Abstract
Diabetes and hypertension are chronic conditions that are growing in prevalence as major causal factors for cardiovascular disease. The need for chronic illness surveillance, population risk management, and successful treatment interventions are critical to reduce the burden of future cardiovascular disease. In order to address these problems, it will require population risk stratification, task sharing and shifting, and community- as well as network -based care. Information technology tools also provide new opportunities for identifying those at risk and for implementing comprehensive approaches to achieving the goal of improved health locally, regionally, nationally and globally. This article discusses ongoing efforts at one university health center in the implementation of management strategies for diabetes and hypertension at the local, regional, national, and global levels.
Introduction
While cardiovascular disease mortality has significantly declined in western countries over the past several decades due to a combination of disease prevention and improved acute care, it remains the leading cause of death (1). Moreover, as developing countries successfully manage infectious diseases, the prevalence of chronic conditions such as diabetes mellitus and hypertension, are increasing and progressively pose major public health problems worldwide. Both diabetes and hypertension can be successfully treated with a variety of effective and relatively inexpensive therapies, yet control of these conditions remains far from ideal. Even in developed countries such as the United States, a substantial number of patients with diabetes and hypertension do not reach their targeted hemoglobin A1c levels or blood pressure goals (2,3). Effective approaches to address substantial cardiovascular health needs and health disparities must go beyond traditional specialty-oriented cardiovascular care. Thus, the need for population disease surveillance, risk management, and durable treatment intervention are critical to reduce the burden of future cardiovascular disease across communities. In order to successfully alter the impact of diabetes and hypertension, it will require concepts typically applied for global health including: population risk stratification, task sharing and shifting, community- and network -based care, and successful application of information technology tools. In this article, we will highlight ongoing efforts involving Duke University in the implementation of management strategies for diabetes and hypertension at local, regional, national, and global levels.
I. Local Perspectives
The Southeastern region of the US has particularly poor outcomes in terms of longevity and functional status. Excessive rates of obesity, diabetes and hypertension are coupled with high rates of stroke, heart failure, renal failure and sudden death. North Carolina is located in a region commonly referred to as the “stroke belt” or the “diabetes belt,” terms coined to reflect particularly high prevalence of these conditions and their risk factors. Durham County, the home of Duke University and its academic health and science system, has rates of death and nonfatal cardiovascular events that are only slightly better than the North Carolina average. The counties surrounding Durham County are heterogeneous with lower than average rates of adverse outcomes in affluent counties, but very high rates in poorer rural counties. There are also substantial disparities in health based on sex, race and ethnicity (4).
Adoption of electronic health records (EHRs) provides a unique opportunity to conduct population health surveillance and management. Over a decade ago, campus collaborations between the Duke University School of the Environment and the Duke University Health System facilitated the conceptualization of a data environment in which every individual receiving care in the Health System and living in the local community could be characterized in multiple dimensions, including the dimensions of social, economic and environmental contributors to health (5). Whole neighborhoods and populations can be characterized by summing and integrating the individual level information.
In 2006 when Duke received one of the original Clinical and Translational Science Awards (CTSAs), a large community engagement program was initiated and given the title Durham Health Innovations (DHI), supported by grant funds and institutional support. We developed a plan for community based health improvement by asking teams to form with a focus on a health problem of importance. Teams were intentionally comprised of both Duke and community members. A consortium of 10 teams evolved to address health issues across the lifespan. Each team developed as set of core priorities for action, evolving around several central themes including: (1) developing a single medical record for the county, (2) locating care as close as possible to home, work or school and (3) tailoring care to match the needs of every individual. Teams spent considerable time considering incentives driving contemporary health care practices, and saw the use of electronic information as a promising vehicle for unifying the traditional healthcare delivery system and social forces to achieve better population health. In addition, teams viewed the use of electronic information as a critically important means to reduce redundant, erroneous, and unnecessary care as well as to prevent expensive hospitalizations precipitated by uncoordinated care.
A grant from the Bristol Myers Squibb Foundation (BMS-F) enabled taking the concepts started by DHI to address diabetes care at the neighborhood and population levels. The plan has included identifying each patient with diabetes in Durham County, characterizing the individual's risk of poor medical outcomes and high financial cost and developing an intervention plan to match the level of risk (Figure 1). A robust effort to identify all people in the Health System and County with Type II diabetes using the Health System enterprise data warehouse “computable phenotypes” demonstrated that the estimate of the proportion of a population with Type II Diabetes could vary by up to twofold, depending on the specific algorithm used from a suite of commonly used “computable phenotype” definitions (6).
Figure 1. Spatial pattern of diabetic patients in Durham County, NC.
