Abstract
Background:
Cardiovascular diseases remain the leading cause of death worldwide. Metabolic syndrome (MetS) is the clustering of risk factors for developing the disease. Strong evidence exists for the efficacy of screening for MetS. However, the potential of novel web-based studies for MetS and online assessing of the quality of life (QOL) for these high-risk participants have not been explored.
Methods:
This was a web-based, cross-sectional study. Participants were recruited through online registering on the study website. Then, those who met the study criteria (waist circumference [WC] ≥90 and blood pressure [BP] ≥130/85) were contacted and invited for the clinical assessments, if they wish. Baseline measurements were MetS risk factors (weight, WC, body mass index and BP, total cholesterol, low-density lipoprotein-cholesterol, high-density lipoprotein-cholesterol, triglycerides, and fasting blood glucose) and health-related QOL (HRQOL) that was measured using the short form-36 (SF-36).
Results:
There were 1436 (male: 928, female: 508) registration data on the study website. Reviewing the data, of 317 eligible participants that were invited to the study, 229 persons were responded to invitation in the screening program. The mean age of participants was 43.8 (standard deviation [SD] = 9.9) years. MetS was more frequent in male and married persons. In addition, participants with MetS had lower mean (SD) scores than participants without MetS for the following subscales of HRQOL as: role-physical (with MetS 51.1±35.2; versus without MetS 65.3 ± SD = 40.1), vitality (with MetS 65± 21; versus without MetS 75.3 ± 21.1), mental health (with MetS 49.5±30.1; versus without MetS 34.1±17.2)(P < 0.05 for all).
Conclusions:
People with MetS experienced lower HRQOL than without MetS. Internet as a powerful medium offers a novel setting for delivery health information. It seems that high BP and abdominal obesity are associated with lower HRQOL in the participants with MetS. A web-based prevention program could make people aware for their vulnerability to MetS and its complications.
Keywords: Cardiovascular diseases, e-screening, Internet, metabolic syndrome, quality of life, web-based study
INTRODUCTION
Cardiovascular diseases (CVDs) remain the leading cause of death worldwide.[1] The metabolic syndrome (MetS) is a complex of risk factor for CVDs.[2] It has been reported that prevalence of MetS in the Islamic republic of Iran is one of the highest in the world.[3] Tehran Lipid and Glucose study (TLGS) reported that the prevalence of MetS among the adult populations is 33.7 (women 42% and men 24%).[3] MetS consisted of abdominal obesity, dyslipidemia, hypertension, and raised plasma glucose. MetS is present when three or more of the listed criteria are met. Abdominal obesity was determined by increased waist circumference (WC).[4] WC is a simple anthropometric measurement for screening and determined high-risk people successfully.[5] The International Diabetes Federation (IDF) has declared that WC is a gender- and ethnic group-specific indicator and has relatively quick and simple measurement. Therefore, this valuable and useful index should be considered to define MetS.[6] To facilitate the prevention of MetS, WHO recommended using anthropometric measurements, especially WC measurement.[7] This tool is widely used as measures of health and could more accurately predict the risk of MetS.[7]
The Internet has the potential to provide large populations with individual health promotion advice at a relatively low cost.[8,9,10] Over the past decade, there has been an explanation in web-based health studies focused on physical activity and nutrition,[11,12] weight loss,[13,14,15] diabetes care,[16,17] chronic conditions,[18,19,20] smoking cessation,[21,22] substance abuse,[23] alcohol consumption,[24,25,26] and depression, anxiety, and stress,[27,28] that use the different methodologies for Internet applications in terms of Internet therapy, Internet treatment, web-based programs, Internet communications, and e-health. Eysenbach defines e-health as follows: “E-health is an emerging field in the intersection of medical informatics, public health, and business, referring to health services and information delivered or enhanced through the Internet and related technologies. In a broader sense, the term characterizes not only a technical development, but also a state of mind, a way of thinking, an attitude, and a commitment for network, global thinking, to improve health care locally, regionally, and worldwide by using information and communication technology.”[29] The Internet as an information tool offers opportunity to aware of diseases, risk factors, symptoms, treatment, and strategies to deal with each of these; consequently increasing their chance for determination, diagnosis, and treatment of the problems.[30,31,32] In addition, research suggests that the Internet has revolutionized the way patient access health care information, learn more about their conditions, and make health care decisions.
It remains a concern that most at-risk people for MetS are unaware of its risk factors.[33] Measurement of WC is a reliable and simple test to identify individuals for MetS.[5] This measurement could be used more frequently in daily practice in primary care to identify at-risk individuals. Thus, it should be important to make people aware of the MetS risk factors and WC through accessible and available communication channels and encourage them to diagnosis, e-screening, and management programs of MetS. The aim of this web-based study was to determine the people who had potential risk for MetS and CVDs, also assessing the association between MetS and the health-related quality of life (HRQOL).
