Abstract
Background
Escherichia coli is the most predominant causative agent of urinary tract infection (UTI). Recently, increase in drug resistance among the uropathogenic bacteria has caused great problem in treatment of UTI. The main objective of this research is to determine the correlation between biofilm formation and resistance toward different commonly used antibiotics along with extended spectrum beta lactamase production in uropathogenic Escherichia coli.
Methods
The urine samples collected from the patients suspected of urinary tract infections (visiting Shree Birendra Hospital, Chhauni, Kathmandu, Nepal between July to December 2013) were cultured in cystine lactose electrolyte deficient (CLED) agar by using semi quantitative culture technique. Extended spectrum beta lactamase (ESBL) production was detected by combined disc diffusion technique and biofilm formation was detected by Congo red agar method. Chi-square test was applied and p-value < 0.05 was considered statistically significant.
Results
Out of 1480 urine samples, E. Coli was isolated from 208 (14.1 %) samples. Of total 69 (33.2 %) ESBL producing uropathogenic strains of E. coli, 20 (29 %) were strong biofilm producers, 22 (31.9 %) were moderate biofilm producers, 11 (15.9 %) were weak biofilm producers and 16 (23.2 %) were biofilm non producers. Whereas among 139 ESBL non producing E. coli, 22 (15.8 %) were strong biofilm producers, 20 (14.4 %) were moderate biofilm producers, 13 (9.4 %) were weak biofilm producers and 84 (60.4 %) were biofilm non producers. Among total 108 biofilm producing E. coli, maximum resistance was observed toward cephalexin followed by amoxicillin and highest susceptibility was seen toward amikacin.
Conclusion
The ability of biofilm formation was found to be significantly higher in ESBL producing strains of E. coli than that in ESBL non producing strains (p < 0.05). There was higher resistance rate to antimicrobial agents among biofilm producing strains of E. coli than that in biofilm non producing strains. According to our antimicrobial susceptibility pattern for E. coli, to start preliminary treatment for UTI in Nepal, we recommend to use amikacin or nitrofurantoin. Further, for the treatment of the UTI, the antibiotics should be selected on the basis of the urine culture and sensitivity report.
Keywords: Escherichia coli, Urinary tract infection, Extended spectrum beta lactamase, Biofilm, Nepal
Background
Urinary tract infection (UTI) is one of the most common bacterial infections acquired both in the community and hospital settings, affecting all age groups [1, 2]. Worldwide, around 150 million cases of UTI are diagnosed each year [3] and Escherichia coli is identified as the most common cause of UTI, accounting for 80 to 85 % of the cases [4–6].
Recently the haphazard uses of antibiotics have resulted in the worldwide spread of antibiotic resistance among the bacteria causing a major problem [7]. The emergence and worldwide rapid increase in prevalence of extended spectrum beta-lactamase (ESBL) producing bacteria that are multidrug resistant, pose treatment problem resulting in high morbidity, high mortality, and increased health care costs [8]. Biofilm production is a mechanism exhibited by several microbes to survive in unfavorable conditions. The bacterial biofilm is a structured community of bacterial cells enclosed in polymeric matrix and adherent to a surface [9]. Biofilm producing uropathogenic bacteria may be responsible for many recurrent UTIs [10]. The bacteria enclosed in the biofilm are highly resistant to antibiotic treatment [9].
In this study we are investigating the incidence of the ESBL producing E. coli in causing UTI. Further we are determining the correlation between biofilm formation and drug resistance with commonly used antibiotics (for treatment of UTI) along with ESBL production in E. coli isolated from the urine samples of the patients suspected of urinary tract infections. This is the first this type of study conducted in Nepal.
Methods
A cross sectional study was conducted among the patients suspected of urinary tract infections (having symptoms like burning micturation, frequent or intense urge to urinate, back pain or lower abdominal pain, fever or chills etc.) visiting Shree Birendra Hospital, Chhauni, Kathmandu, Nepal since May to October 2013.
Total 1480 mid stream urine samples collected from the patients (out patients and in patients) suspected of urinary tract infections were cultured by the semi-quantitative culture technique [11]. The patients having laboratory or radiological evidence of other infections as the cause of the symptoms, patients with urinary catheterization and those who already have received antibiotics were excluded from our study. The bacterial isolates from the urine samples were identified by using microbiological techniques as described in the Bergey’s manual which include morphological appearance of the colonies, staining reactions and biochemical properties. The antimicrobial susceptibility testing was done by Kirby-Bauer disk diffusion technique as recommended by clinical and laboratory standards institute (CLSI) [12].
