SUMMARY
The likelihood of residual hearing preservation in cochlear implantation (CI) is related to surgical factors such as type of cochleostomy (trans-fenestral vs. promontorial), use of lubricants and protective drugs, and device-related factors such as shape, length and flexibility of the array. We investigated the impact of these factors on the hearing preservation rate in adults and children with conventional audiological indications to CI. Eighty-two children aged 1-9 years and 73 adults (16-79 years) received a CI in the right (59%) or left ear (41%). An anterior-inferior promontorial cochleostomy was performed in 143 ears (92%); a trans-fenestral approach was used in 12 (8%). A perimodiolar electrode was implanted in 144 ears (93%), and a straight electrode in the remaining 11 (7%). Overall, some post-operative hearing was retained in 39% of ears. The rate of preservation was higher at the low than at the high frequencies. When correlated with age, side of implant, implant model and type of cochleostomy, the mean threshold variations did not reach statistical significance for any of these variables. A slight trend in favour of better residual hearing preservation in children vs. adults was seen, especially at lower frequencies.
KEY WORDS: Cochlear implant, Residual hearing, Insertion technique, Cochleostomy, Array, Electrode
RIASSUNTO
La possibilità di conservazione dei residui uditivi è stata correlata a fattori chirurgici quali il tipo di cocleostomia (transfenestrale vs. promontoriale), l'uso di lubrificanti e farmaci otoprotettivi, e a fattori legati all'impianto quali la forma, la lunghezza e la flessibilità dell'elettrodo. Abbiamo studiato l'impatto di questi fattori sul tasso di conservazione dell'udito residuo in adulti e bambini con indicazioni audiologiche convenzionali all'impianto cocleare. Ottantadue bambini di età compresa tra 1 e 9 anni e 73 adulti (tra 16 e 79 anni) hanno ricevuto un IC monolaterale, nell'orecchio destro (59%) o sinistro (41%). Una cocleostomia promontoriale antero-inferiore è stata impiegata in 143 orecchi (92%), e un approccio a trans-fenestrale in 12 (8%). Un elettrodo perimodiolare è stato impiantato in 144 orecchi (93%); un elettrodo "straight" è stato utilizzato nei rimanenti 11 (7%). Complessivamente, un residuo uditivo post-operatorio è stato mantenuto nel 39% dei casi. Il tasso di conservazione è stato superiore alle frequenze gravi rispetto alle acute. Quando correlato all'età, al lato dell'impianto, al modello di elettrodo e al tipo di cocleostomia, le variazioni medie di soglia uditiva acustica non sono risultate statisticamente significative per alcuna di queste variabili. Un lieve trend in favore di una migliore conservazione uditiva si è osservato nei bambini rispetto agli adulti, specialmente alle frequenze gravi.
Introduction
Cochlear implantation has been always viewed as a destructive inner ear procedure. For a long time, surgeons believed that the patient's residual hearing would be compromised by surgical trauma, even when great care was taken, during the insertion of the electrode array, and patients were counselled accordingly.
At the end of the 1990s, some clinical studies hypothesised the feasibility of successful hearing preservation with cochlear implants, and thereafter many studies addressed the issue and confirmed the initial observations 1-9. This has radically changed the approach to CIs and widely expanded the audiological indications 6 10.
Previous "soft surgery" techniques 11 have been further refined 5 12-17, and specially designed electrodes have been developed by most producers for this purpose 18-20. The rate of preservation of hearing residuals in CI recipients is related mainly to surgical factors:
type and dimension of array (perimodiolar vs. straight; rounded vs. smoothened tip; short vs. regular; with or without stylet);
type of cochleostomy (round window or fenestral, promontorial);
type of insertion (soft surgery with advance-off-stylet [AOS] vs. standard);
use of lubricants or drugs in the cochlea (e.g. intrascalar corticosteroids) 21 22.
In addition, anatomical factors such as diameter, shape and length of scala tympani, audiological criteria (preoperative amount of residual pure tone hearing and speech perception abilities) 23 24 and demographic factors (age, side of implantation, gender) have been demonstrated to be relevant to hearing preservation in CIs. The objective of this study was to correlate some of these factors with the hearing preservation rate in our initial personal experience in adults and children with conventional indications for CI.
Materials and methods
This study is a retrospective analysis conducted on a group of adult and paediatric CI recipients who were operated upon by the first author at the Otorhinolaryngology Department of the University of Brescia, Italy, between January 2002 and July 2010, with surgical techniques aimed at preservation of residual hearing.
