Abstract
Background:
Programs for improving health status of patients with illness related to pain, such as headache, are often still in their infancy. Mindfulness-based stress reduction (MBSR) is a new psychotherapy that appears to be effective in treating chronic pain and stress. This study evaluated efficacy of MBSR in treatment of perceived stress and mental health of client who has tension headache.
Materials and Methods:
This study is a randomized clinical trial. Sixty patients with tension type headache according to the International Headache Classification Subcommittee were randomly assigned to the Treatment As Usual (TAU) group or experimental group (MBSR). The MBSR group received eight weekly classmates with 12-min sessions. The sessions were based on MBSR protocol. The Brief Symptom Inventory (BSI) and Perceived Stress Scale (PSS) were administered in the pre- and posttreatment period and at 3 months follow-up for both the groups.
Results:
The mean of total score of the BSI (global severity index; GSI) in MBSR group was 1.63 ± 0.56 before the intervention that was significantly reduced to 0.73 ± 0.46 and 0.93 ± 0.34 after the intervention and at the follow-up sessions, respectively (P < 0.001). In addition, the MBSR group showed lower scores in perceived stress in comparison with the control group at posttest evaluation. The mean of perceived stress before the intervention was 16.96 ± 2.53 and was changed to 12.7 ± 2.69 and 13.5 ± 2.33 after the intervention and at the follow-up sessions, respectively (P < 0.001). On the other hand, the mean of GSI in the TAU group was 1.77 ± 0.50 at pretest that was significantly reduced to 1.59 ± 0.52 and 1.78 ± 0.47 at posttest and follow-up, respectively (P < 0.001). Also, the mean of perceived stress in the TAU group at pretest was 15.9 ± 2.86 and that was changed to 16.13 ± 2.44 and 15.76 ± 2.22 at posttest and follow-up, respectively (P < 0.001).
Conclusion:
MBSR could reduce stress and improve general mental health in patients with tension headache.
Keywords: Mental health, tension headache, mindfulness-based stress reduction (MBSR), perceived stress, treatment as usual (TAU)
INTRODUCTION
Tension headache constitutes 90% of total headaches. About 3% of the population are suffering from chronic tension headache.[1] Tension headaches are often associated with lower quality of life and high levels of psychological discomforts.[2] In recent years, several meta-analyses evaluating the established pain treatments used today have shown that medical treatments, which may be effective in acute pain, are not effective with chronic pain and may, in fact, be causing further problems. Most of the pain treatments are designed for and useful for acute pain but if used in the long run may create more problems such as substance abuse and avoidance of important activities.[3] A common element in most of the pain treatments is that they emphasize on either avoiding pain or fighting to reduce pain. The pain in tension headache can be intolerable. Painkillers and pain management strategies can increase intolerance and sensitivity to pain. Therefore, the treatments that increase acceptance and tolerance to pain, especially chronic pain, are effective. Mindfulness-based stress reduction (MBSR) is a new psychotherapy that appears to be effective in improving physical performance and psychological well-being in patients with chronic pain.[4,5,6,7,8] In the past two decades, Kabat-Zinn et al. in the US successfully used mindfulness for the relief of pain and illness related to pain.[9] Recent studies on acceptance-based methods, such as mindfulness, show improved performance in patients with chronic pain. Mindfulness modulates the pain using nonelaborative awareness of thoughts, feelings and sensations, and an emotionally distanced relationship with internal and external experience.[10] Studies found that MBSR program can significantly alleviate medical illness related to chronic pains such as fibromyalgia, rheumatoid arthritis, chronic musculoskeletal pain, chronic low back pain, and multiple sclerosis.[7,11,12,13] MBSR has significant changes in pain intensity, anxiety, depression, somatic complaints, well-being, adaptation, quality of sleep, fatigue, and physical functioning.[6,14,15,16,17] But the programs for improving health status of patients with illness related to pain, such as tension headache, are often still in their infancy. Therefore, the study was conducted to assess the effects of MBSR on perceived stress and general mental health in patients with tension headache.