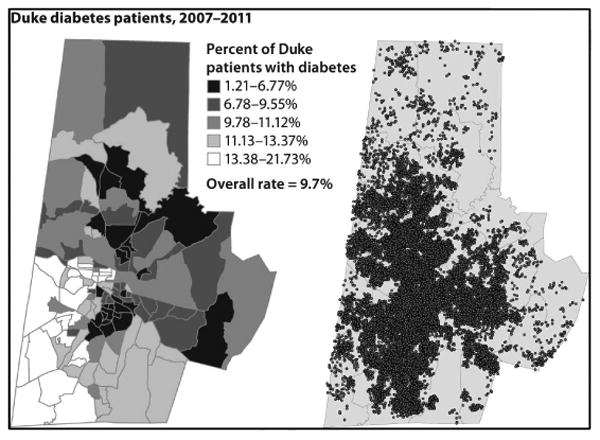
Using the composite of medical information in the electronic health record and geospatially mapped information about homes and neighborhoods, each patient is assigned a score reflecting their risk of developing a poor health outcome (e.g., unnecessary hospitalization). For high-risk patients, a tailored, individualized care plan is developed by a multidisciplinary team, including a physician, nurse practitioner, social worker and dietician. Patients at moderate risk are targeted through care delivery quality improvement in medical practices and clinics throughout the county. Low risk patients benefit from a broad set of neighborhood and public health interventions (e.g., health fairs) aimed at improving awareness, facilitation of exercise, and appropriate diet behaviors.
A critical element of the BMS-F project is the development of community-engaged plans to improve neighborhood health with a focus on high-risk neighborhoods. Using geospatial mapping, areas with high prevalence of high-risk individuals have been located. Relationships have been developed with community leaders and grass-roots organizations, and a specific plan has been developed for each neighborhood. The overall goal is to develop an environment that is conducive to successful diabetes self-management. Interventions are underway for the more than 22,900 people with Type II Diabetes living in Durham County and include neighborhood activities to mobilize resources addressing environmental (e.g., areas for exercise), social (e.g., resources for education and support for medication adherence), and healthcare (e.g., improving transportation to local health care services) determinants of diabetes outcomes.
In order to further address the problems of diabetes and hypertension, it is important to examine all of the modifiable factors. For example, suboptimal risk factor control can be attributed to multiple inter-related patient, provider, and system failures. Some of these factors include inefficiencies in the traditional clinician-patient interaction, provider inertia, misaligned incentives for disease management, and a failure to successfully engage patients in their health management (7). As part of our ongoing efforts to implement best practices, we frequently evaluate clinician-specific performance in our local community and then provide feedback aiming to change behavior. Unfortunately, we have discovered that often feedback alone as an intervention has limited impact on blood pressure control rates, although it does prompt greater provider attention to blood pressure measurements (8).
As a part of our ongoing innovations in the care of chronic diseases such as hypertension, we have advocated for a number of transformative strategies for using technology to support care interventions. For example, we have partnered with the American Heart Association to develop an online web-based patient care platform known as Heart360 to support patient engagement and telemedicine interventions for hypertension. This system allows patients to record heart health data including blood pressure information and share these data with their providers to both promote patient engagement and self-management and stimulate more timely treatment intensification (9).
Another recommendation has been the use of collaborative health care teams to augment risk factor control; in part this helps to reduce clinical inertia but also leverages community health works to raise awareness, and maximize contact points with at-risk patients (10). Health literacy interventions have also been studied to improve medication adherence (11). A randomized trial of tailored case management for diabetes and hypertension management is ongoing in Duke community clinics that combine multiple approaches to improve patient health (12).
II. Regional Perspectives
Additional funding through The Centers for Medicare and Medicaid Services demonstration program provided an opportunity to extend initial BMS-F initiatives to a total of four Southeastern US counties, including Durham, and Cabarrus/Kannapolis Counties in North Carolina as well as Mingo County, West Virginia, and Quitman County, Mssissippi. Through this expanded program, we have developed a multi-county consortium, the Southeastern Diabetes Initiative, which employs similar principles to leverage electronic health data as a means for informing the deployment of tailored services to match population health needs on a county-wide basis.
Through the use of aggregated EHR data for population health risk assessment and management, we have identified large gaps in quality of care and redundancy in procedure and technology use. Patients often receive expensive cardiovascular procedures in large urban hospitals, but then they are sent back to under-served environments where follow-up care may be inadequate. There are many opportunities to improve the health of underserved rural Southeastern populations through improved integration of health care delivery across geographic regions, including the mobilization of health care services closer to patients' communities (e.g., through use of better information to organize health care services by multidisciplinary health professionals and community health workers).
Resource investment to improve the health of Kannapolis and Cabarrus County, NC residents, one of the four counties engaged as part of the Southeastern Diabetes Initiative, has further extended the reach of efforts to improve regional population health. In 2005 philanthropist David H. Murdock announced the formation of the North Carolina Research Campus. As part of this initiative, he funded the MURDOCK Study, a large, molecular epidemiology study oriented towards the definition of health and disease focused on nutrition and exercise. The study now has over 11,000 participants, and it is built on the principles of broad community inclusion and engagement. This study provides an opportunity to not only measure deep phenotypes of health and disease in a Southeastern community, but also to measure the impact of local patient, community, and health system interventions.
