Abstract
Aims
Hypoglycaemia is a serious medical emergency. The need for emergency medical service care and the costs of hypoglycaemic emergencies are not completely known.
Methods
This was a retrospective observational study using Public Company for Health Emergencies (EPES) data for hypoglycaemia in 2012. The EPES provides emergency medical services to the entire population of Andalusia, Spain (8.5 million people). Data on event type, onsite treatments, emergency room visits or hospitalization were collected. Medical costs were estimated using the public rates for healthcare services.
Results
From a total of 1 137 738 emergency calls that requested medical assistance, 8683 had a primary diagnosis of hypoglycaemia (10.34 per 10 000 person‐years). The incidence of severe hypoglycaemic episodes requiring emergency treatment in the estimated population with diabetes was 810 episodes per 10 000 person‐years. A total of 7479 episodes (86%) required an emergency team to visit the patient's residence. The majority of cases (64%) were addressed in the residence, although 1784 (21%) cases were transferred to hospital. A total of 5564 events (65%) involved patients aged > 65 years. Overall mortality was 0.32% (28 cases). The total annual cost of attending a hypoglycaemic episode was €6 093 507, leading to an estimated mean direct cost per episode of €702 ± 565. Episodes that required hospital treatment accounted for 49% of the total costs.
Conclusions
Hypoglycaemia is a common medical emergency that is associated with high emergency medical service utilization, resulting in a significant economic impact on the health system.
What's new?
This is a retrospective study of all registered hypoglycaemic emergency calls (n = 8683) in 2012 that were serviced by the emergency medical services in Andalusia, Spain (8.5 million inhabitants).
Understanding the incidence of hypoglycaemic emergencies in this population (10.34 per 10 000 person‐years) may be valuable for clinical and epidemiological purposes.
The frequency of calls was lower during the night, but the average urgency was higher than during the remainder of the day.
Our results indicate the high cost of treating hypoglycaemia as emergency care (€702 per episode).
The episodes that require referral to a hospital (21%) represented half of the total expenditure.
What's new?
This is a retrospective study of all registered hypoglycaemic emergency calls (n = 8683) in 2012 that were serviced by the emergency medical services in Andalusia, Spain (8.5 million inhabitants).
Understanding the incidence of hypoglycaemic emergencies in this population (10.34 per 10 000 person‐years) may be valuable for clinical and epidemiological purposes.
The frequency of calls was lower during the night, but the average urgency was higher than during the remainder of the day.
Our results indicate the high cost of treating hypoglycaemia as emergency care (€702 per episode).
The episodes that require referral to a hospital (21%) represented half of the total expenditure.
Introduction
Diabetes mellitus affects 13.8% of the Spanish population over 18 years of age 1. Following global trends, the prevalence of the disease in Spain is expected to increase in future years. Diabetes‐associated mortality doubled between 1990 and 2010, and after adjusting the years to reflect disability, the number of healthy years of life that were lost to this disease increased by 70% 2, 3. One of the known causes of death in patients with diabetes is hypoglycaemia 4, 5.
Hypoglycaemia is a common adverse complication of treating diabetes. Event rates for severe hypoglycaemia in people with Type 1 diabetes range from 115 to 320 per 100 person‐years 6, 7, 8, 9. Severe hypoglycaemia in insulin‐treated individuals with Type 2 diabetes has been shown to occur at rates of 10–70 episodes per 100 person‐years 6, 7, 8, 9. However, when broader populations of people with Type 2 diabetes are included, the incidence of severe hypoglycaemia ranges from 0 to 3 per 100 person‐years in adults with Type 2 diabetes 7. However, because Type 2 diabetes is more prevalent than Type 1 diabetes, most episodes of hypoglycaemia, including severe hypoglycaemia, occur in people with Type 2 diabetes 8. Treatment with hypoglycaemic agents, i.e. secretagogues and insulin, and a previous history of hypoglycaemia are powerful risk factors for further hypoglycaemia 6, 7, 10.
