Abstract
Objective
This aim of this study was to characterize trends in alcohol-related hospital admissions among middle-aged and older adults from 1993 to 2010 in relation to age, gender, race, and cohort membership.
Method
This study utilized repeated cross-sectional data from the Nationwide Inpatient Sample. Using alcohol-related classified admissions, yearly rates and longitudinal trends of alcohol-related inpatient hospitalizations based on age, period, birth cohort, gender, and race were estimated.
Results
Among those aged 45 and older, admissions rose from an estimated 610,634 to more than 1,134,876, and rates of any alcohol-related diagnosis also increased from 1993 to 2010. Rates for men were consistently higher than women, and rates for Blacks were higher than Whites. Age was associated with decreasing rates, but post–World War II cohorts displayed higher rates over time.
Discussion
Rates of alcohol-related admissions are increasing among adults above age 45, which may be a function of cohort effects. Training the health care workforce is crucial to respond to this trend.
Keywords: alcohol, epidemiology, health services, trends, cohorts, older adult
Introduction
Substance use disorders (Han, Gfroerer, Colliver, & Penne, 2009; Patterson & Jeste, 1999) and treatment need (Gfroerer, Penne, Pemberton, & Folsom, 2003; Substance Abuse and Mental Health Services Administration, 2011) among older adults are growing and expected to increase in coming years as members of the baby boom generation (born between 1946 and 1964) and subsequent cohorts reach old age. The post–World War II generation is unique in its size and in the fact that it experienced emerging adulthood during a period of more permissive attitudes regarding the use of substances, including alcohol (Johnson & Gerstein, 2000). The period of the 1960s and 1970s was also distinctive for high prevalence of alcohol and drug use in our nation’s history. Forty years later, this generation and those that have followed are reaching old age. Despite the demographic importance of the baby boomer generation and its potential for elevated risk of alcohol use disorders, there has been little research disentangling the effect of age and cohort on alcohol-related morbidity and consequential acute care hospital use.
Unhealthy alcohol use can lead to hospitalization among older adults through two pathways. Chronic heavy alcohol use has direct detrimental effects on health in the form of alcohol-related conditions (e.g., alcoholic cirrhosis) and diseases known to be associated with alcohol use including various cancers, hemorrhagic stroke, and chronic pancreatitis (Rehm et al., 2003). Alcohol use also leads to hospitalizations of older adults through its acute effects such as medication interactions (Moore, Whiteman, & Ward, 2007), alcohol-associated injury (Sorock, Chen, Gonzalgo, & Baker, 2006), and alcohol-involved suicidal behavior (Blow, Brockmann, & Barry, 2004; Rehm et al., 2003)
Research specific to alcohol-related hospitalization among older adults is scant. The preponderance of studies conducted in this area has explored the impact of alcohol use on specific illnesses among older adults or overall hospitalizations attributable to alcohol, but not both. An early study was conducted by Adams, Zhong, Barboriak, and Rimm (1993) using Medicare claims data from 1989. The study is notable for estimating rates of alcohol-related hospitalization among those aged 65 and older that were similar to rates for myocardial infarction (54.7 per 10,000 for men, 14.8 per 10,000 for women).
More recent research has examined rates of alcohol-related admission using data from the National Hospital Discharge Survey (NHDS) from 1988 to 2007. For “first listed” diagnosis, researchers estimated a rate increase from 26.3 to 31.8 per 10,000 for those 45 to 64 and a decrease from 15.8 to 12.5 for those 65 and older. Conversely, rates increased from 69.3 to 104 (ages 45–64) and 57.1 to 70 (65+) for “all-listed” diagnoses. These results suggest that rates have increased over time (Chen & Yi, 2010). However, these studies have not separated the effects of age, period, and cohort necessary to understand potential changes in service use demand.
Existing evidence indicates that rates of substance use disorder (Han et al., 2009), treatment need (Gfroerer et al., 2003), and services use (Sacco, Kuerbis, Goge, & Bucholz, 2013; Substance Abuse and Mental Health Services Administration, 2011) are increasing among older adults. Although recent studies suggest that older adults are presenting for treatment with multiple substances of use, alcohol remains the most commonly used drug among older adults (Moore et al., 2009). This growing population of older adults with substance use disorders may be at higher risk of chronic and acute alcohol-related health consequences (Durnas, Loi, & Cusack, 1990), putting them at risk of alcohol-related hospitalization.