Thus, we have developed regional programs engaging community-health system partnerships, leveraging EHR data, and using principles of geospatial science to identify health improvement priorities and guide resource utilization for population health management. We have also developed strategies to deploy tailored interventions that directly respond to specific individual and community health needs. Through funded projects, we have demonstrated the feasibility of implementing these approaches across broad geographic regions, including in communities with limited resources. In addition to demonstrating generalizability of our approach, programs have spurred more detailed large community-based epidemiological studies on health. Application of similar models holds great promise to improve health across other US geographical regions.
III. National Perspectives
According to recent estimates, the United States ranks poorly (30th to 70th overall) in health and health care delivery compared with most other economically developed countries (13-15). In the United States between 1976- 1980 and 2007-2010, the prevalence of diabetes increased from 4.7% to 11.2% in men and from 5.7% to 8.7% in women (16). Among patients with cardiovascular disease, the increasing prevalence of diabetes will lead to a large population with additional difficulties for preventing secondary cardiovascular events (17). In a recent survey of ACTION Registry-Get With The Guidelines (GWTG), an ongoing voluntary acute myocardial infarction quality improvement registry now involving more than 1000 US hospitals, it was observed that 30% of acute myocardial infarction patients had diabetes on admission, and another 15% of non-diabetics had measured hemoglobin A1c levels >6.5% potentially meeting criteria for newly- diagnosed diabetes (18). As this population grows it will be critically important to address ongoing questions on best therapies for management of diabetes that will not only lead to improved glycemic control, but also improved cardiovascular outcomes.
Similarly, hypertension is a growing problem in the United States with a large population at risk for cardiovascular disease. In an analysis of the National Health and Nutrition Examination Survey (NHANES) the prevalence of uncontrolled hypertensive patients (those requiring 3 or more medications) has increased from 16% in 1998-2004 to 28% in 2005-2008 (19). In 2014, the Guidelines for the Management of High Blood Pressure (JNC 8) were released (20). Panel members agreed that there was strong evidence to support treating hypertensive persons aged 60 years or older to a BP goal of less than 150/90 mm Hg, and recommended a BP of less than 140/90 mm Hg for hypertensive patients either 30-59 years of age, those with chronic kidney disease, and those with diabetes based on expert opinion. We recently re-examined NHANES data to assess the proportion of US adults potentially affected by the recent changes in recommendations for hypertension management. Extrapolating from these data, approximately 5.8 million US adults previously classified as needing hypertension therapy are now reclassified as no longer needing it. However, the number of adults above blood pressure goals remains high, despite guideline recommendation changes, involving an estimated 28 million adults (10% of adults 18-59 years and 21% of adults over age 60) (2). Data from the INVEST study demonstrated that In hypertensive patients with coronary artery disease who are >60 years of age, achieving a BP target of 140 to <150 mm Hg as recommended by the JNC-8 panel is associated with adverse cardiovascular outcomes compared with those who are at the previously recommended target of <140 mm Hg (21). Indeed, the minority viewpoint from some of the members appointed to the JNC 8 expert panel was that evidence was insufficient to increase the SBP goal from its previous level of less than 140 mm Hg because of concern that increasing the goal may cause harm by increasing the risk for cardiovascular disease and partially undoing the remarkable progress in reducing cardiovascular mortality in Americans older than 60 years (22). In the future, it will be critical to assess how best to manage this population and prospectively determine whether changes in guideline recommendations alter outcomes adversely.
While recognition of the large populations with diabetes or hypertension is a step towards prevention, it is critical to continuously assess how these patients are managed and evaluate areas for improvement. The Duke Clinical Research Institute has a longstanding history of quality improvement through national registries partnered with professional societies such as the American Heart Association, American Diabetes Association, and the American College of Cardiology. These efforts largely focus on the highest risk populations that will provide the largest gains for population health. Examples of these efforts include the ACTION Registry, AHA's GWTG registry, and Guideline Advantage Registry (23-25).
To address potential areas for quality improvement, we have consistently demonstrated persistent gaps in care in contemporary national practice across the spectrum of cardiovascular care. In the CRUSADE registry, we observed that acute myocardial infarction patients with insulin-dependent diabetes are less likely to receive key secondary prevention therapies such as heparin and beta-blockers, and are also less likely to undergo an early invasive treatment strategy compared with non-diabetic patients (26). Among patients with acute ischemic stroke in the GWTG-Stroke program, diabetic patients are significantly less likely to receive timely fibrinolytic therapy compared with non-diabetics (27). As efforts have grown substantially towards population management strategies, we have partnered with the American Heart Association and American Diabetes Association to examine almost 150,000 outpatients in the Guidelines Advantage registry focused on harvesting electronic medical records in the ambulatory practice setting. In this registry, the proportion of patients having optimal blood pressure control ranged from 50 to 75% across practices; a lower likelihood of blood pressure control was observed particularly among racial minority groups (28). While patients with diabetes are at substantially higher risk of cardiovascular morbidity and mortality, this adverse association is compounded by a relative underuse of evidence-based medicine in this patient population. More importantly, this registry serves as a platform to continually assess progress toward national goals such as promoted by the Million Hearts initiative (29).
