Abstract
Background:
High blood pressure (BP) has been known as a major risk factor for many chronic diseases. It should be noted, a psychiatric disorder which is common in the people living modern lifestyle may be one of the leading causes of hypertension, and many people are prescribed antidepressant each year. Hence, the purpose of this study was to evaluate the effect of selective serotonin reuptake inhibitors (SSRIs) and alprazolam which defined as antidepressant on the BP levels, and to compare the BP levels between the group of users and nonusers.
Methods:
This randomized clinical trial study was conducted at the Nohom Dey Hospital in the Torbat-e Heydarieh, Iran between December 2011 and March 2012. Participants comprised 101 psychiatric patients with hypertension that randomly separated into users and nonusers of antidepressant. The period of intervention lasted for 3 months. The mean of BP calculated by this formula (systolic BP [SBP] +2 diastolic BP [DBP])/3 which was the main outcome of the study.
Results:
Users of antidepressant drugs did not have any significant changes in BP levels, except in patients who received SSRIs alone, significant improvement was observed in DBP (P = 0.04) and mean of BP (P = 0.03). While, in nonusers of antidepressant, significant development was observed in DBP, and mean of BP. Comparing the users and nonusers did not show any significant differences in SBP, DBP, and Mean of BP; even, when outcomes were adjusted for risk factors and antihypertensive drugs.
Conclusions:
Three months treatment with SSRIs and alprazolam did not have any effect on lowering BP level in patients with the psychiatric disorder.
Keywords: Alprazolam, hypertension, psychiatric disorder, selective serotonin reuptake inhibitors
INTRODUCTION
High blood pressure (BP) is a substantial risk factor for many diseases such as cardiovascular disease,[1] kidney failure,[2] brain injury,[3] and many others. The cause of hypertension is not known in many patients, but renal artery stenosis, severe pain, cerebrovascular disease, acute renal failure, not taking medications, and illegal drugs of antihypertensive treatment, panic attack or depression, and anxiety may lead to hypertension.[4,5,6]
Depression, mental, and psychological problems are common for people living a modern lifestyle, and the majority of these people do not know they are suffering from depression.[7] Hence, the use of antidepressant agents has increased substantially. Despite of some investigations that did not support the role of depressive or anxiety symptoms in the development of hypertension;[8,9] and also they stated, antidepressant use increases the risk for hypertension,[9] many cohort studies after several years follow-up suggested the association of anxiety and depression with the incidence of hypertension and the beneficial effects of antidepressants on lowering BP.[4,5,7,10] According to the studies that performed in psychiatry and primary healthcare units, up to 18% of anxiety disorder patients have hypertension[11] and more than 10% of older people in UK are prescribed an antidepressant each year.[12] In this respect, selective serotonin reuptake inhibitors (SSRIs) are approved for both depression and anxiety disorders.[13] A meta-analysis showed that patients who received psychosocial treatment had significant reductions in psychological distress and systolic BP (SBP).[14] van Haelst et al. in the retrospective observational follow-up study surveyed the association between perioperative use of SSRIs and changes in intraoperative BP by measuring the occurrence of intraoperative hyper- and hypo-tension. The outcomes after adjusted for confounding factors explored that the prevalence of hypertensive incidences was higher in users of SSRIs.[13] As we know, depression and anxiety might contribute to the development of hypertension through physiological deregulation including altered activity of the hypothalamic–pituitary–adrenal axis that observed in approximately 50% of depressed patients[7] and changes in the autonomic nervous system functioning, such as decreased parasympathetic and increased sympathetic tone.[15] In this regard, autonomic dysfunction may increase cardiac output, vascular resistance, and vasoconstriction.[16,17] Studies considering the association between antidepressants and BP levels have not produced consistent results about their efficacy on BP levels, until now. So, the purpose of this study was to evaluate the effect of SSRIs and alprazolam which defined as antidepressants on lowering BP levels, and to compare the BP levels between the group of users and nonusers.