Hypoglycaemia is a frequent cause of hospitalization 11. Recent evidence has indicated that insulin‐related hypoglycaemia is responsible for nearly 100 000 visits to emergency departments in the USA each year 12. This represents ~ 10% of the number of emergency department visits from adverse drug reactions per year. The number of visits is particularly high in the elderly. Those over 80 years of age were more than twice as likely as those aged 45–64 years to visit the emergency department and nearly five times as likely to be hospitalized. These data correspond with those of previous studies, which have shown that treatment with insulin and oral hypoglycaemic drugs (sulfonylureas and meglitinides) are among the main adverse drug‐event‐related causes of hospital admissions in people over 65 years of age 13. In a follow‐up study of self‐reported hypoglycaemia in 630 persons with Type 1 and Type 2 diabetes undergoing insulin therapy, Orozco‐Beltran et al. showed that 30% of respondents who had experienced a severe hypoglycaemia episode (SHE) required an emergency hospital visit following their last SHE and 19% were admitted to hospital 14.
Few studies have reported on the need for emergency medical service care, outcomes, resource utilization and costs of hypoglycaemic emergency care in people with hypoglycaemia. Accordingly, we aimed to determine the incidence and outcomes of hypoglycaemic episodes that require attention from the Andalusia emergency care system and report the economic impact associated with these interventions.
Patients and methods
The Health Emergency Public Company (EPES, for its initials in Spanish) coordinates outpatient assistance for all emergency care for the Andalusia Autonomous Region, serving the entire population of 8 393 159 in 2012 15. This study is embedded in the Emergency Assistance of the Person with Diabetes Project (PAUEPAD, for its initials in Spanish). Institutional review board approval was obtained through the EPES and Investigation Committee, and the requirement for informed consent was waived based on the nature of the study.
We conducted a retrospective observational study of all registered hypoglycaemic calls attended by the EPES between 1 January 2012 and 31 December 2012. Cases that were treated by another emergency medical assistance provider with a final diagnosis of hypoglycaemia must be reported to the EPES, and were also included. Therefore, this study collected all cases of severe hypoglycaemia requiring emergency assistance that occurred in the population during 2012.
As part of their function, the eight EPES coordinator centres systematically gather and register all the information received. The EPES database includes demographic data, the age and gender of the patient, and the date and time of the call. In addition, a computerized system based on the Manchester Triage System was used to determine the urgency of events based on the reported signs and symptoms 16. The following five urgency categories were included: non‐urgent (0), standard (1), urgent (2), very urgent (3) and immediate (4). Medical resources were assigned accordingly.
Episodes were documented as hypoglycaemia if a blood glucose level < 3.9 mmol/l was measured during the episode 10. After treatment, the emergency team assigned codes to diagnoses using the 9th edition of the International Classification of Diseases‐Clinical Modification (ICD‐9‐CM) 17. Unconsciousness was also recorded.
The annual incidence of hypoglycaemia was calculated using the total population of Andalusia registered in the National Institute of Statistics as of 1 January 2013 15. The annual incidence rate (assuming that the majority of cases identified had diabetes) for the Andalusian population with diabetes according to gender and age group was estimated using data on the prevalence of diabetes, as reported in the Di@bet.es Study 18 (Table 1).
Table 1.