This is the first study that we are aware of that uses a longer term (18 years) nationally representative all-payer hospital sample to characterize trends in rates of alcohol-related hospitalizations and to disentangle the effects of the time period, age of individuals, and birth cohort effects. We hypothesize that the increase in rates of alcohol-related hospitalizations among older adults observed by other studies will be confirmed, and that baby boomer cohorts will have an elevated risk of hospitalization compared with previous generations.
Method
Sample
Data for this analysis come from the Nationwide Inpatient Sample (NIS), part of the Healthcare Cost and Utilization Project (HCUP) created by the Agency for Healthcare Research and Quality (AHRQ; HCUP, 2012). The NIS is an approximately 20% national probability sample of short stay (average < 30 days) community hospitals in the United States, including short-term general and specialty hospitals, public hospitals, and academic medical centers. These data are unique for their size and organization. The sample contains between 6.5 and 8 million discharges per year and utilizes a sampling design that allows for the estimation of population estimates for each year and over time (HCUP, 2012). We used the 1993 through 2010 NIS trends files to estimate the total number of alcohol-related hospitalizations in the United States during those years. Data were analyzed longitudinally beginning with the 1993 sample because of changes in the sample make comparisons to data before 1993 problematic (HCUP, 1993–2010). Using U.S. Census data on the total population, we estimated yearly rates of alcohol-related hospitalization.
Variables
Cases of alcohol-related admissions were coded using AHRQ Clinical Classification Software (CCS) for the International Classification of Diseases, Version 9 (ICD-9) codes, which are included in the billing records reported by participating states to the NIS (Elixhauser & McCarthy, 1996). We coded alcohol-related hospitalization variables as any alcohol-related admission. Alcohol-related admission included alcohol withdrawal, including delirium tremens, alcohol intoxication, alcohol-related psychosis and hallucinations, alcohol abuse, alcohol dependence, alcohol-related liver disease, and alcohol-related dementia. An admission was considered an alcohol-related admission if any 1 of the 15 alcohol-related diagnoses or alcohol-related procedures were coded on discharge.
The gender and race of the person admitted were coded using categories developed by the HCUP study group and were used in this analysis to identify gender and race differences in trends of alcohol-related admission. Racial categories provided by HCUP are as follows: White, Black, Hispanic, Asian or Pacific Islander, and Native American. Individuals coded as “other” in the NIS data and data for years before 2000 were excluded from this analysis as specific population denominator data were not available from the census bureau with which to derive rates. SAS Software Version 9.2 (SAS Institute Inc, 2008) was used to code the data. Finally, a variable for age of the person admitted to hospital and the survey year to quantify the patient age and period of the admission. By subtracting the age from the year, we estimated the rate by 5-year birth cohort.
Analysis
For the analysis of trends in the demographics of alcohol-related admission, SAS PROC SURVEYFREQ was used to estimate the number of admissions adjusting the estimates for the sampling design using weights, strata, and sampling units. SAS PROC GLM was used to analyze trends using two constructed data sets of rates, one by year stratified by ages and gender (n = 36) and the other by year stratified by age and race/ethnicity (n = 55). To assess gender differences in time trends, models were estimated using time coded in years, female gender, and the interaction of linear time coded by year and gender. We conducted a similar analysis for race in which we dummy-coded racial categories and estimated models that included time in years, racial categories, and an interaction term between race and time. These models were conducted for the two age groups, middle-aged and older adult based on rates of alcohol-related admission.