METHODS
Study design and participants
This randomized clinical trial study was conducted at the Nohom Dey Hospital in Torbat-e Heydarieh, Iran between December 2011 and March 2012. Participants comprised 106 randomly selected men and women who referred to the hospital fulfilled the inclusion criteria. This trial allocation was parallel and [Figure 1] shows the Consort flow diagram. Inclusion criteria were history of hypertension with antihypertensive treatment or an initial SBP >140 or diastolic BP (DBP) >90 mmHg and repeated high BP after a 5 min resting period. In addition, signs of depression were diagnosed in them by psychiatrist through their psychological status such as feelings of hopelessness, loss of interest in daily activities, sleep disorders, and appetite or weight changes on the basis criteria for depression in Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition. Exclusion criteria included severe other psychiatric disorders such as general anxiety, schizophrenia and obsessive-compulsive disorder, current use of anti-depressants, and liver or kidney diseases. The sample size was calculated according with a comparison of means, which α considered 0.05 and power of the study was 80%. Afterward, all of the eligible participants signed informed consent and they randomly separated to the several groups included: (1) Users of SSRIs, (2) users of alprazolam, (3) users of SSRIs and alprazolam, and (4) users of SSRIs or alprazolam based on random digit number consecutively to four groups. The study protocol was taken under the medical ethics standards and was approved by the Medical Ethics Committee of Hospital by number 7889/a2.
Figure 1.
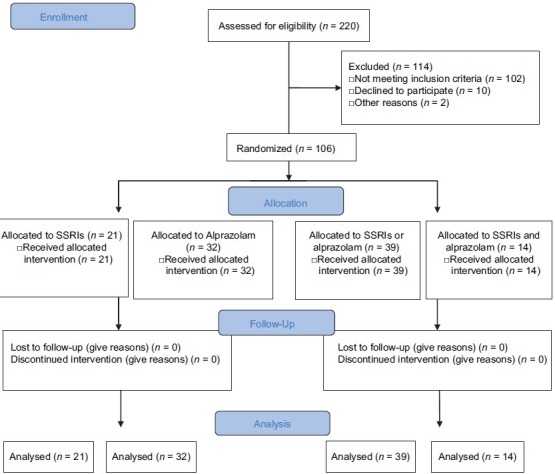
The Consort flow diagram
Procedure and variables assessments
Blood pressure measurement
Before BP measurements, the patients were seated quietly for at least 10 min in the chair and physician measured it with the cuff placed on the right upper arm and with the arm resting on a table. The first pulse sound was recorded as SBP and the level at which the pulse disappeared as DBP. The measurements were repeated after 2 min and the second reading was used in this study. The mean of BP calculated (SBP + 2 DBP)/3 in this study.
Intervention
Following baseline measurement of BP, case groups (users) received alprazolam (0.5 mg) and the group of SSRIs included citalopram (20 mg) or sertraline (50 mg), for 3 months in addition to the antihypertension drugs such as angiotensin-converting enzyme inhibitors (ACE-I), angiotensin II receptor blockers (ARBs), beta-blockers, diuretics, and calcium channel blockers that they used as usual and the dose of their medications were not altered during the study; while, the comparison groups (nonusers) only continued their antihypertension therapy.
Statistical analysis
For evaluation the changes between the results of baseline and postintervention data, paired t-test, or Wilcoxon singed-rank test (nonparametric test) were used. In addition, independent sample t-tests and Wilcoxon test (nonparametric test) were used for two groups’ comparison in case of continuous variables. The association between use of antidepressant drugs and hypertensive variables were done by linear regression. Results were expressed as mean and standard deviation, and the level of significance was set at P < 0.05. All analysis was based on intention to treat analysis.
