Abstract
The pathogenesis of exercise intolerance in patients with heart failure and preserved ejection fraction (HFpEF) is likely multifactorial. In addition to cardiac abnormalities (diastolic dysfunction, abnormal contractile reserve, chronotropic incompetence), several peripheral abnormalities are likely to be involved. These include abnormal pulsatile hemodynamics, abnormal arterial vasodilatory responses to exercise, and abnormal peripheral O2 delivery, extraction and utilization. The nitrate-nitrite-NO pathway is emerging as a potential target to modify key physiologic abnormalities, including late systolic LV load from arterial wave reflections (which has deleterious short- and long-term consequences for the LV), arterial vasodilatory reserve, muscle O2 delivery, and skeletal muscle mitochondrial function. In a recently completed randomized trial, the administration of a single dose of exogenous inorganic nitrate has been shown exert various salutary arterial hemodynamic effects, ultimately leading to enhanced aerobic capacity in patients with HFpEF. These effects have the potential for both immediate improvements in exercise tolerance and for long-term “disease-modifying” effects. In this review, we provide an overview of key mechanistic contributors to exercise intolerance in HFpEF, and of the potential therapeutic role of drugs that target the nitrate-nitrite-NO pathway.
Keywords: heart failure with preserved ejection fraction, inorganic nitrate, wave reflections, afterload, mitochondria, therapy
Introduction
Heart failure (HF) affects ~2% of the western population1 and remains the most common cause of hospitalization in adults >65 years of age.1 Approximately half of patients with HF have HF with preserved ejection fraction (HFpEF).1–13 Multiple therapies that provide substantial clinical benefit are available in HF with reduced ejection fraction (HFrEF).14 In contrast, effective pharmacologic interventions that improve outcomes in patients with HFpEF are not yet available, and are urgently needed.15 Novel therapeutic approaches should be based on the pathophysiology of the disease, which unfortunately remains incompletely understood. Increasing evidence suggests a role for reduced nitric oxide bioavailability in this condition.16, 17
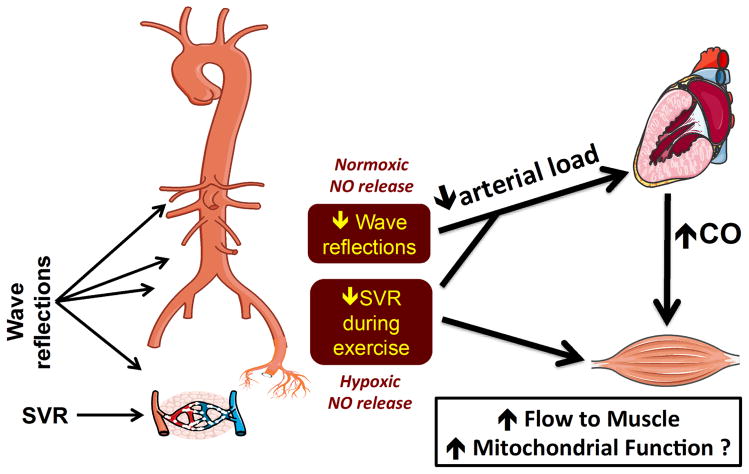
Unfortunately, conventional methods of increasing NO through modulation of the soluble guanylyl cyclase system have been unsuccessful.18 However, the nitrate-nitrite-NO pathway has recently emerged as another therapeutic target for increasing NO signaling, particularly in the presence of hypoxia and acidosis (i.e., in skeletal muscle during exercise). A normoxic mechanism of NO release in conduit arteries has also been reported, which may reduce pulsatile load to the heart. The nitrate-nitrite-NO pathway has the potential target to modify key physiologic abnormalities (late systolic LV load from arterial wave reflections, arterial vasodilator reserve, muscle O2 delivery and utilization, and mitochondrial function), which may lead to both immediate improvements in exercise tolerance and long-term “disease-modifying” effects.
In this review, we provide an overview of peripheral and cardiac abnormalities in HFpEF and the potential role of the nitrate-nitrite-NO pathway as a therapeutic target in HFpEF.
Peripheral mechanisms of exercise intolerance in HFpEF and role of the nitrate-nitrite-NO pathway
Exercise intolerance is the hallmark of HFpEF.19–22 The pathogenesis of exercise intolerance in HFpEF remains incompletely understood. The early pathophysiologic paradigm was that increases in LV filling pressure during exercise were not accompanied by increases in end-diastolic volume, failing to recruit the Frank-Starling mechanism and to augment stroke volume.23 Diastolic dysfunction, with increased diastolic stiffness and impaired relaxation, was proposed to be the key contributor to the pathophysiology of this disease.24 Studies also reported the presence of abnormal contractile reserve and chronotropic incompetence, leading to an abnormal cardiac output reserve.25–27 However, abnormalities in stroke volume reserve25–27 chronotropic incompetence28 or cardiac output reserve26 have not been consistently found in this population (reviewed in 29).
In addition to cardiac abnormalities, HFpEF appears to be associated with key “peripheral” abnormalities, which contribute to exercise intolerance. These include increased arterial stiffness and wave reflections,30 impaired vasodilatory reserve during exercise,31 abnormalities in skeletal muscle fiber type and capillary density,32 and mitochondrial dysfunction.26
Peak O2 uptake (VO2) during exercise, the most widely accepted index of aerobic capacity, is consistently reduced in HFpEF.23, 25–27, 33 Peripheral O2 utilization requires not only an adequate cardiac output during exercise, but also adequate flow redistribution, characterized by blood flow being preferentially directed to exercising skeletal muscle, in order to achieve an adequate matching of perfusion with metabolic demands. This preferential flow distribution is dependent on the exercise-induced reduction in the local resistance of skeletal muscle arterioles (i.e., exercise-induced vasodilation). Therefore, the normal exercise-induced vasodilation in exercising muscle serves 2 important roles: (1) To reduce the “total” (i.e., systemic) vascular resistance during exercise, which reduces LV afterload, promoting a greater cardiac output for any given contractile state; (2) To preferentially divert flow to exercising muscle, promoting matching between metabolic needs and oxygenated blood delivery, thus allowing the “periphery” to optimally “utilize” the cardiac output to maximize oxygen consumption.
In several studies, compared to age-matched hypertensive subjects without HF,28, 33 or age and co-morbidity matched controls,27 patients with HFpEF demonstrated blunted exercise-induced reductions in systemic vascular resistance, indicating reduced vasodilatory reserve.33 This abnormal vasodilatory reserve leads to excessive LV afterload on one hand, and implies abnormal peripheral oxygen delivery on the other. The peripheral ability to redistribute flow to working muscle is a key component of the normal response to exercise,34 and depends on the vasodilatory response in locomotive muscle, allowing it to effectively “compete” for the available cardiac output.34 Given the increase in metabolic demands imposed by active skeletal muscle contraction, vasodilation occurs as an adaptive response to maintain a balance between O2 supply and demand.34, 35 Skeletal muscle vasodilation during exercise allows the local vasculature to overcome humoral and reflex-mediated vasoconstriction.34 Impaired vascular responses within skeletal muscle can have dramatic consequences for O2 extraction, creating a marked imbalance between O2 delivery and requirement in muscle that results in a larger O2 deficit, accentuated intracellular metabolic perturbations and enhanced glycolysis even at low levels of activity (reviewed in 34).
The vasodilator response in exercising muscle is dependent on both endothelium and endothelium-independent pathways.34 As will be discussed below, nitrite-derived NO is an endothelium-independent mediator of hypoxic vasodilation35–37 and increased muscle blood flow during exercise.38, 39
While addressing exercise intolerance in HFpEF is a key therapeutic goal, there is also a need to address long-term underlying abnormalities that contribute to chronic LV remodeling and the long-term course of the disease. A large body of evidence now indicates that late systolic pulsatile load from wave reflections (which are increased in HFpEF30) have adverse long-term consequences on LV remodeling and function.40–42 The pulse wave generated by the LV travels forward in arteries and is partially reflected at sites of impedance mismatch (i.e., bifurcations, points of change in arterial size or wall stiffness, predominantly in middle-sized conduit arteries).42–44 Wave reflections travel back to the heart, merging into a discrete reflected wave that arrives while the LV is still ejecting blood in mid-to-late systole.42, 45 Wave reflections increase the late systolic workload of the LV and profoundly impact the LV loading sequence (late relative to early systolic load).43, 44, 46–48 Experimental animal data demonstrate that late systolic load from wave reflections leads to LV hypertrophy and fibrosis.40 These causal findings are supported by human data demonstrating an association between reflected wave amplitude an LV hypertrophy in the general population49 and between reductions in reflection magnitude and the regression of LV mass during antihypertensive therapy (independent of blood pressure reduction).50 Experimental studies also demonstrate that late systolic load promotes abnormal relaxation.41 In support of these causal findings, wave reflections have been shown to be independently associated with diastolic dysfunction in clinical51, 52 and population-based cohorts.53 Similarly, recent data implicate wave reflection magnitude and late systolic load as a strong predictor of incident heart failure in the general population,48, 54 strongly supporting animal and human mechanistic findings from previous studies and demonstrating the relevance of late systolic load in humans. Nitrate-nitrite-pathway-derived NO production has been shown to favorably impact late systolic load.55, 56 Therefore, in addition to their exercise-enhancing mechanistic effects, interventions that enhance the nitrate-nitrite-NO pathway exert peripheral arterial effects with a potential for chronic “disease-modifying” benefits in HFpEF.
The nitrate–nitrite–NO activation pathway
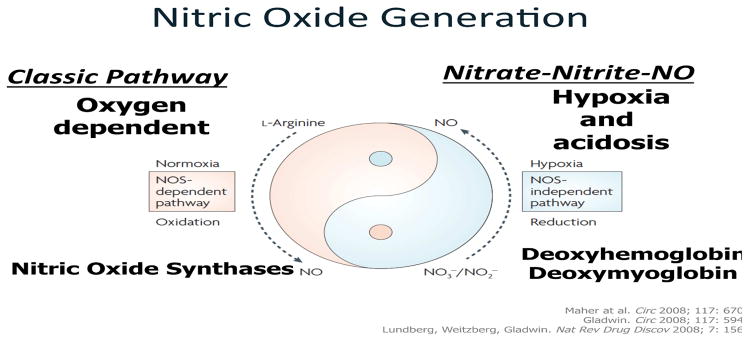
NO formation occurs via 2 known pathways in mammals (Figure 1): (1) NO synthases (NOS) catalyze the formation of NO from L-arginine and O2;57 (2) Circulating nitrate (previously considered an inert product of NO metabolism) can be converted to NO through the nitrate-nitrite-NO pathway, which is largely independent of NOS.39, 57–61
Figure 1.