Severe hypoglycaemia episodes requiring emergency care (total population and population with diabetes) according to age and percentage of transfers to hospital
| Incidence | % Hospital transfers | |||||||
|---|---|---|---|---|---|---|---|---|
| Total populationa (n = number of cases) | Patients with diabetesb (n = estimated number of patients with diabetes) | |||||||
| Age (years) | Men | Women | All | Men | Women | All | Men | Women |
| 0–17 | 1.07 | 1.10 | 1.08 | 478 (387–584) | 707 (571–864) | 569 (459–656) | 41.7 | 42 |
| n = 91 | n = 88 | n = 179 | n = 1895 | n = 1,242 | n = 3,157 | n = 38 | n = 37 | |
| 18–30 | 3.69 | 3.13 | 3.41 | 264 (232–297) | 448 (391–511) | 323 (295–354 | 22.6 | 20.6 |
| n = 256 | n = 209 | n = 465 | n = 9,713 | n = 4,667 | n = 14,380 | n = 58 | n = 43 | |
| 31–45 | 5.33 | 3.72 | 4.54 | 69 (64–75) | 149 (135–165) | 88 (83–94) | 22 | 17.1 |
| n = 563 | n = 380 | n = 943 | n = 81,295 | n = 25,492 | n = 106,787 | n = 124 | n = 65 | |
| 46–60 | 7.77 | 5.15 | 6.45 | 32 (29–34) | 42 (38–46) | 35 (33–37) | 23.5 | 21 |
| n = 649 | n = 433 | n = 1082 | n = 204,567 | n = 103,402 | n = 307,978 | n = 153 | n = 91 | |
| 61–75 | 19.53 | 19.50 | 19.52 | 41 (39–44) | 68 (64–72) | 52 (50–54) | 25.6 | 20.6 |
| n = 970 | n = 1,079 | n = 2,049 | n = 234,842 | n = 159,301 | n = 394,143 | n = 248 | n = 222 | |
| > 75 | 62.60 | 71.78 | 68.22 | 154 (146–162) | 160 (154–167) | 158 (153–163) | 23.4 | 18.4 |
| n = 1,411 | n = 2,554 | n = 3,965 | n = 91,728 | n = 159,397 | n = 251,125 | n = 330 | n = 470 | |
| Total | 9.48 | 11.19 | 10.34 | 63 (61–65) | 105 (102–108) | 80 (78–83) | 24.1 | 19.6 |
| n = 3,940 | n = 4,743 | n = 8,683 | n = 624,063 | n = 453,507 | n = 1,077,570 | n = 950 | n = 930 | |
Incidence rates (events per 10,000 person‐years) calculated among the total population, corresponding to confidence intervals of 100%.
Incidence rates among people with diabetes (DM): events per 10,000 person‐years (95% CI)
The reference time corresponds to the moment that assistance was requested. Events were classified as severe nocturnal hypoglycaemic episodes if the calls were received between 00:00 and 07:59.
Direct costs were estimated using the public prices published by the Andalusia Public Healthcare System 19, updated for 2012. Transfer distance was calculated from the primary care setting to the corresponding hospital. The estimate excludes the costs of incidents that the physician solved over the phone from the coordinator centre. The costs of hospitalization after emergency assistance and costs resulting from a stay of > 24 h were also excluded from the study.
Data analysis was performed using the PASW statistical package, v. 18.0 (SPSS Inc. Quarry Bay, Hong Kong). The results are presented using the mean and standard deviation for the quantitative variables and the absolute and relative frequencies for the qualitative variables. Confidence intervals (95% CI) were obtained using the exact binomial method. The frequency of SHEs or the mean category of urgency was evaluated using a t–test for unequal variance samples. We performed a logistic regression analysis to quantify the influence of sex, age group, time interval, month of referral and hospital location.
Results
During 2012, the EPES coordinator centres answered 1 137 738 calls for assistance in Andalusia 20, of which 8683 (0.76%) were classified as hypoglycaemia requiring assistance. All cases were classified as SHEs because third‐party assistance was needed to correct the hypoglycaemic condition 10.
The 8683 SHEs had the following frequency distribution: one SHE, 5990 cases; two SHEs, 841 cases; three SHEs, 212 cases; four SHEs, 63 cases; five SHEs, 8 cases; six SHEs, 9 cases; nine SHEs, 1 cases; and ten SHEs, 2 cases. Thus, 16% of patients requested assistance for more than one episode.
The mean age of the patients was 66 ± 20.2 years (range: 1–107), and 54.6% of patients were women. More than two thirds of the patients were over 60 years of age, and 45.6% were over 76 years of age. The accumulated annual incidence of SHEs requiring emergency care for the study population was 10.34 per 10 000 person‐years (11.19 for women and 9.48 for men). In patients over 75 years of age, the annual incidence was 68.22 per 10 000 person‐years (Table 1). Data on the estimated accumulated annual incidence of hypoglycaemia in the Andalusia population with diabetes according to gender and age group are shown in Table 1. The incidence rate in the population with diabetes was higher in the two extreme age populations, i.e. 0–30 years: 367 events per 10 000 person‐years (95% CI: 329–409); and > 75 years: 158 events per 10 000 person‐years (95% CI: 153–163).