METHODS
Study design and participants
This was a web-based, cross-sectional study that carried out in Tehran, Iran. The study presents the screening results of “Red Ruby” study, a web-based, randomized, controlled trial for lifestyle modifying on people with MetS. Details of the study design have been submitted elsewhere.[33,34] Participants were recruited from an online registration website namely Healthy Heart Education (http://www.Heartresearch.ir). This website is designed to increase public's awareness about CVDs and MetS. It is providing reliable information for users about MetS risk factors and CVDs. There was general information about hypertension, MetS, diabetes, obesity and central obesity, nutrition for healthy heart, and CVDs that were available for users in HTML and PDF formats. The participants were registered through registration page that invited people to participate in a study as “Red Ruby.” Required information for registration on the study were name, gender, age, WC, weight, height, E-mail, and address. Self-measuring of WC was showed on the homepage. Eligibility for participating in the study was WC 90 cm and blood pressure (BP) of ≥130/85 mmHg and one more MetS components. Trained research assistants reviewed the study website database and identified registrants aged 20 years and older with WC 90 cm over from Tehran and contacted them by telephone. During the contact, individuals were screened for eligibility and participants who consented to participate were asked to schedule to free clinical measurements by the trained research assistant at Tehran Heart Center (local hospital).
Data collection and variables’ measurements
Baseline measurements were MetS risk factors that were measured as primary outcomes: Weight, WC, body mass index (BMI) and BP, total cholesterol, low-density lipoprotein-cholesterol, high-density lipoprotein-cholesterol (HDL-C), triglycerides, and fasting blood glucose [FBG]). Briefly, weight was measured while the subjects were minimally clothed without shoes using a calibrated scale (Seca model 8811021658). Height was measured in a standing position, without shoes, using a tape measure, while the shoulders were in a normal position. BMI was calculated as weight in kilograms divided by height in meters squared. WC was measured at the narrowest level over light clothing, using a tape measure, and without any pressure to body surface. The HRQOL using the SF-36[35] is measured as secondary outcome. The SF-36 yields an 8-scale profile of scores: Physical functioning, role-physical, bodily pain, general health, vitality, social functioning; role-emotional and mental health. The SF-36 subscales are standardized to a 0–100 point scale, and higher scores represent better QOL. Questionnaire was completed online.
The MetS was defined according to the criteria of the National Cholesterol Education Program's Adult Treatment Panel III (ATP III).[36] metabolic syndrome was determined according to following components: WC 90 cm both gender 90 (cut-off for MetS in Iran for both genders),[37,38,39] serum triglycerides ≥150 mg/dl, HDL-C <40 mg/dl in men and <50 mg/dl in women, systolic/diastolic BP ≥130/≥85 mmHg, and fasting glucose ≥110 mg/dl.
Statistical analysis
All statistical analyses were performed by SPSS software (version 21.0, IBM Co., Chicago, IL). P < 0.05 considered as statistically significant. To explore the data, we used descriptive statistics including reporting on mean, standard deviation (SD), frequency, and percentage. To evaluate the differences among groups, we used Chi-square test and independent t-test.
Ethics
Ethical approval was granted by the Ethics Committee of Tehran University of Medical Sciences (the project number: 90/130/1736). We obtained written informed consent from all the participants.
