Abstract
The ways in which humans affect and are affected by their environments have been studied from many different perspectives over the past decades. However, it was not until the 1970s that the discussion of the ethical relationship between humankind and the environment formalized as an academic discipline with the emergence of environmental ethics. A few decades later, environmental health emerged as a discipline focused on the assessment and regulation of environmental factors that affect living beings. Our goal here is to begin a discussion specifically about the impact of modern environmental change on biomedical and social understandings of brain and mental health, and to align this with ethical considerations. We refer to this focus as Environmental Neuroethics, offer a case study to illustrate key themes and issues, and conclude by offering a five-tier framework as a starting point of analysis.
Keywords: Brain health, Mental health, Environment, Ethics, Social implications
Background: At the crossroads of environment, brain and mental health
Humans have altered their environments in pursuit of self-improvement and better opportunities since ancient times, but the scope and impact of these changes are unprecedented today [1]. Technological advancements have yielded positive economic growth, improved standards of living, and provided new ways of protecting human health. At the same time, technology has contributed to widespread negative changes in the environment that include global climate change, deforestation, suburban sprawl, ecosystem loss, and increased health risks from exposure to radiation, toxicants, and stress.
While there are different views among scholars of environmental ethics about why humans should value the environment [2], a common position focuses on direct and potential consequences to human health and well-being [3]. Environmental health experts similarly focus on environmental changes in terms of their impact on human health. However, within approaches to environmental ethics and environmental health, less attention has been paid to the specific ethical, social and legal implications of these changes for brain and mental health.1 To do so, requires that we probe the intersection of diverse biological, social and cultural contexts of human well-being.
Brain and mental health are determined by complex interactions between individual predispositions and behavior, social and economic processes, and the environment [4, 5]. Classic examples pointing to an association between neurological function and environmental changes include neurological deficits from exposure to mercury [6] and lead [7–9], various forms of air [10–14] and water pollution [15], pesticides, and solvents [16–20]. Moreover, cross-cultural studies of indigenous worldviews on identity, concepts of the self, and wellness have highlighted the direct and intimate connections between individuals and their environments [21, 22]. These studies remind us not only about cross-cultural differences involved in experiencing brain health and the environment, but also about different layers of vulnerability [23] brought forward by the impact of environmental change. Children [24], the elderly [25], workers who may be exposed occupationally to neurotoxicants [20] and people who live in the proximity of neurotoxicant sources [26] are more vulnerable than other sectors of the population. These unequal levels of exposure interacting with brain stage in development or decline, and differential effects from environmental risks are at the core of the environmental justice movement and, in regard to brain and mental health outcomes, are a central concern of Environmental Neuroethics.
Our goal here is to begin a discussion specifically about the impact of modern environmental change on biomedical and social understandings of brain and mental health, and to align this with ethical considerations. There are several reasons for thinking that this approach is timely. To start, brain and mental health disorders, many of which have important environmental factors, are leading contributors to disabilities and morbidity that produce critical public health, societal and economic impacts [27]. In addition, brain development, as well as its optimal function throughout the life of individuals, is particularly susceptible to the environment to which a person is exposed [24]. Considering the vulnerability of brains towards environmental exposures that are not easy to identify or to eliminate [24], we can see why brain and mental health are matters of global concern and social justice and, in particular, as the health risks related to environmental exposures are often distributed unequally. Thus, it becomes crucial to mitigate the negative impacts of environmental change while ensuring fair distribution of the positive ones. This balance represents a key aspect of the Environmental Neuroethics approach we present here.
Fracking as a case study
Fuel sources with low greenhouse gas emissions are frequently advanced as a replacement to the rapid expansion in fossil fuel usage [28]. Technological advancements such as hydraulic fracturing (fracking) have now made extraction of these gas reserves profitable. The fracking process can impact the environment in various ways through the extraction and discharge of massive quantities of contaminated water, injection of various chemicals into the ground, and the disruption of the landscape with high densities of roads and well-heads that encroach on human settlements and wild habitats [29]. Like other literature on environmental change, contamination of the air and water supplies in the vicinity of fracking operations [17, 30] has been linked to health impacts that include asthma, respiratory complaints, gastro-intestinal effects and nosebleeds [31, 32]. Such contamination is also related to negative neurological effects. For example, McKenzie and colleagues [26] carried out a retrospective cohort study of 124,842 births between 1996 and 2009 in rural Colorado examining the associations between maternal proximity to fracking sites and birth outcomes. They found that births to mothers residing close to or surrounded by wells (>125 wells/mile) were twice as likely to have a neural tube defects compared to those with no wells within a 10-mile radius (OR = 2.0; 95 % CI: 1.0, 3.9, based on 59 cases).