Urgency category and the time distribution of the SHEs are shown in Fig. 1. Nocturnal SHEs were less frequent than diurnal SHEs with 0.34 ± 0.03 (n = 2297) vs. 0.47 ± 0.09 (n = 6386) episodes per hour (P ˂ 0.001). Nevertheless, mean urgency category was higher during the night than during the day, with 3.36 ± 0.04 (n = 2297) vs. 3.31 ± 0.04 (n = 6386) episodes (P = 0.01). The mean age of patients treated during the night was similar to that of those treated during the day (66.7 ± 20.1 vs. 66.6 ± 24.6, P = 0.934). There were also no gender differences in treatments between day and night, as follows: 54.7% of the episodes in women occurred at night vs. 54.4% during the day (P = 0.804).
Figure 1.
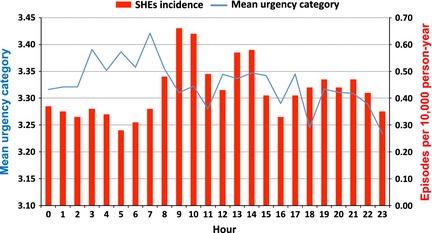
Incidence of severe hypoglycaemic episodes (SHEs) (n = 8683) and average category of urgency per hour. A computerized system based on the Manchester Triage System 16 was used to determine the urgency of events in the following five categories: non‐urgent (0), standard (1), urgent (2), very urgent (3) and immediate (4).
The seasonal distribution of SHEs requiring emergency service assistance and the mean urgency category are shown in Fig. 2.
Figure 2.
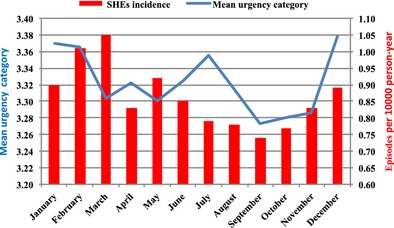
Seasonal incidence of severe hypoglycaemic episodes (SHEs) requiring emergency care (n = 8683) and average category of urgency. A computerized system based on the Manchester Triage System 16 was used to determine the urgency of events in the following five categories: non‐urgent (0), standard (1), urgent (2), very urgent (3) and immediate (4).
In 75% of the cases, hypoglycaemia was recognized by the patient (home blood glucose monitoring) or by family members. In the remaining cases, hypoglycaemia was confirmed during emergency assistance.
Emergency care and resource utilization
Eighty‐five per cent of the calls due to hypoglycaemia required a medical emergency team visit to the patient's home, and 13.83% were solved over the phone by the EPES coordinator centres. A small percentage (0.46%) of patients rejected assistance during the telephone calls, and 28 patients (0.32%) died before or while receiving emergency support.
After receiving domiciliary medical assistance, 1784 patients (21%) required a hospital referral. Nearly half (45%) were over 76 years of age, and only 4% were between 0 and 17 years of age. However, hospital referral was more frequent in the 0–17‐year‐old age group, where 42% of the episodes required referral to hospital emergency services (Table 1).
Among the hospital referrals, 49% were transported in an ambulance attended by healthcare professionals, and the remaining referrals used a transport ambulance without a medical team. In the 0–17‐year‐old age group, 77% of the cases required a healthcare professional‐aided transfer; for the remaining age groups, half required an ambulance‐assisted transfer.
Regarding the factors associated with a hospital referral, we found a higher probability for men [odds ratio (OR) = 1.30, 95% CI: 1.17–1.44, P ˂ 0.001] for the time of day between 08:00 and 15:59 (OR = 1.45, 95% CI: 1.27–1.65, P ˂ 0.001, reference time interval 0–8 h) and a significantly lower OR for all groups compared with the 0–17‐year‐old age group (reference). The lowest OR for referral was observed in the 31–45‐year‐old age group (OR 0.35, 95% CI: 0.25–0.49, P ˂ 0.001).