RESULTS
General characteristics in study participants
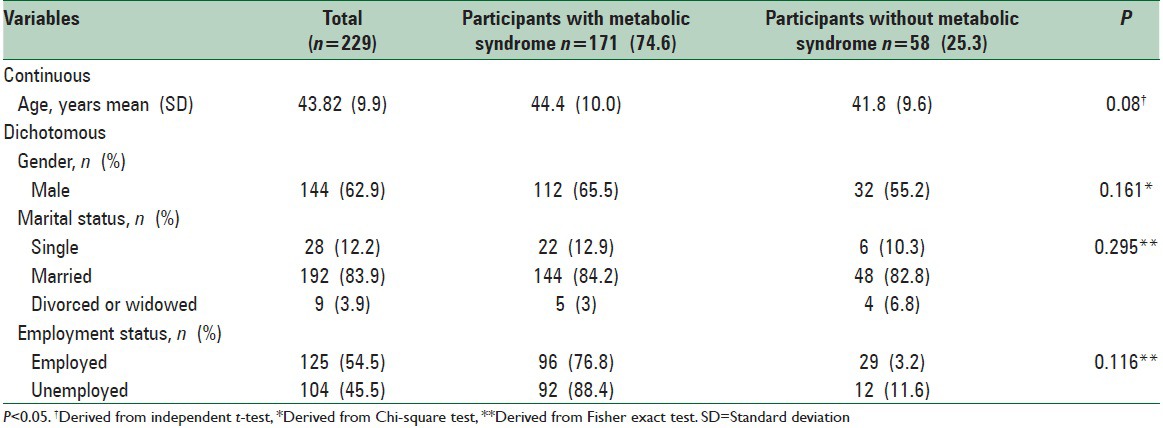
Figure 1 shows the flow of study procedure. Data were extracted from the registration records of the study website, 1436 (male: 928, female 508). The age ranged from 18 to 78 years with an average of 39.3 (SD = 11.4), 64.63% were male. The mean weight, WC, and BMI was 77.3 kg (SD = 16.4), 94 cm (13.84), and 26 kg/m2 (SD = 4.6), respectively. For web-based self-report of WC measurement, of 1081 participants, 392 were excluded for WC < 90 cm; 37 for incomplete response, and 30 for invalid telephone number. Thus, 622 people that had the WC ≥ 90 cm on the registration data were interviewed by the telephone. Those with a history of CVDs (68), diabetics (51), use of antihypertensive medications (45), cholesterol-lowering medications (32), BP <130/85 mmHg (96), renal and cancer diseases (12), and 1 being pregnant were excluded. Thus, 317 eligible participants were invited to the study out of which 229 responded and investigated for the presence of MetS and its components. The basic characteristics of the participants are summarized in Table 1. The majority of the participants were male (62.9%) with a mean age of 43.8 ± 9.9 years and 55.5% participants had higher education. Although the mean age of participants with MetS (44.4 ± 10.0) was higher than non-MetS (41.8 ± 9.6), this difference was not statistically significant (P < 0.05).
Figure 1.
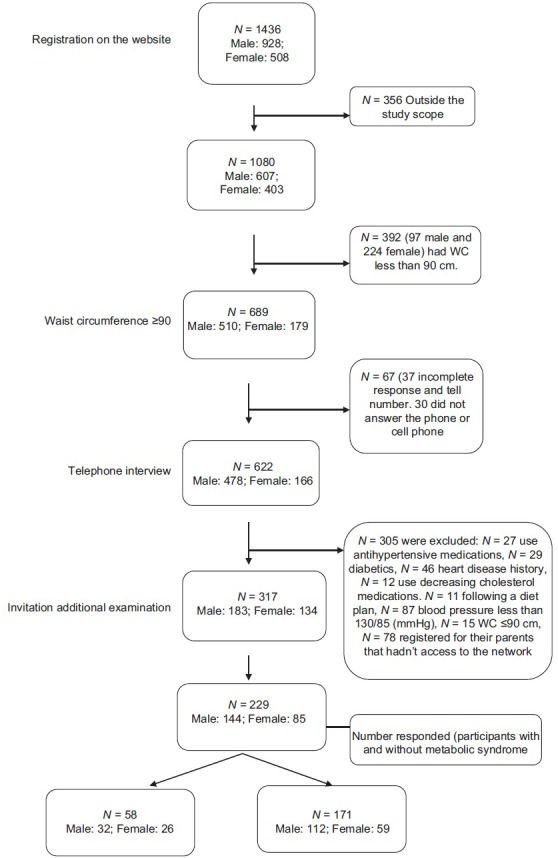
Web screening for metabolic syndrome
Table 1.
Demographic characteristics of participants in a web-based study
Metabolic syndrome components in study participants
Table 2 presents mean (SD) of clinical measurements of participants with and without MetS. Participants with and without MetS did not differ in weight, BMI, FBG, and HDL (for men). MetS was more frequent in male genders and married persons. Diastolic BP ≥ 85 was the most common metabolic abnormality (64.2%) among all participants. Among participants with MetS, hypertriglyceridemia (79.6) was the most common followed by systolic BP ≥ 130 (76.5%), low HDL-C (71.3%), and high FBG (12.8).
Table 2.
