Abstract
Objectives:
This study aimed to compare the microleakage beneath metallic brackets following two different methods of enamel preparation and light curing.
Materials and Methods:
A total of 120 bovine deciduous lower incisors were randomly divided into four groups of 30 teeth. The preparations were as follows: Group I: Acid etching + Transbond XT primer + direct illumination, group II: acid etching + Transbond XT primer + transillumination, group III: Transbond XT self-etching primer + direct illumination and Group IV: Transbond XT self-etching primer + transillumination. Dye penetration was used as the method of microleakage evaluation. Sections made at the enamel-adhesive and adhesive-bracket interfaces were evaluated under a stereomicroscope. The Kruskal-Wallis and Mann-Whitney U tests were used for statistical analysis. The level of significance was set at P<0.05.
Results:
All groups showed greater microleakage at the gingival in comparison to the incisal margin and the differences were significant among groups with transillumination (P<0.001). No significant differences were observed in the microleakage scores at the gingival and incisal margins in any of the interfaces (P>0.05). Mesiodistal margins of the self-etching group with direct illumination showed significantly lower scores in comparison with acid etched group (P<0.05).
Conclusion:
Use of self-etching primers for bonding of orthodontic brackets yields acceptable results if all bracket margins are cured directly.
Keywords: Orthodontic brackets, Self-etch primer, Transillumination
INTRODUCTION
Iatrogenic demineralization of enamel during orthodontic treatment is a concern for orthodontists [1]. Several attempts have been made to address this problem such as diet changes, lowering carbohydrate intake, efficient oral hygiene measures and rinsing fluoride mouthwashes [2]. Application of sealants [3], fluoride releasing bonding agents [4], elastic modules impregnated with fluoride [5] and fluoride varnishes are the most commonly used preventative methods by orthodontists. Despite all these efforts, we still witness white spot lesions following bracket removal. If a void exists between the adhesive and enamel surface at the margin of brackets, this could lead to microleakage and accumulation of cariogenic bacteria in inaccessible areas [6,7]. Such voids are responsible for some cases of white spot lesions. These lesions occur in about 45% of orthodontic patients [4] and according to a previous study, they have a higher incidence in males [8]. They are unsightly and appear as enamel opacity, involving at least one-third of the labial surface [9]. Occasionally, they may result in discontinuation of treatment without achieving the treatment goals. Another concern is the gap between metal brackets and adhesives. Empty pockets at the margins of this interface should be prevented. Corrosion and craters in the stainless steel bracket base initiate at the gap developed between the brackets and adhesives.
Arhun et al. investigated the amount of microleakage following the application of different adhesive systems for bonding ceramic and metal brackets. In their study, the amount of microleakage was reported to be higher beneath the metal brackets at both interfaces regardless of the adhesive system used [6].
Uysal et al, also reported higher amount of microleakage at the gingival in comparison to the occlusal margin (light curing was done at the occlusal margin for both adhesive systems) [7]. Although use of light activated composites has become popular in orthodontics, prevention of light penetration by metal brackets, the most commonly used attachments in fixed orthodontics, is a major concern [10]. Also, the stress due to the polymerization shrinkage is among the most important problems associated with light-activated composites [11].
If the contracting forces of curing resins overcome the bond of adhesive, marginal failure and microleakage may result [12]. To overcome this side effect, various curing procedures have been proposed.
The suggested three-sided light curing technique was based on the assumption that contraction of photo-activated composite resin is directed toward the light source [13]. In our study, the transillumination technique was used to assess its efficacy for bonding of metal brackets. This method was initially suggested for cementation of acid-etched fixed partial dentures. In this technique, the light is illuminated from the back of the teeth with attachments [14]. Some previous studies have investigated the bond strength of visible light-cured composites using transillumination as a curing technique [15–18].
In 2013, Kumar et al. showed that 90% of light intensity was lost when using transillumination technique for bonding brackets. They demonstrated that this reduction was related to the buccolingual dimension of teeth. However, they found that both the conventional method and transillumination technique yielded similar results in terms of bond strength of metal brackets [17].