Costs
The total estimated emergency care costs in 2012 were €6 093 507, and the mean direct cost per episode was €702 ± 565. Episodes requiring referral to hospital emergency rooms (21%) represented 49% of the total expenditure. The components of the direct costs are reported in Table 2. The hospital emergency department cost represented ~ 30% (€208 ± 408) of the total costs. However, hospitalization costs for children < 17 years of age represented 40% of the total costs.
Table 2.
Costs per SHE
| All SHEs | Nocturnal SHEs (00.00 to 07.59) | SHEs requiring emergency hospital care | SHEs causing loss of consciousness | |
|---|---|---|---|---|
| Total direct costs (€ 1000s) | 6093 | 1527 | 2992 | 564 |
| Number of episodes | 8683 | 2287 | 1784 | 558 |
| Direct cost per individual (€) | 702 ± 565 | 668 ± 11 | 1677 ± 304 | 1012 ± 601 |
| Components of the direct cost (€)a | ||||
| Emergency care in place or residence (%) | 464 ± 273 (66) | 474 ± 252 (71) | 524 ± 311 (31) | 646 ± 264 (64) |
| Transfer | 30 ± 73 (4) | 24 ± 68 (4) | 143 ± 98 (9) | 38 ± 75 (4) |
| Emergency hospital care < 24 h | 208 ± 408 (30) | 170 ± 378 (25) | 1010 ± 0.0 (60) | 328 ± 473 (32) |
Additional information about the unit costs included in the direct cost components of SHEs is given in the Supporting Information (Table S1).
The costs varied according to patient age from €984 ± 759 for children aged < 17 years to €682 ± 549 for adults aged > 65 years. There were no differences in costs between diurnal and nocturnal hypoglycaemia. SHEs leading to a loss of consciousness were more costly (€1011 ± 601) than those that did not (€680 ± 555).
Discussion
We reported data on emergency medical services’ first response care for patients with hypoglycaemia and those patients’ clinical outcomes, need for hospitalization, resource utilization and healthcare costs in a large population (8.5 million people). The incidence of hypoglycaemic emergencies in this population (10.34 per 10 000 person‐years) obtained from our study may be valuable for epidemiological, clinical and administrative purposes.
The rate of SHEs requesting emergency service assistance for the population with diabetes was 810 per 10 000 person‐years. Considering that the incidence of SHEs in adults with diabetes is 300 per 10 000 person‐years 7, our data suggest that 30% require assistance from the emergency services. Structured training in self‐management could reduce both the rate of SHEs requiring emergency treatment and their associated costs 21.
The time distribution analysis of hypoglycaemia provides novel information from a clinical perspective. The frequency of telephone calls is lower during the night (26.45% of the total) and is higher between 09.00 and 11.00 in the morning. By contrast, the nocturnal calls for assistance were more urgent, on average, compared with those made during the remainder of the day. These results are consistent with those of Chico et al. 22, who observed unrecognized hypoglycaemia in 47–62% of people with diabetes, with 73.7% of all events occurring at night. These data underline the need to improve the prevention and detection of nocturnal hypoglycaemia.
The seasonal distribution of SHEs is also interesting because the frequency is unexpectedly lower during the summer (when people participate in more physical activity). By contrast, the mean urgency is higher during this season.
The increase in direct health costs is the largest contributor to the economic impact of diabetes, especially treatment‐related complications, such as those related to severe hypoglycaemia. In the USA, the costs of hospitalization or emergency care for those with diabetes accounted for 21.4% of the total expenditures for diabetes care 23. According to a recent study conducted in Spain and endorsed by the Spanish Society of Diabetes, the direct health costs of the disease comprised 8.2% of the health expenditures of the National Health System (€5809 million) in 2010. Expenses due to hypoglycaemia could increase the estimated costs to at least €12 million 24. In 2007, Guisasola et al. analysed cases of severe hypoglycaemia from a primary healthcare centre in Spain and estimated that each episode had a price of €384, of which €280 and €104 were related to ambulance costs and emergency care in the primary healthcare centre, respectively. Furthermore, the estimated mean admission cost was €2478 25. Our results indicate that emergency care costs are a major component of the total cost of hypoglycaemia care, with an estimated mean direct cost of €702 per episode.