Detection of ESBL producers
Among the uropathogens isolated from suspected cases of UTI, only the strains of E. coli were subjected for detection of ESBL production. The phenotypic confirmation of the ESBL producing strains was done by combined disk method (Fig. 1) [12].
Fig. 1.

Confirmation of ESBL producer E. coli by combined disk method
Detection of biofilm producers
Detection of biofilm production was done for both ESBL positive and ESBL negative strains of E. coli by Congo red agar method (CRA) (Fig. 2) [13].
Fig. 2.
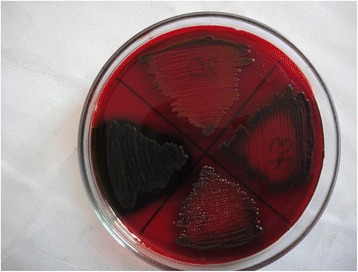
Biofilm detection test for Escherechia coli showing positive result on Congo red agar medium
On the basis of the intensity of color change of CRA medium after inoculation of the organisms, which is directly proportional to the amount of biofilm produced by the organisms, the biofilm producing organisms were classified into three categories as strong biofilm producers, moderate biofilm producers and weak biofilm producers [14, 15].
Data analysis
SPSS version 16.0 statistical software package was used for statistical analysis. Chi-square test was applied. P-value < 0.05 was considered statistically significant.
Results
Out of 1480 mid stream urine samples 278, (18.8 %) samples showed significant growth (≥ 105 cfu/ml). E. coli was isolated from 208 (74.82 %) samples. Out of 208 E. coli isolates 69 (33.2 %) were found to be ESBL producers and 139 (66.8 %) were ESBL non producers. Among 208 E. coli isolates 42 (20.192 %) were found to be strong biofilm producers, 42 (20.192 %) were moderate biofilm producers, 24 (11.538 %) were weak biofilm producers and 100 (48.076 %) were biofilm non producers.
Antibiotic resistance pattern of E. coli among biofilm producers and biofilm non producers
The antibiotic resistance among biofilm producing E. coli was found significantly higher than that of biofilm non producing E. coli (p < 0.05). The correlation between biofilm production and antibiotic resistance was found statistically significant (p < 0.05) in most of the antibiotics (ciprofloxacin, ofloxacin, norfloxacin, amikacin, gentamicin, cotrimoxazole, cephalexin, cefixime, ceftazidime, cefotaxime, ceftriaxone and cefepime) but the correlation was not found to be significant in case of amoxicillin and nitrofurantoin (Table 1).
Table 1.
Antibiotic resistance pattern of E. coli among biofilm producers and non producers along with the antibiotic susceptibility pattern of all the E. coli isolates
| Antibiotics used | Resistance pattern of biofilm producers and biofilm non producers | Total Resistant | Total susceptible | |||
|---|---|---|---|---|---|---|
| Strong producers N = 42 | Moderate producers N = 42 | Weak producers N = 24 | Non producers N = 100 | |||
| No (%) | No (%) | No (%) | No (%) | No (%) | No (%) | |
| Ciprofloxacin | 32 (76.2) | 32 (76.2) | 17 (70.8) | 45 (45.0) | 126 (60.6) | 82 (39.4) |
| Ofloxacin | 30 (71.4) | 30 (71.4) | 14 (58.3) | 39 (39.0) | 113 (54.3) | 95 (45.7) |
| Norfloxacin | 33 (78.6) | 32 (76,2) | 16 (66.7) | 45 (45.5) | 126 (60.6) | 82 (39.4) |
| Gentamicin | 24 (57.1) | 26 (61.9) | 6 (25.0) | 26 (26.0) | 82 (39.4) | 126 (60.6) |
| Amikacin | 7 (16.7) | 11 (26.2) | 3 (12.5) | 5 (5.0) | 26 (12.5) | 182 (87.5) |
| Cotrimoxazole | 27 (64.3) | 29 (69,0) | 17 (70.8) | 42 (42.0) | 115 (55.3) | 93 (44.7) |
| Amoxicillin | 40 (95.2) | 37 (88.1) | 22 (91.7) | 87 (87.0) | 186 (89.4) | 22 (10.6) |
| Cephalexin | 41 (97.6) | 38 (90.5) | 22 (91.7) | 74 (74.0) | 175 (84.1) | 33 (15.9) |
| Cefixime | 37 (88.1) | 41 (97.6) | 20 (83.3) | 59 (59.0) | 157 (75.5) | 51 (24.5) |
| Ceftazidime | 31 (73.8) | 36 (85.7) | 15 (62.7) | 40 (40.0) | 122 (58.7) | 86 (41.3) |
| Cefotaxime | 34 (81.1) | 34 (81.0) | 14 (58.3) | 35 (35.0) | 117 (56.2) | 91 (43.8) |
| Ceftriaxone | 29 (69.0) | 28 (66.7) | 15 (62.5) | 28 (28.0) | 100 (48.1) | 108 (51.9) |
| Cefepime | 31 (73.8) | 27 (64.3) | 12 (50.0) | 33 (33.0) | 103 (49.5) | 105 (50.5) |
| Nitrofurantoin | 12 (28.6) | 11 (26.2) | 6 (26.0) | 28 (28.0) | 57 (27.4) | 151 (72.6) |
Antibiotic susceptibility pattern of the uropathogenic E. coli isolated
Of total 208 E. coli isolates, the highest numbers of the strains were susceptible to amikacin followed by nitrofurantoin, gentamicin, ceftriaxone and cefepime. Similarly least numbers of the strains were susceptible to amoxicillin (Table 1).