RESULTS
A total of the participants (n = 108) with the age of 61.83 ± 11.26 years old with demographic characteristics that were shown in Table 1 reported with a diagnosis of hypertension at the 1st time of assessment. As shown in the Table 2, the subjects who used SSRIs during the investigation (3 months) had significant improvement in DBP (P < 0.05 and mean BP (P < 0.05), while SBP did not have any significant changes. On the other hand, in nonusers of SSRIs significant improvement was seen only in DBP (P < 0.05). When, the differences of the changes were compared between two groups, they did not indicate any significant differences in none of the variables. In addition, users and nonusers of alprazolam were examined and compared. No significant association was found between using alprazolam and all of the variables. However, nonusers of alprazolam had significant improvement in DBP (P < 0.05) and mean BP (P < 0.05). Furthermore, comparison of the changes between the two groups were not significant [Table 3]. Another table displayed the investigation and comparison of users and nonusers of both SSRIs and alprazolam. Results showed that users had no significant changes in each variable. Whereas, nonusers DBP (P < 0.05) and mean BP (P < 0.05) dropped significantly from baseline; in addition, in comparison of the two groups, we did not find the significant differences in any of the variables [Table 4]. Table 5 which was the exploration and comparison of users of SSRIs or alprazolam and nonusers of SSRIs or alprazolam revealed similar results like Table 4.
Table 1.
Demographic characteristics of patients
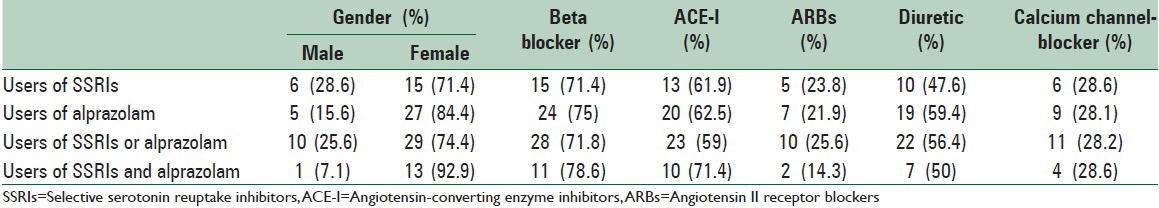
Table 2.
Comparison the changes within group and between groups
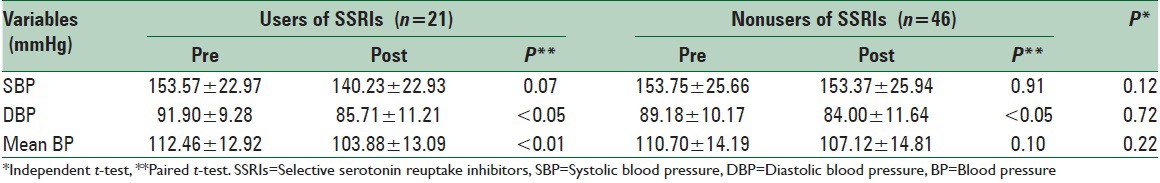
Table 3.
Comparison of the changes within group and between groups
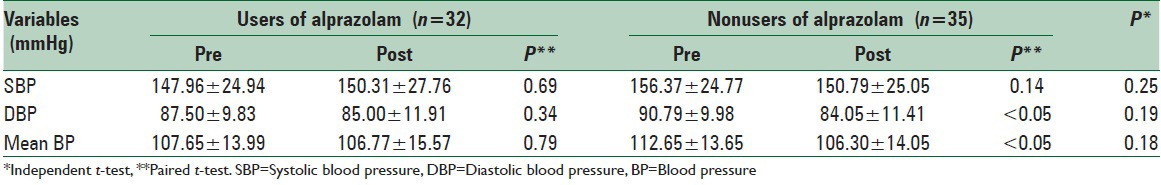
Table 4.
Comparison the changes within group and between groups
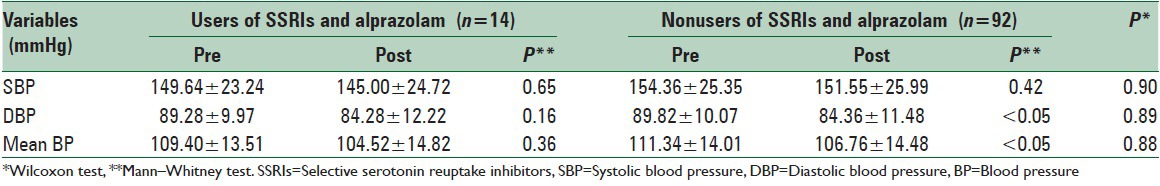
Table 5.