Episodes requiring referral to hospital emergency rooms (21%) represented half of the total expenditure. The results of our study are in agreement with previous studies that demonstrated that most hypoglycaemic events could be treated at home by an emergency response team. Lammert et al. reported that between 23 and 25% of people with a severe hypoglycaemic episode in Germany and the UK, respectively, were referred to a hospital emergency care service 26. In Spain, Orozco‐Beltran et al. reported that ~ 30% were referred to hospitals 14. A retrospective analysis of emergency care in a population of nearly 400 000 inhabitants in the UK reported a higher rate of referrals (59%) to the hospital emergency service 27, but in that study, a glucose value < 3.5 mmol/l and parenteral therapy was an inclusion requirement.
A study in a smaller population in the UK recently described similar results on the incidence of SHEs requiring attendance by emergency medical services 28. However, Farmer et al. estimated a mean average cost per emergency call of €363, approximately half of our estimated costs. However, the economic evaluations incorporated different items in each study. The study by Farmer et al. did not cover some costs that were included in our study, such as the distance between transfers or the use of a helicopter (four of them were used in our study, leading to an additional cost of €17 280) (Table S1). However, they reported that 35% of people were transferred to the hospital compared with 21% in our results. This finding may be related to the fact that EPES includes doctor supervision in each response and could increase the proportion of SHEs that are solved at the scene.
We recognize several limitations in our study, including the retrospective design. Other limitations include the lack of information regarding data relevant to the risk of hypoglycaemia, such as the treatment of diabetes and the degree of glucose control.
In summary, hypoglycaemia requiring emergency treatment is common and is associated with a significant utilization of healthcare resources and financial impact. More effort is needed to reduce this serious complication, which is mainly related to diabetes treatment. In addition, our study indicates the need for well‐structured treatment and hospital transfer protocols that might improve the outcomes and reduce the hospitalization costs for those with hypoglycaemia.
Funding sources
None.
Competing interests
R. J. Barranco – None. F. Gomez‐Peralta – Advisory Panel: Sanofi, Novo Nordisk, Inc.; Research Support: Sanofi, Novo Nordisk, Inc., Boehringer Ingelheim Pharmaceuticals, Inc., Lilly; Speaker's Bureau: Sanofi, Novo Nordisk, Inc., Boehringer Ingelheim Pharmaceuticals, Inc., AstraZeneca Pharmaceuticals LP, Bristol‐Myers Squibb Company, Lilly. C. Abreu – Research Support: Sanofi, Novo Nordisk, Inc., Boehringer Ingelheim Pharmaceuticals, Inc., Lilly; Speaker's Bureau: Sanofi, Novo Nordisk, Inc., Boehringer Ingelheim Pharmaceuticals, Inc., AstraZeneca Pharmaceuticals LP, Bristol‐Myers Squibb Company. M. Delgado‐Rodríguez – None. R. Palomares – Research Support: Almirall, Lilly, MSD, Novartis, Novo Nordisk, Pfizer y Sanofi‐Aventis; Speaker's Bureau: Author: Astra‐Zeneca, Abbott, Almirall, Bayer, Boehringer, Bristol‐Myers, Esteve, Faes Farma, Ferrer, GSK, Lacer, Lifescan, Lilly, Menarini, Merck, MSD, Novartis, Novo Nordisk, Pfizer, Roche, Sanofi‐Aventis, Servier y Takeda. F. Romero – None. C. Morales– None. M. A. De La Cal – None. J. M. Garcia‐Almeida – Advisory Panel: Abbott, Nestle. F. J. Pasquel – None. G. E. Umpierrez – Advisory Panel: Merck, Novo Nordisk, Regeneron, and Boehringer Ingelheim Pharmaceuticals. Research Support to Emory University: Merck, Boehringer Ingelheim Pharmaceuticals, Inc., Novo Nordisk, Inc.
Supporting information
Table S1. Unit costs (2012) of resources, numbers and weights in the total cost of severe hypoglycaemia events requiring emergency care.