NO generation via nitric oxide synthase (NOS) or through the nitrate/nitrite/NO pathway. NOS requires molecular oxygen for conversion of L-arginine to NO and citrulline. In the settings of hypoxia, NOS-mediated NO generation is very inefficient.57 On the other hand, the activation of nitrate/nitrite to NO occurs to a greater extent in the setting of ischemia and acidosis,84, 85 and operates largely through NOS-independent mechanisms and is chiefly driven by deoxyhemoglobin.86, 153 This is ideal for HFpEF because is generates NO “when” and “where” it is needed. Reprinted by permission from Macmillan Publishers Ltd: Nature Reviews Drug Discovery. Lundberg, Weitzberg, Gladwin, 2008.57
Under normal conditions, the nitrate-nitrite-NO pathway appears to be dependent primarily on dietary inorganic nitrate intake. Vegetables (leafy green vegetables and beetroot, in particular)57, 61–64 are the main source of inorganic nitrate in the diet (>80%). Nitrate is also directly absorbed in the gastrointestinal tract (without requiring conversion to nitrite), with high bioavailability (>90%)65 and circulates in plasma with a half-life of ~6–8 hours, in contrast to nitrite, which has a short half-life (~30–40 minutes).66–68 Approximately 25% of circulating nitrate is taken up by the salivary glands, where it is reduced to nitrite by the oral flora; the remaining ~75% of circulating nitrate is excreted by the kidneys.69, 70 Oral cavity commensal bacteria reduce nitrate to nitrite, which has a high oral bioavailability (>90%).61, 63, 64 Nitrite present in the blood stream is reduced directly to NO, a reaction catalyzed by several molecules, particularly deoxygenated myoglobin,36, 71–73 and deoxygenated hemoglobin,74 but also xanthine oxidoreductase,75 mitochondrial respiratory chain enzymes76, aldehyde oxidase77, carbonic anhydrase,78 vitamin C79, polyphenols80, 81 and even endothelial NO synthase.82, 83 Importantly, the conversion of nitrite to NO occurs much more rapidly in the context of hypoxia84 and acidosis.85
In sharp contrast to NO production from the nitrate-nitrite-NO pathway, which is enhanced in the presence of hypoxia, NO production via the classic L-arginine pathway is strongly inhibited by hypoxia,83 given its reliance on molecular oxygen (Figure 1). Exercising muscle is characterized by a low pO2,39, 61 which favors the formation of NO from circulating nitrite. Deoxyhemoglobin supports the reduction of nitrite to NO,86 which plays a key role in modulating small resistance vessels (particularly of skeletal muscle), where O2 extraction from the circulation to the tissues is most marked. In these tissues, the O2 saturation of hemoglobin approaches the P50 (the O2 concentration at which half the hem is saturated), an optimum balance point between the greater reductive potential of hem in the R (oxy) state tetramer and the number of un-ligated deoxy-hem sites necessary for nitrite binding (which are more plentiful in the T-state tetramer). This favors conversion rates of nitrite to NO and hence vasodilatation.87, 88 NO by deoxymyoglobin also enhances blood flow to skeletal muscle and matches O2 supply to increased metabolic demands under hypoxic conditions.36 Xanthine oxidoreductase also converts nitrite to NO when O2 levels are low.75, 89 In summary, the endogenous nitrate-nitrite pathway is a physiological effector of hypoxic vasodilation via NO release, which is independent of the L-arginine pathway and largely independent of NO synthase.
NO generation via the nitrate-nitrite-NO pathway is also preferentially activated in the presence of acidosis.85 This mechanism may enhance the selectivity for vasodilation in tissues in which local PO2 is insufficient to support aerobic metabolism, in which lactate production increases, with a resultant fall in pH.39 The role of this pathway in regulating flow to predominantly aerobic vs. anaerobic fibers requires further research.
Inorganic nitrate as therapeutic approach in HFpEF
The arterial hemodynamic characteristics of HFpEF patients (stiff arteries with wide pulse pressure,30 reduced exercise-induced vasodilation,27, 28, 33, 90 and enhanced wave reflections30) dictate a set of “ideal” characteristics for a vasoactive intervention in this condition, namely, one that: (1) Does not significantly reduce mean arterial pressure at rest, avoiding hypotension; (2) Enhances exercise-induced vasodilation to reduce LV afterload during exercise; (3) Has selectivity for enhancing local vasodilation in hypoxic/acidotic environments, in order to match blood flow to metabolic demands (i.e., directing blood flow to exercising muscle); (4) Reduces wave reflections and late systolic load, which likely contributes to LV diastolic dysfunction and chronic maladaptive remodeling.40–42, 50–53 Inorganic nitrate (or nitrite) precisely satisfies these characteristics.
Inorganic nitrate-nitrite-derived NO exerts weak microvascular vasodilatory effects in the absence of hypoxia but acts as a potent arterial vasodilator in the presence of local hypoxemia.39 Concentrations of nitrite (for which nitrate is a precursor) as high as 100–1000 μmol/L are typically required to induce relaxation of arterial rings in vitro.84, 91 Similarly, a lack of vasodilator activity was seen with a concentration of 200 umol/L of nitrite in the forearms of healthy volunteers.92 This situation is, however, different under hypoxic conditions. Maher et al studied 40 volunteers and demonstrated that, during normoxia, forearm arterial blood flow during local infusions of nitrite at incremental doses (from 40 nmol/min to 7.84 μmol/min) increased by a maximum of 64% during normoxia, but it increased by as much as 121% during hypoxia.84 The nitrate-nitrite pathway thus seems ideal for enhancing vasodilation, O2 extraction, and oxygen utilization during exercise. Indeed, inorganic nitrate improves muscle blood flow during exercise.38, 39 Interestingly, in addition to the predominantly hypoxic microvascular dilation (required to reduce local resistance and increase blood flow), normoxic activation of nitrite in conduit vessels has recently been demonstrated.55 This normoxic nitrite activation is likely responsible for the reduction in indices of wave reflections recently reported with inorganic nitrate in HFpEF and in normal volunteers.55, 56
As described below, recent data support the promise of inorganic nitrate in HFpEF, via promotion of exercise-induced vasodilation (ultimately leading to enhanced aerobic capacity), in the absence of blood pressure reductions at rest, while at the same time reducing LV late systolic load.56 This represents an optimal “tailored” approach to abnormal arterial hemodynamics in HFpEF.
Organic vs. Inorganic Nitrate/Nitrite (Table 1)
Table 1.
Key differences between inorganic and organic nitrate
| Organic nitrates | Inorganic nitrate | |
|---|---|---|
| Chemical Structure | Esters of nitric acid (RONO2), where R-represents an organic residue. They are thus small non-polar hydrocarbon chains attached to a nitrooxy-radical (–ONO2). | Salts of nitric acid (nitrate anion bonded to metal cation, such as Na or K). |
| NO release | Tonic | Released preferentially during hypoxia and acidosis (“when” and “where” it is needed) |
| Tolerance | Yes | No |
| Headaches | Yes, often pronounced | No |
| Currently used by clinicians | Yes, variably | No |
| Oral bioavailability | Variable, due to hepatic first-pass metabolism | High oral bioavailability. Do not undergo first-pass metabolism |
| Metabolism and Elimination | Cytochrome P450 system, ALDH-2 | Via the nitrate-nitrite pathway:
|
| Published or ongoing trials in HFpEF |
|
Published: phase IIa single-dose inorganic nitrate trial, demonstrating improvements in aerobic capacity, exercise vasodilatory and cardiac output reserve, late systolic load. Possible improvement in mitochondrial oxidative function.56 Ongoing, single dose:
|
While both organic and inorganic nitrate/nitrite ultimately both act by increasing nitric oxide bioavailability, important differences between the two classes of drugs lead to substantial differences in their action. Regarding their similarities, both classes of agent lead to venodilation.84, 93 Both agents have the potential to decrease the impact of coronary stenoses on the myocardium.93, 94 Yet despite these important similarities, many differences between these two classes exist, as will be described below.
Ingestion and Activation of Inorganic Nitrate/Nitrite vs. organic nitrates
Because of its reliance on the “enterosalivary” circuit, plasma levels of nitrate peak approximately 1–2 hours after ingestion; whereas, plasma levels of nitrite peak later at around 2–4 hour after ingestion.95 The activation of nitrate to nitrite is reliant upon bacteria within the oral cavity and subsequent swallowing of the formed nitrite; therefore, factors that disrupt these processes will lead to lower plasma nitrite concentrations. These include the use of antibiotics, antiseptic mouthwash, or expectoration.96–100 Importantly, inorganic nitrate/nitrite is not subject to significant first pass hepatic metabolism.66, 70
Organic nitrates, on the other hand, do not require bacterial reduction for their activation and are not available from the diet. Commonly used organic nitrates, such as nitroglycerin and isosorbide dinitrate, are subject to extensive first pass metabolism in the liver making their oral bioavailability more variable,70, 101 though this is the not the case for isosorbide mononitrate.102 Once ingested, organic nitrates require activation in the cytochrome P450 system leading to nitric oxide release.70 Alternative activation via mitochondrial aldehyde dehydrogenase has also been demonstrated.70, 103
Tolerance
While the pathophysiology is not fully understood, a major limitation in the use of organic nitrates is the induction of tolerance over a short time period, leading to reduced efficacy of the agent.104 Consequently, nitrates must be dose intermittently, allowing for periods where the subject is relatively untreated.93, 105 Rebound ischemia has been demonstrated following acute nitrate withdrawal,93, 106 suggesting that even this strategy is not without its limitations.
The available information suggests that inorganic nitrate and inorganic nitrite do not induce tolerance. In a study of chronic (8–11 weeks) nitrate administration in hypertensive rats, blood pressure response remained preserved over the duration of therapy.107 Similarly, inorganic nitrate supplementation with beetroot juice led to sustained reductions in blood pressure in hypertensive adults over a month of therapy.108 In addition to blood pressure, studies in healthy volunteers have demonstrated important ergogenic benefits to inorganic nitrate,38, 109–116 which persist through at least two weeks of therapy.117 Moreover, two-weeks of inorganic nitrate led to improved hemodynamic responses to exercise in healthy volunteers.118
Similar data are available for inorganic nitrite, again suggesting that tolerance does not develop following chronic administration. In a primate study, repeated daily bolus administration of intravenous nitrite, on a background of continuous nitrite infusion, continued to reduce blood pressure over 14 days.67 In a study of two-kidney-one-clip hypertensive rats, 4 weeks of oral sodium nitrite persistently reduced blood pressure.119 Finally, a study of oral nitrite supplementation in spontaneously hypertensive rats demonstrated a continuous blood pressure response over one year of therapy.120
These data combine to demonstrate that while organic nitrate therapy is associated with tolerance if given continuously, the same phenomena does not occur with inorganic nitrate/nitrite.