With these types of foundational studies in mind, we examined the prevalence in the literature of associations made between fracking and neurological or mental health impacts. To this end, we carried out an extensive search of peer-reviewed and gray literature of articles, theses, books, abstracts, and government reports on unconventional gas development (UGD), environment, brain and mental health using Google Scholar, the most comprehensive database relevant to the goals of the study. The searches were based on two primary key terms: (1) unconventional gas development, and (2) brain; key UGD search terms: {unconventional natural gas (+/−) development}, {shale gas (+/−) development}, {fracking} and {hydraulic fracturing}; and, key brain search terms were {brain}, {neuro}, {neurological} and {mental}. We also used a range of secondary search terms to ensure that searches identify studies relevant to culture, First Nations, health, ethics, and solastalgia.2 Of the one hundred and six articles identified, 83 articles originated from the peer-reviewed literature (reviews, N = 57; primary research N = 26) and 23 from the gray literature, dating back to 2009 (Fig. 1).
Fig. 1.
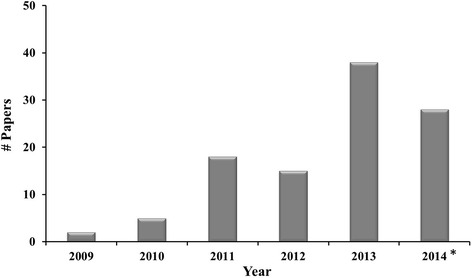
Number of articles on fracking and brain by year (*up to September 2014)
To provide context, we explored the origin of the cases in our sample for country of corresponding author and corresponding author disciplines. Most returns originated from the United States (USA) (N = 83). Twelve papers originated from Australia and six from Canada. One paper meeting our inclusion criteria originated each from China, Germany, New Zealand, Switzerland and United Kingdom. Based on the corresponding authors’ affiliation, we found that the majority of corresponding authors held multiple disciplinary associations (N = 45). Twenty-two held affiliations in the health sciences (e.g., medicine), 21 in the social sciences (e.g., sociology, law), 11 were associated with environmental sciences, such as ecology or forestry, and seven have disciplines represented only in a limited basis such as engineering or regional planning.
To explore the texts in depth, we conducted a three-part content analysis [33, 34] of the full set of cases. Each individual article was used as the unit of analysis. In the first phase of the analysis, we found that the dominant themes relate to public health (N = 31), and regulation and policy (N = 22). Five articles mention UGD and fracking broadly as a threat to Indigenous health.
In a second phase, we focused on brain and mental health. Eight of the 106 papers contain elaborate detailed examination of the impact that UGD poses for brain and mental health, arguments for associations between brain and mental health related to UGD, or both. The remaining papers only explore the relationship between fracking chemicals and neurotoxicity superficially and provide little if any mention of ethical implications.
In the third phase, we focused specifically on content related to ethics. Two papers provide substantial ethical discussion. One paper argues that environmental damage caused by hydraulic fracturing poses “a new threat to human rights” [35]. The other, written by members of the present author group, makes a call to the Presidential Commission for the integration of ethical considerations and neuroscience into the study of environmental change [36]. Sixty-five papers mention safety and issues related to the duty not to inflict harm; 41 papers mention at least one other ethical concern such as trust, vulnerability, justice, and disempowerment but without any further elaboration on the matter. Overall, the findings reveal that while there is emphasis on health, there is limited ethical discussion of brain and mental health impacts.
Environmental Neuroethics in the wild
Environmental Neuroethics can provide a framework to investigate the ethical and social implications of environmental change on brain and mental health. Building on previous work [37], we propose a five-tier framework:
Brain science and the environment: Neuroscience discovery that is aligned with the measurement and evaluation of factors that affect the way individuals, communities and society adapt and cope with real or perceived environmental threats to well-being.