Comparison the changes within group and between groups
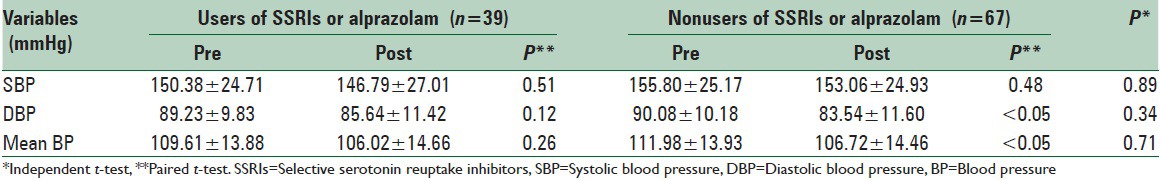
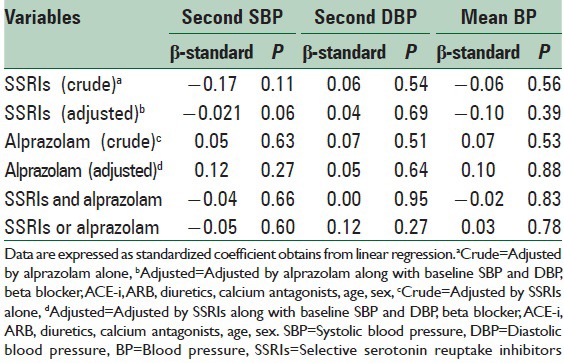
Table 6 showed that when alprazolam or SSRIs was included in the models, significant associations were not seen between drugs and all of the variables. In addition, the association remained nonsignificant when risk factors such as baseline SBP and DBP, age, sex, and antihypertensive drugs such as a beta blocker, ACE-I, ARBs, diuretic, and Ca-blocker were included in the models.
Table 6.
The association between use of antidepressant drugs and hypertensive variables
DISCUSSION
The present study revealed that users of antidepressant did not have any significant changes in BP levels, except in patients who received SSRIs alone, significant improvement was observed in DBP and mean BP. While, in nonusers of antidepressant, significant improvement was observed in DBP and mean BP. Comparing the users and nonusers did not show any significant differences in SBP, DBP, and mean BP; even, when outcomes were adjusted for risk factors and antihypertensive drugs. In fact, in our investigation, antidepressants usage did not have any association in lowering BP levels in depressed patients. According to previous studies, there were investigations which were similar to our results. For example, the article examined the long-term outcomes of depressed patients on SSRIs before coronary artery bypass grafting (CABG), the SSRIs group had a higher prevalence of hypertension, diabetes, hypercholesterolemia, cerebrovascular disease, peripheral vascular disease, and after adjustment for baseline differences, patients on SSRIs before CABG had increased risks of mortality, re-hospitalization.[18] Licht et al. that compared BP levels between subjects with clinical anxiety and depressive disorders (users of antidepressant = 664, nonusers of antidepressant = 1384) with healthy control (n = 590) found that depressive disorder is associated with low SBP and less hypertension, whereas the use of certain antidepressants is associated with both high diastolic and SBPs and hypertension.[9] Toh et al. investigated the effects of treatment with SSRIs on the risks of gestational hypertension in 5731 women with nonmalformed infants and no underlying hypertension. The risks of gestational hypertension were compared between women who did and did not receive SSRI treatment during pregnancy. Results suggested gestational hypertension was present in 9% of the 5532 women who were not treated with SSRIs and 19.1% of the 199 women who were treated with SSRIs. So, SSRIs exposure during pregnancy might identify women who are at an increased risk for gestational hypertension.[19] Lespérance et al. studied the effects of SSRIs (citalopram) on depression in patients with coronary artery disease (CAD) and compared users of citalopram for 12 weeks and matching placebo. Data revealed that citalopram or sertraline plus clinical management should be considered as a first step treatment for patients with CAD and major depression. In addition, they found no citalopram-placebo difference in systolic and diastolic BP.[20] In this regard, there were some studies on the contrary with our outcomes which suggested the safety and efficacy treatment of antidepressants on lowering BP. The investigation of Krishnan et al. with the aim of the safety and efficacy of sertraline as an antidepressant in the treatment of moderate-to-severe major depression in elderly outpatients with comorbid vascular disease revealed that sertraline was found to be a safe, well-tolerated, and effective in elderly patients suffering from hypertension and other forms of vascular comorbidity.