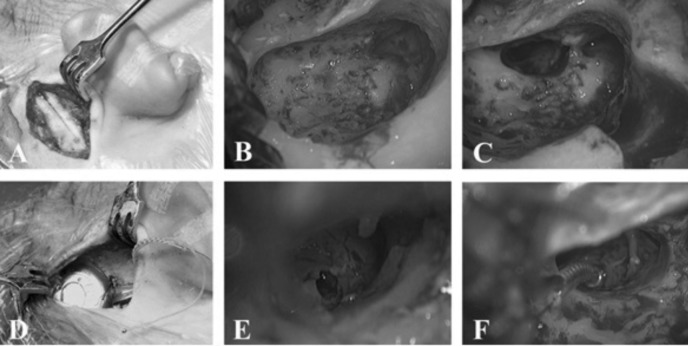
All patients underwent the same mini-invasive surgical approach under general anaesthesia. A linear incision about 3 cm long was made in the retroauricular skin, 1.5 cm from the sulcus, at or just behind the hairline (Fig. 1A). A subperiosteal pocket is dissected at 45° angle to the Frankfurt line, tailored to the dimensions of the receiver/stimulator of the implant that will be used. In situ trials with the silicone dummies provided by the factories helped to adjust the size of the pocket. A minimal mastoidectomy with sharp edges is drilled and the usual landmarks are identified (lateral semicircular canal, short process of incus); the posterior bony canal wall is thinned (Fig. 1B). An enlarged posterior tympanotomy is drilled between the chorda tympani and the mastoid segment of the Fallopian canal (Fig. 1C). The round window (RW) niche is exposed and, if necessary, its prominent anterior or superior bony lip is removed by a low-speed drill-out under constant irrigation. An appropriate well for the receiver/stimulator is drilled in the subperiosteal pocket and connected to the mastoidectomy with a semi-channel. The device is inserted in the pocket and fitted to the well (Fig. 1D). The ground electrode is recessed under the temporalis muscle. A promontorial cochleostomy (at the anterior-inferior edge of the RW niche) is achieved (Fig. 1E). When the RW exposure allows it, a trans-fenestral approach with direct piercing of the RW membrane is preferred.
Fig. 1.
Intraoperative images of the surgical procedure. A: retroauricolar incision and subperiosteal dissection; B: “minimal“ mastoidectomy; C: posterior tympanotomy; D: insertion of receiver/stimulator in subperiosteal pocket after drilling of a well; E: iuxtafenestral cochleostomy; F: insertion of electrode array.
Dexamethasone (4 mg/ml) solution is gently flushed into the middle ear cavity and the cochleostomy; hyaluronic acid gel is then placed to temporarily seal the latter in order to prevent bone dust or blood to enter the cochlear lumen. The electrode array is slowly inserted into the scala tympani, with the standard technique or the AOS technique described by Roland et al. 13 (Fig. 1F). The cochleostomy site is then sealed with autologous connective tissue, as well as the posterior tympanotomy, and the rest of the array is laid in the mastoidectomy cavity and the connecting semi-channel.
The study population was extracted from a pool of CI patients operated consecutively. Those who showed some residual hearing at any frequency before implantation were included; ears with no measurable threshold (anacusis) were excluded. Ears with middle or inner ear anomalies and cholesteatoma, which have a higher risk of cochlear damage or other complications during surgery 25 26, were also excluded from the analysis to make the cohort more homogeneous.
All patients suffered from severe to profound bilateral hearing loss, with less than 50% dissyllabic word recognition abilities in the best aided condition. Children showed poor aided speech perception abilities by age appropriate behavioural and electrophysiological measures. Thus, all patients were "regular" CI candidates by conventional standards of practice.
All patients were fitted with a postauricular speech processor.
In all patients the pre- vs. post-operative variations of air-conducted (AC) thresholds were recorded at each frequency (0.5, 1, 2, 4 kHz) in the ear to be implanted with an insert probe. Personnel exclusively dedicated to paediatric audiology performed all audiometric tests in children.
Post-operative thresholds were measured between one and two months after the operation to exclude a possible residual conductive component of hearing loss.
All pure tone tests were performed with a calibrated audiometer whose maximal output was 120 dB HL. For tabulation purposes, an arbitrary value of 125 dB HL was recorded in case of absent response at maximal signal intensity.
We considered the hearing residuals to be preserved when any measurable response was obtainable at low frequencies (0.5-1-2 kHz). In our study, we decided to extend the measurement to 4 kHz. Patient age, cause of hearing loss, side of implantation, cochleostomy site (fenestral vs. promontorial) and electrode model according to insertion technique were the categorical variables considered for statistical analysis.
The aims of the study were: 1) to evaluate the post-operative threshold variations at different frequencies; 2) to correlate the overall hearing preservation rates with the selected variables.
The long-term outcomes of preserved residual hearing and the correlation with speech perception outcomes is outside the scope of this paper and will be presented in a future study.
Statistical analysis was performed using the Mann-Whitney U-test to evaluate median differences of hearing deterioration between groups; the Kruskall-Wallis method was applied to test the significance of 3 different parameters; the chi-square test was used to compare categorical variables between groups. A p value < 0.05 was considered statistically significant. Results are expressed as medians and interquartile ranges (IQR).
Results
Pre-operatively, 155 patients met inclusion criteria and had a measurable hearing threshold at 500 Hz; at 1 kHz 6 of 155 had no sensation (4%), as well as 11 patients at 2 kHz (7%) and 19 at 4 kHz (12%).