The relational self and the environment: The interface between the environment and brain and mental health, and the mechanisms by which exposures at key points in life may mediate different brain and mental effects; relationships among mental health stressors, susceptibility to mental health issues, and resilience within the context of changing environments.
Cross-cultural factors and the environment: Exploration of the role of culture in the relationship between environment and brain and mental health; interactions between Traditional Ecological Knowledge and neuroscience evidence; the impact of environmental change and varying effects on First Nations and settler communities given respective relationships between culture and the environment.
Social policy and the environment: Priorities and allocation of resources of local social organizations to deal with environmental impacts on brain and mental health.
Public discourse and the environment: The engagement of professional disciplines and communities in multidirectional communication and discourse about neurological, psychological, sociological and ethical dimensions of environmental change; facilitation of international, cross-disciplinary, transdisciplinary collaborations; creation of effective outreach programs that promote public understanding about the impact of environmental change on brain and mental health.
This framework can be extended more broadly to other environmental impacts such as the extraction of natural resources, air pollution, use of agricultural chemicals, water contamination, proximity to noxious facilities, mining waste and nuclear plants, ocean degradation, food contamination, and habitat destruction. Moreover, while the focus here has been on changes to the physical environment, Environmental Neuroethics is also concerned with other environments such as digital and social environments, and how these impact neurological health.
Notwithstanding the opportunity to expand ethical and social discussion around environmental change, priority setting and paths to action are not without challenges. Reliability and stability of evidence [38], knowledge of impacts [39], and appreciation of risk [40–42] are perceived and weighted differently by different stakeholders and are among the key obstacles.
Conclusions
The identified gaps in the ethical discussion related to environmental change and health as well as the vulnerability of brains, suggest that it is time for an Environmental Neuroethics dedicated to address the interaction of biomedical and social understandings of anthropogenic environmental change. In moving forward, results and resulting scholarship and guidance must be specific, solution-oriented, and proportionate to the benefits and risks in play.
Acknowledgments
We would like to acknowledge the support of CIHR (MOP-111240), the North Growth Foundation, and the Canada Research Chairs Program. This work was further enabled by support from the British Columbia Knowledge Development Fund, the Canadian Foundation for Innovation and the Vancouver Coastal Health Research Institute.
Footnotes
We use the term mental health to include “well-being, everyday problems in living associated with bodily symptoms of stress and anxiety, mild depression, and seasonal fluctuations in mood and energy, as well as more severe psychiatric disorders, such as major depression, bipolar disorder, schizophrenia, and other psychotic disorders” [21 xiv].
A term used to refer to distress cause by environmental change.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
LC participated in the design of the study, carried out analysis of data and drafted the manuscript. MC gathered the data and helped with the analysis. JT, RM participated in the design of the study and interpretation of data. JI conceived the study, participated in its design and coordination, and helped to draft the manuscript. All authors read and approved the final manuscript.
Contributor Information
Laura Y. Cabrera, Email: Laura.cabrera@singularityu.org
Jordan Tesluk, Email: jdtesluk@gmail.com.
Michelle Chakraborti, Email: michelle5ubc@gmail.com.
Ralph Matthews, Email: ralph.matthews@ubc.ca.
Judy Illes, Email: jilles@mail.ubc.ca.