Anthropometric and laboratory results of web-based screening participants with and without metabolic syndrome
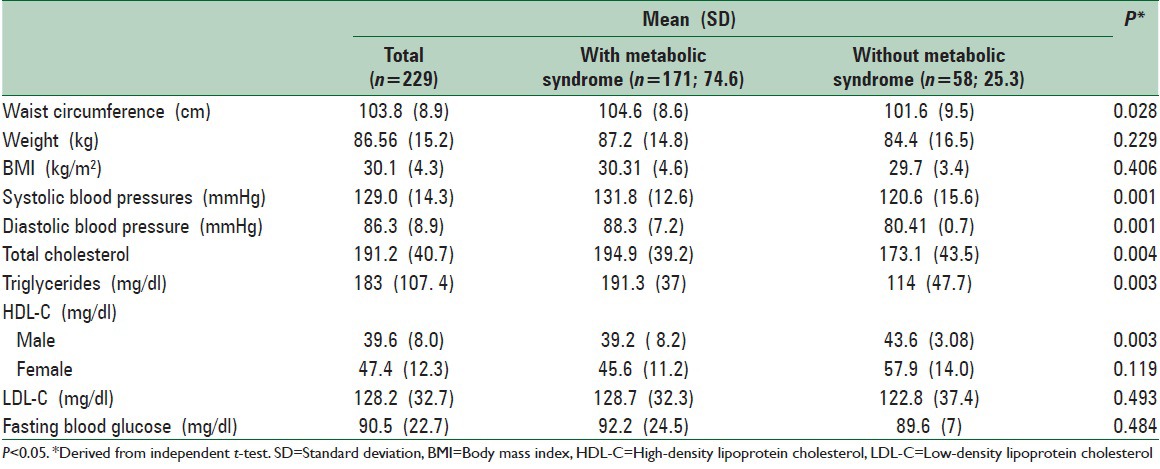
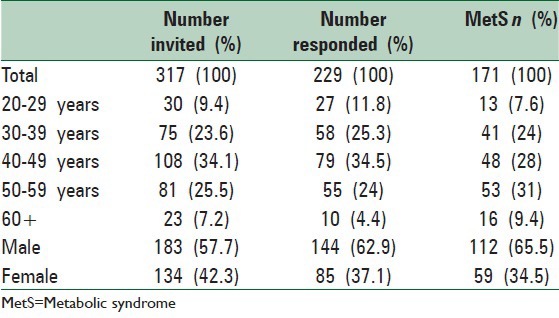
Table 3 shows response rate according to age and gender classification. The overall response rate for invitation in the web-based screening program for MetS was 72.2%. Male (68.6) and 40–49 years old participants (34.5) were more likely to participate in the study. The MetS is more common in older age groups, but there is a growth in 30–39 years (55.6).
Table 3.
Response rate and MetS in a web-based screening program for MetS
Health-related quality of life
The SF-36 scores for people with and without MetS are shown in Figure 2. Individual with MetS had significantly lower scores on three of the eight subscales of the SF-36. These were role-physical, vitality, and mental health subscales of SF-36 (P < 0.001). In addition, participants with MetS had lower mean (SD) scores than participants without MetS for the following subscales of HRQOL as: role-physical (with MetS 51.1±35.2; versus without MetS 65.3 ± SD = 40.1), vitality (with MetS 65± 21; versus without MetS 75.3 ± 21.1), mental health (with MetS 49.5±30.1; versus without MetS 34.1±17.2) (P < 0.05 for all).
Figure 2.
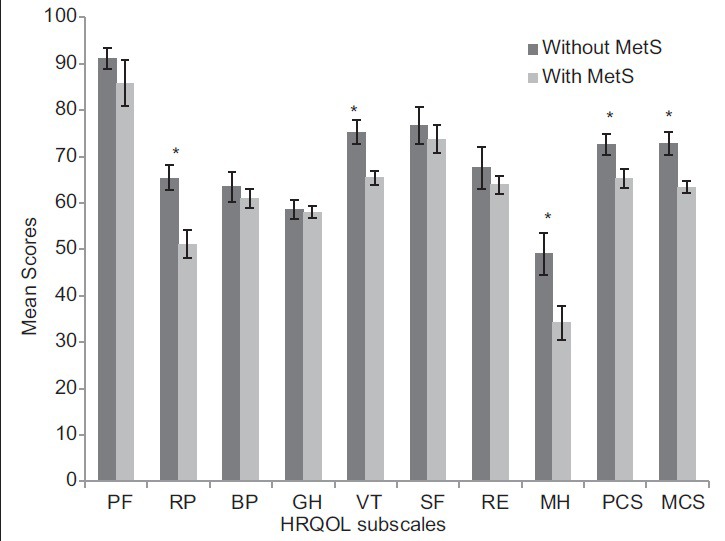
Health-related quality of life mean scores according to with and without metabolic syndrome. *P < 0.05. PF: Physical functioning, RP: Role-physical, BP: Bodily pain, GH: General health, VT: Vitality, SF: Social functioning, RE: Role emotional, MH: Mental health, PCS: Physical component summary, MCS: Mental components summary
DISCUSSION
The main finding of our study is that MetS was associated with poorer HRQOL in participants with MetS than participants without MetS. In spite of different method of the study, our results are consistent with the other studies.[40,41]
Lower HRQOL on three subscales of the SF-36 was observed that includes role-physical, vitality, and mental health. In addition, participants with MetS had significantly lower scores on the PCS and mental components summary components than participants without MetS. Several studies have investigated on HRQOL among people with MetS by using HRQOL instrument.[42,43] The study by Tsai et al.[44] showed that participants with MetS had lower scores on physical function and general health. The other study in Iran that used the different questionnaire for assessing the QOL (WHOQOL-BREF) reported no association between QOL domains and MetS in men, while only social relations and physical health scores were higher in women.[45]
Creating and promoting a website for increasing public awareness and invitation to screening for MetS resulted in a significant number of registering users on the study website. The purpose of the present study was to encourage users with MetS through a website to participate in the screening program and assessing their HRQOL. The large proportion of visitors was men who respond to the invitation in the screening program. It appears that using of abdominal obesity as an increased WC might make it a useful tool when assessing MetS.[5] A single self-measurement of WC is easy to perform and it is known in related to CVDs.[46] To our knowledge, there is no previous web-based study focusing on the screening of MetS. From a public health point of view, early identification of high risk and difficult to reach individuals via the Internet is an important issue, especially in primary care.