MATERIALS AND METHODS
This randomized controlled clinical trial was performed in 2012 in Shahid Beheshti Hospital in Kashan City. The Research Ethics Committee of the Kashan University of Medical Sciences approved this study (IRCT No: 2014061618106N1). The participants of the study included adults with tension headache who were referred by the psychiatrists and neurologists in Kashan. The inclusion criteria were as follows: Having tension headache according to the International Headache Classification Subcommittee, willing to participate in the study, not having a medical diagnosis of organic brain disorder or psychotic disorder, and not having a history of psychological treatment during the preceding 6 months. The patients who did not complete the intervention and missed more than two sessions were excluded from the study. The participants, who signed an informed consent form, completed the measures as a pretest. For estimating the sample size, we referred to another study in which changes in mean of scores of fatigue was 62 ± 9.5 in the pretreatment period and 54.5 ± 11.5 in the posttreatment period.[18] Then, by utilizing the sample size calculation, 33 participants (with attrition risk) in each group with α = 0.95 and 1 – β = 0.9 were segregated. After sample size calculation, 66 patients with tension headache were selected via convenient sampling according to the inclusion criteria. Then, the patients were called and invited to participate in the study. If a patient agreed to participate, then he/she was invited to attend the study-briefing session and if not another patient was selected similarly. Then using a random number table, they were assigned either to the experimental group (MBSR) or to the control group that treated as usual. Finally, 3 patients were excluded from each group and 60 patients were included (30 patients in each group). The TAU group was treated only by antidepressant medication and clinical management. The MBSR group received MBSR training in addition to TAU. The patients in MBSR group were trained for 8 weeks by a clinical psychologist with PhD degree. The Brief Symptom Inventory (BSI) and Perceived Stress Scale (PSS) were administered before the first treatment session in the MBSR group, after the eighth session (posttest), and 3 months after the test (follow-up) in both groups. The TAU group was invited to Shahid Beheshti Hospital to fill out the questionnaires. Figure 1 shows a Consolidated Standards of Reporting Trials (CONSORT) diagram depicting the flow of study participants.
Figure 1.
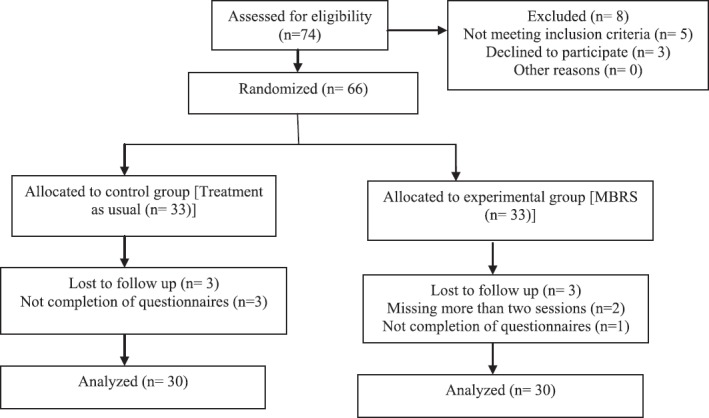
CONSORT diagram depicting flow of study participants
Intervention
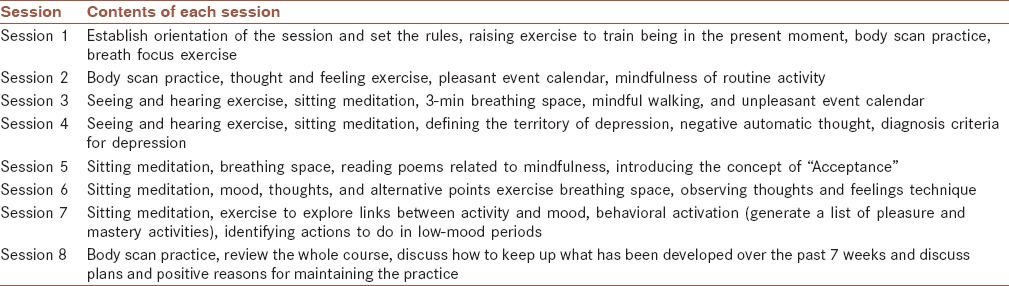
The intervention group (MBSR) was trained in Shahid Beheshti Hospital. The eight weekly sessions (120 min) were held according to the standard MBSR protocol as developed by Kabat-Zinn.[11] Additional sessions were held for the participants who had missed one or two sessions. At the end of the training and 3 months later (follow-up), both MBSR and TAU groups were invited to Shahid Beheshti Hospital (the place of MBSR trial) and were instructed to complete the questionnaires. During the MBSR sessions, the participants were trained to be aware of their thoughts, feelings, and physical sensations nonjudgmentally. Mindfulness exercises are taught as two forms of meditation practices — formal and informal. Formal type exercises include trained sitting meditation, body scan, and mindful yoga. In informal meditation, attention and awareness are focused not only on daily activities, but also on thoughts, feelings, and physical sensation even they are problematic and painful. The overall content of the sessions were mentioned in Table 1.