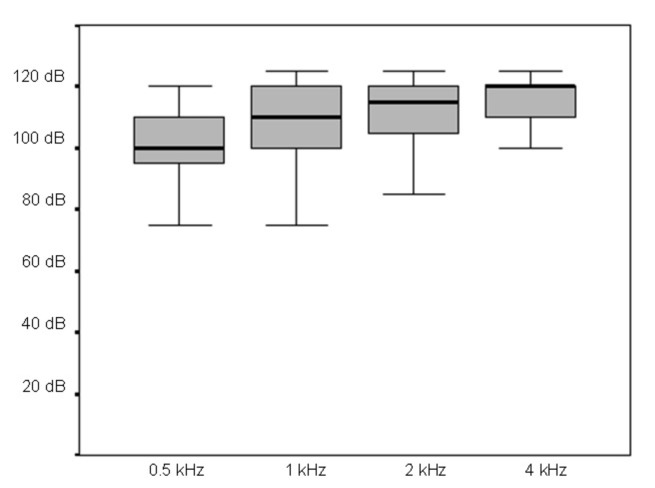
The median IQR, minimum and maximum pre-operative thresholds of the entire group of patients included in the study were 100 dB (95-110) at 0.5 kHz, 110 dB (100-120) at 1 kHz, 115 dB (105-120) at 2 kHz and 120 dB (110- 120) at 4 kHz, and are plotted in Figure 2.
Fig. 2.
Median, IQR, minimum and maximum pre-operative thresholds of the entire group of patients included in the study.
They were 82 children (53%) and 73 adults (47%). Children's ages at implantation ranged between 1 and 16 years (median 4, IQR 2-8 years); adults ranged between 18 and 79 years (median 53, IQR 39-65 years).
The cause of hearing loss was genetic in 33 ears (26 nonsyndromic, 7 syndromic), whereas in 53 ears is was related to diverse aetiologies (otosclerosis, 11; non-cholesteatomatous otitis media, 8; prenatal infections, 7; acoustic trauma, 6; meningitis, 6; sudden hearing loss, 5; Meniere disease, 4; other causes, 6). In 69 ears the cause of hearing loss remained undetermined.
The right ear was implanted in 92 cases (59%) and the left in 63 (41%).
An anterior-inferior promontorial cochleostomy was performed in 143 ears (92%); a trans-fenestral approach was preferred in 12 (8%). The implants had a straight electrode in 11 cases (7%) and a peri-modiolar electrode in 144 (93%); a standard technique of electrode insertion was used in 37 cases (24%), while the AOS technique was used in 118 (76%).
Overall, some residual hearing was preserved post-surgery in 60 of the 155 CI recipients (39%). Children and genetic hearing loss had a higher probability of retaining residual hearing (Tab. I). When matching these two variables, significant difference for aetiology was present only in children (probability of preserving residual hearing: idiopathic 46%, genetic 58%, other 10%; p = 0.03).
Table I.
Comparison of retained residuals after surgery between analysed variables.
| Variable | p value | |
|---|---|---|
| Age | 0.04 | |
| Children | 46% (38/82) | |
| Adults | 30% (22/73) | |
| Aetiology | 0.007 | |
| Genetic | 54% (18/33) | |
| Non-genetic | 23% (12/53) | |
| Idiopathic | 43% (30/69) | |
| Side | 0.4 | |
| Right | 36% (33/92) | |
| Left | 43% (27/63) | |
| Cochleostomy | 0.7 | |
| Promontorial | 33% (4/12) | |
| Round window | 39% (56/143) | |
| Electrode | 0.2 | |
| Perimodiolar with AOS | 35% (41/118) | |
| Perimodiolar | 50% (13/26) | |
| Straight | 54% (6/11) |
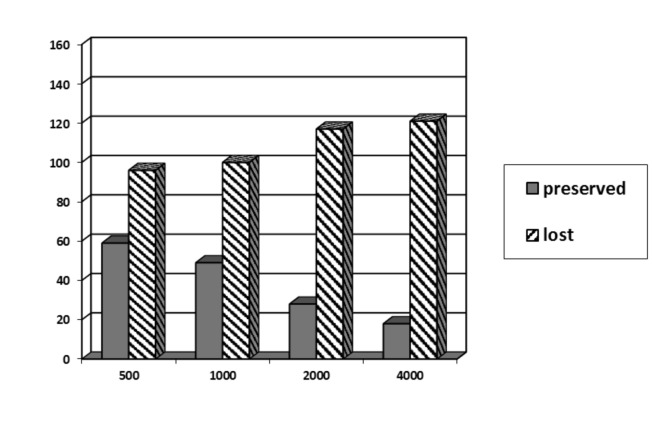
The rates of hearing threshold preservation at different frequencies in the whole sample is shown in Figure 3. It is evident that the preservation rate progressively decreased from the low to the high frequencies.
Fig. 3.
Rate of threshold preservation at different frequencies for the entire sample.
The median (IQR) difference between the pre- and postoperative hearing threshold (without the implant) was 12.5 dB (6.25-20): it was 15 dB (10-30) at 0.5 kHz, 10 dB (5-20) at 1 kHz, 10 dB (5-20) at 2 kHz and 5 dB (5-15) at 4 kHz.
The median threshold variation values were correlated with age (Tab. II), aetiology of hearing loss (Tab. III), side of implant (Tab. IV), type of cochleostomy (Tab. V) and electrode model according to insertion technique (Tab. VI). None of the abovementioned variables showed a statistically significant difference in terms of residual hearing preservation scores at any of the investigated frequencies. A slight trend towards lesser hearing deterioration for some variables was seen, but this did not reach statistical significance in any case; furthermore, the size of some of the subgroups is very limited, hindering comparison.
Table II.