According to the results of our study, men were more interested in web-based health programs (64.6 registrants) and had higher response rate (68.6) than women. A significant number of participants who visited and registered on the study website were patients with chronic diseases (18.1). A study conducted by Shuyler and Knight[47] found that patients frequently search on the Internet to find information about a condition, treatment, or symptoms of the diseases. It is also possible for the Internet to provide information about alternative treatments and whether specific conditions were curable.[48]
Whether the study is benefited from participants of general population with wide range of age that recruiting through virtual environments who have experienced MetS and never looking for health care or carried out clinical assessments for MetS. MetS is not a disease, but it is a high-risk condition with a cluster of metabolic disturbances that is associated with a 2-fold increase in cardiovascular outcomes and 3.5–5-fold in type 2 diabetes.[2] It is argued that relatively simple approach for diagnosing the MetS by employing easily measurable risk factors might be provided in the prevention of MetS. In addition, it seems that self-measurement of WC is easy to perform and it is known in related to CVDs.[5] Thus, from a public health point of view, early identification of high risk and difficult to reach individuals via the Internet is an important issue, especially in primary care.
Although, in this study, participants were selected those who had high BP and WC 90 cm and over, there were significant differences between participants with and without MetS (P < 0. 05). It seems that high BP and abdominal obesity are associated with lower HRQOL in the participants of the study. The previous study on the relationship between MetS and HRQOL confirmed these findings.[42,43]
Internet as a powerful medium offers a novel setting for delivering health information. In summary, our study found that designing trusted and reliable health websites and delivering information about risk factors, symptoms, and treatment of MetS help to overcome the problem. However, participants of web-based studies were high-educated, but according with the previous report,[49] HRQOL in participants with MetS appeared better than participants who lost from the study.
CONCLUSIONS
An Internet-based prevention program could make high-risk people aware for their vulnerability to MetS and its complications, early diagnosis of disorder, increase their knowledge, encourage them to regular clinical testing, and may contribute to risk reduction.