Table 1.
Agendas for sessions of mindfulness-based stress reduction
Measurement tools
International Headache Classification Subcommittee diary scale for headache
Headache was measured by diary scale for headache.[19] The patients were asked to record the pain severity diary on a 0-10 rating scale. Absence of pain and the most intense disabling headache were characterized by 0 and 10, respectively. The mean of headache severity in a week was calculated by dividing the sum of the severity scores by 7. Moreover, the mean of headache severity in a month was calculated by dividing the sum of the severity scores by 30. The minimum and maximum scores of headache severity were 0 and 10, respectively. Headache diary was given to five patients and a neurologist and a psychiatrist confirmed the content validity of the instrument.[20] The reliability coefficient of Persian version of this scale was calculated as 0.88.[20]
Brief symptom inventory (BSI)
Psychological symptoms were assessed with the BSI.[21] The inventory consist 53 items and 9 subscales that assess psychological symptoms. Each item scores between 0 and 4 (for example: I have nausea or upset in my stomach). BSI has a global severity index (GSI) achieved a total score of 53 items. The reliability of the test has reported a score of 0.89.[22] In our study, GSI test–retest estimate was .90 based on a sample of 60 patients with tension headache who completed the BSI.
Perceived stress scale (PSS)
Perceived stress was assessed using the PSS,[21,23] a 10-item scale that assesses the degree of uncontrollable and unpredictable situations of life during the past month (for example: Felt that you were unable to control the important things in your life?). Respondents report the prevalence of an item within the last month on a 5-point scale, ranging from 0 (never) to 4 (very often). Scoring is completed by reverse scoring of four positively worded items[4,5,7,8] and summing all item scores. The scale scores range from 0-40. Higher scores indicate higher levels of stress. It assumes that people depending on their coping resources evaluate level of threatening or challenging events. A higher score indicates a greater degree of perceived stress. Adequate test–retest reliability and convergent and discriminate validity have also been reported.[19] In our study, Cronbach's alpha coefficients for assessing internal consistency of this scale were calculated to be 0.88.
The repeated measures analysis of variance was performed to compare the MBSR and TAU groups on measures of perceived stress and GSI at pretreatment, posttreatment, and 3-month follow-up. Also, Chi-square test was used to compare the demographics in the two groups. P value less than 0.05 was considered significant in all tests.
RESULTS
Among 66 subjects, 2 participants from the MBSR group were excluded because of missing more than 2 sessions. Also, three participants were excluded because of did not complete the questionnaires in post-test or follow-up who one of them were from MBSR group and three participants from TAU group. Table 2 showed demographic characteristics of the subjects and results of the randomization check. The results of t-test for differences between the MBSR and TAU groups in age variable and Chi-square test in other variables showed that there was no significant difference between demographic variables in two groups and the subjects were randomly assigned to two groups.
Table 2.