Endothelial Dysfunction
Through related pathways as induced with the development of tolerance,106 the administration of organic nitrates, whether intravenous, transdermal, or orally, has been shown to worsen endothelial function.106, 121–124 As endothelial dysfunction is thought to be a contributing factor to the development of HFpEF,16, 17 avoiding further compromise in endothelial function and nitric oxide bioavailability may be an important goal. Conversely, inorganic nitrate/nitrite do not worsen endothelial function,125, 126 with some reports demonstrating an improvement in endothelial function following the administration of nitrate100, 108, 118, 127, 128 or nitrite.94
Adverse Effects of Organic nitrates vs. Inorganic Nitrate/nitrite
Headache is a common side effect following the administration of organic nitrate,101 and can limit compliance with the medication. In the African-American Heart Failure Trial, nearly 50% of subjects randomized to the organic nitrate-containing arm complained of headache, with approximately one-third developing dizziness.129 Moreover, hypotension can be seen, and may rarely result in syncope.101
Inorganic nitrate is very well tolerated, with no limiting side effects consistently reported in the literature with its oral use.108 When administered in the form of beetroot juice, red urine and stools can be observed.100, 108 The hypotensive effects of nitrate are dose-dependent and fairly mild, averaging −4.4/−1.1 mm Hg in a recent meta-analysis,65 though age may modify the blood pressure response.130
In a recent single-dose cross-over trial in HFpEF, we did not observe any vasoactive symptoms (such as headache) or any change in blood pressure following nitrate ingestion. This suggests that resting hypotension is an unlikely adverse effect of inorganic nitrate in this population.130 Importantly, the lack of a blood pressure response to nitrate has also been shown in both elderly130, 131 and diabetic individuals,126 further suggesting that there may be important differences in nitrate effects in different patient populations.
Inorganic nitrite may have more pronounced hypotensive effects than inorganic nitrate. Even low dose infusions of nitrite can decrease mean arterial pressure significantly,39 with more prolonged infusions and higher doses leading to more pronounced hypotensive effects.66–68 Moreover, as with organic nitrates, a significant proportion of subjects given oral inorganic nitrite developed headache and dizziness, with greater incidence noted with higher doses.66, 132
Another consideration is the short half-life of nitrite, which may lead to nitrite level swings during intermittent administration.133 For oral formulations without enteric coating, the production of NO from nitrite in the acidic environment of the stomach may lead to the production of large amounts of NO soon after administration, which may explain some of the adverse effects seen with this formulation.134 The side effect profile of inhaled sodium nitrite may differ from the profile of the oral formulations, but it needs to be better defined in the HFpEF patient population.
Methemoglobinemia is an uncommon but well recognized risk of nitrite therapy66,68 However, recent studies in PAD suggest that, at dose that can exert adequate vasoactive effects, the risk of clinically-significant methemoglobinemia is very low.132, 135, 136 Importantly, in the only study of chronic (10 weeks) sodium nitrite supplementation, methemoglobin levels did not increase over 3% of total hemoglobin,132 thus remaining in ranges that are generally considered safe.136 Prior studies of intravenous sodium nitrite, however, have led to more significant increases in methemoglobin levels.68 Methemoglobinemia is unlikely to be an important side effect of organic nitrate therapy, although studies are underway in HFpEF, which will provide better information about the incidence of side effects at different doses in patients with HFpEF (see below).
Cancer and inorganic nitrate
There has been concern regarding whether a high nitrate diet may predispose to gastric cancer in humans through conversion to nitrite in the stomach and the generation of N-nitroso compounds.137–139 This is a controversial issue derived from animal studies140, although the relationship between nitrate intake and cancer has not been demonstrated in humans.59, 117, 141 In fact, many studies show either no relationship or even an inverse relationship between a high intake of nitrate and the occurrence of gastric cancer.142, 143,137, 144,145, 146 The Joint FAO/WHO Expert Committee on Food reviewed all the available evidence, but failed to establish a definite link between nitrate intake and risk of developing cancer.147, 148 Furthermore, The World Cancer Research Fund/American Institute of Cancer Research found no evidence linking ingestion of vegetables which are known to be high in nitrate with the development of cancer149.
Effects of inorganic nitrate in HFpEF
We recently performed a randomized double-blinded cross-over trial56 of a single dose of 12.9 mmol of inorganic nitrate (nitrate-rich beet root juice, NR-BRJ) versus a nitrate-depleted placebo (PB) in stable subjects with symptomatic HFpEF.56 Serum NO metabolites were markedly greater after NO3− supplementation (326.0 vs. 10.0 μM, P=0.0003). Nitrate supplementation resulted in a greater peak VO2 (12.6±3.7 versus 11.6±3.1 mL O2/kg/min; P=0.005) and total work performed (55.6±35.3 vs. 49.2±28.9 kJ; P=0.04). Ventilatory threshold (a marker of the cellular anaerobic threshold) was also greater following NO3- supplementation (7.6±1.8 versus 7.0±1.4 mL O2/kg/min, P=0.03). Because total work performed and O2 consumption increased in tandem, exercise efficiency was not different between the interventions. Interestingly, the later effect is different than the effect seen in athletes and younger subjects, among whom exercise efficiency increases,38, 95, 110, 114, 115, 117 demonstrating the importance of characterizing specific adaptations to exercise in this particular patient population.
Inorganic nitrate led to a greater fall in systemic vascular resistance (SVR) at peak exercise (−42% vs. −32%; P=0.03). This was accompanied by a greater increase in cardiac output (change 122 %vs. 89%, P=0.006), increased heart rate (78 vs. 65.6; P=0.001) and a trend towards greater stroke volume increase (22.6 vs. 12.7%, P=0.13). The aortic augmentation index (derived from radial arterial tonometry) was significantly decreased by NO3− supplementation (NO3− 132.2 vs. 141%, P=0.03). There was no significant change in resting blood pressure with NO3− supplementation. This is in contrast to blood pressure-lowering effect in healthy volunteers and drug-naive hypertensive subjects89, 150 and may partially be explained by recent data indicating that the BP-lowering effect of inorganic nitrate is modified by age130 or the renal effects in pathways downstream of the AT1-receptor.151 We also assessed local skeletal muscle mitochondrial oxidative capacity following a standardized forearm exercise protocol and demonstrated a trend towards improved skeletal muscle mitochondrial function following NR-BRJ.
In summary (figure 2), inorganic nitrate increased peak VO2 and total work during a maximal exercise test. It enhanced the exercise vasodilatory reserve, without affecting SVR or blood pressure at rest. It also reduced late systolic LV load, which is implicated in diastolic dysfunction and LV remodeling. Nitrate also led to increased cardiac output during exercise, likely from reduced afterload, although direct myocardial effects might be involved. Finally, in accordance with other studies, our recent pilot data suggest an improvement in mitochondrial oxidative function.113, 152 However, nitrate did not affect the O2 cost of exercise, as has been demonstrated in younger and/or healthier populations38, 109, 112, 115, 117 Although the cross-over design allowed for adequate power to assess physiologic endpoints, this trial was limited by its small sample size, and the inclusion of a predominantly male (88%) and African-American (82%) population.
Figure 2.
Systemic peripheral mechanisms by which inorganic nitrate enhanced aerobic capacity in HFpEF
Other ongoing trials with inorganic nitrate and nitrite
Based on these initial findings, we are currently finalizing a phase IIa dose-response and pharmacokinetic study (NCT02256345) of repeated nitrate supplementation in HFpEF. We are also and initiating a phase IIb cross-over randomized clinical trial of sustained administration of potassium nitrate (KNO3). The Effect of KNO3 Compared to KCl on Oxygen UpTake in HFpEF (KNO3CK OUT HFpEF) trial will enroll 76 subjects, and will assess the effects of a 6-week period of potassium nitrate administration on aerobic capacity (primary endpoint), quality of life, late systolic LV load, myocardial function and various physiologic adaptations to exercise (vasodilatory response to exercise, skeletal muscle phosphocreatine recovery kinetics, muscle tissue perfusion and spatial matching between perfusion and oxidative capacity). Each subject will be exposed to both the active drug (potassium nitrate) and control (potassium chloride) in a randomized, cross-over, blinded design. Subjects will be enrolled with explicit assurance for adequate representation of women and African Americans.
Other phase IIa trials are assessing the hemodynamic effects of single-dose inhaled-nitrite supplementation (NCT02262078) and intravenous sodium nitrite administration in the catheterization laboratory (NCT01932606), are also underway.
Conclusion
Novel therapies for HFpEF are urgently needed. As our understanding of this condition increases, evidence suggests an increasing role for peripheral abnormalities in the pathogenesis of the disease, including abnormal pulsatile load, and reduced exercise-induced vasodilation. Furthermore, given the increased arterial stiffness and preload dependence in this population, excessive reductions in systemic vascular resistance at rest need to be avoided. However, selective vasodilators, such as inorganic nitrate, which can lead to preferential vasodilation at the time of exercise and in the appropriate vascular beds, have great potential in increasing O2 availability in the periphery and ultimately, aerobic capacity. Moreover, evidence suggests that inorganic nitrate also improves late systolic load via normoxic NO production in conduit arteries, which may ultimately exert long-term disease-modifying effects via reductions in maladaptive LV remodeling and improvements in LV function. Modulation of the inorganic nitrate/nitrite pathway thus represents a novel avenue by which to improve exercise capacity in HFpEF.
Footnotes
Compliance with Ethics Guidelines
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest
Julio A. Chirinos has received personal fees from Brystol Myers Squibb, OPKO Healthcare, Fukuda Denshi, Microsoft and Merck, grants from National Institutes of Health, American College of Radiology Network, Fukuda Denshi, Microsoft, Brystol Myers Squibb, and non-financial support from Atcor Medical outside the submitted work. In addition, Dr. Chirinos is named as inventor in a pending University of Pennsylvania patent application for the use of inorganic nitrates/nitrites for the treatment of HFpEF.
Payman Zamani declares that he has no conflict of interest.