Also, in 2013 Heravi et al. concluded that to achieve an acceptable bracket bond strength for the posterior teeth, doubling the curing time from 40 to 80 seconds and increasing the light intensity to 800 mW/cm2 during transillumination technique were required [18]. From the previous studies it can be concluded that transillumination is an applicable technique for improving the bond strength; however, marginal seal is also an important factor to prevent marginal corrosion and bacterial attacks, and inappropriate marginal seal can lead to white spot lesions or bracket bond failure during the course of treatment. To the best of our knowledge, no study has evaluated the effect of transillumination as a curing technique on the microleakage beneath metal orthodontic brackets. The aim of this study was to evaluate the effect of transillumination as a light curing technique on the amount of microleakage, in comparison to the conventional technique of curing, using two methods of enamel conditioning.
MATERIALS AND METHODS
According to a study by Arhun et al, 120 freshly extracted bovine deciduous mandibular incisors were collected for this study [6]. The teeth were examined to be free of surface developmental defects and cracks under direct light. The soft tissue remnants and the debris were removed and the specimens were polished with pumice paste and rubber cups for 10 seconds each, and were then stored in distilled water for one month. Before the onset of the bonding process, all the specimens were disinfected by immersion in 1% thymol solution for one week.
The middle-third of the enamel surface of each tooth was prepared using two enamel preparation methods. The first method included the use of 37% phosphoric acid gel (Unitek, Monrovia, CA) for enamel conditioning and Transbond XT primer (3M, Unitek, Monrovia, CA) as a sealant. In the second method, Transbond Plus (3M, Unitek, Monrovia, CA) was applied as self-etching primer. The stainless steel twin maxillary central incisor brackets (.022-in-Daynalock series, 3M, Monrovia, CA) were bonded on the middle third of the buccal surface in all samples with Transbond XT (3M, Unitek, Monrovia, CA), a light-cured orthodontic resin, using a light curing unit (Coltolux 75, Coltene/Whaledent GmbH, Langenau, Germany) with a light intensity of 530 mW/mm2.
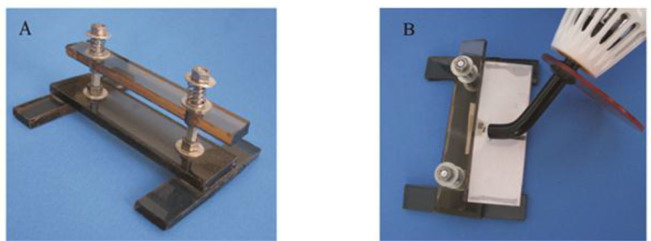
In order to maintain a fixed distance and angle of light curing, a holder was designed and used to set the position of the samples at 5 mm distance from the tip of the light-curing unit. The device held the samples vertically in such a way that the tip of the light-curing unit was perpendicular to the long axis of the samples on both sides depending on the group of samples (Fig. 1). The samples were randomly divided into four groups of 30 teeth and were prepared as follows:
Group I: The teeth were etched with 37% phosphoric acid for 30 seconds, and then rinsed and dried for 20 seconds with oil-free air spray. The brackets were bonded using Transbond XT primer as the sealant and Transbond XT as the adhesive. Finally, the mesial and distal margins of the brackets were light cured for 10 seconds each.
Group II: The same methods of enamel preparation and bracket bonding were applied as in group I; but transillumination (applying the light source to the middle third of the lingual surface) was used for 50 seconds as the technique of resin polymerization.
Group III: Transbond Plus self-etching primer was applied for 3–5 seconds with mild pressure of the brush according to the manufacturer’s instructions, followed by a gentle burst of air for 1–2 seconds. Then, the brackets were bonded using Transbond XT and 10 seconds of light curing was performed at the mesial and distal margins.
Group IV: The same method of enamel preparation as in group III was applied; but transillumination for 50 seconds from the lingual side was used as the method of curing. Thermal cycling in deionized water was performed at 5 ± 2° C – 55 ± 2° C for 500 cycles with a dwell time of 30 seconds and transfer time of 5 seconds. Then, the samples were stored in distilled water at room temperature and a dark environment for three months for the aging process.
Fig. 1.
(A) The holder used for sample preparation. (B) Light curing of a sample fixed in the holder.