Association of ESBL production and biofilm formation among E. coli isolates
Out of 69 ESBL producing uropathogenic strains of E. coli, 20 (29 %) were strong biofilm producers, 22 (31.9 %) were moderate biofilm producers, 11 (15.9 %) were weak biofilm producers and 16 (23.2 %) were biofilm non producers. Whereas among 139 ESBL non producing E. coli, 22 (15.8 %) were strong biofilm producers, 20 (14.4 %) were moderate biofilm producers, 13 (9.4 %) were weak biofilm producers and 84 (60.4 %) were biofilm non producers. The ability of biofilm formation was found to be significantly higher in ESBL producing strains of E. coli than that in ESBL non producing strains (p < 0.05).
Discussion
Among 208 E. coli isolates, 108 (51.92 %) were biofilm producers. This finding agrees with the findings of different authors from different parts of the world [16, 17]. Biofilm protects bacteria from host defense mechanisms, along with the antibiotics [18].
In this study, the antibiotic resistance of biofilm producing E. coli was found significantly higher than that of biofilm non producing E. coli (p < 0.05). Among biofilm producing E. coli, higher antibiotic resistance was observed in strong and moderate biofilm producers. The association between biofilm production and antibiotic resistance was found to be statistically significant (p < 0.05) except in case of amoxicillin and nitrofurantoin. Microorganisms growing in a biofilm are intrinsically resistant to many antibiotics increasing the antibiotic resistance up to 1000 folds and high antimicrobial concentrations are required to inactivate organisms growing in a biofilm [19, 20]. This may be because of the insufficient concentration of the antibiotics reaching some areas of the biofilms and metabolic inactiveness (along with the presence of active antibiotic degradation mechanisms contributing to halt the accumulation of the drugs up to an effective concentration) of the bacteria located at the base of the biofilms [9].
The biofilm forming ability was found to be significantly higher in ESBL positive strains of uropathogenic E. coli than that of ESBL negative strains [p < 0.05]. The study by Subramanian et al. in India also reported the higher ability of the ESBL producing organisms to form biofilm in comparison to that of ESBL non-producing isolates. It has been postulated that during occurrence of the large numbers of the chromosomal gene rearrangements upon acquisition of the ESBL plasmids the bacteria express several virulence genes [21].
ESBLs are enzymes that are responsible for resistance of bacteria toward third generation cephalosporins and monobactams [22]. Most of the plasmids responsible for ESBL production carry genes encoding resistance to other drugs also [23]. Due to frequent presence of cross-resistance to several other classes of antibiotics (like aminoglycosides and fluoroquinolones), in ESBL-producing organisms, the treatment of the infections by these bacteria are often present as the therapeutic challenges [22]. Further higher ability of the ESBL producing organisms to form biofilm makes the treatment even more difficult, increasing the mortality and severity of the infections [21]. Macrolides (erythromycin, clarithromycin, and azithromycin) are known to have antibiofilm activity against biofilm producing organisms by inhibiting a key component of the biofilm, alginate. And several studies have recommended, the combined therapy (being macrolides one of the first antibiotics chosen) as the treatment of choice in infections caused by biofilm producing organisms [9].