Demographic characteristics of the subjectsa,b
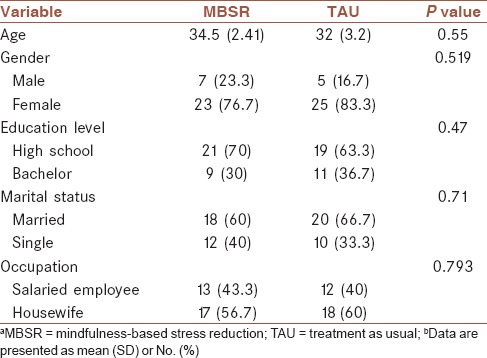
Table 3 provides the mean scores and standard deviations of the dependent variables (perceived stress and GSI) and comparison of outcome measures at pretreatment period, posttreatment period, and 3-month follow-up.
Table 3.
Means, standard deviations, and comparison of outcome measures at pretreatment, posttreatment, and follow-up stages in the MBSR and TAU groupsa,b
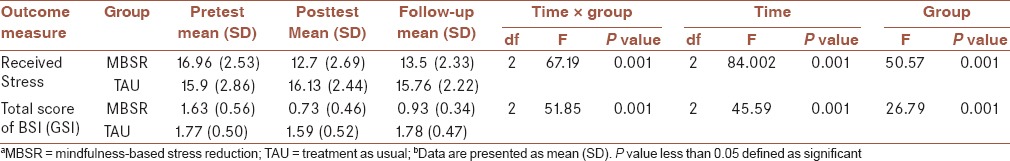
Table 3 shows the more reduction in received stress and GSI in the intervention group (MBSR) compared to TAU group, while the reduction in received stress and GSI were not observed in the TAU group. The results revealed the significant effect of time and interaction between time and type of treatment on the changes of scores (P < 0.001).
Figures 2 and 3 present mean received stress and GSI scores for MBSR and TAU groups at posttest and follow-up stages.
Figure 2.
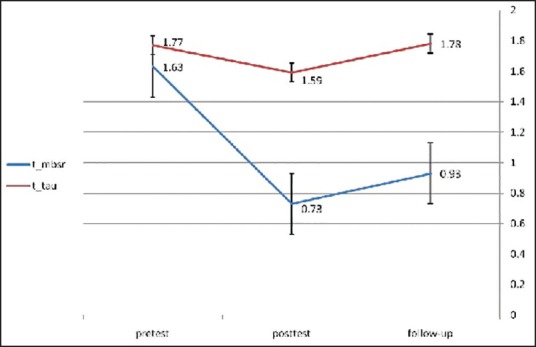
CONSORT diagram depicting flow of study participants
Figure 3.
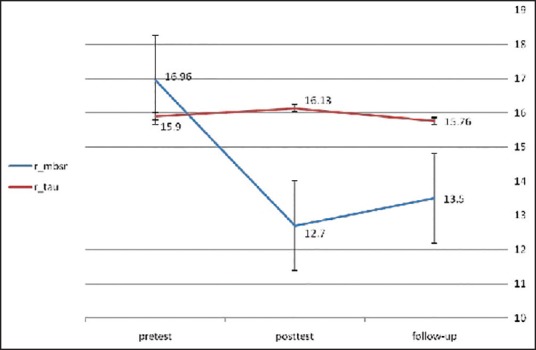
Mean of perceived stress in MBSR and control groups in pretest, posttest, and follow-up
DISCUSSION
This study compared efficacy of MBSR and Treatment As Usual (TAU) in perceived stress and mental health of patients with tension headache. Although MBSR is recognized as an effective treatment for stress symptoms and pain, there is a need to examine its efficacy for the treatment of mental health problems in patients with tension headache, which is one of the common complaints in the population.
The findings of our study demonstrate enhanced general mental health in the GSI index of BSI. In some study, significant improvements by MBSR intervention were reported on all indexes of the 36-item Short Form Health Survey (SF-36).[20,24] Studies showed significant reduction in psychological problems in the Symptom Checklist-90-Revised (SCL-90-R) subscale such as anxiety and depression by MBSR after intervention and 1-year follow-up.[5] Reibel et al. showed MBSR in patients with chronic pain reported a decrease in medical symptoms such as anxiety, depression, and pain.[5] It has been shown that tension headache and anxiety are accompanied with deficits in controlled cognitive processing such as sustained attention and working memory.[25] Negative emotions may amplify suffering associated with pain perception.