As efforts for population surveillance focused on key risk factors of diabetes and hypertension grow, national registries provide an effective platform for extending our ability to accelerate new evidence into practice. Registries also allow for careful monitoring of any unexpected safety issues as a new therapy diffuses into a population that was under-represented in clinical trials. Increasingly, there are great efforts to implement new therapies due to the prior reports showing a lag of greater than 10 years before implementation of best evidence (30). While speeding the delivery of best evidence into practice is a worthy and necessary goal, the potential risk is having large populations from the ‘real-world’ that were not included in clinical trials. To address this dual need of implementing emerging evidence more quickly while surveying for potential unexpected adverse outcomes in these unique populations, national registries linked to Medicare claims offer a promising solution. In multiple studies, our group has used national cardiovascular registries to examine the comparative effectiveness and safety of therapies in understudied populations such as older patients or patients with multiple comorbidities including diabetes and hypertension (31). As access improves to more ‘real-time’ data such as the Medicare Data Enclave, the power to simultaneously assess diffusion of new therapies using registries and survey longitudinal outcomes becomes an important element for delivering high quality care in an expedient, effective and safe fashion.
IV. Global Perspectives
Duke University has a number of global health initiatives and our major efforts in diabetes and hypertension are centered in China and Kenya. Both efforts received funding from the National Heart Lung and Blood Institute in response to a solicitation to create Centers of Excellence (COE) in non-communicable disease research in low- and middle-income countries (32). Duke University was awarded a COE in partnership with The George Institute in China and an additional COE with Moi University in Kenya. The COEs are distinctive in two main ways: 1) they undertake research into approaches to prevent or treat chronic disease alongside developing clinical research infrastructure and research training programs; 2) they have become a new global research network for non-communicable diseases based in low- and middle-income countries (33),
The China COE is focused on hypertension, which is the single most important determinant of cardiovascular disease in China (34); its importance is greatest in rural and northern regions where salt consumption and the incidence of stroke are both very high. It has been estimated that each 2 percent rise in population blood pressure levels in China results in an additional 500,000 strokes and other major cardiovascular events each year (35). The COE is currently in the analysis phase of a large-scale cluster randomized controlled study in five provinces and 120 villages. Sixty intervention villages received general health education advising reduced salt risk, specific health education targeting reduced salt intake in patients with a high risk of cardiovascular disease, and a food supply strategy designed to promote the sale of a reduced sodium added potassium salt substitute through village convenience stores. Sixty control villages received no intervention and continued their usual practices. The 24 hr urine sodium, blood pressure, 24 hr urine potassium, and urine sodium: potassium ratio are being analyzed in 2400 patients in intervention and control villages (36).
The Kenya COE exemplifies another major global health effort in chronic cardiovascular disease management. It is especially notable for its multi-disciplinary, multi-university approach to achieving the tripartite academic mission. Moi University, located in western Kenya (Figure 2), has a >25 year relationship with over a dozen North American medical schools led by Indiana University (37). This collaboration – Academic Model Providing Access to Healthcare (AMPATH) – has the goal to leverage the power of the academic foundation to support service, teaching and research. In keeping with the AMPATH model, Duke University took a lead role in achieving the missions as they relate to cardiovascular diseases (38). The COE in cardiovascular and pulmonary disease leverages the administrative, healthcare, research, and personnel infrastructure already in place through the HIV program and enabled the team to avoid “reinventing the wheel” for diseases such as hypertension and diabetes (39).
Figure 2. Map of the Academic Model Providing Access to Healthcare Catchment Area and Clinic Locations in Western Kenya.

Owing to the evidence gaps regarding chronic cardiovascular diseases in Kenya, the research program of the COE encompasses a variety of methodological approaches including surveillance, epidemiology, trials and implementation science. While the eventual goal was to tackle primary prevention and care for hypertension, diabetes and other non-communicable diseases, there were important knowledge gaps to address. This included observational descriptions of these diseases in western Kenya as there was evidence that determinants of hypertension and diabetes might be sufficiently different from those in high-income countries. In addition, the magnitude of need for clinical cardiovascular expertise required directing efforts towards building facilities, training healthcare personnel, and working with partner institutions and industry to procure necessary equipment to deliver appropriate cardiovascular care alongside research, training, and education. The attention to improving cardiovascular clinical care infrastructure and services is in some ways unique among the COEs and these efforts have largely been supported by philanthropy via the Hubert-Yeargan Center for Global Health at Duke University (40).