Microleakage evaluation:
For evaluation of microleakage in all margins, each group was randomly divided into two subgroups of 15 samples in order to perform tooth sectioning in two different directions. In subgroup one, the teeth were sectioned from the middle of the brackets in incisogingival direction while in subgroup two, the teeth were sectioned in mesiodistal direction to evaluate the margins that were directly light cured as instructed by the manufacturer. The apices of all teeth were sealed with sticky wax and then all surfaces were coated with two layers of nail varnish except for 1 mm around the bracket margins. In the next step, the samples were immersed in 0.5% basic fuchsine solution for 24 hours at room temperature.
After removal from the solution, the teeth were rinsed with distilled water, the superficial dye was removed with a brush and the teeth were left to dry.
The samples were embedded in epoxy resin blocks according to the direction of sections using an index in the heavy putty impression (Fig. 2).
Fig. 2.
One sample fixed in the holding chuck of the cutting machine (Struers, Denmark) before sectioning (A) and after sectioning (B)
Sectioning was carried out using a low-speed diamond saw (Accutom-50, Struers, Denmark).
All samples were numbered before sectioning according to their group allocation and were examined randomly under a stereomicroscope (Motic, Xiamen, China) at ×40 magnification. The microleakage scores were directly recorded using an electronic digital caliper (GuangLu Measuring Instrument Co. Ltd, Shanghai, China) by a single blinded observer (SH.A).
Half of the samples were randomly examined blindly for the second time under the same stereomicroscope by the same observer (SH.A) after a week to assess the intra-observer error of measurements. The incisogingival and mesiodistal dimensions of each section were examined at enamel-adhesive and adhesive-bracket interfaces (in each side) and scored based on the amount of microleakage (Fig. 3).
Fig. 3.
Stereomicroscopic views (A and B) of a sample sectioned in mesiodistal direction (black arrow: enamel-adhesive interface, white arrow: adhesive-bracket interface)
Statistical analysis:
For data analysis, the mean and standard deviation values of all groups were obtained using SPSS version 15.0 (Microsoft, IL, USA).
To compare the sides and interfaces within each group (dependent samples), the non-parametric Wilcoxon Singed Rank test was used. The Kruskal-Wallis (independent non-parametric test) and the Mann-Whitney U tests with Bonferroni correction were used to compare the groups. Intra-examiner error was evaluated by the kappa statistic. The level of statistical significance was set at α=0.05.
RESULTS
The overall intra-observer agreement for each group was high (kappa value of 0.792).
In case of disagreements, the mean of measurements was reported. All groups showed microleakage at the incisal and gingival margins; but in comparison between conventional and transillumination groups, significant differences were observed only between incisal and gingival margins in the transillumination group (P<0.001).
Comparison of mesial and distal margins revealed no statistically significant differences in any group (P>0.05). When direct illumination and transillumination were compared as the two methods of curing, the amount of microleakage was significantly higher at the gingival margins compared to the incisal margins in both interfaces in the transillumination group irrespective of the method of enamel preparation (P<0.05).
At the mesial and distal margins, there were no differences among the groups (Tables 1 and 2). Comparison of groups based on the method of enamel conditioning revealed no significant differences at the incisal and gingival margins in any of the interfaces; but at the mesial and distal margins, only group seven (self-etching primer + direct illumination) showed significantly lower microleakage score in comparison with group five (acid-etching + direct illumination) (P=0.001).
Table 1.
Comparison of microleakage scores (mm) between enamel-adhesive and adhesive-bracket interfaces in buccolingual sectionsa
| Margin | N | Groupb | Enamel-adhesive | Adhesive-bracket | P value | |||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||||
| Incisal | 15 | 1 | 0.18 | 0.10 | 0.13 | 0.19 | .066 | NS |
| 15 | 2 | 0.16 | 0.16 | 0.13 | 0.12 | .475 | NS | |
| 15 | 3 | 0.18 | 0.10 | 0.14 | 0.12 | .125 | NS | |
| 15 | 4 | 0.12 | 0.10 | 0.12 | 0.13 | .553 | NS | |
| Gingival | 15 | 1 | 0.21 | 0.18 | 0.18 | 0.22 | .476 | NS |
| 15 | 2 | 0.40 | 0.16 | 0.35 | 0.14 | .142 | NS | |
| 15 | 3 | 0.21 | 0.09 | 0.21 | 0.13 | .556 | NS | |
| 15 | 4 | 0.34 | 0.14 | 0.26 | 0.09 | .056 | NS | |
N indicates sample size; SD, standard deviation; S, significant; NS, not significant
Group 1: Acid etching + direct illumination; Group 2: Acid etching + transillumination; Group 3: Self etching primer + direct illumination; Group 4: Self etching primer + transillumination.