MBSR implements the following mechanisms to improve the patient's mental status: First, mindfulness leads to increased awareness for what is happening in each moment, with an accepting attitude, without getting caught up in habitual thoughts, emotions, and behavior patterns. The increased awareness then gives rise to new ways to respond and cope in relation to oneself and the world around.[3] Mindfulness establishes a sense of self that is greater than one's thoughts, feelings, and bodily sensation such as pain. Mindfulness exercises, learned clients develop an “observer–self”. With this ability, they can observe their thoughts and feelings in a nonreactive and nonjudgmental way that previously avoided, that previously avoided thoughts and feelings be observed in a nonreactive and nonjudgmental way. The clients learn to notice thoughts without necessarily acting on them, being controlled by them, or believing them.[3]
Second, mindfulness helps the client develop persistence in taking steps in valued directions that are important to them. Most clients with chronic pain want to become pain free rather than living the vital lives of their choice. But the MBSR program trained them to engage in valued action despite the the pain. Studies have shown attention and emotional reaction to pain has an important role in becoming persistent the pain.[26] Emotional and cognitive components can modulate attention to pain and worry about it that could intensify pain and disrupt the patients activities.[27,28]
Third, findings from some studies indicate that MBSR can alter the function of the brain that is responsible for affect regulation and the areas that govern how we react to stressful impulses, and this in turn may normalize body functions such as breathing, heart rate, and immune function.[29,30] Mindfulness practice reduces reactivity to distressing thoughts and feelings that comorbid and strengthen pain perception.[31] Also mindfulness may lessen psychophysiological activation related to stress and mood dysfunction by strengthening positive reappraisal and emotion regulation skills.[32]
The strength of this study is the use of a new effective psychotherapy in reducing the stress on a complaint that is less studied, but it is a common medical problem. The implications of our study are using a simple psychotherapy that does not make too much cognitive demand and is readily usable as a coping skill for the patient with tension headache. Therefore, the health-care professionals related to this complaint and the patient will be able to use this treatment. Also, MBSR will change the patient's lifestyle who would be exacerbated by his/her problem. The main limitation of this study was the lack of comparison between MBSR and the gold standard psychotherapies such as cognitive behavior therapy (CBT). It is suggested that future studies need to compare the efficacy of MBSR and other traditional and newer cognitive behavioral therapies in patients with tension headache.
CONCLUSION
Our study supports the hypothesis that patients suffering from tension headache can enhance their general mental health by participating in the MBSR program. In summary, the results of the present study suggest that MBSR can reduce pain-related anxiety and interference in daily activities in the short term. The unique features of mindfulness exercises are easy training and no need to complex cognitive abilities.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
AUTHOR'S CONTRIBUTION
AO contributed in the conception of the work, conducting the study, and agreed for all aspects of the work. FZ contributed in the conception of the work, revising the draft, approval of the final version of the manuscript and agreed for all aspects of the work.
Acknowledgments
Authors are grateful to the staff of Shahid Beheshti Hospital and participants. Authors also express their gratitude to Kabat-Zinn from the Center for Mindfulness (CFM) at the University of Massachusetts who graciously provided electronic copies of the MBSR guidelines.