Epidemiologic surveillance systems for cardiovascular disease are poor in low-and middle-income countries (LMICs) like Kenya owing to the low rate of cardiovascular research and productivity (41). The initial thrust of the research endeavor in the Kenya COE has therefore been focused on gathering basic information on the nature and degree of cardiovascular and pulmonary diseases in the region. As hypertension is one of the most common cardiovascular risk factors in sub-Saharan Africa and treatment rates are suboptimal, the next phase of research has focused on identifying the context –specific risk factors and treatment approaches for hypertension (42-44). Delivering context-specific interventions for hypertension in western Kenya has required an accurate description of the burden and severity of disease as most estimates for Kenya are based on extrapolation. The COE's research program has resulted in knowledge regarding the appropriate screening strategies and the burden of hypertension and target organ damage in rural and peri-urban settings in western Kenya (45, 46).
Heart failure, often secondary to hypertension, is one of the most common admission diagnoses in western Kenya (47). In addition to describing the etiologies of heart failure in western Kenya for the first time using contemporary echocardiography, the team also piloted a training method for non-physician healthcare workers to employ handheld echocardiography in remote settings to diagnose the most common cardiac disorders in the region. Relocating echocardiographic services to rural settings in LMICs offers the opportunity for early diagnosis and avoids unnecessary late presentations of advanced disease. In a similar vein, the COE is involved in closing the “know-do gap” in the areas of hypertension and cardiovascular diseases (48).
The foundation of the COE has also fostered productive partnerships, which leverage the perspectives and unique strengths of many institutions. Hypertension and mobile communication technology in the health arena (mHealth) characterize the current focus of these efforts owing to the burden of disease and the untapped and yet unproven potential of mHealth for non-communicable diseases in sub-Saharan Africa (49). By virtue of a project lead by the Icahn School of Medicine at Mount Sinai University, the chronic disease management program at Moi University has embarked on a program to optimize linkage and retention to hypertension care in rural Kenya (50). This program will test the hypothesis that community health workers armed with a tailored behavioral communication strategy and a smart-phone based tool linked to an electronic health record can increase linkage and retention of hypertensive individuals to a care program and ultimately reduce blood pressure among these individuals. In addition to community health workers, investigators are also exploring a task-sharing approach to hypertension treatment with nurse-lead interventions employing mHealth (51). These results of these activities have the potential to impact how evidence-based care is delivered to individuals with chronic non-communicable diseases in rural settings in sub-Saharan Africa and globally.
Conclusion
Diabetes and hypertension are growing chronic health problems that are major contributors to cardiovascular disease. At an academic medical center, we have made substantial efforts at the local, regional, national, and global levels to implement improved care for these diseases through research and education in order to reduce the burden of cardiovascular disease in our patients and their communities. Partnerships with other medical centers, government, and industry have been successful in combination with technologies such as geospatial mapping, electronic health records, and mobile communication tools. In the future, integration of these efforts may contribute towards the translation of improved health in local and global health settings.
Acknowledgments
Supported by a grant from the National Center for Advancing Translational Sciences of the National Institutes of Health under award number UL1TR001117.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Global status report on noncommunicable diseases 2010. Geneva: World Health Organization; 2011. [Google Scholar]
- 2.Navar-Boggan AM, Pencina MJ, Williams K, Sniderman AD, Peterson ED. Proportion of US adults potentially affected by the 2014 hypertension guideline. JAMA. 2014 Apr 9;311(14):1424–9. doi: 10.1001/jama.2014.2531. [DOI] [PubMed] [Google Scholar]