Table 2.
Comparison of microleakage scores (mm) between enamel-adhesive and adhesive-bracket interfaces in mesiodistal sectionsa
| Margin | N | Groupb | Enamel-adhesive | Adhesive-bracket | P value | |||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||||
| Mesial | 15 | 5 | 0.19 | 0.18 | 0.18 | 0.15 | .783 | NS |
| 15 | 6 | 0.14 | 0.13 | 0.17 | 0.15 | 261 | NS | |
| 15 | 7 | 0.03 | 0.04 | 0.16 | 0.16 | .018 | S | |
| 15 | 8 | 0.07 | 0.10 | 0.17 | 0.14 | .054 | NS | |
| Distal | 15 | 5 | 0.22 | 0.21 | 0.26 | 0.22 | .414 | NS |
| 15 | 6 | 0.13 | 0.15 | 0.14 | 0.16 | .767 | NS | |
| 15 | 7 | 0.02 | 0.04 | 0.17 | 0.15 | .008 | S | |
| 15 | 8 | 0.10 | 0.12 | 0.14 | 0.10 | .332 | NS | |
N indicates sample size; SD, standard deviation; S, significant; NS, not significant
Group 5: Acid etching + direct illumination; Group 6: Acid etching + transillumination; Group 7: Self etching primer + direct illumination; Group 8: Self etching primer + transillumination
Multiple comparisons among all groups are shown in Tables 3 and 4 with Bonferroni correction.
Table 3.
Multiple comparisons of microleakage scores among groups at incisal and gingival margins in enamel-adhesive and adhesive-bracket interfacesa
| Interface | Margin | N | Groupb | One-way ANOVA P value | Multiple Comparisons | ||
|---|---|---|---|---|---|---|---|
| Group 2 | Group 3 | Group 4 | |||||
| Enamel-adhesive interface | Incisal | 15 | Group 1 | .492 | NS | NS | |
| 15 | Group 2 | NS | |||||
| 15 | Group 3 | NS | |||||
| 15 | Group 4 | ||||||
| Gingival | 15 | Group 1 | .003 | ** | NS | ||
| 15 | Group 2 | NS | |||||
| 15 | Group 3 | * | |||||
| 15 | Group 4 | ||||||
| Adhesive-bracket interface | Incisal | 15 | Group 1 | .932 | NS | NS | |
| 15 | Group 2 | NS | |||||
| 15 | Group 3 | NS | |||||
| 15 | Group 4 | ||||||
| Gingival | 15 | Group 1 | .006 | * | NS | ||
| 15 | Group 2 | NS | |||||
| 15 | Group 3 | * | |||||
| 15 | Group 4 | ||||||
N indicates sample size; SD, standard deviation; S, significant; NS, not significant;
P< 0.05;
P<0.01
Group 1: Acid etching + direct illumination; Group 2: Acid etching + transillumination; Group 3: Self etching primer + direct illumination; Group 4: Self etching primer + transillumination.
Table 4.
Multiple comparisons of microleakage scores among groups at the mesial and distal margins in enamel-adhesive and adhesive-bracket interfacesa
| Interface | Margin | N | Groupb | P value | Multiple comparisons | ||
|---|---|---|---|---|---|---|---|
| Group 6 | Group 7 | Group 8 | |||||
| Enamel-adhesive interface | Mesial | 15 | Group 5 | .012 | NS | ** | |
| 15 | Group 6 | NS | |||||
| 15 | Group 7 | NS | |||||
| 15 | Group 8 | ||||||
| Distal | 15 | Group 5 | .008 | NS | ** | ||
| 15 | Group 6 | NS | |||||
| 15 | Group 7 | NS | |||||
| 15 | Group 8 | ||||||
| Adhesive-bracket interface | Mesial | 15 | Group 5 | .955 | NS | NS | |
| 15 | Group 6 | NS | |||||
| 15 | Group 7 | NS | |||||
| 15 | Group 8 | ||||||
| Distal | 15 | Group 5 | .271 | NS | NS | ||
| 15 | Group 6 | NS | |||||
| 15 | Group 7 | NS | |||||
| 15 | Group 8 | ||||||
N indicates sample size; SD, standard deviation; S, significant; NS, not significant;
P< 0.05;
P<0.01
Group 5: Acid etching + direct illumination; Group 6: Acid etching + transillumination; Group 7: Self etching primer + direct illumination; Group 8: Self etching primer +transillumination.