References
* of importance
** of major importance
- 1.Lam CS, Donal E, Kraigher-Krainer E, Vasan RS. Epidemiology and clinical course of heart failure with preserved ejection fraction. European journal of heart failure. 2011;13:18–28. doi: 10.1093/eurjhf/hfq121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vasan RS, Benjamin EJ, Levy D. Prevalence, clinical features and prognosis of diastolic heart failure: an epidemiologic perspective. Journal of the American College of Cardiology. 1995;26:1565–74. doi: 10.1016/0735-1097(95)00381-9. [DOI] [PubMed] [Google Scholar]
- 3.Redfield MM, Jacobsen SJ, Burnett JC, Jr, Mahoney DW, Bailey KR, Rodeheffer RJ. Burden of systolic and diastolic ventricular dysfunction in the community: appreciating the scope of the heart failure epidemic. JAMA : the journal of the American Medical Association. 2003;289:194–202. doi: 10.1001/jama.289.2.194. [DOI] [PubMed] [Google Scholar]
- 4.Kitzman DW, Gardin JM, Gottdiener JS, Arnold A, Boineau R, Aurigemma G, Marino EK, Lyles M, Cushman M, Enright PL. Importance of heart failure with preserved systolic function in patients > or = 65 years of age. CHS Research Group. Cardiovascular Health Study. The American journal of cardiology. 2001;87:413–9. doi: 10.1016/s0002-9149(00)01393-x. [DOI] [PubMed] [Google Scholar]
- 5.Devereux RB, Roman MJ, Liu JE, Welty TK, Lee ET, Rodeheffer R, Fabsitz RR, Howard BV. Congestive heart failure despite normal left ventricular systolic function in a population-based sample: the Strong Heart Study. The American journal of cardiology. 2000;86:1090–6. doi: 10.1016/s0002-9149(00)01165-6. [DOI] [PubMed] [Google Scholar]
- 6.Ceia F, Fonseca C, Mota T, Morais H, Matias F, de Sousa A, Oliveira A. Prevalence of chronic heart failure in Southwestern Europe: the EPICA study. European journal of heart failure. 2002;4:531–9. doi: 10.1016/s1388-9842(02)00034-x. [DOI] [PubMed] [Google Scholar]
- 7.Mosterd A, Hoes AW, de Bruyne MC, Deckers JW, Linker DT, Hofman A, Grobbee DE. Prevalence of heart failure and left ventricular dysfunction in the general population; The Rotterdam Study. European heart journal. 1999;20:447–55. [PubMed] [Google Scholar]
- 8.Morgan S, Smith H, Simpson I, Liddiard GS, Raphael H, Pickering RM, Mant D. Prevalence and clinical characteristics of left ventricular dysfunction among elderly patients in general practice setting: cross sectional survey. Bmj. 1999;318:368–72. doi: 10.1136/bmj.318.7180.368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cortina A, Reguero J, Segovia E, Rodriguez Lambert JL, Cortina R, Arias JC, Vara J, Torre F. Prevalence of heart failure in Asturias (a region in the north of Spain) The American journal of cardiology. 2001;87:1417–9. doi: 10.1016/s0002-9149(01)01568-5. [DOI] [PubMed] [Google Scholar]
- 10.Kupari M, Lindroos M, Iivanainen AM, Heikkila J, Tilvis R. Congestive heart failure in old age: prevalence, mechanisms and 4-year prognosis in the Helsinki Ageing Study. J Intern Med. 1997;241:387–94. doi: 10.1046/j.1365-2796.1997.129150000.x. [DOI] [PubMed] [Google Scholar]
- 11.Fonarow GC, Stough WG, Abraham WT, Albert NM, Gheorghiade M, Greenberg BH, O’Connor CM, Sun JL, Yancy CW, Young JB. Characteristics, treatments, and outcomes of patients with preserved systolic function hospitalized for heart failure: a report from the OPTIMIZE-HF Registry. Journal of the American College of Cardiology. 2007;50:768–77. doi: 10.1016/j.jacc.2007.04.064. [DOI] [PubMed] [Google Scholar]
- 12.Yancy CW, Lopatin M, Stevenson LW, De Marco T, Fonarow GC. Clinical presentation, management, and in-hospital outcomes of patients admitted with acute decompensated heart failure with preserved systolic function: a report from the Acute Decompensated Heart Failure National Registry (ADHERE) Database. Journal of the American College of Cardiology. 2006;47:76–84. doi: 10.1016/j.jacc.2005.09.022. [DOI] [PubMed] [Google Scholar]
- 13.Lenzen MJ, Scholte op Reimer WJ, Boersma E, Vantrimpont PJ, Follath F, Swedberg K, Cleland J, Komajda M. Differences between patients with a preserved and a depressed left ventricular function: a report from the EuroHeart Failure Survey. European heart journal. 2004;25:1214–20. doi: 10.1016/j.ehj.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 14.Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Jr, Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi JL, Johnson MR, Kasper EK, Levy WC, Masoudi FA, McBride PE, McMurray JJ, Mitchell JE, Peterson PN, Riegel B, Sam F, Stevenson LW, Tang WH, Tsai EJ, Wilkoff BL American College of Cardiology F, American Heart Association Task Force on Practice G. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Journal of the American College of Cardiology. 2013;62:e147–239. doi: 10.1016/j.jacc.2013.05.019. [DOI] [PubMed] [Google Scholar]
- 15.Oghlakian GO, Sipahi I, Fang JC. Treatment of heart failure with preserved ejection fraction: have we been pursuing the wrong paradigm? Mayo Clin Proc. 2011;86:531–9. doi: 10.4065/mcp.2010.0841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ferrari R, Bohm M, Cleland JG, Paulus WJ, Pieske B, Rapezzi C, Tavazzi L. Heart failure with preserved ejection fraction: uncertainties and dilemmas. European journal of heart failure. 2015;17:665–71. doi: 10.1002/ejhf.304. [DOI] [PubMed] [Google Scholar]
- 17.Paulus WJ, Tschope C. A novel paradigm for heart failure with preserved ejection fraction: comorbidities drive myocardial dysfunction and remodeling through coronary microvascular endothelial inflammation. Journal of the American College of Cardiology. 2013;62:263–71. doi: 10.1016/j.jacc.2013.02.092. [DOI] [PubMed] [Google Scholar]
- 18.Redfield MM, Chen HH, Borlaug BA, Semigran MJ, Lee KL, Lewis G, LeWinter MM, Rouleau JL, Bull DA, Mann DL, Deswal A, Stevenson LW, Givertz MM, Ofili EO, O’Connor CM, Felker GM, Goldsmith SR, Bart BA, McNulty SE, Ibarra JC, Lin G, Oh JK, Patel MR, Kim RJ, Tracy RP, Velazquez EJ, Anstrom KJ, Hernandez AF, Mascette AM, Braunwald E, Trial R. Effect of phosphodiesterase-5 inhibition on exercise capacity and clinical status in heart failure with preserved ejection fraction: a randomized clinical trial. Jama. 2013;309:1268–77. doi: 10.1001/jama.2013.2024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hoekstra T, Lesman-Leegte I, van Veldhuisen DJ, Sanderman R, Jaarsma T. Quality of life is impaired similarly in heart failure patients with preserved and reduced ejection fraction. European journal of heart failure. 2011;13:1013–8. doi: 10.1093/eurjhf/hfr072. [DOI] [PubMed] [Google Scholar]
- 20.Lewis EF, Lamas GA, O’Meara E, Granger CB, Dunlap ME, McKelvie RS, Probstfield JL, Young JB, Michelson EL, Halling K, Carlsson J, Olofsson B, McMurray JJ, Yusuf S, Swedberg K, Pfeffer MA. Characterization of health-related quality of life in heart failure patients with preserved versus low ejection fraction in CHARM. European journal of heart failure. 2007;9:83–91. doi: 10.1016/j.ejheart.2006.10.012. [DOI] [PubMed] [Google Scholar]
- 21.Kitzman DW, Little WC, Brubaker PH, Anderson RT, Hundley WG, Marburger CT, Brosnihan B, Morgan TM, Stewart KP. Pathophysiological characterization of isolated diastolic heart failure in comparison to systolic heart failure. Jama. 2002;288:2144–50. doi: 10.1001/jama.288.17.2144. [DOI] [PubMed] [Google Scholar]
- 22.Phan TT, Shivu GN, Abozguia K, Sanderson JE, Frenneaux M. The pathophysiology of heart failure with preserved ejection fraction: From molecular mechanisms to exercise haemodynamics. Int J Cardiol. 2012;158:337–43. doi: 10.1016/j.ijcard.2011.06.113. [DOI] [PubMed] [Google Scholar]
- 23.Kitzman DW, Higginbotham MB, Cobb FR, Sheikh KH, Sullivan MJ. Exercise intolerance in patients with heart failure and preserved left ventricular systolic function: failure of the Frank-Starling mechanism. Journal of the American College of Cardiology. 1991;17:1065–72. doi: 10.1016/0735-1097(91)90832-t. [DOI] [PubMed] [Google Scholar]
- 24.Zile MR, Baicu CF, Gaasch WH. Diastolic heart failure--abnormalities in active relaxation and passive stiffness of the left ventricle. The New England journal of medicine. 2004;350:1953–9. doi: 10.1056/NEJMoa032566. [DOI] [PubMed] [Google Scholar]
- 25.Maeder MT, Thompson BR, Brunner-La Rocca HP, Kaye DM. Hemodynamic basis of exercise limitation in patients with heart failure and normal ejection fraction. Journal of the American College of Cardiology. 2010;56:855–63. doi: 10.1016/j.jacc.2010.04.040. [DOI] [PubMed] [Google Scholar]
- 26.Bhella PS, Prasad A, Heinicke K, Hastings JL, Arbab-Zadeh A, Adams-Huet B, Pacini EL, Shibata S, Palmer MD, Newcomer BR, Levine BD. Abnormal haemodynamic response to exercise in heart failure with preserved ejection fraction. European journal of heart failure. 2011;13:1296–304. doi: 10.1093/eurjhf/hfr133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Borlaug BA, Melenovsky V, Russell SD, Kessler K, Pacak K, Becker LC, Kass DA. Impaired chronotropic and vasodilator reserves limit exercise capacity in patients with heart failure and a preserved ejection fraction. Circulation. 2006;114:2138–47. doi: 10.1161/CIRCULATIONAHA.106.632745. [DOI] [PubMed] [Google Scholar]
- 28.Ennezat PV, Lefetz Y, Marechaux S, Six-Carpentier M, Deklunder G, Montaigne D, Bauchart JJ, Mounier-Vehier C, Jude B, Neviere R, Bauters C, Asseman P, de Groote P, Lejemtel TH. Left ventricular abnormal response during dynamic exercise in patients with heart failure and preserved left ventricular ejection fraction at rest. Journal of cardiac failure. 2008;14:475–80. doi: 10.1016/j.cardfail.2008.02.012. [DOI] [PubMed] [Google Scholar]
- 29**.Houstis NE, Lewis GD. Causes of exercise intolerance in heart failure with preserved ejection fraction: searching for consensus. Journal of cardiac failure. 2014;20:762–78. doi: 10.1016/j.cardfail.2014.07.010. Excellent review article discussing the mechanisms of exertional intolerance in HFpEF. [DOI] [PubMed] [Google Scholar]