Correlation of differences between post- and pre-operative hearing thresholds and age of the subject at implantation (Median, IQR).
| Frequency | Children (n = 82) | Adults (n = 73) | p value |
|---|---|---|---|
| Average | 12 (6-20) | 12 (6-20) | 0.6 |
| 0.5 kHz | 15 (5-25) | 20 (10-30) | 0.2 |
| 1 kHz | 15 (5-25) | 10 (5-20) | 0.6 |
| 2 kHz | 10 (5-20) | 10 (5-15) | 1 |
| 4 kHz | 5 (5-20) | 5 (5-10) | 0.5 |
Table III.
Correlation of differences between post- and pre-operative hearing thresholds and aetiology. (Median, IQR).
| Frequency | Genetic (n = 33) | Other (n = 53) | Idiopathic (n = 69) | p value |
|---|---|---|---|---|
| Average | 11 (6-16) | 11 (5-21) | 14 (6-21) | 0.5 |
| 0.5 kHz | 15 (5-25) | 15 (5-25) | 20 (10-30) | 0.4 |
| 1 kHz | 15 (5-15) | 10 (5-20) | 15 (5-25) | 0.3 |
| 2 kHz | 5 (5-15) | 10 (5-20) | 10 (5-20) | 0.5 |
| 4 kHz | 5 (5-10) | 5 (5-20) | 5 (5-15) | 0.3 |
Table IV.
Correlation of differences between post- and pre operative hearing thresholds and side of implantation (Median, IQR).
| Frequency | Right (n = 92) | Left (n = 63) | p value |
|---|---|---|---|
| Average | 11 (6-19) | 14 (6-20) | 0.6 |
| 0.5 kHz | 15 (5-27) | 20 (10-30) | 0.9 |
| 1 kHz | 10 (5-20) | 15 (5-20) | 0.3 |
| 2 kHz | 5 (5-15) | 15 (5-20) | 0.3 |
| 4 kHz | 5 (5-15) | 5 (5-15) | 0.7 |
Table V.
Correlation of differences between post- and pre-operative hearing thresholds and type of cochleostomy (Median, IQR).
| Frequency | Fenestral (n=12) | Promontorial (n=143) | p value |
|---|---|---|---|
| Average | 11 (7-18) | 12 (6-20) | 1 |
| 0.5 kHz | 20 (12-27) | 15 (7-30) | 0.5 |
| 1 kHz | 10 (5-20) | 10 (5-20) | 0.7 |
| 2 kHz | 5 (0-22) | 10 (5-20) | 0.5 |
| 4 kHz | 5 (0-12) | 5 (5-15) | 0.3 |
Table VI.
Correlation of differences between post- and pre-operative hearing thresholds and electrode model according to insertion technique (Median, IQR).
| Frequency | Straight (n=11) | Perimodiolar (n=26) | Perimodiolar AOS (n=118) | p value |
|---|---|---|---|---|
| Average | 14 (7-17) | 12 (7-24) | 11 (6-20) | 0.7 |
| 0.5 kHz | 20 (15-27) | 20 (10-30) | 15 (5-25) | 0.6 |
| 1 kHz | 5 (0-12) | 15 (5-20) | 12 (5-20) | 0.1 |
| 2 kHz | 15 (2-15) | 10 (5-15) | 10 (5-20) | 1 |
| 4 kHz | 5 (5-17) | 5 (5-20) | 5 (5-15) | 0.7 |
The post-operative pure tone thresholds obtained with the CI in free-field were satisfactory for all patients. The median (IQR) scores are reported in Table VII. At each frequency, the thresholds were slightly better in recipients who retained residual hearing: the difference was not significant (Tab. VII).
Table VII.
Correlation of differences in free-field hearing thresholds with CI between lost or preserved residual hearing (Median, IQR).
| Frequency | Loss | Preserved | p value |
|---|---|---|---|
| Average | 34 (27-40) | 30 (26-41) | 0.3 |
| 0.5 kHz | 35 (30-40) | 30 (25-40) | 0.2 |
| 1 kHz | 35 (30-40) | 30 (25-40) | 0.1 |
| 2 kHz | 30 (25-40) | 30 (25-40) | 0.3 |
| 4 kHz | 35 (25-40) | 30 (25-40) | 0.8 |
Discussion
Reasons for preserved hearing are several-fold: the conservation of the anatomical integrity of the cochlear duct, i.e. spiral lamina and ligament, organ of Corti and stria vascularis, favours the modulation of activity of spiral ganglion cells, supports the survival of neural elements and allows integration of spectral and temporal features of the stimulus, through a better CI-neural tissue interface 27-30. This leads to improved perceptive performances, possible delivery of protective drugs, rescuing agents and/or regenerating factors, and opens new scenarios for possible future intracochlear interventions.
Reviewing the literature, it is evident that the loss of residual hearing is mainly related to insertion of the electrode array 31 32. The inevitable surgical trauma due to the electrode insertion can be minimised by strictly adhering to the rules of "soft surgery" proposed by Lenhardt in 1993 11. Following other experiences in the literature 13 14 16 33, these rules have been further refined and we strictly apply them, as described in the previous section, even to patients who are not candidates for hearing preservation. Notwithstanding, the meticulous application of soft surgery techniques in all patients, our overall residual hearing preservation results did not exceed 40% of CI recipients.
In the literature a high variability of results is reported: hearing preservation scores range between 18% and 100% 2 5-9 31 34-36; 60% of the variability is due to surgical factors 37.