DISCUSSION
Enamel decalcification during fixed orthodontic treatment is a major concern for clinicians. This process occurs rapidly and mineral loss has been reported even within a few months of treatment initiation [1,19]. The aim of the current study was to compare the amount of microleakage of an orthodontic adhesive following the use of two different methods of enamel conditioning and light curing.
In this study, we used bovine incisors as available substitutes for human incisors. Bovine deciduous lower incisors have nearly the size of permanent human maxillary central incisors, which are the most ideal for testing bonding properties since they provide flat bonding surfaces. These two types of teeth have been compared in a number of previous studies [15,20, 21]. The assumption that the contraction of photo-activated composite resins is directed toward the light source [13], and also the problem of not being able to directly cure the composite resin under metal brackets led to the idea of evaluating transillumination as a method of curing in this study. Behrents et al, also supported the use of this technique for bonding of lingual attachments due to its practical application in the oral environment [22]. In the current study, the group conditioned with self-etching primer showed less microleakage. One reason for less microleakage following the use of self-etching adhesive systems at margins cured directly could be the simultaneous penetration of etchant and monomer and the identical length of primer tags in the etched enamel.
In contrast to the conventional method of enamel conditioning, self-etching primers produce a uniform and more conservative etched pattern providing uniform adhesive penetration and less aggressive enamel demineralization [23]. In a study conducted by Vicente et al, on the effect of thermocycling on the microleakage beneath brackets bonded to bovine incisors, they found that microleakage increased significantly at the enamel-adhesive interface when using Transbond XT as the bonding agent [20]. In the current study, thermocycling was performed for all samples. This may explain the greater amount of microleakage at all margins in comparison with some other studies on this topic [7, 24]. In 2013, Sabzevari et al. demonstrated that thermocycling did not significantly increase the microleakage when a self-etching primer was used as a conditioner. However, comparison of different methods of bonding after thermocycling showed no significant differences between self-etching primers and the conventional method of conditioning [25].
Surface conditioning causes leakage of fluid and bacteria beneath the orthodontic brackets; thus, a deeper etching pattern with acid etchant cannot guarantee an interface free of microleakage [26]. This is also supported by an in vivo study by Feigal and Quelhas [27].
On the other hand, less penetrated resin tags in these systems may not resist the contracting forces of resin shrinkage [28]. However, this is acceptable in restorative dentistry when a bulk of composite is placed in a prepared cavity [29]. Orthodontic adhesive layers are very thin and the free, floating brackets are pulled closer to the enamel surface by the shrinkage [30]. The amount of microleakage reported in our study was lower than that in some previous studies [6,7]; this finding is in agreement with less microleakage reported for Transbond XT in an in vitro study by Sener et al [31].
Less microleakage at the margins of specimens in self-etching primer groups cured directly is similar to the results of a study by Uysal et al, which showed significantly higher scores at the gingival compared to the occlusal margins (where the tip of the light curing unit was positioned) [7].
Another factor that should be taken into account regarding the microleakage scores is a phenomenon called percolation. The linear coefficient of thermal expansion for enamel, metal brackets and the adhesive is not the same (α=12 for enamel, α=16 for stainless steel brackets and α=20–55 ppm/c for composite resin) [6]. These materials expand and contract at different rates when hot and cold foods are consumed; thus, the fluids are sucked in and pushed out at the margins of the brackets bonded to the teeth in both tooth-adhesive and adhesive-bracket interfaces. This can lead to microbial leakage at both interfaces [6].