ACKNOWLEDGEMENTS
This manuscript originated from a PhD thesis (240\2425) by Leila Jahangiry, Department of Health Education and Promotion, School of Public Health, Tehran University of Medical Sciences, Tehran, Iran. We acknowledge the contributions of Tehran Heart Center for providing facilities to the study. Finally, we wish to thank the Iranian Institute for Health Sciences Research (ACECR) for their time and support for this research.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Burke V, Beilin LJ, Cutt HE, Mansour J, Williams A, Mori TA. A lifestyle program for treated hypertensives improved health-related behaviors and cardiovascular risk factors, a randomized controlled trial. J Clin Epidemiol. 2007;60:133–41. doi: 10.1016/j.jclinepi.2006.05.012. [DOI] [PubMed] [Google Scholar]
- 2.Grundy SM, Cleeman JI, Bairey Merz CN, Brewer JHB, Clark LT, Hunninghake DB, et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. J Am Coll Cardiol. 2004;44:720–32. doi: 10.1016/j.jacc.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 3.Azizi F, Hadaegh F, Khalili D, Esteghamati A, Hosseinpanah F, Delavari A, et al. Appropriate definition of metabolic syndrome among Iranian adults: Report of the Iranian National Committee of Obesity. Arch Iran Med. 2010;13:426–8. [PubMed] [Google Scholar]
- 4.Beilby J. Definition of metabolic syndrome: Report of the National Heart, Lung, and Blood Institute/American Heart Association Conference on Scientific Issues Related to Definition. Clin Biochem. 2004;25:195–8. [Google Scholar]
- 5.Siren R, Eriksson JG, Vanhanen H. Waist circumference a good indicator of future risk for type 2 diabetes and cardiovascular disease. BMC Public Health. 2012;12:631. doi: 10.1186/1471-2458-12-631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alberti KG, Zimmet P, Shaw J. The Metabolic Syndrome – A New Worldwide Definition. A Consensus Statement from the International Diabetes Federation. Diabet Med. 2006;23:469–80. doi: 10.1111/j.1464-5491.2006.01858.x. [DOI] [PubMed] [Google Scholar]
- 7.Shiwaku K, Anuurad E, Enkhmaa B, Kitajima K, Yamane Y. Appropriate BMI for Asian populations. Lancet. 2004;363:1077. doi: 10.1016/S0140-6736(04)15856-X. [DOI] [PubMed] [Google Scholar]
- 8.Mahdieh Abbasalizad Farhangi, Leila Jahangiry, Mir-Mousa Mirinazhad, Davoud Shojaeezade, Ali Montazeri, Alireza Yaghoubi. A web-based interactive lifestyle modification program improves lipid profile and serum adiponectin concentrations in patients with metabolic syndrome: The “Red Ruby” study. International Journal of Diabetes in Developing Countries 2015; In press. DOI 10.1007/s13410-015-0395-z. [Google Scholar]
- 9.Myung SK, McDonnell DD, Kazinets G, Seo HG, Moskowitz JM. Effects of Web- and computer-based smoking cessation programs: Meta-analysis of randomized controlled trials. Arch Intern Med. 2009;169:929–37. doi: 10.1001/archinternmed.2009.109. [DOI] [PubMed] [Google Scholar]
- 10.Danaher BG, Seeley JR. Methodological issues in research on web-based behavioral interventions. Ann Behav Med. 2009;38:28–39. doi: 10.1007/s12160-009-9129-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mauriello LM, Sherman KJ, Driskell MM, Prochaska JM. Using interactive behavior change technology to intervene on physical activity and nutrition with adolescents. Adolesc Med State Art Rev. 2007;18:383–99, xiii. [PubMed] [Google Scholar]
- 12.Hamel LM, Robbins LB, Wilbur J. Computer- and web-based interventions to increase preadolescent and adolescent physical activity: A systematic review. J Adv Nurs. 2011;67:251–68. doi: 10.1111/j.1365-2648.2010.05493.x. [DOI] [PubMed] [Google Scholar]
- 13.Tate DF. A series of studies examining Internet treatment of obesity to inform Internet interventions for substance use and misuse. Subst Use Misuse. 2011;46:57–65. doi: 10.3109/10826084.2011.521089. [DOI] [PubMed] [Google Scholar]
- 14.Arem H, Irwin M. A review of web-based weight loss interventions in adults. Obes Rev. 2011;12:e236–43. doi: 10.1111/j.1467-789X.2010.00787.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nguyen B, Kornman KP, Baur LA. A review of electronic interventions for prevention and treatment of overweight and obesity in young people. Obes Rev. 2011;12:e298–314. doi: 10.1111/j.1467-789X.2010.00830.x. [DOI] [PubMed] [Google Scholar]