References
- 1.Watts N, Maiero M, Olson S, Hales J, Miller C, Campbell K, Romanelli C, Cooper D. Our planet, our health, our future. Geneva: World Health Organization; 2012. [Google Scholar]
- 2.Sagoff M. Zuckerman’s dilemma: A plea for environmental ethics. Hastings Cent Rep. 2008;21:1–10. [PubMed] [Google Scholar]
- 3.Katz E, Light A. Environmental pragmatism. New York: Routledge; 1996. [Google Scholar]
- 4.Blas E, Sommerfeld J, Kurup AS. Social determinants approaches to public health. Geneva: World Health Organization; 2011. [Google Scholar]
- 5.Public Health Agency of Canada . What determines health? 2011. [Google Scholar]
- 6.Grandjean P, Herz KT. Methylmercury and brain development: Imprecision and underestimation of developmental neurotoxicity in humans. Mt Sinai J Med. 2011;78:107–18. doi: 10.1002/msj.20228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Patterson CC. Contaminated and natural lead environments of man. Arch Environ Health. 1965;11:344–60. doi: 10.1080/00039896.1965.10664229. [DOI] [PubMed] [Google Scholar]
- 8.Needleman HL, Schell A, Bellinger D, Leviton A, Allred EN. The long-term effects of exposure to low doses of lead in childhood. An 11-year follow-up report. N Engl J Med. 1990;322:83–8. doi: 10.1056/NEJM199001113220203. [DOI] [PubMed] [Google Scholar]
- 9.Nelson RM. Appropriate risk exposure in environmental health research. The Kennedy-Krieger lead abatement study. Neurotoxicol Teratol. 2002;24:445–9. doi: 10.1016/S0892-0362(02)00236-2. [DOI] [PubMed] [Google Scholar]
- 10.Calderón-Garcidueñas L, Azzarelli B, Acuna H, Garcia R, Gambling TM, Osnaya N, Monroy S, Tizapantzi MD, Carson JL, Villarreal-Calderon A, Rewcastle B. Air pollution and brain damage. Toxicol Pathol. 2002;30:373–89. doi: 10.1080/01926230252929954. [DOI] [PubMed] [Google Scholar]
- 11.Calderón-Garcidueñas L, Mora-Tiscareño A. Air pollution, cognitive deficits and brain abnormalities: A pilot study with children and dogs. Brain Cogn. 2008;68:117–27. doi: 10.1016/j.bandc.2008.04.008. [DOI] [PubMed] [Google Scholar]
- 12.Calderón-Garcidueñas L, Reed W, Maronpot R, Henriquez-Rold NC, Delgado-Chavez R, Calderón-Garcidueñas A, Dragustinovis I, Franco-Lira M, Aragón-Flores M, Solt A, Altenburg M, Torres-Jard NR, Swenberg J. Brain inflammation and Alzheimer’s-like pathology in individuals exposed to severe air pollution. Toxicol Pathol. 2004;32:650–8. doi: 10.1080/01926230490520232. [DOI] [PubMed] [Google Scholar]
- 13.Field RA, Soltis J, Murphy S. Air quality concerns of unconventional oil and natural gas production. Environ Sci Process Impacts. 2014;16:954–69. doi: 10.1039/c4em00081a. [DOI] [PubMed] [Google Scholar]
- 14.Peters A, Veronesi B, Calderón-Garcidueñas L, Gehr P, Chen LC, Geiser M, Reed W, Rothen-Rutishauser B, Schürch S, Schulz H. Translocation and potential neurological effects of fine and ultrafine particles a critical update. Part Fibre Toxicol. 2006;3:13. doi: 10.1186/1743-8977-3-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Villanueva CM, Kogevinas M, Cordier S, Templeton MR, Vermeulen R, Nuckols JR, Nieuwenhuijsen MJ, Levallois P. Assessing exposure and health consequences of chemicals in drinking water: Current state of knowledge and research needs. Environ Health Perspec. 2014;122:213–21. doi: 10.1289/ehp.1206229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dick FD. Solvent neurotoxicity. Occup Environ Med. 2006;63:221–6. doi: 10.1136/oem.2005.022400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grandjean P, Landrigan PJ. Developmental neurotoxicity of industrial chemicals. Lancet. 2006;368:2167–78. doi: 10.1016/S0140-6736(06)69665-7. [DOI] [PubMed] [Google Scholar]
- 18.Grandjean P, Harari R, Barr DB, Debes F. Pesticide exposure and stunting as independent predictors of neurobehavioral deficits in Ecuadorian school children. Pediatrics. 2006;117:e546–56. doi: 10.1542/peds.2005-1781. [DOI] [PubMed] [Google Scholar]