According to Roland et al. 13, the cochlear damage that can result from placement of the array can be condensed in 2 large groups of aetiopathogenetic factors: 1) trauma related to the cochleostomy, including 1a - complete or partial loss of perilymph fluid, 1b - bone dust penetration into the scala tympani and delayed neo-osteogenesis, or 1c - reactive fibrous tissue formation around the array; 2) Insertion trauma: 2a - damage to the organ of Corti through breakdown of basilar membrane or 2b - osseous spiral lamina or 2c lateral wall.
Other phenomena that can lead to a delayed loss of residual hearing are: 1) related with surgical trauma: 1a - middle ear lesion (effusion, TM perforation, ossicular disruption); 1b - cochleostomy (drilling, perilymph suction, ionic homeostasis disruption, bone dust); 1c - electrode insertion (perilymph outflow, direct inner ear damage); 2) reactive (delayed): 2a - inner ear toxicity (blood, irrigation fluids, bone dust, device material); 2b - primary disease progression; 2c - inflammation (infection, fibrosis, effusion).
In our group of patients there was the opportunity to analyse the impact of several variables on residual hearing preservation after cochlear implantation.
Age at implantation
There are few reports on hearing preservation surgery in children. Skarzinski et al. 38 initially reported the feasibility of conservation of low frequency hearing in 8 of 9 children implanted for partial, down-sloping sensorineural hearing loss. The preservation was total in 44.5% and partial in 55.5%. In our experience, children seem to benefit more than adults from hearing preservation techniques (Tab. I). To our knowledge, this effect has not been reproduced in other studies 39.
Aetiology of deafness
Some considerations about the aetiology of deafness and hearing preservation have been reported in the literature 39. Congenital hearing loss has better hearing preservation outcomes and is attributed to the possibility that subjects with congenital hearing loss have more stable auditory systems that can tolerate the CI procedure better 39. Our experience can support this hypothesis for genetic hearing loss in children due to the small subgroup of adults with this type of deafness.
Side of implant
Even if our results are below the level of statistical significance, the left ear seems to be advantaged, but in terms of residual preservation scores right ear had lower median variations. This might be related to the right-handedness of surgeons or to a more favourable anatomy, although these remain only speculative hypotheses. We could not find significant data in the literature supporting or refuting our findings; no definitive conclusions can be drawn on this subject, and further studies are required.
Type of cochleostomy
Some authors claim the superiority of the trans-fenestral (RW) approach in terms of hearing preservation 39 40. In the study by Skarzynski et al. 16 hearing preservation was achieved in the majority of their implanted patients through RW insertion; on that basis, the authors proposed to proceed to a CI even in cases with partial deafness, i.e. with profound sensorineural hearing loss limited to the frequencies equal or higher than 2000 Hz.
Conversely, recent experimental studies in guinea pigs 17 has shown that the type of cochleostomy is only marginally relevant to inner ear damage, while it is tightly related with the features of the selected array. Berrettini et al. 41 were able to preserve residual hearing in 81.8% of patients implanted with a perimodiolar electrode using the AOS technique by an anterior inferior cochleostomy. They observed that this combination of device and technique reduced the trauma to the lateral wall of the cochlea during electrode insertion.
In agreement with our results, the majority of the clinical studies report no significant differences between the two types of cochleostomies 42-44. A systematic review on the topic 45 confirmed that the percentage of patients with postoperative complete hearing preservation ranged from 0% to 40% for the cochleostomy group and from 13% to 59% in the RW group. Unfortunately, no doubleblind prospective studies have directly compared the two cochleostomy approaches, which deserve to be addressed more specifically.
Electrode array model and insertion technique
Shortened arrays have been designed with the purpose of preserving the low-frequency residual hearing by limiting the penetration of the electrode to the basal and midportion of the middle cochlear turn.
An initial FDA trial with a hybrid 10 mm electrode with 87 patients showed that over time 30% of patients partially or totally lost their low-frequency residual hearing 18. Preliminary outcomes of a European multicentre clinical trial 46 demonstrated the ability to preserve residual hearing within 15dB in 68% of subjects implanted with a 16 mm long hybrid electrode, with results that were stable over time.
Another multicentre study 47 investigated a different type of array; similar to the 16 mm long hybrid model, this electrode showed a 68% hearing preservation score, with 16% of patients unfortunately losing residual hearing over 6 months after the CI.
Perimodiolar CIs have been related to a higher risk of intracochlear traumatisation compared to free-fitting arrays 15. A perimodiolar model has been proven to be traumatic to inner ear structures when inserted through the RW in 50% of patients in the case series in Melbourne and 33% of those in Dallas 48. However, some clinical studies offer evidence for atraumatic implantation and preservation of residual hearing even with perimodiolar arrays 7 49 50, provided that promontorial cochleostomy is selected. In agreement with our present findings, no significant differences were found by Di Nardo et al. 51 in terms of hearing preservation between electrode arrays bearing a stylet or not.
In a study comparing two electrodes designed for hearing preservation purposes (slim straight electrode vs. hybrid electrode), in a large cohort of consecutive CI patients with substantial residuals at the low frequencies, Jurawitz et al. 52 found that the median hearing loss of patients with the first model (n = 97) was 10 dB at initial fitting and 15 dB after 24 months. For those with the second electrode (n = 100), the median loss was 14.4-dB at activation and 30 dB at 2 years. The first model recipients exhibited greater threshold stability and lesser hearing loss over time than those with the second model.