- 30.Weber T, Wassertheurer S, O’Rourke MF, Haiden A, Zweiker R, Rammer M, Hametner B, Eber B. Pulsatile hemodynamics in patients with exertional dyspnea: potentially of value in the diagnostic evaluation of suspected heart failure with preserved ejection fraction. Journal of the American College of Cardiology. 2013;61:1874–83. doi: 10.1016/j.jacc.2013.02.013. [DOI] [PubMed] [Google Scholar]
- 31.Haykowsky MJ, Brubaker PH, John JM, Stewart KP, Morgan TM, Kitzman DW. Determinants of exercise intolerance in elderly heart failure patients with preserved ejection fraction. Journal of the American College of Cardiology. 2011;58:265–74. doi: 10.1016/j.jacc.2011.02.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32**.Kitzman DW, Nicklas B, Kraus WE, Lyles MF, Eggebeen J, Morgan TM, Haykowsky M. Skeletal muscle abnormalities and exercise intolerance in older patients with heart failure and preserved ejection fraction. American journal of physiology Heart and circulatory physiology. 2014;306:H1364–70. doi: 10.1152/ajpheart.00004.2014. This study demonstrates important structural abnormalities within the peripheral skeletal muscles of HFpEF patients including reduced Type I fibers and reduced capillary to fiber ratios, both of which correlated with impaired peak aerobic capacity. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33**.Borlaug BA, Olson TP, Lam CS, Flood KS, Lerman A, Johnson BD, Redfield MM. Global cardiovascular reserve dysfunction in heart failure with preserved ejection fraction. Journal of the American College of Cardiology. 2010;56:845–54. doi: 10.1016/j.jacc.2010.03.077. Important article demonstrating key hemodynamic limitations identified in HFpEF patients. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34**.Poole DC, Hirai DM, Copp SW, Musch TI. Muscle oxygen transport and utilization in heart failure: implications for exercise (in)tolerance. American journal of physiology Heart and circulatory physiology. 2012;302:H1050–63. doi: 10.1152/ajpheart.00943.2011. Excellent review article describing impairments in oxygen transport found in heart failure and their implications for exercise intolerance. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Umbrello M, Dyson A, Feelisch M, Singer M. The key role of nitric oxide in hypoxia: hypoxic vasodilation and energy supply-demand matching. Antioxid Redox Signal. 2013 doi: 10.1089/ars.2012.4979. [DOI] [PubMed] [Google Scholar]
- 36.Totzeck M, Hendgen-Cotta UB, Luedike P, Berenbrink M, Klare JP, Steinhoff HJ, Semmler D, Shiva S, Williams D, Kipar A, Gladwin MT, Schrader J, Kelm M, Cossins AR, Rassaf T. Nitrite regulates hypoxic vasodilation via myoglobin-dependent nitric oxide generation. Circulation. 2012;126:325–34. doi: 10.1161/CIRCULATIONAHA.111.087155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dufour SP, Patel RP, Brandon A, Teng X, Pearson J, Barker H, Ali L, Yuen AH, Smolenski RT, Gonzalez-Alonso J. Erythrocyte-dependent regulation of human skeletal muscle blood flow: role of varied oxyhemoglobin and exercise on nitrite, S-nitrosohemoglobin, and ATP. American journal of physiology Heart and circulatory physiology. 2010;299:H1936–46. doi: 10.1152/ajpheart.00389.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bailey SJ, Winyard P, Vanhatalo A, Blackwell JR, Dimenna FJ, Wilkerson DP, Tarr J, Benjamin N, Jones AM. Dietary nitrate supplementation reduces the O2 cost of low-intensity exercise and enhances tolerance to high-intensity exercise in humans. Journal of applied physiology. 2009;107:1144–55. doi: 10.1152/japplphysiol.00722.2009. [DOI] [PubMed] [Google Scholar]
- 39**.Cosby K, Partovi KS, Crawford JH, Patel RP, Reiter CD, Martyr S, Yang BK, Waclawiw MA, Zalos G, Xu X, Huang KT, Shields H, Kim-Shapiro DB, Schechter AN, Cannon RO, 3rd, Gladwin MT. Nitrite reduction to nitric oxide by deoxyhemoglobin vasodilates the human circulation. Nature medicine. 2003;9:1498–505. doi: 10.1038/nm954. Important article demonstrating increased conversion of nitrite to NO in the context of exercise. [DOI] [PubMed] [Google Scholar]
- 40**.Kobayashi S, Yano M, Kohno M, Obayashi M, Hisamatsu Y, Ryoke T, Ohkusa T, Yamakawa K, Matsuzaki M. Influence of aortic impedance on the development of pressure-overload left ventricular hypertrophy in rats. Circulation. 1996;94:3362–8. doi: 10.1161/01.cir.94.12.3362. This study demonstrates the adverse effects of wave reflections arriving during late-systole and shows greater degrees of hypertrophy and fibrosis associated with late-systolic load. [DOI] [PubMed] [Google Scholar]
- 41**.Gillebert TC, Lew WY. Influence of systolic pressure profile on rate of left ventricular pressure fall. The American journal of physiology. 1991;261:H805–13. doi: 10.1152/ajpheart.1991.261.3.H805. this study demonstrates that, for any given increase in pressure, late systolic load leads to a much greater impairement in ventricular relaxation, compared to early systolic load. [DOI] [PubMed] [Google Scholar]
- 42.Nichols WWORM, Vlachopoulos C. Theoretical, Experimental and Clinical Principles. 6. Hodder Arnold; 2011. McDonald’s blood flow in arteries. [Google Scholar]
- 43.Chirinos JA, Segers P. Noninvasive evaluation of left ventricular afterload: part 1: pressure and flow measurements and basic principles of wave conduction and reflection. Hypertension. 2010;56:555–62. doi: 10.1161/HYPERTENSIONAHA.110.157321. [DOI] [PubMed] [Google Scholar]
- 44.Chirinos JA, Segers P. Noninvasive evaluation of left ventricular afterload: part 2: arterial pressure-flow and pressure-volume relations in humans. Hypertension. 2010;56:563–70. doi: 10.1161/HYPERTENSIONAHA.110.157339. [DOI] [PubMed] [Google Scholar]
- 45.Chirinos JA, Segers P. Noninvasive evaluation of left ventricular afterload: part 2: arterial pressure-flow and pressure-volume relations in humans. Hypertension. 56:563–70. doi: 10.1161/HYPERTENSIONAHA.110.157339. [DOI] [PubMed] [Google Scholar]
- 46.Chirinos JA, Segers P, Rietzschel ER, De Buyzere ML, Raja MW, Claessens T, De Bacquer D, St John Sutton M, Gillebert T. Early and late systolic wall stress differentially relate to myocardial contraction and relaxation in middle-aged adults. The Asklepios study. Hypertension. 2013 doi: 10.1161/HYPERTENSIONAHA.111.00530. In press. [DOI] [PubMed] [Google Scholar]
- 47.Chirinos JA, Segers P, Gillebert TC, Gupta AK, De Buyzere ML, De Bacquer D, St John-Sutton M, Rietzschel ER, Asklepios I. Arterial properties as determinants of time-varying myocardial stress in humans. Hypertension. 2012;60:64–70. doi: 10.1161/HYPERTENSIONAHA.112.190710. [DOI] [PubMed] [Google Scholar]
- 48.Shah SJ, Wasserstrom JA. Increased arterial wave reflection magnitude: a novel form of stage B heart failure? Journal of the American College of Cardiology. 2012;60:2178–81. doi: 10.1016/j.jacc.2012.07.055. [DOI] [PubMed] [Google Scholar]
- 49.Zamani P, Bluemke DA, Jacobs DR, Jr, Duprez DA, Kronmal R, Lilly SM, Ferrari VA, Townsend RR, Lima JA, Budoff M, Segers P, Hannan P, Chirinos JA. Resistive and pulsatile arterial load as predictors of left ventricular mass and geometry: the multi-ethnic study of atherosclerosis. Hypertension. 2015;65:85–92. doi: 10.1161/HYPERTENSIONAHA.114.04333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hashimoto J, Westerhof BE, Westerhof N, Imai Y, O’Rourke MF. Different role of wave reflection magnitude and timing on left ventricular mass reduction during antihypertensive treatment. J Hypertens. 2008;26:1017–24. doi: 10.1097/HJH.0b013e3282f62a9b. [DOI] [PubMed] [Google Scholar]
- 51.Fukuta H, Ohte N, Wakami K, Asada K, Goto T, Mukai S, Tani T, Kimura G. Impact of arterial load on left ventricular diastolic function in patients undergoing cardiac catheterization for coronary artery disease. Circulation journal : official journal of the Japanese Circulation Society. 2010;74:1900–5. doi: 10.1253/circj.cj-10-0283. [DOI] [PubMed] [Google Scholar]
- 52.Weber T, O’Rourke MF, Ammer M, Kvas E, Punzengruber C, Eber B. Arterial stiffness and arterial wave reflections are associated with systolic and diastolic function in patients with normal ejection fraction. American journal of hypertension. 2008;21:1194–202. doi: 10.1038/ajh.2008.277. [DOI] [PubMed] [Google Scholar]
- 53**.Chirinos JA, Segers P, Rietzschel ER, De Buyzere ML, Raja MW, Claessens T, De Bacquer D, St John Sutton M, Gillebert TC, Asklepios I. Early and late systolic wall stress differentially relate to myocardial contraction and relaxation in middle-aged adults: the Asklepios study. Hypertension. 2013;61:296–303. doi: 10.1161/HYPERTENSIONAHA.111.00530. This study demonstrates the relationship between late systolic load (wall stress) and abnormal myocardial relaxation. [DOI] [PubMed] [Google Scholar]
- 54**.Chirinos JA, Kips JG, Jacobs DR, Jr, Brumback L, Duprez DA, Kronmal R, Bluemke DA, Townsend RR, Vermeersch S, Segers P. Arterial wave reflections and incident cardiovascular events and heart failure: MESA (Multiethnic Study of Atherosclerosis) Journal of the American College of Cardiology. 2012;60:2170–7. doi: 10.1016/j.jacc.2012.07.054. This study demonstrates the strong association between wave reflections, which cause late systolic load, and incident heart failure over ~8 years in the MESA cohort. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55*.Omar SA, Fok H, Tilgner KD, Nair A, Hunt J, Jiang B, Taylor P, Chowienczyk P, Webb AJ. Paradoxical normoxia-dependent selective actions of inorganic nitrite in human muscular conduit arteries and related selective actions on central blood pressures. Circulation. 2015;131:381–9. doi: 10.1161/CIRCULATIONAHA.114.009554. discussion 389. this article demonstrates the reduction in augmentation index, a metric of wave reflections, in conduit arteries with nitrite infusion. [DOI] [PubMed] [Google Scholar]