- 16.Azar M, Gabbay R. Web-based management of diabetes through glucose uploads: Has the time come for telemedicine? Diabetes Res Clin Pract. 2009;83:9–17. doi: 10.1016/j.diabres.2008.09.055. [DOI] [PubMed] [Google Scholar]
- 17.Kaufman N. Internet and information technology use in treatment of diabetes. Int J Clin Pract Suppl. 2010;166:41–6. doi: 10.1111/j.1742-1241.2009.02277.x. [DOI] [PubMed] [Google Scholar]
- 18.Murray E, Burns J, See TS, Lai R, Nazareth I. Interactive health communication applications for people with chronic disease. Cochrane Database Syst Rev. 2005;4:CD004274. doi: 10.1002/14651858.CD004274.pub4. [DOI] [PubMed] [Google Scholar]
- 19.Webb TL, Joseph J, Yardley, Michie S. Using the Internet to Promote Health Behavior Change: A Systematic Review and Meta-analysis of the Impact of Theoretical Basis, Use of Behavior Change Techniques, and Mode of Delivery on Efficacy. Journal of internet medical research. 2010;1:e4. doi: 10.2196/jmir.1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schubart JR, Stuckey HL, Ganeshamoorthy A, Sciamanna CN. Chronic health conditions and internet behavioral interventions: A review of factors to enhance user engagement. Comput Inform Nurs. 2011;29:81–92. doi: 10.1097/NCN.0b013e3182065eed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bock BC, Graham AL, Whiteley JA, Stoddard JL. A review of web-assisted tobacco interventions (WATIs) J Med Internet Res. 2008;10:e39. doi: 10.2196/jmir.989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hutton HE, Wilson LM, Apelberg BJ, Tang EA, Odelola O, Bass EB, et al. A systematic review of randomized controlled trials: Web-based interventions for smoking cessation among adolescents, college students, and adults. Nicotine Tob Res. 2011;13:227–38. doi: 10.1093/ntr/ntq252. [DOI] [PubMed] [Google Scholar]
- 23.Copeland J, Martin G. Web-based interventions for substance use disorders: A qualitative review. J Subst Abuse Treat. 2004;26:109–16. doi: 10.1016/S0740-5472(03)00165-X. [DOI] [PubMed] [Google Scholar]
- 24.Finfgeld-Connett D. Web-based treatment for problem drinking. J Psychosoc Nurs Ment Health Serv. 2006;44:20–7. doi: 10.3928/02793695-20060901-04. [DOI] [PubMed] [Google Scholar]
- 25.Vernon ML. A review of computer-based alcohol problem services designedfor the general public. J Subst Abuse Treat. 2010;3:203–11. doi: 10.1016/j.jsat.2009.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Walters ST, Wright JA, Shegog R. A review of computer and Internet-based interventions for smoking behavior. Addict Behav. 2006;31:264–77. doi: 10.1016/j.addbeh.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 27.Robertson L, Smith M, Castle D, Tannenbaum D. Using the Internet to enhance the treatment of depression. Australas Psychiatry. 2006;14:413–7. doi: 10.1080/j.1440-1665.2006.02315.x. [DOI] [PubMed] [Google Scholar]
- 28.Van’t Hof E, Cuijpers P, Stein DJ. Self-help and Internet-guided interventions in depression and anxiety disorders: A systematic review of meta-analyses. CNS Spectr. 2009;14(2 Suppl 3):34–40. doi: 10.1017/s1092852900027279. [DOI] [PubMed] [Google Scholar]
- 29.Eysenbach G. What is e-Health? J Med Internet Res. 2001;3:e20. doi: 10.2196/jmir.3.2.e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Southard BH, Southard DR, Nuckolls J. Clinical trial of an Internet-based case management system for secondary prevention of heart disease. J Cardiopulm Rehabil. 2003;23:341–8. doi: 10.1097/00008483-200309000-00003. [DOI] [PubMed] [Google Scholar]
- 31.Padilla R, Bull S, Raghunath SG, Fernald D, Havranek EP, Steiner JF. Designing a cardiovascular disease prevention web site for Latinos: Qualitative community feedback. Health Promot Pract. 2010;11:140–7. doi: 10.1177/1524839907311051. [DOI] [PubMed] [Google Scholar]
- 32.Whittemore R, Grey M, Lindemann E, Ambrosino J, Jaser S. Development of an Internet coping skills training program for teenagers with type 1 diabetes. Comput Inform Nurs. 2010;28:103–11. doi: 10.1097/NCN.0b013e3181cd8199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Leila Jahangiry, Davoud Shojaeizadeh, Ali Montazeri, Mahdi Najafi, Kazem Mohammad, Mahdieh Abbasalizad Farhangi. Modifiable Lifestyle Risk Factors and Metabolic Syndrome: Opportunities for a Web-Based Preventive Program. Journal of research in health sciences. 2014;14:303–7. [PubMed] [Google Scholar]