Acknowledgments
The authors acknowledge the editorial assistance of Ines Hernando, Cociente, Ltd, Dr Sergio Valdes, for providing Di@bet.es Study data from the population of Andalusia and Dr Manuel Aguilar, Director of the Andalusia Plan for Diabetes.
Author contributions
RJB researched the data and provided final approval of the manuscript. RJB and FG‐P wrote the manuscript, contributed to the data interpretation, and provided critical revisions. GEU contributed to the data interpretation and provided critical revisions. MD‐R contributed to the data interpretation and statistical analyses. All the other authors contributed to the discussion and reviewed the manuscript. RJB is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Diabet. Med. 32, 1520–1526 (2015)
Parts of this study were presented in poster form at the 74th Scientific Session of the American Diabetes Association, San Francisco, CA, June 13–17, 2014.
References
- 1. Soriguer F, Goday A, Bosch‐Comas A, Bordiú E, Calle‐Pascual A, Carmena R et al Prevalence of diabetes mellitus and impaired glucose regulation in Spain: the Di@bet.es Study. Diabetologia 2012; 55: 88–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Byass P, de Courten M, Graham WJ, Laflamme L, McCaw‐Binns A, Sankoh OA, et al Reflections on the global burden of disease 2010 estimates. PLoS Med 2013; 10: e1001477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bastida Lopez J, Boronat M, Moreno Oliva J, Schurer W. Costs, outcomes and challenges for diabetes care in Spain. Global Health 2013; 9: 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. McCoy RG, Van Houten HK, Ziegenfuss JY, Shah ND, Wermers RA, Smith SA. Increased mortality of patients with diabetes reporting severe hypoglycemia. Diabetes Care 2012; 35: 1897–1900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hsu P‐F, Sung S‐H, Cheng H‐M, Yeh J‐S, Liu W‐L, Chan W‐L, et al Association of clinical symptomatic hypoglycemia with cardiovascular events and total mortality in Type 2 diabetes: a nationwide population‐based study. Diabetes Care 2013; 36: 894–900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Donnelly LA, Morris AD, Frier BM, Ellis JD, Donnan PT, Durrant R, et al Frequency and predictors of hypoglycaemia in Type 1 and insulin‐treated Type 2 diabetes: a population‐based study. Diabet Med 2005; 22: 749–755. [DOI] [PubMed] [Google Scholar]
- 7. Bloomfield HE, Greer N, Newman D, MacDonald R, Carlyle M, Fitzgerald P, et al Predictors and Consequences of Severe Hypoglycemia in Adults with Diabetes ‐ A systematic review of the evidence. Washington, DC: Department of Veterans Affairs, 2012. [PubMed] [Google Scholar]
- 8. Brito‐Sanfiel M, Diago‐Cabezudo J, Calderon A. Economic impact of hypoglycemia on healthcare in Spain. Expert Rev Pharmacoecon Outcomes Res 2010; 10: 649–660. [DOI] [PubMed] [Google Scholar]
- 9. UK Hypoglycaemia Study Group . Risk of hypoglycaemia in types 1 and 2 diabetes: effects of treatment modalities and their duration. Diabetologia 2007; 50: 1140–1147. [DOI] [PubMed] [Google Scholar]
- 10. Seaquist ER, Anderson J, Childs B, Cryer P, Dagogo‐Jack S, Fish L, et al Hypoglycemia and diabetes: a report of a workgroup of the American Diabetes Association and The Endocrine Society. Diabetes Care 2013; 36: 1384–1395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Oliva J, Lobo F, Molina B, Monereo S. Direct health care costs of diabetic patients in Spain. Diabetes Care 2004; 27: 2616–2621. [DOI] [PubMed] [Google Scholar]
- 12. Geller AI, Shehab N, Lovegrove MC, Kegler SR, Weidenbach KN, Ryan GJ, et al National estimates of insulin‐related hypoglycemia and errors leading to emergency department visits and hospitalizations. JAMA Intern Med 2014; 174: 678–686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Budnitz DS, Maribeth C, Lovegrove NS, Richards CL. Emergency hospitalizations for adverse drug events in older Americans. N Engl J Med 2011; 365: 2002–2012. [DOI] [PubMed] [Google Scholar]
- 14. Orozco‐Beltran D, Mezquita‐Raya P, Ramirez de Arellano A, Galan M. Self‐reported frequency and impact of hypoglycemic events in Spain. Diabetes Ther 2014; 5: 155–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. National Institute of Statistics . Population and Housing Census. Population figures from January 1st, 2013. Available at http://www.ine.es Last accessed 24 January 2014.