[21] Another study which assessed the cardiovascular effect of citalopram in 811 elderly depressed patients concluded that the significant decrease in SBP and heart rate suggests that citalopram may reduce sympathoadrenal hyperactivity and the related increased cardiovascular morbidity and mortality associated with depression.[22] However, our results showed improvement in SBP according to the SSRIs usage but this improvement was not significant. Yilmaz et al. studied the relationship of anxiety with BP and the effect of anxiolytic treatment on BP of emergency department patients over 18-year-old with an initial hypertension. Their finding revealed that alprazolam is as effective as captopril in lowering BP in these patients, and anxiety is relieved more effectively with alprazolam;[10] whereas, this favorable changes did not observe in our study as a result of alprazolam usage. Another article carried out to compare the efficacy and safety of antianxiety treatment with sublingual captopril administration in 36 patients with excessive hypertension. Data showed antianxiety treatment is effective in lowering BP in patients with excessive hypertension without acute target organ damage.[6] According to contradictory between our results and the investigations mentioned above, it should be noted, the kind of SSRIs that used, the period of follow-up (short-term or long-term), the level of baseline BP (hypertension or excessive hypertension), low number of samples or even the age of the participants may be the causes of these variations.
The mechanisms linking the influence of SSRIs on the BP have been proposed to be the effects of several pathways. Serotonin may play the main role in the regulation of vascular tone, as serotonergic neurons, and receptors modulate vascular resistance.[23] It has been revealed that SSRIs not only affect neuronal serotonin uptake but also modulate peripheral serotonin. Sertraline, fluvoxamine, and paroxetine reduce platelet and whole blood serotonin concentrations after continual doses.[24] Additionally, SSRIs have been shown to affect circulating serotonin levels.[23] The inhibitory effect of SSRIs on the synthesis of nitric oxide as a vasodilator that seems to play a role in vascular tone has been mentioned as another potential pathway.[19,25] Some studies suggested that short-term SSRIs usage may reduce sympathetic nervous system activation[26] and the short-term responses may be different from those due to the long-term usage of SSRIs.[27]
CONCLUSIONS
Finally, we concluded that 3 months treatment with antidepressant did not have any effect on lowering BP level in patients with psychiatric disorder, and may be continuation of treatment with these drugs, more than 3 months, was necessary for getting significant findings.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Flack JM, Neaton J, Grimm R, Jr, Shih J, Cutler J, Ensrud K, et al. Blood pressure and mortality among men with prior myocardial infarction. Multiple Risk Factor Intervention Trial Research Group. Circulation. 1995;92:2437–45. doi: 10.1161/01.cir.92.9.2437. [DOI] [PubMed] [Google Scholar]