- 3.Decker SL, Kostova D, Kenney GM, Long SK. Health status, risk factors, and medical conditions among persons enrolled in Medicaid vs uninsured low-income adults potentially eligible for Medicaid under the Affordable Care Act. JAMA. 2013 Jun 26;309(24):2579–86. doi: 10.1001/jama.2013.7106. [DOI] [PubMed] [Google Scholar]
- 4.Murray CJL, Kulkarni SC, Michaud C, Tomijima N, Bulzacchelli MT, et al. Eight Americas: Investigating Mortality Disparities across Races, Counties, and Race-Counties in the United States. PLoS Med. 2006;3(9):e260. doi: 10.1371/journal.pmed.0030260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Miranda ML, Ferranti J, Strauss B, Neelon B, Califf RM. Geographic health information systems: a platform to support the ‘triple aim’. Health Aff (Millwood) 2013 Sep;32(9):1608–15. doi: 10.1377/hlthaff.2012.1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Richesson RL, Rusincovitch SA, Wixted D, Batch BC, Feinglos MN, Miranda ML, Hammond WE, Califf RM, Spratt SE. A comparison of phenotype definitions for diabetes mellitus. J Am Med Inform Assoc. 2013 Dec;20(e2):e319–26. doi: 10.1136/amiajnl-2013-001952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Roark RF, Shah BR, Udayakumar K, Peterson ED. The need for transformative innovation in hypertension management. Am Heart J. 2011 Sep;162(3):405–11. doi: 10.1016/j.ahj.2011.06.010. [DOI] [PubMed] [Google Scholar]
- 8.Navar-Boggan AM, Fanaroff A, Swaminathan A, Belasco A, Stafford J, Shah B, Peterson ED. The impact of a measurement and feedback intervention on blood pressure control in ambulatory cardiology practice. Am Heart J. 2014 Apr;167(4):466–71. doi: 10.1016/j.ahj.2013.12.015. [DOI] [PubMed] [Google Scholar]
- 9.Shah BR, Thomas KL, Elliot-Bynum S, Thomas K, Damon K, Allen LaPointe N, Calhoun SA, Thomas L, Mathews R, Califf RM, Peterson ED. Check it, change it: a community-based intervention to improve blood pressure control. Circ Cardiovasc Qual Outcomes. 2013 Nov;6(6):741–8. doi: 10.1161/CIRCOUTCOMES.113.000148. [DOI] [PubMed] [Google Scholar]
- 10.Bosworth HB, Powers BJ, Oddone EZ. Patient self-management support: novel strategies in hypertension and heart disease. Cardiol Clin. 2010 Nov;28(4):655–63. doi: 10.1016/j.ccl.2010.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zullig LL, Sanders LL, Shaw RJ, McCant F, Danus S, Bosworth HB. A randomised controlled trial of providing personalised cardiovascular risk information to modify health behavior. J Telemed Telecare. 2014 Apr;20(3):147–52. doi: 10.1177/1357633X14528446. [DOI] [PubMed] [Google Scholar]
- 12.Crowley MJ, Bosworth HB, Coffman CJ, Lindquist JH, Neary AM, Harris AC, Datta SK, Granger BB, Pereira K, Dolor RJ, Edelman D. Tailored Case Management for Diabetes and Hypertension (TEACH-DM) in a community population: study design and baseline sample characteristics. Contemp Clin Trials. 2013 Sep;36(1):298–306. doi: 10.1016/j.cct.2013.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Available at: http://www.skollfoundation.org/economic-growth-does-not-automatically-lead-to-social-advancement-new-social-progress-index/
- 14.National Research Council, Institute of Medicine. US Health in International Perspective: Shorter Lives, Poorer Health. Panel on Understanding Cross-National Health Differences Among High-Income Countries. In: Woolf Steven H, Aron Laudan., editors. Committee on Population, Division of Behavioral and Social Sciences and Education, and Board on Population Health and Public Health Practice, Institute of Medicine. Washington, D.C: National Academies Press; 2013. [PubMed] [Google Scholar]
- 15.US Burden of Disease Collaborators. The state of US health, 1990-2010: burden of diseases, injuries, and risk factors. JAMA. 2013 Aug 14;310(6):591–608. doi: 10.1001/jama.2013.13805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Menke A, Rust KF, Fradkin J, Cheng YJ, Cowie CC. Associations Between Trends In Race/Ethnicity, Aging, and Body Mass Index With Diabetes Prevalence in the United States: A Series of Cross-sectional Studies. Ann Intern Med. 2014 Sep 2;161(5):328–35. doi: 10.7326/M14-0286. [DOI] [PubMed] [Google Scholar]
- 17.Gore MO, Patel MJ, Kosiborod M, Parsons LS, Khera A, de Lemos JA, Rogers WJ, Peterson ED, Canto JC, McGuire DK, National Registry of Myocardial Infarction Investigators Diabetes mellitus and trends in hospital survival after myocardial infarction, 1994 to 2006: data from the national registry of myocardial infarction. Circ Cardiovasc Qual Outcomes. 2012 Nov;5(6):791–7. doi: 10.1161/CIRCOUTCOMES.112.965491. [DOI] [PubMed] [Google Scholar]