REFERENCES
- 1.Trkanjec Z, Aleksic-Shihabi A. Tension-type headaches. Acta Med Croatica. 2008;62:205–10. [PubMed] [Google Scholar]
- 2.Zirke N, Seydel C, Szczepek AJ, Olze H, Haupt H, Mazurek B. Psychological comorbidity in patients with chronic tinnitus: Analysis and comparison with chronic pain, asthma or atopic dermatitis patients. Qual Life Res. 2013;22:263–72. doi: 10.1007/s11136-012-0156-0. [DOI] [PubMed] [Google Scholar]
- 3.Dionne F, Blais MC, Monestes JL. Acceptance and commitment therapy in the treatment of chronic pain. Sante Ment Que. 2013;38:131–52. doi: 10.7202/1023993ar. [DOI] [PubMed] [Google Scholar]
- 4.Cathcart S, Galatis N, Immink M, Proeve M, Petkov J. Brief mindfulness-based therapy for chronic tension-type headache: A randomized controlled pilot study. Behav Cogn Psychother. 2013;42:1–15. doi: 10.1017/S1352465813000234. [DOI] [PubMed] [Google Scholar]
- 5.Reibel DK, Greeson JM, Brainard GC, Rosenzweig S. Mindfulness-based stress reduction and health-related quality of life in a heterogeneous patient population. Gen Hosp Psychiatry. 2001;23:183–92. doi: 10.1016/s0163-8343(01)00149-9. [DOI] [PubMed] [Google Scholar]
- 6.Grossman P, Niemann L, Schmidt S, Walach H. Mindfulness-based stress reduction and health benefits. A meta-analysis. J Psychosom Res. 2004;57:35–43. doi: 10.1016/S0022-3999(03)00573-7. [DOI] [PubMed] [Google Scholar]
- 7.Rosenzweig S, Greeson JM, Reibel DK, Green JS, Jasser SA, Beasley D. Mindfulness-based stress reduction for chronic pain conditions: Variation in treatment outcomes and role of home meditation practice. J Psychosom Res. 2010;68:29–36. doi: 10.1016/j.jpsychores.2009.03.010. [DOI] [PubMed] [Google Scholar]
- 8.Kerrigan D, Johnson K, Stewart M, Magyari T, Hutton N, Ellen JM, et al. Perceptions, experiences, and shifts in perspective occurring among urban youth participating in a mindfulness-based stress reduction program. Complement Ther Clin Pract. 2011;17:96–101. doi: 10.1016/j.ctcp.2010.08.003. [DOI] [PubMed] [Google Scholar]
- 9.Kabat-Zinn J. New York: Dell Publishing; 1990. Full Catastrophe Living; p. 185. [Google Scholar]
- 10.Hayes AM, Feldman G. Clarifying the construct of mindfulness in the context of emotion regulation and the process of change in therapy. Clin Psychol-Sci Pr. 2004:255–62. [Google Scholar]
- 11.Schmidt S, Grossman P, Schwarzer B, Jena S, Naumann J, Walach H. Treating fibromyalgia with mindfulness-based stress reduction: Results from a 3-armed randomized controlled trial. Pain. 2011;152:361–9. doi: 10.1016/j.pain.2010.10.043. [DOI] [PubMed] [Google Scholar]
- 12.Pradhan EK, Baumgarten M, Langenberg P, Handwerger B, Gilpin AK, Magyari T, et al. Effect of Mindfulness-Based Stress Reduction in rheumatoid arthritis patients. Arthritis Rheum. 2007;57:1134–42. doi: 10.1002/art.23010. [DOI] [PubMed] [Google Scholar]
- 13.Cramer H, Haller H, Lauche R, Dobos G. Mindfulness-based stress reduction for low back pain. A systematic review. BMC Complement Altern Med. 2012;12:162. doi: 10.1186/1472-6882-12-162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bazarko D, Cate RA, Azocar F, Kreitzer MJ. The impact of an innovative mindfulness-based stress reduction program on the health and well-being of nurses employed in a corporate setting. J Workplace Behav Health. 2013;28:107–33. doi: 10.1080/15555240.2013.779518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Carlson LE, Garland SN. Impact of mindfulness-based stress reduction (MBSR) on sleep, mood, stress and fatigue symptoms in cancer outpatients. Int J Behav Med. 2005;12:278–85. doi: 10.1207/s15327558ijbm1204_9. [DOI] [PubMed] [Google Scholar]
- 16.Lengacher CA, Kip KE, Barta M, Post-White J, Jacobsen PB, Groer M, et al. A pilot study evaluating the effect of mindfulness-based stress reduction on psychological status, physical status, salivary cortisol, and interleukin-6 among advanced-stage cancer patients and their caregivers. J Holist Nurs. 2012;30:170–85. doi: 10.1177/0898010111435949. [DOI] [PubMed] [Google Scholar]