The greater the light energy received by the composite, the greater the polymerization; therefore, transillumination must provide greater light energy than direct curing [32,33]. Since pulpal temperature should not exceed 5°–6° C, extending the exposure time should be done with caution. With 1 mm of dentine between the composite and the pulp, the temperature increases to 6°C with 40 seconds of continuous exposure [34]. In orthodontics, the enamel and dentine are thicker and provide greater pulpal insulation. Oesterle and Shellhart reported comparable bond strength in the group using transillumination for 50 seconds with the group cured for 40 seconds at the margins [16]. However, Heravi et al. concluded that 80 seconds of curing with high power mode of Blue Phase C8LED light curing unit with transillumination technique resulted in a clinically acceptable shear bond strength of brackets to posterior teeth with no risk of pulpal damage [18].
As reported by Yazici et al, and Haiduc et al, LED units cause significantly lower rise of pulp temperature in comparison with halogen light curing units [35,36]. In the current study, the amount of microleakage in the transillumination groups was comparable to that in the conventional curing groups at most of the margins of brackets except for the gingival margin. This may be due to the reflection of light from the bracket base as was pointed out by Oesterle and Shellhart [16].
Also, in 2013 Kumar et al. showed that even though the amount of light intensity lost in transillumination technique was significant, there were no differences in the shear bond strength of brackets bonded by transillumination technique or conventional method of curing at the mesial and distal margins [17].
In our study, only at the gingival margin of the samples, irrespective of the method of enamel conditioning, a significant amount of microleakage was observed. This may be explained by the gradual increase of buccolingual width from the incisal toward the gingival side. Consequently, although some studies reported adequate bond strength by transillumination, microleakage should be a concern especially in teeth with greater thickness.
As concluded by Heravi et al, to achieve an acceptable bracket bond strength to the posterior teeth, doubling the curing time from 40 to 80 seconds and increasing the light intensity to 800 mW/cm2 during the transillumination technique should be done [18].
In studies by Ramuglu et al, and Uysal et al, light was irradiated from the occlusal surface and a significant amount of microleakage was reported at the gingival margin. They reasoned that this result might be due to the degradation of light intensity and insufficient polymerization of composite [24,7]. Other studies in which the samples were cured according to the manufacturer’s instructions did not score the microleakage at the directly cured margins (mesial and distal margins) [32,33].
In our study, the manufacturers’ instructions were followed in all groups and evaluation of all margins showed that the amount of microleakage at the mesial and distal margins was lower than that at the incisal and gingival margins and these differences were statistically significant in groups which received self-etching primer for enamel conditioning. Polymerization starts in areas of resin closest to the light source. Even for metal brackets the best result will be gained if light is irradiated from all four sides of brackets. However, a well-designed study on this technique of curing may better elucidate this topic. It is impossible to extrapolate the results of an in vitro study to the actual oral environment; thus, future studies are necessary for further assessment of results.
CONCLUSION
Within the limitations of this study, use of self-etching primer and conventional light curing method caused less microleakage compared to the transillumination technique. Microleakage will be minimized if all margins of brackets are cured directly. The transillumination technique, irrespective of the method of enamel preparation, caused greater microleakage in both interfaces at the gingival margin and thus should not be used as the method of curing in orthodontic treatment.