The main criticism to the use of shorter electrodes regards their inability to stimulate sufficient extension of the acoustic nerve endings toward the cochlear apex in the case the residual hearing is lost after implantation.
However, in the most recent meta-analysis on the subject 32 the use of longer length electrode arrays with deeper insertion or contoured vs. straight-electrode arrays was not found to endanger hearing preservation.
To date, no single array design achieves all three objectives of deep insertion, proximity to modiolus and atraumatic introduction of the array. Long, flexible and progressively thinner electrodes (from base to apex) should be the aim of production of new devices by manufacturers 35 36.
Conclusions
In our experience with 155 "conventional" CI recipients (82 children and 73 adults), who were all operated upon by a refined soft surgery technique, the overall likelihood of preservation of residual hearing was 39%. The threshold conservation rate was higher at lower than at higher frequencies.
When correlated with age, aetiology of deafness, side of implant, type of cochleostomy, implant model and insertion technique, a significant rate of hearing preservation was observed for children with genetic hearing loss, whereas the median differences in threshold variation did not reach statistical significance for any of these variables. A slight trend in favour of better residual median hearing preservation for children, left side, perimodiolar electrodes inserted with AOS through fenestral cochleostomy was observed. The post-operative pure tone thresholds obtained with the CI in free-field were slightly better for individuals with preserved residuals. Due to the limited power of the study, no definitive conclusions can be drawn, and further studies are required.
Acknowledgments
The authors wish to thank Dr. Chiara Campovecchi, MD for the initial data collection, Dr. Sara Pasini, PhD for adult patient testing, and Dr. Mariagrazia Barezzani, MD for useful clinical advice.
Footnotes
Disclosure: This study was partially funded by a grant from Associazione Progetto Udire Onlus, Brescia, Italy.
References
- 1.Hodges AV, Schloffman J, Balkany T. Conservation of residual hearing with cochlear implantation. Am J Otol. 1997;18:179–183. [PubMed] [Google Scholar]
- 2.Kiefer J, Gstoettner W, Baumgartner W, et al. Conservation of low-frequency hearing in cochlear implantation. Acta Otolaryngol. 2004;124:272–280. doi: 10.1080/00016480310000755a. [DOI] [PubMed] [Google Scholar]
- 3.Ilberg C, Kiefer J, Tillein J, et al. Electric-acoustic stimulation of the auditory system. New technology for severe hearing loss. ORL J Otorhinolaryngol Relat Spec. 1999;61:334–340. doi: 10.1159/000027695. [DOI] [PubMed] [Google Scholar]
- 4.Gantz BJ, Turner CW. Combining acoustic and electrical hearing. Laryngoscope. 2003;113:1726–1730. doi: 10.1097/00005537-200310000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Gstoettner W, Kiefer J, Baumgartner WD, et al. Hearing preservation in cochlear implantation for electric acoustic stimulation. Acta Otolaryngol. 2004;124:348–352. doi: 10.1080/00016480410016432. [DOI] [PubMed] [Google Scholar]
- 6.James C, Albegger K, Battmer R, et al. Preservation of residual hearing with cochlear implantation: how and why. Acta Otolaryngol. 2005;125:481–491. doi: 10.1080/00016480510026197. [DOI] [PubMed] [Google Scholar]
- 7.Fraysse B, Macías AR, Sterkers O, et al. Residual hearing conservation and electroacoustic stimulation with the Nucleus 24 contour advance cochlear implant. Otol Neurotol. 2006;27:624–633. doi: 10.1097/01.mao.0000226289.04048.0f. [DOI] [PubMed] [Google Scholar]
- 8.Balkany TJ, Connell SS, Hodges AV, et al. Conservation of residual acoustic hearing after cochlear implantation. Otol Neurotol. 2006;27:1083–1088. doi: 10.1097/01.mao.0000244355.34577.85. [DOI] [PubMed] [Google Scholar]
- 9.Garcia-Ibanez L, Macias AR, Morera C, et al. An evaluation of the preservation of residual hearing with the Nucleus Contour Advance electrode. Acta Otolaryngol. 2009;129:651–654. doi: 10.1080/00016480802369278. [DOI] [PubMed] [Google Scholar]
- 10.Dorman MF, Wilson BF. The design and function of cochlear implants. Am Sci. 2004;92:436–443. [Google Scholar]
- 11.Lehnhardt E. [[Intracochlear placement of cochlear implant electrodes in soft surgery technique]]. HNO. 1993;41:356–359. [PubMed] [Google Scholar]
- 12.Gantz BJ, Turner C, Gfeller KE, et al. Preservation of hearing in cochlear implant surgery: advantages of combined electrical and acoustical speech processing. Laryngoscope. 2005;115:796–802. doi: 10.1097/01.MLG.0000157695.07536.D2. [DOI] [PubMed] [Google Scholar]