- 17.Simpson J, Mapel T. An investigation into the health benefits of mindfulness-based stress reduction (MBSR) for people living with a range of chronic physical illnesses in New Zealand. N Z Med J. 2011;124:68–75. [PubMed] [Google Scholar]
- 18.Omidi A, Mohammadi A, Zargar F, Akbari H. Efficacy of mindfulness-based stress reduction on mood States of veterans with post-traumatic stress disorder. Arch Trauma Res. 2013;1:151–4. doi: 10.5812/atr.8226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–96. [PubMed] [Google Scholar]
- 20.Roth B, Robbins D. Mindfulness-based stress reduction and health-related quality of life: Findings from a bilingual inner-city patient population. Psychosom Med. 2004;66:113–23. doi: 10.1097/01.psy.0000097337.00754.09. [DOI] [PubMed] [Google Scholar]
- 21.Brown KW, Ryan RM. The benefits of being present: Mindfulness and its role in psychological well-being. J Pers Soc Psychol. 2003;84:822–48. doi: 10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- 22.Astin JA, Shapiro SL, Lee RA, Shapiro DH., Jr The construct of control in mind-body medicine: Implications for healthcare. Altern Ther Health Med. 1999;5:42–7. [PubMed] [Google Scholar]
- 23.Cohen S, Williamson G. Perceived stress in a probability sample of the United States. In: Spacapan S, Oskamp S, editors. The Social Psychology of Health. Newbury Park, CA: Sage; 1988. p. 185. [Google Scholar]
- 24.Geary C, Rosenthal SL. Sustained impact of MBSR on stress, well-being, and daily spiritual experiences for 1 year in academic health care employees. J Altern Complement Med. 2011;17:939–44. doi: 10.1089/acm.2010.0335. [DOI] [PubMed] [Google Scholar]
- 25.Dick BD, Rashiq S, Verrier MJ, Ohinmaa A, Zhang J. Symptom burden, medication detriment, and support for the use of the 15D health-related quality of life instrument in a chronic pain clinic population. Pain Res Treat 2011. 2011:809071. doi: 10.1155/2011/809071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McCabe C, Lewis J, Shenker N, Hall J, Cohen H, Blake D. Don’t look now! Pain and attention. Clin Med. 2005;5:482–6. doi: 10.7861/clinmedicine.5-5-482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bener A, Verjee M, Dafeeah EE, Falah O, Al-Juhaishi T, Schlogl J, et al. Psychological factors: Anxiety, depression, and somatization symptoms in low back pain patients. J Pain Res. 2013;6:95–101. doi: 10.2147/JPR.S40740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lee JE, Watson D, Frey-Law LA. Psychological factors predict local and referred experimental muscle pain: A cluster analysis in healthy adults. Eur J Pain. 2013;17:903–15. doi: 10.1002/j.1532-2149.2012.00249.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Davidson RJ, Kabat-Zinn J, Schumacher J, Rosenkranz M, Muller D, Santorelli SF, et al. Alterations in brain and immune function produced by mindfulness meditation. Psychosom Med. 2003;65:564–70. doi: 10.1097/01.psy.0000077505.67574.e3. [DOI] [PubMed] [Google Scholar]
- 30.Lazar SW, Kerr CE, Wasserman RH, Gray JR, Greve DN, Treadway MT, et al. Meditation experience is associated with increased cortical thickness. Neuroreport. 2005;16:1893–7. doi: 10.1097/01.wnr.0000186598.66243.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McCracken LM, Jones R. Treatment for chronic pain for adults in the seventh and eighth decades of life: A preliminary study of Acceptance and Commitment Therapy (ACT) Pain Med. 2012;13:860–7. doi: 10.1111/j.1526-4637.2012.01407.x. [DOI] [PubMed] [Google Scholar]
- 32.McCracken LM, Gutiérrez-Martínez O. Processes of change in psychological flexibility in an interdisciplinary group-based treatment for chronic pain based on Acceptance and Commitment Therapy. Behav Res Ther. 2011;49:267–74. doi: 10.1016/j.brat.2011.02.004. [DOI] [PubMed] [Google Scholar]