- 56**.Zamani P, Rawat D, Shiva-Kumar P, Geraci S, Bhuva R, Konda P, Doulias PT, Ischiropoulos H, Townsend RR, Margulies KB, Cappola TP, Poole DC, Chirinos JA. The Effect of Inorganic Nitrate on Exercise Capacity in Heart Failure with Preserved Ejection Fraction. Circulation. 2015;131:371–380. doi: 10.1161/CIRCULATIONAHA.114.012957. This study provides the first evidence that targetting the inorganic nitrate-nitrite-NO pathway in HFpEF leads to improvements in aerobic capacity, mediated by improved vasodilatory and cardiac output reserves. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lundberg JO, Weitzberg E, Gladwin MT. The nitrate-nitrite-nitric oxide pathway in physiology and therapeutics. Nature reviews Drug discovery. 2008;7:156–67. doi: 10.1038/nrd2466. [DOI] [PubMed] [Google Scholar]
- 58.Machha A, Schechter AN. Inorganic nitrate: a major player in the cardiovascular health benefits of vegetables? Nutrition reviews. 2012;70:367–72. doi: 10.1111/j.1753-4887.2012.00477.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Tang Y, Jiang H, Bryan NS. Nitrite and nitrate: cardiovascular risk-benefit and metabolic effect. Current opinion in lipidology. 2011;22:11–5. doi: 10.1097/MOL.0b013e328341942c. [DOI] [PubMed] [Google Scholar]
- 60.Weitzberg E, Hezel M, Lundberg JO. Nitrate-nitrite-nitric oxide pathway: implications for anesthesiology and intensive care. Anesthesiology. 2010;113:1460–75. doi: 10.1097/ALN.0b013e3181fcf3cc. [DOI] [PubMed] [Google Scholar]
- 61.Lundberg JO, Carlstrom M, Larsen FJ, Weitzberg E. Roles of dietary inorganic nitrate in cardiovascular health and disease. Cardiovascular research. 2011;89:525–32. doi: 10.1093/cvr/cvq325. [DOI] [PubMed] [Google Scholar]
- 62.Dibble CT, Lima JA, Bluemke DA, Chirinos JA, Chahal H, Bristow MR, Kronmal RA, Barr RG, Ferrari VA, Propert KJ, Kawut SM. Regional left ventricular systolic function and the right ventricle: the multi-ethnic study of atherosclerosis right ventricle study. Chest. 2011;140:310–6. doi: 10.1378/chest.10-1750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rubin MF, Rosas SE, Chirinos JA, Townsend RR. Surrogate markers of cardiovascular disease in CKD: what’s under the hood? Am J Kidney Dis. 2011;57:488–97. doi: 10.1053/j.ajkd.2010.08.030. [DOI] [PubMed] [Google Scholar]
- 64.Durand M, Koistinen R, Chirinos M, Rodriguez JL, Zambrano E, Seppala M, Larrea F. Hormonal evaluation and midcycle detection of intrauterine glycodelin in women treated with levonorgestrel as in emergency contraception. Contraception. 2010;82:526–33. doi: 10.1016/j.contraception.2010.05.015. [DOI] [PubMed] [Google Scholar]
- 65.Siervo M, Lara J, Ogbonmwan I, Mathers JC. Inorganic nitrate and beetroot juice supplementation reduces blood pressure in adults: a systematic review and meta-analysis. The Journal of nutrition. 2013;143:818–26. doi: 10.3945/jn.112.170233. [DOI] [PubMed] [Google Scholar]
- 66.Hunault CC, van Velzen AG, Sips AJ, Schothorst RC, Meulenbelt J. Bioavailability of sodium nitrite from an aqueous solution in healthy adults. Toxicol Lett. 2009;190:48–53. doi: 10.1016/j.toxlet.2009.06.865. [DOI] [PubMed] [Google Scholar]
- 67.Dejam A, Hunter CJ, Tremonti C, Pluta RM, Hon YY, Grimes G, Partovi K, Pelletier MM, Oldfield EH, Cannon RO, 3rd, Schechter AN, Gladwin MT. Nitrite infusion in humans and nonhuman primates: endocrine effects, pharmacokinetics, and tolerance formation. Circulation. 2007;116:1821–31. doi: 10.1161/CIRCULATIONAHA.107.712133. [DOI] [PubMed] [Google Scholar]
- 68.Pluta RM, Oldfield EH, Bakhtian KD, Fathi AR, Smith RK, Devroom HL, Nahavandi M, Woo S, Figg WD, Lonser RR. Safety and feasibility of long-term intravenous sodium nitrite infusion in healthy volunteers. PLoS One. 2011;6:e14504. doi: 10.1371/journal.pone.0014504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Omar SA, Webb AJ. Nitrite reduction and cardiovascular protection. Journal of molecular and cellular cardiology. 2014;73:57–69. doi: 10.1016/j.yjmcc.2014.01.012. [DOI] [PubMed] [Google Scholar]
- 70.Omar SA, Artime E, Webb AJ. A comparison of organic and inorganic nitrates/nitrites. Nitric oxide : biology and chemistry / official journal of the Nitric Oxide Society. 2012;26:229–40. doi: 10.1016/j.niox.2012.03.008. [DOI] [PubMed] [Google Scholar]
- 71.Shiva S, Huang Z, Grubina R, Sun J, Ringwood LA, MacArthur PH, Xu X, Murphy E, Darley-Usmar VM, Gladwin MT. Deoxymyoglobin is a nitrite reductase that generates nitric oxide and regulates mitochondrial respiration. Circulation research. 2007;100:654–61. doi: 10.1161/01.RES.0000260171.52224.6b. [DOI] [PubMed] [Google Scholar]
- 72.Rassaf T, Flogel U, Drexhage C, Hendgen-Cotta U, Kelm M, Schrader J. Nitrite reductase function of deoxymyoglobin: oxygen sensor and regulator of cardiac energetics and function. Circulation research. 2007;100:1749–54. doi: 10.1161/CIRCRESAHA.107.152488. [DOI] [PubMed] [Google Scholar]
- 73.Hendgen-Cotta UB, Merx MW, Shiva S, Schmitz J, Becher S, Klare JP, Steinhoff HJ, Goedecke A, Schrader J, Gladwin MT, Kelm M, Rassaf T. Nitrite reductase activity of myoglobin regulates respiration and cellular viability in myocardial ischemia-reperfusion injury. Proceedings of the National Academy of Sciences of the United States of America. 2008;105:10256–61. doi: 10.1073/pnas.0801336105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Gladwin MT, Kim-Shapiro DB. The functional nitrite reductase activity of the heme-globins. Blood. 2008;112:2636–47. doi: 10.1182/blood-2008-01-115261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Webb A, Bond R, McLean P, Uppal R, Benjamin N, Ahluwalia A. Reduction of nitrite to nitric oxide during ischemia protects against myocardial ischemia-reperfusion damage. Proceedings of the National Academy of Sciences of the United States of America. 2004;101:13683–8. doi: 10.1073/pnas.0402927101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kozlov AV, Staniek K, Nohl H. Nitrite reductase activity is a novel function of mammalian mitochondria. FEBS Lett. 1999;454:127–30. doi: 10.1016/s0014-5793(99)00788-7. [DOI] [PubMed] [Google Scholar]
- 77.Zweier JL, Li H, Samouilov A, Liu X. Mechanisms of nitrite reduction to nitric oxide in the heart and vessel wall. Nitric oxide : biology and chemistry / official journal of the Nitric Oxide Society. 2010;22:83–90. doi: 10.1016/j.niox.2009.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Aamand R, Dalsgaard T, Jensen FB, Simonsen U, Roepstorff A, Fago A. Generation of nitric oxide from nitrite by carbonic anhydrase: a possible link between metabolic activity and vasodilation. American journal of physiology Heart and circulatory physiology. 2009;297:H2068–74. doi: 10.1152/ajpheart.00525.2009. [DOI] [PubMed] [Google Scholar]
- 79.Carlsson S, Wiklund NP, Engstrand L, Weitzberg E, Lundberg JO. Effects of pH, nitrite, and ascorbic acid on nonenzymatic nitric oxide generation and bacterial growth in urine. Nitric oxide : biology and chemistry / official journal of the Nitric Oxide Society. 2001;5:580–6. doi: 10.1006/niox.2001.0371. [DOI] [PubMed] [Google Scholar]
- 80.Gago B, Lundberg JO, Barbosa RM, Laranjinha J. Red wine-dependent reduction of nitrite to nitric oxide in the stomach. Free radical biology & medicine. 2007;43:1233–42. doi: 10.1016/j.freeradbiomed.2007.06.007. [DOI] [PubMed] [Google Scholar]
- 81.Gago B, Nystrom T, Cavaleiro C, Rocha BS, Barbosa RM, Laranjinha J, Lundberg JO. The potent vasodilator ethyl nitrite is formed upon reaction of nitrite and ethanol under gastric conditions. Free radical biology & medicine. 2008;45:404–12. doi: 10.1016/j.freeradbiomed.2008.04.027. [DOI] [PubMed] [Google Scholar]
- 82.Gautier C, van Faassen E, Mikula I, Martasek P, Slama-Schwok A. Endothelial nitric oxide synthase reduces nitrite anions to NO under anoxia. Biochem Biophys Res Commun. 2006;341:816–21. doi: 10.1016/j.bbrc.2006.01.031. [DOI] [PubMed] [Google Scholar]
- 83.Vanin AF, Bevers LM, Slama-Schwok A, van Faassen EE. Nitric oxide synthase reduces nitrite to NO under anoxia. Cell Mol Life Sci. 2007;64:96–103. doi: 10.1007/s00018-006-6374-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84*.Maher AR, Milsom AB, Gunaruwan P, Abozguia K, Ahmed I, Weaver RA, Thomas P, Ashrafian H, Born GV, James PE, Frenneaux MP. Hypoxic modulation of exogenous nitrite-induced vasodilation in humans. Circulation. 2008;117:670–7. doi: 10.1161/CIRCULATIONAHA.107.719591. Important article demonstrating the increased conversion of nitrite to NO in the context of hypoxia. [DOI] [PubMed] [Google Scholar]
- 85*.Modin A, Bjorne H, Herulf M, Alving K, Weitzberg E, Lundberg JO. Nitrite-derived nitric oxide: a possible mediator of ‘acidic-metabolic’ vasodilation. Acta physiologica Scandinavica. 2001;171:9–16. doi: 10.1046/j.1365-201X.2001.00771.x. Important article demonstrating the increased conversion of nitrite to NO in the context of acidemia. [DOI] [PubMed] [Google Scholar]
- 86**.Liu C, Wajih N, Liu X, Basu S, Janes J, Marvel M, Keggi C, Helms CC, Lee AN, Belanger AM, Diz DI, Laurienti PJ, Caudell DL, Wang J, Gladwin MT, Kim-Shapiro DB. Mechanisms of human erythrocytic bioactivation of nitrite. The Journal of biological chemistry. 2015;290:1281–94. doi: 10.1074/jbc.M114.609222. Important article demonstrating the importance of deoxyhemoglobin in catalyzing the reduction of nitrite to nitric oxide. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Huang Z, Shiva S, Kim-Shapiro DB, Patel RP, Ringwood LA, Irby CE, Huang KT, Ho C, Hogg N, Schechter AN, Gladwin MT. Enzymatic function of hemoglobin as a nitrite reductase that produces NO under allosteric control. The Journal of clinical investigation. 2005;115:2099–107. doi: 10.1172/JCI24650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Gladwin MT, Raat NJ, Shiva S, Dezfulian C, Hogg N, Kim-Shapiro DB, Patel RP. Nitrite as a vascular endocrine nitric oxide reservoir that contributes to hypoxic signaling, cytoprotection, and vasodilation. American journal of physiology Heart and circulatory physiology. 2006;291:H2026–35. doi: 10.1152/ajpheart.00407.2006. [DOI] [PubMed] [Google Scholar]