- 13.Roland PS, Gstöttner W, Adunka O. Method for hearing preservation in cochlear implant surgery. Oper Tech Otolaryngol Head Neck Surg. 2005;16:93–100. [Google Scholar]
- 14.Wright CG, Roland PS. Temporal bone microdissection for anatomic study of cochlear implant electrodes. Cochl Impl Int. 2005;6:159–168. doi: 10.1179/cim.2005.6.4.159. [DOI] [PubMed] [Google Scholar]
- 15.Adunka OF, Pillsbury HC, Kiefer J. Combining perimodiolar electrode placement and atraumatic insertion properties in cochlear implantation – fact or fantasy? Acta Otolaryngol. 2006;126:475–482. doi: 10.1080/00016480500437393. [DOI] [PubMed] [Google Scholar]
- 16.Skarzynski H, Lorens A, Piotrowska A, et al. Preservation of low frequency hearing in partial deafness cochlear implantation (PDCI) using the round window surgical approach. Acta Otolaryngol. 2007;127:41–48. doi: 10.1080/00016480500488917. [DOI] [PubMed] [Google Scholar]
- 17.Giordano P, Hatzopoulos S, Giarbini N, et al. A soft-surgery approach to minimize hearing damage caused by the insertion of a cochlear implant electrode: a guinea pig animal model. Otol Neurotol. 2014;35:1440–1445. doi: 10.1097/MAO.0000000000000440. [DOI] [PubMed] [Google Scholar]
- 18.Gantz BJ, Hansen MR, Turner CW, et al. Hybrid 10 clinical trial: preliminary results. Audiol Neurootol. 2009;14(Suppl 1):32–38. doi: 10.1159/000206493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lenarz T, StoverT, Buechner A, et al. Hearing conservation surgery using the Hybrid-L electrode: results from the first clinical trial at the Medical University of Hannover. Audiol Neurotol. 2009;14:22–31. doi: 10.1159/000206492. [DOI] [PubMed] [Google Scholar]
- 20.Jolly C, Garnham C, Mirzadeh H, et al. Electrode features for hearing preservation and drug delivery strategies. Adv Otorhinolaryngol. 2010;67:28–42. doi: 10.1159/000262594. [DOI] [PubMed] [Google Scholar]
- 21.Chang A, Eastwood H, Sly D, et al. Factors influencing the efficacy of round window dexamethasone protection of residual hearing post-cochlear implant surgery. Hear Res. 2009;255:67–72. doi: 10.1016/j.heares.2009.05.010. [DOI] [PubMed] [Google Scholar]
- 22.Barriat S, Poirrier A, Malgrange B, et al. Hearing preservation in cochlear implantation and drug treatment. Adv Otorhinolaryngol. 2010;67:6–13. doi: 10.1159/000262592. [DOI] [PubMed] [Google Scholar]
- 23.Turner CW, Gantz BJ, Vidal C, et al. Speech recognition in noise for cochlear implant listeners: benefits of residual acoustic hearing. J Acoust Soc Am. 2004;115:1729–1735. doi: 10.1121/1.1687425. [DOI] [PubMed] [Google Scholar]
- 24.Pelliccia P, Venail F, Bonafé A, et al. Cochlea size variability and implications in clinical practice. Acta Otorhinolaryngol Ital. 2014;34:42–49. [PMC free article] [PubMed] [Google Scholar]
- 25.Berrettini S, Forli F, Vito A, et al. Cochlear implant in incomplete partition type I. Acta Otorhinolaryngol Ital. 2013;33:56–62. [PMC free article] [PubMed] [Google Scholar]
- 26.Vincenti V, Pasanisi E, Bacciu A, et al. Cochlear implantation in chronic otitis media and previous middle ear surgery: 20 years of experience. Acta Otorhinolaryngol Ital. 2014;34:272–277. [PMC free article] [PubMed] [Google Scholar]
- 27.Ching TYC. Acoustic cues for consonant perception with combined acoustic and electric hearing in children. Semin Hear. 2011;32:32–41. [Google Scholar]
- 28.Yoon YS, Li Y, Fu QJ. Speech recognition and acoustic features in combined electric and acoustic stimulation. J Speech Lang Hear Res. 2012;55:105–124. doi: 10.1044/1092-4388(2011/10-0325). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mosca F, Grassia R, Leone CA. Longitudinal variations in fitting parameters for adult cochlear implant recipients. Acta Otorhinolaryngol Ital. 2014;34:111–116. [PMC free article] [PubMed] [Google Scholar]
- 30.D'Elia A, Bartoli R, Giagnotti F, et al. The role of hearing preservation on electrical thresholds and speech performances in cochlear implantation. Otol Neurotol. 2012;33:343–347. doi: 10.1097/MAO.0b013e3182487dbb. [DOI] [PubMed] [Google Scholar]
- 31.Miranda PC, Sampaio AL, Lopes RA, et al. Hearing preservation in cochlear implant surgery. Int J Otolaryngol. 2014;2014:468515–468515. doi: 10.1155/2014/468515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Maria PL, Gluth MB, Yuan Y, et al. Hearing preservation surgery for cochlear implantation: a meta-analysis. Otol Neurotol. 2014;35:e256–e269. doi: 10.1097/MAO.0000000000000561. [DOI] [PubMed] [Google Scholar]
- 33.Kiefer J, Pok M, Adunka O, et al. Combined electric and acoustic stimulation of the auditory system: result of a clinical study. Audiol Neurotol. 2005;10:134–144. doi: 10.1159/000084023. [DOI] [PubMed] [Google Scholar]
