski, BA and Wolfe, JH (2006). Genetic correction of the fetal brain increases the lifespan of mice with the severe multisystemic disease mucopolysaccharidosis type VII. Mol Ther 14: 14–24. [DOI] [PubMed] [Google Scholar]
- Sun, H and Wolfe, JH (2001). Recent progress in lysosomal alpha-mannosidase and its deficiency. Exp Mol Med 33: 1–7. [DOI] [PubMed] [Google Scholar]
- Lock, M, Alvira, M, Vandenberghe, LH, Samanta, A, Toelen, J, Debyser, Z et al. (2010). Rapid, simple, and versatile manufacturing of recombinant adeno-associated viral vectors at scale. Hum Gene Ther 21: 1259–1271. [DOI] [PMC free article] [PubMed] [Google Scholar]