Increasing irrational and haphazard use of antibiotics, sales of substandard antibiotics and transmission of drug resistant bacteria among people may be responsible for the rise in antibiotic resistance among the bacteria [24]. Antimicrobial resistance has become a serious global public health issue. Infections caused by drug resistant bacteria are responsible for increased morbidity and mortality [25]. The selection of the antibiotics for treatment of the bacterial infections should be based on culture and sensitivity reports.
Conclusion
The ability of biofilm formation was found higher among ESBL producing strains of E. coli. There was higher resistance rate among biofilm producing E. coli isolates to almost all the antimicrobial agents except a few. According to our antimicrobial susceptibility pattern for E. coli, to start preliminary treatment for UTI in Nepal, we recommend to use amikacin or nitrofurantoin. Further, for the treatment of the UTI, the antibiotics should be selected on the basis of the urine culture and sensitivity report.
Limitations of the study
Due to lack of easy availability of the advanced laboratory in Nepal and due to lack of the fund we could not confirm the ESBL producing and biofilm producing organisms by using molecular technology.
Acknowledgements
The authors would like to thank all who contributed directly or indirectly in conduction of this research.
Abbreviations
- ATCC
American type culture collection
- CLED
Cystine lactose electrolyte deficient agar
- CLSI
Clinical and laboratory standards institute
- CRA
Congo red agar
- ESBL
Extended spectrum beta lactamase
- MHA
Mueller Hinton agar
- SPSS
Statistical package for the social sciences
- UTI
Urinary tract infection
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
SN designed the study, collected and processed the samples and analysed the data, NDP designed the study, analysed the data and prepared the manuscript, SK analysed the data, RC and MRB monitored the study. All authors read and approved the final manuscript.
Contributor Information
Sanjeev Neupane, Email: Neupane.sanjeev89@gmail.com.
Narayan Dutt Pant, Phone: +977-9749008524, Email: ndpant1987@gmail.com.
Saroj Khatiwada, Email: khatiwadasaroj22@gmail.com.
Raina Chaudhary, Email: raina_chaudhary@yahoo.co.in.
Megha Raj Banjara, Email: Banjaramr@gmail.com.
References
- 1.Ramesh N, Sumathi CS, Balasubramanian V, Palaniappan KR, Kannan VR. Urinary tract infection and antimicrobial susceptibility pattern of extended spectrum beta lactamase producing clinical isolates. Adv Biol Res. 2008;2:78–82. [Google Scholar]
- 2.Dromigny JA, Nabeth P, Perrier Gros Claude JD. Distribution and susceptibility of bacterial urinary tract infection in Dakar, Senegal. Int J Antimicrob Agents. 2002;20:339–47. doi: 10.1016/S0924-8579(02)00196-6. [DOI] [PubMed] [Google Scholar]
- 3.Gupta K. Increasing antimicrobial resistance and the management of uncomplicated community acquired urinary tract infections. Int J Antimicrob. 2001;135:41–50. doi: 10.7326/0003-4819-135-1-200107030-00012. [DOI] [PubMed] [Google Scholar]
- 4.Nicolle LE. Uncomplicated urinary tract infection in adults including uncomplicated pyelonephritis. Urol Clin North Am. 2008;35:1–12. doi: 10.1016/j.ucl.2007.09.004. [DOI] [PubMed] [Google Scholar]
- 5.Bhatta CP, Shrestha B, Khadka S, Swar S, Shah B, Pun K. Etiology of urinary tract infection and drug resistance cases of uropathogens. J Kath Med coll. 2012;2:114–20. [Google Scholar]
- 6.Sahm DF, Thornsberry C, Mayfield DC, Jones ME, Karlowsky JA. Multidrug-resistant urinary tract isolates of E. coli: prevalence and patient demographics in the United States. J Antimicrob Chemother. 2001;45:1402–6. doi: 10.1128/AAC.45.5.1402-1406.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goldstein FW. Antibiotic susceptibility of bacterial strains isolated from patients with community-acquired urinary tract infections in France. Multicentre Study Group. Eur J Clin Microbiol Infect Dis. 2000;19:112–7. doi: 10.1007/s100960050440. [DOI] [PubMed] [Google Scholar]