- 89.Ghosh SM, Kapil V, Fuentes-Calvo I, Bubb KJ, Pearl V, Milsom AB, Khambata R, Maleki-Toyserkani S, Yousuf M, Benjamin N, Webb AJ, Caulfield MJ, Hobbs AJ, Ahluwalia A. Enhanced vasodilator activity of nitrite in hypertension: critical role for erythrocytic xanthine oxidoreductase and translational potential. Hypertension. 2013;61:1091–102. doi: 10.1161/HYPERTENSIONAHA.111.00933. [DOI] [PubMed] [Google Scholar]
- 90.Borlaug BA, Nishimura RA, Sorajja P, Lam CS, Redfield MM. Exercise hemodynamics enhance diagnosis of early heart failure with preserved ejection fraction. Circulation Heart failure. 2010;3:588–95. doi: 10.1161/CIRCHEARTFAILURE.109.930701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Furchgott RF, Bhadrakom S. Reactions of strips of rabbit aorta to epinephrine, isopropylarterenol, sodium nitrite and other drugs. J Pharmacol Exp Ther. 1953;108:129–43. [PubMed] [Google Scholar]
- 92.Lauer T, Preik M, Rassaf T, Strauer BE, Deussen A, Feelisch M, Kelm M. Plasma nitrite rather than nitrate reflects regional endothelial nitric oxide synthase activity but lacks intrinsic vasodilator action. Proceedings of the National Academy of Sciences of the United States of America. 2001;98:12814–9. doi: 10.1073/pnas.221381098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Abrams J. Beneficial actions of nitrates in cardiovascular disease. The American journal of cardiology. 1996;77:31C–7C. doi: 10.1016/s0002-9149(96)00186-5. [DOI] [PubMed] [Google Scholar]
- 94.Ingram TE, Fraser AG, Bleasdale RA, Ellins EA, Margulescu AD, Halcox JP, James PE. Low-dose sodium nitrite attenuates myocardial ischemia and vascular ischemia-reperfusion injury in human models. Journal of the American College of Cardiology. 2013;61:2534–41. doi: 10.1016/j.jacc.2013.03.050. [DOI] [PubMed] [Google Scholar]
- 95.Wylie LJ, Kelly J, Bailey SJ, Blackwell JR, Skiba PF, Winyard PG, Jeukendrup AE, Vanhatalo A, Jones AM. Beetroot juice and exercise: pharmacodynamic and dose-response relationships. Journal of applied physiology. 2013;115:325–36. doi: 10.1152/japplphysiol.00372.2013. [DOI] [PubMed] [Google Scholar]
- 96.Govoni M, Jansson EA, Weitzberg E, Lundberg JO. The increase in plasma nitrite after a dietary nitrate load is markedly attenuated by an antibacterial mouthwash. Nitric oxide : biology and chemistry / official journal of the Nitric Oxide Society. 2008;19:333–7. doi: 10.1016/j.niox.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 97.Lundberg JO, Govoni M. Inorganic nitrate is a possible source for systemic generation of nitric oxide. Free radical biology & medicine. 2004;37:395–400. doi: 10.1016/j.freeradbiomed.2004.04.027. [DOI] [PubMed] [Google Scholar]
- 98.Petersson J, Carlstrom M, Schreiber O, Phillipson M, Christoffersson G, Jagare A, Roos S, Jansson EA, Persson AE, Lundberg JO, Holm L. Gastroprotective and blood pressure lowering effects of dietary nitrate are abolished by an antiseptic mouthwash. Free radical biology & medicine. 2009;46:1068–75. doi: 10.1016/j.freeradbiomed.2009.01.011. [DOI] [PubMed] [Google Scholar]
- 99.Kapil V, Haydar SM, Pearl V, Lundberg JO, Weitzberg E, Ahluwalia A. Physiological role for nitrate-reducing oral bacteria in blood pressure control. Free radical biology & medicine. 2013;55:93–100. doi: 10.1016/j.freeradbiomed.2012.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Webb AJ, Patel N, Loukogeorgakis S, Okorie M, Aboud Z, Misra S, Rashid R, Miall P, Deanfield J, Benjamin N, MacAllister R, Hobbs AJ, Ahluwalia A. Acute blood pressure lowering, vasoprotective, and antiplatelet properties of dietary nitrate via bioconversion to nitrite. Hypertension. 2008;51:784–90. doi: 10.1161/HYPERTENSIONAHA.107.103523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Kosoglou T, Patrick JE, Cohen A, Radwanski E, Christopher D, Affrime MB. Pharmacokinetics of isosorbide-5-mononitrate after oral administration of an extended-release mononitrate formulation versus a standard dinitrate formulation. Clinical therapeutics. 1995;17:241–51. doi: 10.1016/0149-2918(95)80022-0. [DOI] [PubMed] [Google Scholar]
- 102.Abshagen UW. Pharmacokinetics of isosorbide mononitrate. The American journal of cardiology. 1992;70:61G–66G. doi: 10.1016/0002-9149(92)90028-w. [DOI] [PubMed] [Google Scholar]
- 103.Chen Z, Zhang J, Stamler JS. Identification of the enzymatic mechanism of nitroglycerin bioactivation. Proceedings of the National Academy of Sciences of the United States of America. 2002;99:8306–11. doi: 10.1073/pnas.122225199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Elkayam U, Kulick D, McIntosh N, Roth A, Hsueh W, Rahimtoola SH. Incidence of early tolerance to hemodynamic effects of continuous infusion of nitroglycerin in patients with coronary artery disease and heart failure. Circulation. 1987;76:577–84. doi: 10.1161/01.cir.76.3.577. [DOI] [PubMed] [Google Scholar]
- 105.Waller DG. Optimal nitrate therapy with a once-daily sustained-release formulation of isosorbide mononitrate. J Cardiovasc Pharmacol. 1999;34(Suppl 2):S21–7. doi: 10.1097/00005344-199908002-00005. discussion S29–31. [DOI] [PubMed] [Google Scholar]
- 106.Munzel T, Daiber A, Mulsch A. Explaining the phenomenon of nitrate tolerance. Circulation research. 2005;97:618–28. doi: 10.1161/01.RES.0000184694.03262.6d. [DOI] [PubMed] [Google Scholar]
- 107.Carlstrom M, Persson AE, Larsson E, Hezel M, Scheffer PG, Teerlink T, Weitzberg E, Lundberg JO. Dietary nitrate attenuates oxidative stress, prevents cardiac and renal injuries, and reduces blood pressure in salt-induced hypertension. Cardiovascular research. 2011;89:574–85. doi: 10.1093/cvr/cvq366. [DOI] [PubMed] [Google Scholar]
- 108.Kapil V, Khambata RS, Robertson A, Caulfield MJ, Ahluwalia A. Dietary nitrate provides sustained blood pressure lowering in hypertensive patients: a randomized, phase 2, double-blind, placebo-controlled study. Hypertension. 2015;65:320–7. doi: 10.1161/HYPERTENSIONAHA.114.04675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Bailey SJ, Fulford J, Vanhatalo A, Winyard PG, Blackwell JR, DiMenna FJ, Wilkerson DP, Benjamin N, Jones AM. Dietary nitrate supplementation enhances muscle contractile efficiency during knee-extensor exercise in humans. Journal of applied physiology. 2010;109:135–48. doi: 10.1152/japplphysiol.00046.2010. [DOI] [PubMed] [Google Scholar]
- 110.Bescos R, Rodriguez FA, Iglesias X, Ferrer MD, Iborra E, Pons A. Acute administration of inorganic nitrate reduces VO(2peak) in endurance athletes. Medicine and science in sports and exercise. 2011;43:1979–86. doi: 10.1249/MSS.0b013e318217d439. [DOI] [PubMed] [Google Scholar]
- 111.Bond V, Jr, Curry BH, Adams RG, Millis RM, Haddad GE. Cardiorespiratory function associated with dietary nitrate supplementation. Appl Physiol Nutr Metab. 2014;39:168–72. doi: 10.1139/apnm-2013-0263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Lansley KE, Winyard PG, Fulford J, Vanhatalo A, Bailey SJ, Blackwell JR, DiMenna FJ, Gilchrist M, Benjamin N, Jones AM. Dietary nitrate supplementation reduces the O2 cost of walking and running: a placebo-controlled study. Journal of applied physiology. 2011;110:591–600. doi: 10.1152/japplphysiol.01070.2010. [DOI] [PubMed] [Google Scholar]
- 113.Larsen FJ, Schiffer TA, Borniquel S, Sahlin K, Ekblom B, Lundberg JO, Weitzberg E. Dietary inorganic nitrate improves mitochondrial efficiency in humans. Cell metabolism. 2011;13:149–59. doi: 10.1016/j.cmet.2011.01.004. [DOI] [PubMed] [Google Scholar]
- 114.Larsen FJ, Weitzberg E, Lundberg JO, Ekblom B. Dietary nitrate reduces maximal oxygen consumption while maintaining work performance in maximal exercise. Free radical biology & medicine. 2010;48:342–7. doi: 10.1016/j.freeradbiomed.2009.11.006. [DOI] [PubMed] [Google Scholar]
- 115.Larsen FJ, Weitzberg E, Lundberg JO, Ekblom B. Effects of dietary nitrate on oxygen cost during exercise. Acta physiologica. 2007;191:59–66. doi: 10.1111/j.1748-1716.2007.01713.x. [DOI] [PubMed] [Google Scholar]
- 116.Coggan AR, Leibowitz JL, Anderson Spearie C, Kadkhodayan A, Thomas DP, Ramamurthy S, Mahmood K, Park S, Waller S, Farmer M, Peterson LR. Acute Dietary Nitrate Intake Improves Muscle Contractile Function in Patients with Heart Failure: A Double-Blind, Placebo-Controlled, Randomized Trial. Circulation Heart failure. 2015 doi: 10.1161/CIRCHEARTFAILURE.115.002141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Vanhatalo A, Bailey SJ, Blackwell JR, DiMenna FJ, Pavey TG, Wilkerson DP, Benjamin N, Winyard PG, Jones AM. Acute and chronic effects of dietary nitrate supplementation on blood pressure and the physiological responses to moderate-intensity and incremental exercise. American journal of physiology Regulatory, integrative and comparative physiology. 2010;299:R1121–31. doi: 10.1152/ajpregu.00206.2010. [DOI] [PubMed] [Google Scholar]
- 118.Lee JS, Stebbins CL, Jung E, Nho H, Kim JK, Chang MJ, Choi HM. Effects of chronic dietary nitrate supplementation on the hemodynamic response to dynamic exercise. American journal of physiology Regulatory, integrative and comparative physiology. 2015;309:R459–66. doi: 10.1152/ajpregu.00099.2015. [DOI] [PubMed] [Google Scholar]
- 119.Montenegro MF, Amaral JH, Pinheiro LC, Sakamoto EK, Ferreira GC, Reis RI, Marcal DM, Pereira RP, Tanus-Santos JE. Sodium nitrite downregulates vascular NADPH oxidase and exerts antihypertensive effects in hypertension. Free radical biology & medicine. 2011;51:144–52. doi: 10.1016/j.freeradbiomed.2011.04.005. [DOI] [PubMed] [Google Scholar]
- 120.Haas M, Classen HG, Thoni H, Classen UG, Drescher B. Persistent antihypertensive effect of oral nitrite supplied up to one year via the drinking water in spontaneously hypertensive rats. Arzneimittel-Forschung. 1999;49:318–23. doi: 10.1055/s-0031-1300421. [DOI] [PubMed] [Google Scholar]