- 18.Rousan TA, Pappy RM, Chen AY, Roe MT, Saucedo JF. Impact of Diabetes Mellitus on Clinical Characteristics, Management, and In-hospital Outcomes in Patients With Acute Myocardial Infarction (from the NCDR) Am J Cardiol. 2014 Jul 30; doi: 10.1016/j.amjcard.2014.07.031. [DOI] [PubMed] [Google Scholar]
- 19.Egan BM, Zhao Y, Axon RN, Brzezinski WA, Ferdinand KC. Uncontrolled and apparent treatment resistant hypertension in the United States, 1988 to 2008. Circulation. 2011 Aug 30;124(9):1046–58. doi: 10.1161/CIRCULATIONAHA.111.030189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, Lackland DT, LeFevre ML, MacKenzie TD, Ogedegbe O, Smith SC, Jr, Svetkey LP, Taler SJ, Townsend RR, Wright JT, Jr, Narva AS, Ortiz E. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8) JAMA. 2014 Feb 5;311(5):507–20. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 21.Bangalore S, Gong Y, Cooper-DeHoff RM, Pepine CJ, Messerli FH. 2014 Eighth Joint National Committee Panel Recommendation for Blood Pressure Targets Revisited: Results From the INVEST Study. J Am Coll Cardiol. 2014 Aug 26;64(8):784–93. doi: 10.1016/j.jacc.2014.05.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wright JT, Jr, Fine LJ, Lackland DT, Ogedegbe G, Dennison Himmelfarb CR. Evidence supporting a systolic blood pressure goal of less than 150 mm Hg in patients aged 60 years or older: the minority view. Ann Intern Med. 2014 Apr 1;160(7):499–503. doi: 10.7326/M13-2981. [DOI] [PubMed] [Google Scholar]
- 23.Available at: https://www.ncdr.com/webncdr/action/
- 24.Available at: http://www.heart.org/HEARTORG/HealthcareResearch/GetWithTheGuidelines/Get-With-The-Guidelines---HFStroke_UCM_001099_SubHomePage.isp
- 25.Available at: http://www.guidelineadvantage.org/TGA
- 26.Brogan GX, Jr, Peterson ED, Mulgund J, Bhatt DL, Ohman EM, Gibler WB, Pollack CV, Jr, Farkouh ME, Roe MT. Treatment disparities in the care of patients with and without diabetes presenting with non-ST-segment elevation acute coronary syndromes. Diabetes Care. 2006 Jan;29(1):9–14. [PubMed] [Google Scholar]
- 27.Reeves MJ, Vaidya RS, Fonarow GC, Liang L, Smith EE, Matulonis R, Olson DM, Schwamm LH. Get With The Guidelines Steering Committee and Hospitals. Quality of care and outcomes in patients with diabetes hospitalized with ischemic stroke: findings from Get With the Guidelines-Stroke. Stroke. 2010 May;41(5):e409–17. doi: 10.1161/STROKEAHA.109.572693. [DOI] [PubMed] [Google Scholar]
- 28.Eapen ZJ, Liang L, Shubrook JH, Bauman MA, Bufalino VJ, Bhatt DL, Peterson ED, Hernandez AF. Current quality of cardiovascular prevention for Million Hearts: An analysis of 147,038 outpatients from The Guideline Advantage. Am Heart J. 2014 Sep;168(3):398–404. doi: 10.1016/j.ahj.2014.06.007. [DOI] [PubMed] [Google Scholar]
- 29.Available at: http://www.millionhearts.hhs.gov/index.html
- 30.Crossing the Quality Chasm, A New Health System for the 21st Century Committee on Quality of Health Care in America Institute of Medicine. National Academy Press; Washington, D.C: 2006. [Google Scholar]
- 31.Curtis LH, Mi X, Quails LG, Hammill BG, Hammill SC, Heidenreich PA, Masoudi FA, Setoguchi S, Hernandez AF, Fonarow GC. Design and rationale of a retrospective clinical effectiveness study of aldosterone antagonist therapy in patients with heart failure. Am Heart J. 2012 Jun;163(6):946–953.el. doi: 10.1016/j.ahj.2012.03.007. [DOI] [PubMed] [Google Scholar]
- 32.Nabel EG, Stevens S, Smith R. Combating chronic disease in developing countries. Lancet. 2009 Jun 13;373(9680):2004–6. doi: 10.1016/S0140-6736(09)61074-6. [DOI] [PubMed] [Google Scholar]
- 33.UnitedHealth Group/National Heart, Lung, and Blood Institute Centres of Excellence. A global research network for non-communicable diseases. Lancet. 2014 Apr 26;383(9927):1446–7. doi: 10.1016/S0140-6736(13)61808-5. [DOI] [PubMed] [Google Scholar]
- 34.Moran A, Gu D, Zhao D, Coxson P, Wang YC, Chen CS, Liu J, Cheng J, Bibbins-Domingo K, Shen YM, He J, Goldman L. Future Cardiovascular Disease in China Markov Model and Risk Factor Scenario Projections From the Coronary Heart Disease Policy Model-China. Circulation: Cardiovascular Quality and Outcomes. 2010:243–252. doi: 10.1161/CIRCOUTCOMES.109.910711. 3.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Available at: http://www.nhlbi.nih.gov/about/org/globalhealth/centers/china-center-of-excellence.htm