- 34.Jahangiry L, Shojaeizadeh D, Najafi M, Mohammad K, Abbasalizad Farhangi M, Montazeri A. ‘Red Ruby’: An interactive web-based intervention for lifestyle modification on metabolic syndrome: A study protocol for a randomized controlled trial. BMC Public Health. 2014;14:748. doi: 10.1186/1471-2458-14-748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Montazeri A, Goshtasebi A, Vahdaninia M, Gandek B. The Short Form Health Survey (SF-36): Translation and validation study of the Iranian version. Qual Life Res. 2005;14:875–82. doi: 10.1007/s11136-004-1014-5. [DOI] [PubMed] [Google Scholar]
- 36.John B. Definition of Metabolic Syndrome: Report of the National Heart, Lung, and Blood Institute/American Heart Association Conference on Scientific Issues Related to Definition. 2009 [Google Scholar]
- 37.Esteghamati A, Abbasi M, Rashidi A, Meysamie A, Khalilzadeh O, Haghazali M, et al. Optimal waist circumference cut-offs for the diagnosis of metabolic syndrome in Iranian adults: Results of the third national survey of risk factors of non-communicable diseases (SuRFNCD-2007) Diabet Med. 2009;26:745–6. doi: 10.1111/j.1464-5491.2009.02756.x. [DOI] [PubMed] [Google Scholar]
- 38.Delavari A, Forouzanfar MH, Alikhani S, Sharifian A, Kelishadi R. First nationwide study of the prevalence of the metabolic syndrome and optimal cutoff points of waist circumference in the Middle East: The national survey of risk factors for noncommunicable diseases of Iran. Diabetes Care. 2009;32:1092–7. doi: 10.2337/dc08-1800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Azizi F, Khalili D, Aghajani H, Esteghamati A, Hosseinpanah F, Delavari A, et al. Appropriate waist circumference cut-off points among Iranian adults: The first report of the Iranian National Committee of Obesity. Arch Iran Med. 2010;13:243–4. [PubMed] [Google Scholar]
- 40.Miettola J, Niskanen LK, Viinamäki H, Sintonen H, Kumpusalo E. Metabolic syndrome is associated with impaired health-related quality of life: Lapinlahti 2005 study. Qual Life Res. 2008;17:1055–62. doi: 10.1007/s11136-008-9386-6. [DOI] [PubMed] [Google Scholar]
- 41.Corica F, Corsonello A, Apolone G, Mannucci E, Lucchetti M, Bonfiglio C, et al. Metabolic syndrome, psychological status and quality of life in obesity: The QUOVADIS Study. Int J Obes (Lond) 2008;32:185–91. doi: 10.1038/sj.ijo.0803687. [DOI] [PubMed] [Google Scholar]
- 42.Laudisio A, Marzetti E, Antonica L, Pagano F, Vetrano DL, Bernabei R, et al. Metabolic syndrome and quality of life in the elderly: Age and gender differences. Eur J Nutr. 2013;52:307–16. doi: 10.1007/s00394-012-0337-1. [DOI] [PubMed] [Google Scholar]
- 43.Tziallas D, Kastanioti C, Kostapanos MS, Skapinakis P, Elisaf MS, Mavreas V. The impact of the metabolic syndrome on health-related quality of life: A cross-sectional study in Greece. Eur J Cardiovasc Nurs. 2012;11:297–303. doi: 10.1016/j.ejcnurse.2011.02.004. [DOI] [PubMed] [Google Scholar]
- 44.Tsai AG, Wadden TA, Sarwer DB, Berkowitz RI, Womble LG, Hesson LA, et al. Metabolic syndrome and health-related quality of life in obese individuals seeking weight reduction. Obesity (Silver Spring) 2008;16:59–63. doi: 10.1038/oby.2007.8. [DOI] [PubMed] [Google Scholar]
- 45.Sarrafzadegan N, Gharipour M, Ramezani MA, Rabiei K, Zolfaghar B, Tavassoli AA, et al. Metabolic syndrome and health-related quality of life in Iranian population. J Res Med Sci. 2011;16:254–61. [PMC free article] [PubMed] [Google Scholar]
- 46.Janiszewski PM, Janssen I, Ross R. Does waist circumference predict diabetes and cardiovascular disease beyond commonly evaluated cardiometabolic risk factors? Diabetes Care. 2007;30:3105–9. doi: 10.2337/dc07-0945. [DOI] [PubMed] [Google Scholar]
- 47.Shuyler KS, Knight KM. What are patients seeking when they turn to the Internet?. Qualitative content analysis of questions asked by visitors to an orthopaedics Web site. J Med Internet Res. 2003;5:e24. doi: 10.2196/jmir.5.4.e24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Eysenbach G, Diepgen TL. Patients looking for information on the Internet and seeking teleadvice: Motivation, expectations, and misconceptions as expressed in e-mails sent to physicians. Arch Dermatol. 1999;135:151–6. doi: 10.1001/archderm.135.2.151. [DOI] [PubMed] [Google Scholar]
- 49.Jahangiry L, Shojaeizadeh D, Montazeri A, Najafi M, Mohammad K, Yaseri M. Adherence and attrition in a web-based lifestyle intervention for people with metabolic syndrome. Iran J Public Health. 2014;43:1248–58. [PMC free article] [PubMed] [Google Scholar]