- 19.Harari R, Julvez J, Murata K, Barr D, Bellinger DC, Debes F, Grandjean P. Neurobehavioral deficits and increased blood pressure in school-age children prenatally exposed to pesticides. Environ Health Perspec. 2010;118:890–6. doi: 10.1289/ehp.0901582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tang CY, Carpenter DM, Eaves EL, Ng J, Ganeshalingam N, Weisel C, Qian H, Lange G, Fiedler NL. Occupational solvent exposure and brain function: An fMRI study. Environ Health Perspec. 2011;119:908–13. doi: 10.1289/ehp.1002529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kirmayer LJ, Valaskakis GG. Healing traditions: The mental health of aboriginal peoples in Canada. Vancouver: UBC Press; 2009. [Google Scholar]
- 22.Vukic A, Gregory D, Martin-Misener R, Etowa J. Aboriginal and Western Conceptions of Mental Health and Illness. Pimatisiwin. 2011;9:65–86. [Google Scholar]
- 23.Luna F. Elucidating the concept of vulnerability: Layers not labels. Int J Fem Approaches Bioeth. 2009;2:121–39. doi: 10.2979/FAB.2009.2.1.121. [DOI] [Google Scholar]
- 24.Grandjean P. Only one chance: How environmental pollution impairs brain development - and how to protect the brains of the next generation. New York: Oxford University Press; 2013
- 25.Grossman E. Time after time: Environmental influences on the aging brain. Environ Health Perspec. 2014;122:A238–43. doi: 10.1289/ehp.122-A238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McKenzie LM, Guo R, Witter R, Savitz D, Newman L, Adgate J. Birth outcomes and maternal residential proximity to natural gas development in rural Colorado. Environ Health Perspect. 2014;122(4):412–7. doi: 10.1289/ehp.1306722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pruss-Ustun A, Corvalan C. Preventing disease through healthy environments. Geneva: World Health Organization; 2006. [Google Scholar]
- 28.The Royal Society . Shale gas extraction in the UK: A review of hydraulic fracturing. London: The Royal Society and the Royal Academy of engineering; 2012. [Google Scholar]
- 29.Council of Canadian Academies. Environmental impacts of shale gas extraction in Canada. Ottawa: Council of Canadian Academies; 2014.
- 30.Burton GA, Basu N, Ellis BR, Kapo KE, Entrekin S, Nadelhoffer K. Hydraulic “fracking”: Are surface water impacts an ecological concern? Environ Toxicol Chem. 2014;33:1679–89. doi: 10.1002/etc.2619. [DOI] [PubMed] [Google Scholar]
- 31.McDermott-Levy R, Kaktins N, Sattler B. Fracking, the environment, and health. Am J Nurs. 2013;113:45–51. doi: 10.1097/01.NAJ.0000431272.83277.f4. [DOI] [PubMed] [Google Scholar]
- 32.Somerset FF. The health implications of fracking. Lancet. 2014;383:757–8. doi: 10.1016/S0140-6736(13)62700-2. [DOI] [PubMed] [Google Scholar]
- 33.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101. doi: 10.1191/1478088706qp063oa. [DOI] [Google Scholar]
- 34.Saldana J. The coding manual for qualitative researchers. London: Sage; 2012. An intro to codes and coding; pp. 1–40. [Google Scholar]
- 35.Kern TA. A human rights assessment of hydraulic fracturing for natural gas. 2011. [Google Scholar]
- 36.Illes J, Davidson J, Matthews R. Environmental neuroethics: Changing the environment changing the brain. Recommendations submitted to the Presidential Commission for the Study of Bioethical Issues. J Law Biosci. 2014;1:221–3. doi: 10.1093/jlb/lsu015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Marcus S. Neuroethics: Mapping the field. Conference proceedings. New York: The Dana Press; 2002. [Google Scholar]
- 38.Dudgeon RC, Berkes F. Local understandings of the land: Traditional Ecological Knowledge and indigenous knowledge. In: Selin H, editor. Nature across cultures: Views of nature and the environment in non-Western cultures. Dordrecht: Kluwer Academic Publishers; 2003. pp. 75–96. [Google Scholar]
- 39.Goldstein BD, Kriesky J, Pavliakova B. Missing from the table: Role of the environmental public health community in governmental advisory commissions related to Marcellus Shale drilling. Environ Health Perspec. 2012;120:483–6. doi: 10.1289/ehp.1104594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sjoberg L. Factors in risk perception. Risk Anal. 2000;20:1–12. doi: 10.1111/0272-4332.00001. [DOI] [PubMed] [Google Scholar]
- 41.Slimak MW, Dietz T. Personal values, beliefs, and ecological risk perception. Risk Anal. 2006;26:1689–705. doi: 10.1111/j.1539-6924.2006.00832.x. [DOI] [PubMed] [Google Scholar]
- 42.Beck U. Risk society: Towards a new modernity. London: Sage; 1992. [Google Scholar]


