Abstract
Context:
ST-segment elevations in two or more contiguous leads or new left bundle branch block (LBBB) on electrocardiography (ECG) in a patient with acute onset chest pain are diagnostic criteria for acute myocardial infarction (AMI) and generally warrant urgent coronary angiography and cardiac catheterization. However, the significance of new right bundle branch block (RBBB) without other acute ECG changes is unclear and is currently not considered a criterion.
Case Report:
We present a patient with chest pain, positive biomarkers of myocardial necrosis and isolated new right bundle block on ECG. He was diagnosed with AMI but did not undergo urgent reperfusion therapy in the absence of ST-segment elevations or new LBBB. However, angiography ultimately demonstrated complete coronary occlusion.
Conclusion:
The established criteria for emergent catheterization may prove to be more sensitive with the inclusion of the presence of new RBBB on ECG.
Keywords: Cardiac catheterization, coronary angiography, myocardial infarction, percutaneous coronary intervention, right bundle branch block
Introduction
ST-segment elevations in two or more contiguous leads or new left bundle branch block (LBBB) on electrocardiography (ECG) in a patient with acute onset chest pain are criteria for acute myocardial infarction (AMI) and generally warrant urgent coronary angiography and cardiac catheterization.[1] While it has been demonstrated that the co-existence of bundle branch block and AMI confers a worse prognosis than AMI without a conduction abnormality,[2,3] the significance of new right bundle branch block (RBBB) without other acute ECG changes is unclear and currently not a part of the diagnostic criteria. We present a patient with chest pain and isolated new right bundle block who was ultimately diagnosed with an AMI with complete coronary occlusion, but did not undergo timely reperfusion therapy because he did not meet current guidelines for emergent intervention.
Case Presentation
The patient was a 67-year-old Caucasian male with a history of hypertension and tobacco abuse, who presented with the complaint of right-sided chest pain that he experienced while mowing his lawn earlier in the day. He described the pain as dull, rated 7/10, and radiating to his right shoulder and jaw. He denied associated palpitations, dyspnea, diaphoresis, dizziness, or nausea. With rest, the pain improved but did not resolve. He took aspirin 325 mg once prior to the presentation.
On initial evaluation, he reported the pain was 4/10, which subsequently resolved with sublingual nitroglycerin. He was noted to have elevated cardiac enzymes (troponin 3.18, creatine kinase (CK)-MB 29.1), and a new RBBB on ECG [Figure 1]. He was given a clopidogrel loading dose, metoprolol, started on an intravenous infusion of heparin, and admitted for further monitoring and a coronary angiogram and cardiac catheterization. His cardiac enzymes continued to rise and peaked 6 h after admission (troponin 6.39, CK-MB 33.3). In addition, he required the administration of intravenous nitroglycerin for recurrent chest pain.
Figure 1.
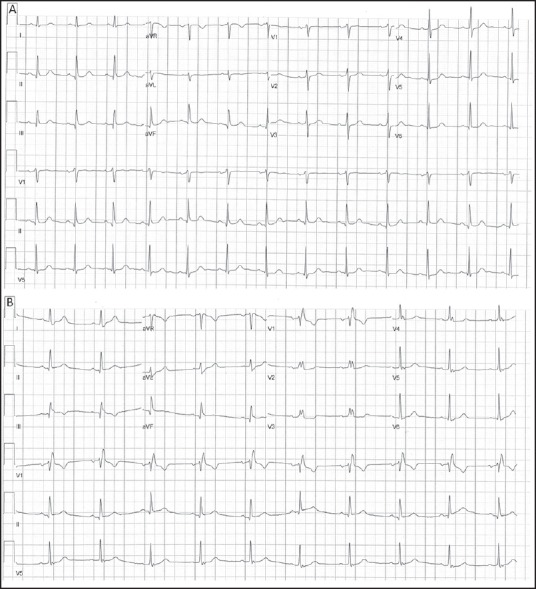
Electrocardiography (a) Prior to presentation and (b) On presentation, the latter demonstrating an isolated new right bundle branch block
On hospital day 2, he underwent cardiac catheterization and coronary angiography, where he was found to have 100% proximal occlusion of his right coronary [Figure 2]. Two drug-eluting stents were placed, with subsequent TIMI 3 flow.
Figure 2.
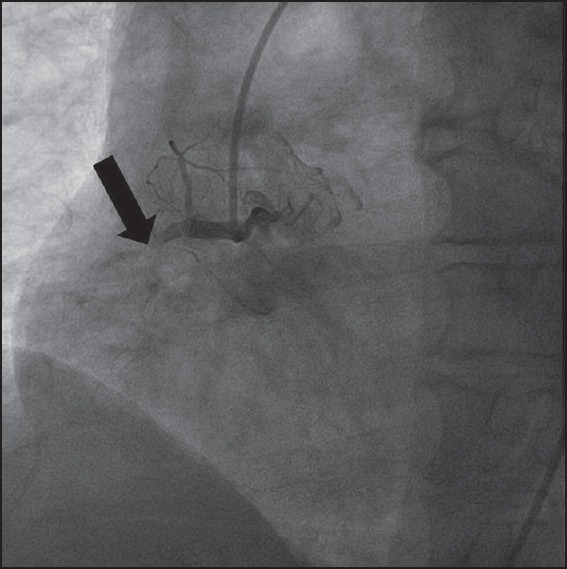
The right coronary artery is completely occluded in the proximal segment (arrow)
On hospital day 3, the patient remained asymptomatic and was discharged with lisinopril, metoprolol, atorvastatin, aspirin and clopidogrel. He was encouraged to stop smoking and instructed on a heart-healthy diet and exercise program.