- 34.Mowry SE, Woodson E, Gantz BJ. New frontiers in cochlear implantation: acoustic plus electric hearing, hearing preservation, and more. Otolaryngol Clin North Am. 2012;45:187–203. doi: 10.1016/j.otc.2011.09.001. [DOI] [PubMed] [Google Scholar]
- 35.Abel KM, Dunn CC, Sladen DP, et al. Hearing preservation among patients undergoing cochlear implantation. Otol Neurotol. 2015;36:416–421. doi: 10.1097/MAO.0000000000000703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Brown KD, Melton MF, Shonfield H, et al. Preserved lowfrequency hearing following 20-mm cochlear implantation. Otol Neurotol. 2015;36:240–243. doi: 10.1097/MAO.0000000000000684. [DOI] [PubMed] [Google Scholar]
- 37.Verbist BM, Skinner MW, Cohen LT, et al. Consensus panel on a cochlear coordinate system applicable in histologic, physiologic, and radiologic studies of the human cochlea. Otol Neurotol. 2010;31:722–730. doi: 10.1097/MAO.0b013e3181d279e0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Skarzynski H, Lorens A, Piotrowska A, et al. Partial deafness cochlear implantation in children. Int J Pediatr Otorhinolaryngol. 2007;71:1407–1413. doi: 10.1016/j.ijporl.2007.05.014. [DOI] [PubMed] [Google Scholar]
- 39. Causon A, Verschuur C, Newman TA. A retrospective analysis of the contribution of reported factors in cochlear implantation on hearing preservation outcomes. Otol Neurotol. 2015;36:1137–1145. doi: 10.1097/MAO.0000000000000753. [DOI] [PubMed] [Google Scholar]
- 40.Adunka OF, Buss E, Clark MS, et al. Effect of preoperative residual hearing on speech perception after cochlear implantation. Laryngoscope. 2008;118:2044–2049. doi: 10.1097/MLG.0b013e3181820900. [DOI] [PubMed] [Google Scholar]
- 41.Berrettini S, Forli F, Passetti S. Preservation of residual hearing following cochlear implantation: comparison between three surgical techniques. J Laryngol Otol. 2008;122:246–252. doi: 10.1017/S0022215107000254. [DOI] [PubMed] [Google Scholar]
- 42.Briggs RJ, Tykocinski M, Xu J, et al. Comparison of round window and cochleostomy approaches with a prototype hearing preservation electrode. Audiol Neurotol. 2006;11:42–48. doi: 10.1159/000095613. [DOI] [PubMed] [Google Scholar]
- 43.Gudis DA, Montes M, Douglas C, et al. The round window: is it the ''cochleostomy'' of choice? Experience in 130 consecutive cochlear implants. Otol Neurotol. 2012;33:1497–1501. doi: 10.1097/MAO.0b013e31826a52c7. [DOI] [PubMed] [Google Scholar]
- 44.Sun CH, Hsu CJ, Chen PR, et al. Residual hearing preservation after cochlear implantation via round window or cochleostomy approach. Laryngoscope. 2015;125:1715–1719. doi: 10.1002/lary.25122. [DOI] [PubMed] [Google Scholar]
- 45.Havenith S, Lammers MJ, Tange RA, et al. Hearing preservation surgery: cochleostomy or round window approach? A systematic review. Otol Neurotol. 2013;34:667–674. doi: 10.1097/MAO.0b013e318288643e. [DOI] [PubMed] [Google Scholar]
- 46.Lenarz T, James C, Cuda D, et al. European multi-centre study of the Nucleus Hybrid L24 cochlear implant. Int J Audiol. 2013;52:838–848. doi: 10.3109/14992027.2013.802032. [DOI] [PubMed] [Google Scholar]
- 47.Gstoettner W, Heyning P, O'Connor AF, et al. Electric acoustic stimulation of the auditory system: results of a multi- centre investigation. Acta Otolaryngol. 2008;128:968–975. doi: 10.1080/00016480701805471. [DOI] [PubMed] [Google Scholar]
- 48.Souter MA, Briggs RJ, Wright CG, et al. Round window insertion of pre-curved perimodiolar electrode arrays: how successful is it? Otol Neurotol. 2011;32:58–63. doi: 10.1097/MAO.0b013e3182009f52. [DOI] [PubMed] [Google Scholar]
- 49.Nardo W, Cantore I, Cianfrone F, et al. Residual hearing thresholds in cochlear implantation and reimplantation. Audiol Neurootol. 2007;12:165–169. doi: 10.1159/000099019. [DOI] [PubMed] [Google Scholar]
- 50.Rebscher SJ, Hetherington A, Bonham B, et al. Considerations for design of future cochlear implant electrode arrays: electrode array stiffness, size, and depth of insertion. J Rehabil Res Dev. 2008;45:731–747. doi: 10.1682/jrrd.2007.08.0119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Nardo W, Cantore I, Melillo P, et al. Residual hearing in cochlear implant patients. Eur Arch Otorhinolaryngol. 2007;264:855–860. doi: 10.1007/s00405-007-0270-8. [DOI] [PubMed] [Google Scholar]
- 52.Jurawitz MC, Büchner A, Harpel T, et al. Hearing preservation outcomes with different cochlear implant electrodes: Nucleus® Hybrid™-L24 and Nucleus Freedom™ CI422. Audiol Neurotol. 2014;19:293–309. doi: 10.1159/000360601. [DOI] [PubMed] [Google Scholar]