- 2.Borrelli S, De Nicola L, Stanzione G, Conte G, Minutolo R. Resistant hypertension in nondialysis chronic kidney disease. Int J Hypertens 2013. 2013:929183. doi: 10.1155/2013/929183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yuan Q, Liu H, Wu X, Sun Y, Zhou L, Hu J. Predictive value of initial intracranial pressure for refractory intracranial hypertension in persons with traumatic brain injury: A prospective observational study. Brain Inj. 2013;27:664–70. doi: 10.3109/02699052.2013.775497. [DOI] [PubMed] [Google Scholar]
- 4.Jonas BS, Franks P, Ingram DD. Are symptoms of anxiety and depression risk factors for hypertension?. Longitudinal evidence from the National Health and Nutrition Examination Survey I Epidemiologic Follow-up Study. Arch Fam Med. 1997;6:43–9. doi: 10.1001/archfami.6.1.43. [DOI] [PubMed] [Google Scholar]
- 5.Markovitz JH, Matthews KA, Kannel WB, Cobb JL, D’Agostino RB. Psychological predictors of hypertension in the Framingham Study. Is there tension in hypertension? JAMA. 1993;270:2439–43. [PubMed] [Google Scholar]
- 6.Grossman E, Nadler M, Sharabi Y, Thaler M, Shachar A, Shamiss A. Antianxiety treatment in patients with excessive hypertension. Am J Hypertens. 2005;18(9 Pt 1):1174–7. doi: 10.1016/j.amjhyper.2005.03.728. [DOI] [PubMed] [Google Scholar]
- 7.Ginty AT, Carroll D, Roseboom TJ, Phillips AC, de Rooij SR. Depression and anxiety are associated with a diagnosis of hypertension 5 years later in a cohort of late middle-aged men and women. J Hum Hypertens. 2013;27:187–90. doi: 10.1038/jhh.2012.18. [DOI] [PubMed] [Google Scholar]
- 8.Shinn EH, Poston WS, Kimball KT, St Jeor ST, Foreyt JP. Blood pressure and symptoms of depression and anxiety: A prospective study. Am J Hypertens. 2001;14(7 Pt 1):660–4. doi: 10.1016/s0895-7061(01)01304-8. [DOI] [PubMed] [Google Scholar]
- 9.Licht CM, de Geus EJ, Seldenrijk A, van Hout HP, Zitman FG, van Dyck R, et al. Depression is associated with decreased blood pressure, but antidepressant use increases the risk for hypertension. Hypertension. 2009;53:631–8. doi: 10.1161/HYPERTENSIONAHA.108.126698. [DOI] [PubMed] [Google Scholar]
- 10.Yilmaz S, Pekdemir M, Tural U, Uygun M. Comparison of alprazolam versus captopril in high blood pressure: A randomized controlled trial. Blood Press. 2011;20:239–43. doi: 10.3109/08037051.2011.553934. [DOI] [PubMed] [Google Scholar]
- 11.Rogers MP, White K, Warshaw MG, Yonkers KA, Rodriguez-Villa F, Chang G, et al. Prevalence of medical illness in patients with anxiety disorders. Int J Psychiatry Med. 1994;24:83–96. doi: 10.2190/TXM9-EVX8-Q4WT-G03J. [DOI] [PubMed] [Google Scholar]
- 12.Tata LJ, West J, Smith C, Farrington P, Card T, Smeeth L, et al. General population based study of the impact of tricyclic and selective serotonin reuptake inhibitor antidepressants on the risk of acute myocardial infarction. Heart. 2005;91:465–71. doi: 10.1136/hrt.2004.037457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.van Haelst IM, van Klei WA, Doodeman HJ, Kalkman CJ, Egberts TC. Selective serotonin reuptake inhibitors and intraoperative blood pressure. Am J Hypertens. 2012;25:223–8. doi: 10.1038/ajh.2011.194. [DOI] [PubMed] [Google Scholar]
- 14.Linden W, Stossel C, Maurice J. Psychosocial interventions for patients with coronary artery disease: A meta-analysis. Arch Intern Med. 1996;156:745–52. [PubMed] [Google Scholar]