- 121.Thomas GR, DiFabio JM, Gori T, Parker JD. Once daily therapy with isosorbide-5-mononitrate causes endothelial dysfunction in humans: evidence of a free-radical-mediated mechanism. Journal of the American College of Cardiology. 2007;49:1289–95. doi: 10.1016/j.jacc.2006.10.074. [DOI] [PubMed] [Google Scholar]
- 122.Gori T, Mak SS, Kelly S, Parker JD. Evidence supporting abnormalities in nitric oxide synthase function induced by nitroglycerin in humans. Journal of the American College of Cardiology. 2001;38:1096–101. doi: 10.1016/s0735-1097(01)01510-8. [DOI] [PubMed] [Google Scholar]
- 123.Heitzer T, Just H, Brockhoff C, Meinertz T, Olschewski M, Munzel T. Long-term nitroglycerin treatment is associated with supersensitivity to vasoconstrictors in men with stable coronary artery disease: prevention by concomitant treatment with captopril. Journal of the American College of Cardiology. 1998;31:83–8. doi: 10.1016/s0735-1097(97)00431-2. [DOI] [PubMed] [Google Scholar]
- 124.Caramori PR, Adelman AG, Azevedo ER, Newton GE, Parker AB, Parker JD. Therapy with nitroglycerin increases coronary vasoconstriction in response to acetylcholine. Journal of the American College of Cardiology. 1998;32:1969–74. doi: 10.1016/s0735-1097(98)00456-2. [DOI] [PubMed] [Google Scholar]
- 125.Bahra M, Kapil V, Pearl V, Ghosh S, Ahluwalia A. Inorganic nitrate ingestion improves vascular compliance but does not alter flow-mediated dilatation in healthy volunteers. Nitric oxide : biology and chemistry / official journal of the Nitric Oxide Society. 2012;26:197–202. doi: 10.1016/j.niox.2012.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Gilchrist M, Winyard PG, Aizawa K, Anning C, Shore A, Benjamin N. Effect of dietary nitrate on blood pressure, endothelial function, and insulin sensitivity in type 2 diabetes. Free radical biology & medicine. 2013;60:89–97. doi: 10.1016/j.freeradbiomed.2013.01.024. [DOI] [PubMed] [Google Scholar]
- 127.Rammos C, Hendgen-Cotta UB, Sobierajski J, Bernard A, Kelm M, Rassaf T. Dietary nitrate reverses vascular dysfunction in older adults with moderately increased cardiovascular risk. Journal of the American College of Cardiology. 2014;63:1584–5. doi: 10.1016/j.jacc.2013.08.691. [DOI] [PubMed] [Google Scholar]
- 128.Kapil V, Milsom AB, Okorie M, Maleki-Toyserkani S, Akram F, Rehman F, Arghandawi S, Pearl V, Benjamin N, Loukogeorgakis S, Macallister R, Hobbs AJ, Webb AJ, Ahluwalia A. Inorganic nitrate supplementation lowers blood pressure in humans: role for nitrite-derived NO. Hypertension. 2010;56:274–81. doi: 10.1161/HYPERTENSIONAHA.110.153536. [DOI] [PubMed] [Google Scholar]
- 129.Taylor AL, Ziesche S, Yancy C, Carson P, D’Agostino R, Jr, Ferdinand K, Taylor M, Adams K, Sabolinski M, Worcel M, Cohn JN African-American Heart Failure Trial I. Combination of isosorbide dinitrate and hydralazine in blacks with heart failure. The New England journal of medicine. 2004;351:2049–57. doi: 10.1056/NEJMoa042934. [DOI] [PubMed] [Google Scholar]
- 130.Siervo M, Lara J, Jajja A, Sutyarjoko A, Ashor AW, Brandt K, Qadir O, Mathers JC, Benjamin N, Winyard PG, Anning C, Shore A, Gilchrist M. Ageing modifies the effects of beetroot juice supplementation on 24-hour blood pressure variability: An individual participant meta-analysis. Nitric oxide : biology and chemistry / official journal of the Nitric Oxide Society. 2015;47:97–105. doi: 10.1016/j.niox.2015.04.007. [DOI] [PubMed] [Google Scholar]
- 131.Miller GD, Marsh AP, Dove RW, Beavers D, Presley T, Helms C, Bechtold E, King SB, Kim-Shapiro D. Plasma nitrate and nitrite are increased by a high-nitrate supplement but not by high-nitrate foods in older adults. Nutrition research. 2012;32:160–8. doi: 10.1016/j.nutres.2012.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Mohler ER, 3rd, Hiatt WR, Gornik HL, Kevil CG, Quyyumi A, Haynes WG, Annex BH. Sodium nitrite in patients with peripheral artery disease and diabetes mellitus: safety, walking distance and endothelial function. Vasc Med. 2014;19:9–17. doi: 10.1177/1358863X13515043. [DOI] [PubMed] [Google Scholar]
- 133.Greenway FL, Predmore BL, Flanagan DR, Giordano T, Qiu Y, Brandon A, Lefer DJ, Patel RP, Kevil CG. Single-dose pharmacokinetics of different oral sodium nitrite formulations in diabetes patients. Diabetes Technol Ther. 2012;14:552–60. doi: 10.1089/dia.2011.0291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Pinheiro LC, Montenegro MF, Amaral JH, Ferreira GC, Oliveira AM, Tanus-Santos JE. Increase in gastric pH reduces hypotensive effect of oral sodium nitrite in rats. Free radical biology & medicine. 2012;53:701–9. doi: 10.1016/j.freeradbiomed.2012.06.001. [DOI] [PubMed] [Google Scholar]
- 135.Maher AR, Arif S, Madhani M, Abozguia K, Ahmed I, Fernandez BO, Feelisch M, O’Sullivan AG, Christopoulos A, Sverdlov AL, Ngo D, Dautov R, James PE, Horowitz JD, Frenneaux MP. Impact of chronic congestive heart failure on pharmacokinetics and vasomotor effects of infused nitrite. British journal of pharmacology. 2013;169:659–70. doi: 10.1111/bph.12152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Wright RO, Lewander WJ, Woolf AD. Methemoglobinemia: etiology, pharmacology, and clinical management. Annals of emergency medicine. 1999;34:646–56. doi: 10.1016/s0196-0644(99)70167-8. [DOI] [PubMed] [Google Scholar]
- 137.Forman D, Al-Dabbagh S, Doll R. Nitrates, nitrites and gastric cancer in Great Britain. Nature. 1985;313:620–5. doi: 10.1038/313620a0. [DOI] [PubMed] [Google Scholar]
- 138.Sindelar JJ, Milkowski AL. Human safety controversies surrounding nitrate and nitrite in the diet. Nitric oxide : biology and chemistry / official journal of the Nitric Oxide Society. 2012;26:259–66. doi: 10.1016/j.niox.2012.03.011. [DOI] [PubMed] [Google Scholar]
- 139.Weitzberg E, Lundberg JO. Novel aspects of dietary nitrate and human health. Annu Rev Nutr. 2013;33:129–59. doi: 10.1146/annurev-nutr-071812-161159. [DOI] [PubMed] [Google Scholar]
- 140.Eichholzer M, Gutzwiller F. Dietary nitrates, nitrites, and N-nitroso compounds and cancer risk: a review of the epidemiologic evidence. Nutrition reviews. 1998;56:95–105. doi: 10.1111/j.1753-4887.1998.tb01721.x. [DOI] [PubMed] [Google Scholar]
- 141.Lundberg JO, Weitzberg E, Cole JA, Benjamin N. Nitrate, bacteria and human health. Nature reviews Microbiology. 2004;2:593–602. doi: 10.1038/nrmicro929. [DOI] [PubMed] [Google Scholar]
- 142.Al-Dabbagh S, Forman D, Bryson D, Stratton I, Doll R. Mortality of nitrate fertiliser workers. British journal of industrial medicine. 1986;43:507–15. doi: 10.1136/oem.43.8.507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Fandrem SI, Kjuus H, Andersen A, Amlie E. Incidence of cancer among workers in a Norwegian nitrate fertiliser plant. British journal of industrial medicine. 1993;50:647–52. doi: 10.1136/oem.50.7.647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Powlson DS, Addiscott TM, Benjamin N, Cassman KG, de Kok TM, van Grinsven H, L’Hirondel JL, Avery AA, van Kessel C. When does nitrate become a risk for humans? Journal of environmental quality. 2008;37:291–5. doi: 10.2134/jeq2007.0177. [DOI] [PubMed] [Google Scholar]
- 145.van Loon AJ, Botterweck AA, Goldbohm RA, Brants HA, van Klaveren JD, van den Brandt PA. Intake of nitrate and nitrite and the risk of gastric cancer: a prospective cohort study. British journal of cancer. 1998;78:129–35. doi: 10.1038/bjc.1998.454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.McKnight GM, Duncan CW, Leifert C, Golden MH. Dietary nitrate in man: friend or foe? The British journal of nutrition. 1999;81:349–58. doi: 10.1017/s000711459900063x. [DOI] [PubMed] [Google Scholar]
- 147.Mensinga TT, Speijers GJ, Meulenbelt J. Health implications of exposure to environmental nitrogenous compounds. Toxicological reviews. 2003;22:41–51. doi: 10.2165/00139709-200322010-00005. [DOI] [PubMed] [Google Scholar]
- 148.Speijers GBP. Nitrate. Food Additives Series Geneva: Joint FAO/WHO Expert Committee on Food Additives. 2003 [Google Scholar]
- 149.Wiseman M. The second World Cancer Research Fund/American Institute for Cancer Research expert report. Food, nutrition, physical activity, and the prevention of cancer: a global perspective. The Proceedings of the Nutrition Society. 2008;67:253–6. doi: 10.1017/S002966510800712X. [DOI] [PubMed] [Google Scholar]
- 150.Larsen FJ, Ekblom B, Sahlin K, Lundberg JO, Weitzberg E. Effects of dietary nitrate on blood pressure in healthy volunteers. The New England journal of medicine. 2006;355:2792–3. doi: 10.1056/NEJMc062800. [DOI] [PubMed] [Google Scholar]
- 151.Gao X, Yang T, Liu M, Peleli M, Zollbrecht C, Weitzberg E, Lundberg JO, Persson AE, Carlstrom M. NADPH Oxidase in the Renal Microvasculature Is a Primary Target for Blood Pressure-Lowering Effects by Inorganic Nitrate and Nitrite. Hypertension. 2014 doi: 10.1161/HYPERTENSIONAHA.114.04222. [DOI] [PubMed] [Google Scholar]
- 152.Clerc P, Rigoulet M, Leverve X, Fontaine E. Nitric oxide increases oxidative phosphorylation efficiency. Journal of bioenergetics and biomembranes. 2007;39:158–66. doi: 10.1007/s10863-007-9074-1. [DOI] [PubMed] [Google Scholar]
- 153.Tsuchiya K, Kanematsu Y, Yoshizumi M, Ohnishi H, Kirima K, Izawa Y, Shikishima M, Ishida T, Kondo S, Kagami S, Takiguchi Y, Tamaki T. Nitrite is an alternative source of NO in vivo. American journal of physiology Heart and circulatory physiology. 2005;288:H2163–70. doi: 10.1152/ajpheart.00525.2004. [DOI] [PubMed] [Google Scholar]
- 154.Zakeri R, Levine JA, Koepp GA, Borlaug BA, Chirinos JA, LeWinter M, VanBuren P, Davila-Roman VG, de Las Fuentes L, Khazanie P, Hernandez A, Anstrom K, Redfield MM. Nitrate’s effect on activity tolerance in heart failure with preserved ejection fraction trial: rationale and design. Circulation Heart failure. 2015;8:221–8. doi: 10.1161/CIRCHEARTFAILURE.114.001598. [DOI] [PMC free article] [PubMed] [Google Scholar]