REFERENCES
- 1-. Gorelick L, Geiger AM, Gwinnett AJ. Incidence of white spot formation after bonding and banding. Am J Orthod. 1982. February; 81 (2): 93– 8. [DOI] [PubMed] [Google Scholar]
- 2-. Geiger AM, Gorelick L, Gwinnett AJ, Benson BJ. Reducing white spot lesions in orthodontic populations with fluoride rinsing. Am J Orthod Dentofacial Orthop. 1992. May; 101 (5): 403– 7. [DOI] [PubMed] [Google Scholar]
- 3-. Frazier MC, Southard TE, Doster PM. Prevention of enamel demineralization during orthodontic treatment an in vitro study using pit and fissure sealants. Am J Orthod Dentofacial Orthop. 1996. November; 110 (5): 459– 65. [DOI] [PubMed] [Google Scholar]
- 4-. Millett DT, McCabe JF. Orthodontic bonding with glass ionomer cement: a review. Eur J Orthod. 1996. August; 18 (4): 385– 99. [DOI] [PubMed] [Google Scholar]
- 5-. Mattick CR, Mitchell L, Chadwick SM, Wright J. Fluoride-releasing elastomeric modules reduce decalcification a randomized controlled trial. J Orthod. 2001. September; 28 (3): 217– 9. [DOI] [PubMed] [Google Scholar]
- 6-. Arhun N, Arman A, Cehreli SB, Arikan S, Karabulut E, Gulsahi K. Microleakage beneath ceramic and metal brackets bonded with a conventional and an Antibacterial adhesive system. Angle Orthod. 2006. November; 76 (6): 1028– 34. [DOI] [PubMed] [Google Scholar]
- 7-. Uysal T, Ulker M, Ramoglu SI, Ertas H. Microleakage under metallic and ceramic brackets bonded with orthodontic Self-etching Primer Systems. Angle Orthod. 2008. November; 78 (6): 1089– 94. [DOI] [PubMed] [Google Scholar]
- 8-. Mizrahi E. Enamel demineralization following orthodontic treatment. Am J Orthod. 1982. July; 82 (1): 62– 7. [DOI] [PubMed] [Google Scholar]
- 9-. Nunn JH, Rugg-Gunn AJ, Ekanayake L, Saparamadu KD. Prevalence of developmental defects of enamel in areas with differing water fluoride levels and socioeconomic groups in Seri Lanka and England. Int Dent J. 1994. April; 44 (2): 165– 73. [PubMed] [Google Scholar]
- 10-. Greenlaw R, Way DC, Galil KA. An in vitro evaluation of a visible light-cured resin as an alternative to conventional resin bonding systems. Am J Orthod Dentofacial Orthop. 1989. September; 96 (3): 214– 20. [DOI] [PubMed] [Google Scholar]
- 11-. Peutzfeldt A, Asmussen E. Determinants of in vitro gap formation of resin composites. J Dent. 2004. February; 32 (2): 109– 15. [DOI] [PubMed] [Google Scholar]
- 12-. Davidson CL, de Gee AJ, Feilzer A. The competition between the composite-dentin bond strength and the polymerization contraction stress. J Dent Res. 1984. December; 63 (12): 1396– 9. [DOI] [PubMed] [Google Scholar]
- 13-. Lutz E, Krejci I, Oldenburg TR. Elimination of polymerization stresses at the margins of posterior composite resin restorations: A new restorative technique. Quintessence Int. 1986. December;17(12):777–84. [PubMed] [Google Scholar]
- 14-. Wendt SL, Jr, Convington JS. The use of light-cured composite resin to cement acid-etched fixed partial dentures. J Prosthet Dent. 1986. May; 55 (5): 578– 82. [DOI] [PubMed] [Google Scholar]
- 15-. King L, Smith RT, Wendt SL, Jr, Behrents RG. Bond strength of lingual orthodontic brackets bonded with light-cured composite resin cured by transillumination. Am J Orthod Dentofacial Orthop. 1987. April; 91 (4): 312– 5. [DOI] [PubMed] [Google Scholar]
- 16-. Oesterle LJ, Shellhart WC. Bracket bond strength with transillumination of a light-Activated orthodontic adhesive. Angle Orthod. 2001. August; 71 (4): 307– 11. [DOI] [PubMed] [Google Scholar]
- 17-. Kumar P, Nayak RS, Tan K, Mohan KA, Pasha A. Bracket bond strength with transillumination of a light activated orthodontic adhesive and the effect of time and tooth thickness on it: An in vitro study. J Ind Orthod Soc. 2013; 47 (3): 148– 153. [Google Scholar]