- 36.Available at: http://my.americanheart.org/idc/groups/ahamahpublic/@wcm/@sop/@scon/documents/downloadable/ucm_458224.pdf
- 37.Einterz RM, Kimaiyo S, Mengech HN, Khwa-Otsyula BO, Esamai F, Quigley F, Mamlin JJ. Responding to the FflV pandemic: the power of an academic medical partnership. Acad Med. 2007 Aug;82(8):812–8. doi: 10.1097/ACM.0b013e3180cc29f1. [DOI] [PubMed] [Google Scholar]
- 38.Available at: http://www.ampathkenya.org/our-programs/primary-care-chronic-diseases/cardiovascular-and-pulmonary-disease/
- 39.Rabkin M, El-Sadr WM. Why reinvent the wheel? Leveraging the lessons of FflV scale-up to confront non-communicable diseases. Glob Public Health. 2011;6(3):247–56. doi: 10.1080/17441692.2011.552068. [DOI] [PubMed] [Google Scholar]
- 40.Available at: http://dukeglobalhealth.org/
- 41.Huffman MD, Baldridge A, Bloomfield GS, Colantonio LD, Prabhakaran P, Ajay VS, Suh S, Lewison G, Prabhakaran D. Global cardiovascular research output, citations, and collaborations: a time-trend, bibliometric analysis (1999-2008) PLoS One. 2013 Dec 31;8(12):e83440. doi: 10.1371/journal.pone.0083440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mathenge W, Foster A, Kuper H. Urbanization, ethnicity and cardiovascular risk in a population in transition in Nakuru, Kenya: a population-based survey. BMC Public Health. 2010 Sep 22;10:569. doi: 10.1186/1471-2458-10-569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.de Ramirez SS, Enquobahrie DA, Nyadzi G, Mjungu D, Magombo F, Ramirez M, Sachs SE, Willett W. Prevalence and correlates of hypertension: a cross-sectional study among rural populations in sub-Saharan Africa. J Hum Hypertens. 2010 Dec;24(12):786–95. doi: 10.1038/jhh.2010.14. [DOI] [PubMed] [Google Scholar]
- 44.Pereira M, Lunet N, Azevedo A, Barros H. Differences in prevalence, awareness, treatment and control of hypertension between developing and developed countries. J Hypertens. 2009 May;27(5):963–75. doi: 10.1097/hjh.0b013e3283282f65. [DOI] [PubMed] [Google Scholar]
- 45.Bloomfield GS, Mwangi A, Chege P, Simiyu CJ, Aswa DF, Odhiambo D, Obala AA, Ayuo P, Khwa-Otsyula BO. Multiple cardiovascular risk factors in Kenya: evidence from a health and demographic surveillance system using the WHO STEPwise approach to chronic disease risk factor surveillance. Heart. 2013 Sep;99(18):1323–9. doi: 10.1136/heartjnl-2013-303913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pastakia SD, Ali SM, Kamano JH, Akwanalo CO, Ndege SK, Buckwalter VL, Vedanthan R, Bloomfield GS. Screening for diabetes and hypertension in a rural low income setting in western Kenya utilizing home-based and community-based strategies. Global Health. 2013 May 16;9:21. doi: 10.1186/1744-8603-9-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Stone GS, Tarus T, Shikanga M, Biwott B, Ngetich T, Andale T, Cheriro B, Aruasa W. The association between insurance status and in-hospital mortality on the public medical wards of a Kenyan referral hospital. Glob Health Action. 2014 Feb 11;7:23137. doi: 10.3402/gha.v7.23137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bloomfield, et al. HIV and Noncommunicable Cardiovascular and Pulmonary Diseases in Low- and Middle-Income Countries in the ART Era: What We Know and Best Directions for Future Research. J Acquir Immune Defic Syndr. 2014;67(Suppl 1):S40–53. doi: 10.1097/QAI.0000000000000257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bloomfield GS, Vedanthan R, Vasudevan L, Kithei A, Were M, Velazquez EJ. Mobile health for non-communicable diseases in Sub-Saharan Africa: a systematic review of the literature and strategic framework for research. Global Health. 2014 Jun 13;10:49. doi: 10.1186/1744-8603-10-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Vedanthan R, Kamano JH, Naanyu V, Delong AK, Were MC, Finkelstein EA, Menya D, Akwanalo CO, Bloomfield GS, Binanay CA, Velazquez EJ, Hogan JW, Horowitz CR, Inui TS, Kimaiyo S, Fuster V. Optimizing linkage and retention to hypertension care in rural Kenya (LARK hypertension study): study protocol for a randomized controlled trial. Trials. 2014 Apr 27;15:143. doi: 10.1186/1745-6215-15-143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Vedanthan R, Kamano JH, Horowitz CR, Ascheim D, Velazquez EJ, Kimaiyo S, Fuster V. Nurse management of hypertension in rural Western Kenya: implementation research to optimize delivery. Ann Glob Health. 2014 Jan-Feb;80(1):5–12. doi: 10.1016/j.aogh.2013.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]