- 16. Mackway‐Jones K. Emergency Triage, Manchester Triage Group. London: BMJ Publishing, 1997. [Google Scholar]
- 17. Ministry of Health, Social Policy and Equality .CIE‐9 MC. Coding, information and health statistics manual 2011. Madrid: Ministry of Health, Social Policy and Equality, 2011. [Google Scholar]
- 18. Valdés S, Garcia‐Torres F, Maldonado‐Araque C, Goday A, Calle‐Pascual A, Soriguer F, et al Prevalence of obesity, diabetes mellitus and other cardiovascular risk factors in Andalusia. Comparison of the national prevalence data. Di@bet.es Study. Rev Esp Cardiol 2014; 67: 442–448. [DOI] [PubMed] [Google Scholar]
- 19. BOJA num . 210 of the 27th of October of 2005. ORDER of the 14th of October of 2005, in which the public costs for healthcare services in Centers from the Andalusia Public Healthcare System are established. Available at http://www.juntadeandalucia.es/boja/2005/210/boletin.210.pdf Last accessed 10 November 2014.
- 20. Department of Health and Social Welfare of the Regional Government of Andalusia . EPES Annual Report 2012. Seville: Department of Health and Social Welfare of the Regional Government of Andalusia, 2012. Available at http://www.epes.es/anexos/publicacion/Memoria_2012_en/Memoria2012_en_web.pdf Last accessed 10 November 2014.
- 21. Elliott J, Jacques RM, Kruger J, Campbell MJ, Amiel SA, Mansell P, et al Substantial reductions in the number of diabetic ketoacidosis and severe hypoglycaemia episodes requiring emergency treatment lead to reduced costs after structured education in adults with Type 1 diabetes. Diabet Med 2014; 31: 847–853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Chico A, Vidal‐Rios P, Subirà M, Novials A. The continuous glucose monitoring system is useful for detecting unrecognized hypoglycemias in patients with Type 1 and Type 2 diabetes but is not better than frequent capillary glucose measurements for improving metabolic control. Diabetes Care 2003; 26: 1153–1157. [DOI] [PubMed] [Google Scholar]
- 23. American Diabetes Association . Economic costs of diabetes in the U.S. in 2012. Diabetes Care 2013; 36: 1033–1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Crespo C, Brosa M, Soria‐Juan A, Lopez‐Alba A, López‐Martínez N, Soria B. Direct costs of diabetes mellitus and its complications in Spain (SECCAID Study: Spain estimated Ciberdem‐Cabimer cost in Diabetes). Av en Diabetol 2013; 29: 182–189. [Google Scholar]
- 25. Guisasola F, Casal Llorente C, Rubio‐Terrés C. Cost analysis of Type 2 diabetes mellitus treatment with glargina insulin or detemir insulin in Spain. Rev Española Econ la Salud 2007; 6: 37–43. [Google Scholar]
- 26. Lammert M, Hammer M, Frier BM. Management of severe hypoglycaemia: cultural similarities, differences and resource consumption in three European countries. J Med Econ 2009; 12: 269–280. [DOI] [PubMed] [Google Scholar]
- 27. Graham PL, Wang J, Kelly P, Marsden A, Morrison W, Frier BM, et al Frequency of severe hypoglycemia requiring emergency treatment in Type 1 and Type 2 Diabetes. Diabetes Care 2003; 26: 1176–1180. [DOI] [PubMed] [Google Scholar]
- 28. Farmer AJ, Brockbank KJ, Keech ML, England EJ, Deakin CD. Incidence and costs of severe hypoglycaemia requiring attendance by the emergency medical services in South Central England. Diabet Med 2012; 29: 1447–1450. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Unit costs (2012) of resources, numbers and weights in the total cost of severe hypoglycaemia events requiring emergency care.