- 18-. Heravi F, Moazzami SM, Ghaffari N, Jalayer J, Bozorgnea Y. Evaluation of shear bond strength of orthodontic brackets using trans-illumination technique with different curing profiles of LED light-curing unit in posterior teeth. Prog Orthod. 2013. November 21; 14: 49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19-. O’Reilly MM, Featherstone JD. Demineralization and remineralization around orthodontic appliances: An in vivo study. Am J Orthod Dentofacial Orthop. 1987. July; 92 (1): 33– 40. [DOI] [PubMed] [Google Scholar]
- 20-. Vicente A, Ortiz AJ, Bravo LA. Microleakage beneath brackets bonded with flowable materials: effects of thermocycling. Eur J Orthod. 2009. August; 31 (4): 390– 6. [DOI] [PubMed] [Google Scholar]
- 21-. Canbek K, Karbach M, Gottschalk F, Erbe C, Wehrbein H. Evaluation of bovine and human teeth exposed to thermocycling for microleakage under bonded metal brackets. J Orofac Orthop. 2013. March; 74 (2): 102– 12. [DOI] [PubMed] [Google Scholar]
- 22-. Behrents RG, Wendt SL, Fox DM, Smith RT, King L. A Transillumination technique for lingual bonding. J Clin Orthod. 1987. May; 21 (5): 324– 5. [PubMed] [Google Scholar]
- 23-. Cal-Neto JP, Miguel JA. Scanning electron microscopy evaluation of the bonding mechanism of a self-etching primer on enamel. Angle Orthod. 2006. January; 76 (1): 132– 6. [DOI] [PubMed] [Google Scholar]
- 24-. Ramaglu SI, Uysal T, Ulker M, Ertas H. Microleakage under ceramic and metallic brackets bonded with resin-modified glass ionomer. Angle Orthod. 2009. January; 79 (1): 138– 43. [DOI] [PubMed] [Google Scholar]
- 25-. Sabzevari B, Ramazanzadeh BA, Moazzami SM, Sharifi A. Microleakage under orthodontic metal brackets bonded with three different bonding techniques with/without thermocycling. J Dent Mater Tech. 2013. Winter; 2 (1): 21– 8. [Google Scholar]
- 26-. Celiberti P, Lussi A. Use of a self-etching adhesive on previously etched intact enamel and its effect on sealant microleakage and tag formation. J Dent. 2005. February; 33 (2): 163– 71. [DOI] [PubMed] [Google Scholar]
- 27-. Feigal RJ, Quelhas I. Clinical trial of a self-etchings adhesive for sealant application: success at 24 months with Prompt L-pop. Am J Dent. 2003. August; 16 (4): 249– 51. [PubMed] [Google Scholar]
- 28-. Mandras RS, Retief DH, Russell CM. The effects of thermal and occlusal stresses on the microleakage of the Scotchbond 2 dentinal bonding system. Dent Mater. 1991. January; 7 (1): 63– 7. [DOI] [PubMed] [Google Scholar]
- 29-. James JW, Miller BH, English JD, Tadlock LP, Buschang PH. Effects of high-speed curing devices on shoar bond strength and microleakage of orthodontic brackets. Am J Orthod Dentofacial Orthop. 2003. May; 123(5):555–61. [DOI] [PubMed] [Google Scholar]
- 30-. Oesterle LJ, Newman SM, Shellhart WC. Rapid curing of bonding composite with a xenon plasma arc light. Am J Orthod Dentofacial Orthop. 2001. June;119(6): 610–6. [DOI] [PubMed] [Google Scholar]
- 31-. Sener Y, Uysal T, Basciftici FA, Demir A, Bost MS. Conventional and high-intensity halogen light effects on polymerization shrinkage of orthodontic adhesives. Angle Orthod. 2006. July; 76 (4): 677– 81. [DOI] [PubMed] [Google Scholar]
- 32-. Tavas MA, Watts DC. Bonding of orthodontic brackets by transillumination of a light activated composite: an invitro study. Br J Orthod. 1979. October; 6 (4): 207– 8. [DOI] [PubMed] [Google Scholar]
- 33-. Miyazaki M, Oshida Y, Moore BK, Onose H. Effect of light exposure on fracture toughness and flexural strength of light-cured composite. Dent Mater. 1996. November; 12 (6): 328– 32. [DOI] [PubMed] [Google Scholar]
- 34-. Hanning M, Bott B. In-vitro pulp chamber temperature rise during composite resine polymerization with various light-curing sources. Dent Mater. 1999. July; 15 (4): 275– 81. [DOI] [PubMed] [Google Scholar]
- 35-. Yazici AR, Muftu A, Kugel G, Perry RD. Comparison of temperature changes in the pulp chamber induced by various light curing units, in vitro. Oper Dent. 2006. Mar-Apr; 31 (2): 261– 5. [DOI] [PubMed] [Google Scholar]
- 36-. Haiduc C, Dodenciu D, Sinescu C, Negrutiu M, Draganescu G, Mara V. Pulp chamber temperature variations using three types of light curing units. Eur Cell Mater. 2007; 13 (Suppl 3): 19. [Google Scholar]