- 15.Patten SB, Williams JV, Lavorato DH, Campbell NR, Eliasziw M, Campbell TS. Major depression as a risk factor for high blood pressure: Epidemiologic evidence from a national longitudinal study. Psychosom Med. 2009;71:273–9. doi: 10.1097/PSY.0b013e3181988e5f. [DOI] [PubMed] [Google Scholar]
- 16.Grassi G. Role of the sympathetic nervous system in human hypertension. J Hypertens. 1998;16(12 Pt 2):1979–87. doi: 10.1097/00004872-199816121-00019. [DOI] [PubMed] [Google Scholar]
- 17.Mancia G. Björn Folkow Award Lecture. The sympathetic nervous system in hypertension. J Hypertens. 1997;15(12 Pt 2):1553–65. doi: 10.1097/00004872-199715120-00056. [DOI] [PubMed] [Google Scholar]
- 18.Xiong GL, Jiang W, Clare R, Shaw LK, Smith PK, Mahaffey KW, et al. Prognosis of patients taking selective serotonin reuptake inhibitors before coronary artery bypass grafting. Am J Cardiol. 2006;98:42–7. doi: 10.1016/j.amjcard.2006.01.051. [DOI] [PubMed] [Google Scholar]
- 19.Toh S, Mitchell AA, Louik C, Werler MM, Chambers CD, Hernández-Díaz S. Selective serotonin reuptake inhibitor use and risk of gestational hypertension. Am J Psychiatry. 2009;166:320–8. doi: 10.1176/appi.ajp.2008.08060817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lespérance F, Frasure-Smith N, Koszycki D, Laliberté MA, van Zyl LT, Baker B, et al. Effects of citalopram and interpersonal psychotherapy on depression in patients with coronary artery disease: The Canadian Cardiac Randomized Evaluation of Antidepressant and Psychotherapy Efficacy (CREATE) trial. JAMA. 2007;297:367–79. doi: 10.1001/jama.297.4.367. [DOI] [PubMed] [Google Scholar]
- 21.Krishnan KR, Doraiswamy PM, Clary CM. Clinical and treatment response characteristics of late-life depression associated with vascular disease: A pooled analysis of two multicenter trials with sertraline. Prog Neuropsychopharmacol Biol Psychiatry. 2001;25:347–61. doi: 10.1016/s0278-5846(00)00168-8. [DOI] [PubMed] [Google Scholar]
- 22.Tecco J, Monreal J, Staner L. Citalopram may reduce sympathoadrenal hyperactivity in elderly depressed patients: An open multicenter study in Belgium and Luxembourg. Psychiatr Danub. 2011;23(Suppl 1):S35–42. [PubMed] [Google Scholar]
- 23.Skop BP, Brown TM. Potential vascular and bleeding complications of treatment with selective serotonin reuptake inhibitors. Psychosomatics. 1996;37:12–6. doi: 10.1016/S0033-3182(96)71592-X. [DOI] [PubMed] [Google Scholar]
- 24.Meier CR, Schlienger RG, Jick H. Use of selective serotonin reuptake inhibitors and risk of developing first-time acute myocardial infarction. Br J Clin Pharmacol. 2001;52:179–84. doi: 10.1046/j.0306-5251.2001.01426.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Seddon MD, Chowienczyk PJ, Brett SE, Casadei B, Shah AM. Neuronal nitric oxide synthase regulates basal microvascular tone in humans in vivo. Circulation. 2008;117:1991–6. doi: 10.1161/CIRCULATIONAHA.107.744540. [DOI] [PubMed] [Google Scholar]
- 26.van Melle JP, de Jonge P, van den Berg MP, Pot HJ, van Veldhuisen DJ. Treatment of depression in acute coronary syndromes with selective serotonin reuptake inhibitors. Drugs. 2006;66:2095–107. doi: 10.2165/00003495-200666160-00005. [DOI] [PubMed] [Google Scholar]
- 27.Shores MM, Pascualy M, Lewis NL, Flatness D, Veith RC. Short-term sertraline treatment suppresses sympathetic nervous system activity in healthy human subjects. Psychoneuroendocrinology. 2001;26:433–9. doi: 10.1016/s0306-4530(01)00002-6. [DOI] [PubMed] [Google Scholar]