- 8.Schwaber MJ, Carmeli Y. Mortality and delay in effective therapy associated with extended-spectrum -lactamase production in Enterobacteriaceae bacteraemia: a systemic review and meta-analysis. J Antimicrob Chemother. 2007;60:913–20. doi: 10.1093/jac/dkm318. [DOI] [PubMed] [Google Scholar]
- 9.Soto SM. Importance of biofilms in urinary tract infections: new therapeutic approaches. Adv Biol. 2014;2014(2014):543974. [Google Scholar]
- 10.Rijavec M, Muller-Premru M, Zakotnik B, Bertok DZ. Virulence factors and biofilm production among Escherichia coli strains causing bacteraemia of urinary tract origin. J Med Microbio. 2008;57:1329–34. doi: 10.1099/jmm.0.2008/002543-0. [DOI] [PubMed] [Google Scholar]
- 11.Cheesbrough M. District laboratory practice in tropical countries, part II. 2. New York: Cambridge university press; 2006. pp. 112–3. [Google Scholar]
- 12.Clinical Laboratory Standards Institute . (CLSI) CLSI document M100S-S22. Performance standards for antimicrobial susceptibility testing: Twenty second informational supplement ed. Wayne: CLSI; 2012. [Google Scholar]
- 13.Mathur T, Singhal S, Khan S, Upadhyay DJ, Fatma T, Rattan A. Detection of biofilm formation among the clinical isolates of staphylococci: an evaluation of three different screening methods. Indian J Med Microbiol. 2006;24:25–9. doi: 10.4103/0255-0857.19890. [DOI] [PubMed] [Google Scholar]
- 14.Poovendran P, Vidhya N, Murugan S. Antimicrobial susceptibility pattern of ESBL and non-ESBL producing uropathogenic Escherichia coli (UPEC) and their correlation with biofilm formation. Intl J Microbiol Res. 2013;4:56–63. [Google Scholar]
- 15.Christensen GD, Simpson WA, Bisno AL, Beachey EH. Adherence of slime producing strains of Staphylococcus epidermidis to smooth surface. Infec Immun. 1982;37:318–26. doi: 10.1128/iai.37.1.318-326.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Anandkumar H, Soham G, Vinodkumar CS, Rao A, Srinivasa H. Detection of Cell Surface Hydrophobicity and Biofilm formation among ESBL and non-ESBL producing uropathogenic Escherichia coli. J Med Educ Res. 2012;2:12–20.
- 17.Nair BT, Bhat KG, Shantaram M. In vitro biofilm production and virulence factors of uropathogenic Escherichia coli. Int J Pharm Bio Sci. 2013;4:951–6. [Google Scholar]
- 18.Hanna A, Berg M, Stout V, Razatos A. Role of capsular colanic acid in adhesion of uropathogenic Escherichia coli. Appl Environ Microbiol. 2003;69:4474–81. doi: 10.1128/AEM.69.8.4474-4481.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thien-fah UK, George PA. Mechanism of biofilm resistance to antimicrobial agents. Trends Microbiol. 2001;9:34–9. doi: 10.1016/S0966-842X(00)01913-2. [DOI] [PubMed] [Google Scholar]
- 20.Stewart PS, Costerton JW. Antibiotic resistance of bacteria in biofilms. Lancet. 2001;358:135–8. doi: 10.1016/S0140-6736(01)05321-1. [DOI] [PubMed] [Google Scholar]
- 21.Subramanian P, Umadevi S, Kumar S, Stephen S. Determination of correlation between biofilm and extended spectrum β lactamases producers of Enterobacteriaceae. Scho Res J. 2012;2:2–6. doi: 10.4103/2249-5975.119797. [DOI] [Google Scholar]
- 22.Black JA, Moland ES, Thomson KS. AmpC disk test for detection of plasmid-mediated AmpC-b lactamases in Enterobacteriaceae lacking chromosomal AmpC-b lactamases. J Clin Microbiol. 2005;43:3110–3. doi: 10.1128/JCM.43.7.3110-3113.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Paterson DL, Bonomo RA. Extended-spectrum beta-lactamases: a clinical update. Clin Microbiol Rev. 2005;18:657–86. doi: 10.1128/CMR.18.4.657-686.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gautam R, Chapagain ML, Acharya A, Rayamajhi N, Shrestha S, Ansari S, et al. Antimicrobial susceptibility patterns of Escherichia coli from various clinical sources. JCMC. 2013;3:14–7. [Google Scholar]
- 25.Awasthi TR, Pant ND, Dahal PR. Prevalence of Multidrug Resistant Bacteria in Causing Community Acquired Urinary Tract Infection Among the Patients Attending Outpatient Department of Seti Zonal Hospital, Dhangadi, Nepal. Nepal J Biotechnol. 2015;3(1):55–9. doi: 10.3126/njb.v3i1.14232. [DOI] [Google Scholar]