When seen 2 months later in outpatient cardiology clinic, the patient reported compliance with his medications and denied any recurrence of symptoms.
Discussion
Patients who present with acute-onset chest pain need to be rapidly triaged in order to maximally preserve viable myocardium and limit mortality in the cases of coronary artery plaque rupture and subsequent occlusion.[4] At this time, the ECG criteria to determine which patients require emergent cardiac catheterization and possible emergent percutaneous intervention include ST-segment elevations in two or more contiguous leads or new LBBB.[1] The reason for the latter is because, with an LBBB, ST-segments and T-waves tend to be shifted in discordant directions, which may either mimic or mask an ST-segment elevation. This does not hold true, however, in RBBB, and so this has not been traditionally used as a criterion for emergent cardiac catheterization. However, RBBB may in fact mask subtle ST-segment elevations in the anterior leads (V1-4) due to secondary repolarization changes resulting in the depression of ST-segments after the rSR′ deflection. This may falsely depress the ST-segments below the threshold recommended to formally diagnose an ST-segment elevation. In fact, a retrospective analysis by Widimsky et al. of patients presenting with AMI found that 47% of ECGs with RBBB failed to demonstrate ST-segment elevations.[5] Of those patients, 67% were subsequently found to have TIMI flow 0-2.
Beyond the diagnostic limitations due to RBBB, the HERO-2 trial demonstrated that the co-existence of RBBB and acute anterior MI confers a 3-4 times higher 30-day mortality than anterior MI without a conduction abnormality.[2] Results also indicate that it is the width of the QRS complexes, and not the degree of ST-segment elevations that correlate with 30-day mortality.[6]
With regard to chronicity of RBBB, data indicate that new onset (or presumed new, when prior ECG data were unavailable) should be treated as a more emergent finding than old. Data by Widimsky et al. demonstrate that new RBBB is associated with a higher mean Killip class (1.88% vs. 1.45%), percentage of TIMI flow 0 (55% vs. 34.9%), and in-hospital mortality (18.8% vs. 6.4%) than if RBBB existed prior to the AMI.[5]
Since the establishment of coronary reperfusion therapy, mortality rates from AMI have declined and continued to improve as guidelines for emergent coronary angiography and cardiac catheterization have been implemented. However, improved outcomes require timely triage of patients with AMI from suspected complete coronary occlusion, which, in part, relies on the sensitivity of ECG guidelines. While new LBBB is an established surrogate for ST-elevation on ECG, in a retrospective study, 51.7% of patients presenting with AMI and new RBBB had TIMI flow 0 in the infarct-related artery, statistically more than the 39.4% of patients with new LBBB.[5] In addition, in-hospital mortality was 18.8% for those with new RBBB, significantly higher than 13.2% for those with new LBBB. There is a growing wealth of data on the significance of new RBBB in AMI including the resulting challenges in diagnosis by ECG and associated increased mortality. The established criteria for emergent catheterization may prove to be more sensitive and result in improved mortality with the inclusion of the presence of new RBBB on ECG.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.American College of Emergency Physicians; Society for Cardiovascular Angiography and Interventions. O’Gara PT, Kushner FG, Ascheim DD, Casey DE, Jr, Chung MK, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;61:e78–140. doi: 10.1016/j.jacc.2012.11.019. [DOI] [PubMed] [Google Scholar]
- 2.Wong CK, Stewart RA, Gao W, French JK, Raffel C. White HD Prognostic differences between different types of bundle branch block during the early phase of acute myocardial infarction: Insights from the Hirulog and Early Reperfusion or Occlusion HERO-2 trial. Eur Heart J. 2006;27:21–8. doi: 10.1093/eurheartj/ehi622. [DOI] [PubMed] [Google Scholar]
- 3.Sgarbossa EB, Pinski SL, Topol EJ, Califf RM, Barbagelata A, Goodman SG, et al. Acute myocardial infarction and complete bundle branch block at hospital admission: Clinical characteristics and outcome in the thrombolytic era. GUSTO-I Investigators. Global Utilization of Streptokinase and t-PA [tissue-type plasminogen activator] for Occluded Coronary Arteries. J Am Coll Cardiol. 1998;31:105–10. doi: 10.1016/s0735-1097(97)00446-4. [DOI] [PubMed] [Google Scholar]
- 4.Cannon CP, Gibson CM, Lambrew CT, Shoultz DA, Levy D, French WJ, et al. Relationship of symptom-onset-to-balloon time and door-to-balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction. JAMA. 2000;283:2941–7. doi: 10.1001/jama.283.22.2941. [DOI] [PubMed] [Google Scholar]
- 5.Widimsky P, Rohác F, Stásek J, Kala P, Rokyta R, Kuzmanov B, et al. Primary angioplasty in acute myocardial infarction with right bundle branch block: Should new onset right bundle branch block be added to future guidelines as an indication for reperfusion therapy? Eur Heart J. 2012;33:86–95. doi: 10.1093/eurheartj/ehr291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wong CK, Gao W, Stewart RA, van Pelt N, French JK, Aylward PE, et al. Risk stratification of patients with acute anterior myocardial infarction and right bundle-branch block: Importance of QRS duration and early ST-segment resolution after fibrinolytic therapy. Circulation. 2006;114:783–9. doi: 10.1161/CIRCULATIONAHA.106.639039. [DOI] [PubMed] [Google Scholar]