Then, age, period, cohort (APC) analysis was conducted to understand the effects of these parameters on alcohol-related admissions. For APC, we utilized the intrinsic estimator (IE; Yang, Schulhofer-Wohl, Fu, & Land, 2008) method, which is implemented as a statistical add-on in Stata (Statacorp, 2013). In APC, there is an inherent linear dependency between age, period, and cohort, that is, Period = Age + Cohort, also known as the identification problem. Simply put, when APC are entered into a single regression model, it is not possible to derive unique coefficient estimates. In the past, researchers have addressed this problem by imposing constraints to allow for identifiability, but these constraints are problematic in that estimates may vary based on the type of constraint chosen (Keyes & Miech, 2013; Yang et al., 2008). IE addresses the collinearity between age, period, and cohort effects without introducing bias in model parameter estimates. The IE method is a special form of principal component estimator, but one in which the coefficients of the principal components are not directly interpreted as the effects on the parameters. An extra step of inverse orthonormal transformation brings the coefficient estimates to the original space of age, period, and cohort variables.
Results
Age Trends
Figure 1 displays the age distribution among those 45 years and older for 1995, 2000, 2005, and 2010 as well as rates by cohorts at different ages. Each cell reports the rate per 10,000 people in the U.S. population based on census estimates. For alcohol-related admissions, the distribution of rates appears to change, with a growth in rates of admissions among middle-aged and young-old under age 60. Looking at cohort differences in Figure 1, rates of alcohol-related admissions show increases for each subsequent cohort when they reach the same age.
Figure 1.
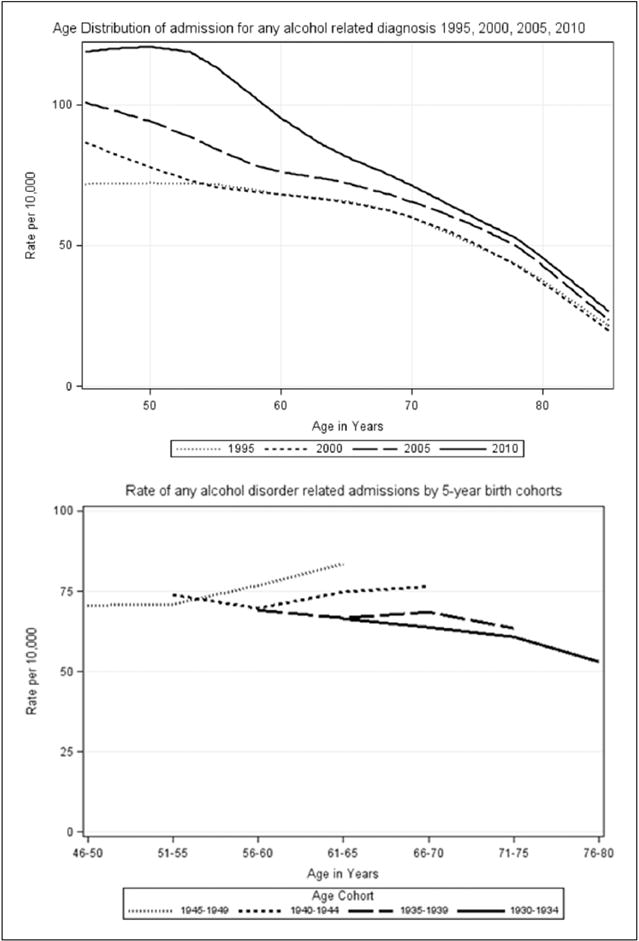
Age and cohort distribution of alcohol-related admissions, 1995, 2000, 2005, and 2010.
Gender and Race Differences
Rates of alcohol-related admission among men and women displayed increasing trends over time. Figure 2 provides a graphical display of trends divided by gender and age group (45–64 and 65+). To test for linear trends and gender differences, we estimated regression models using time (years) and gender and their interaction as independent variable of rates. Among those 45–64 and 65+, rates of alcohol-related admissions were significantly lower in women than men (See Table 1). The trends for alcohol-related admission were notable as they increased over time among those 45 to 64 years old (b = 3.25; t = 15.87; p < .001) and 65+ years old (b = 0.88; t = 8.84; p < .001), although this increasing time trend was steeper in the middle-aged admission rate. Using an interaction term, we tested for differences in linear trends in rate between men and women. For rates of alcohol-related admission, there was a slower increase among women than men for rates among those 45 to 64 (b = −1.79; t = −6.18; p < .001) and among those 65+ (b = −0.68; t = −4.82; p < .001).
Figure 2.
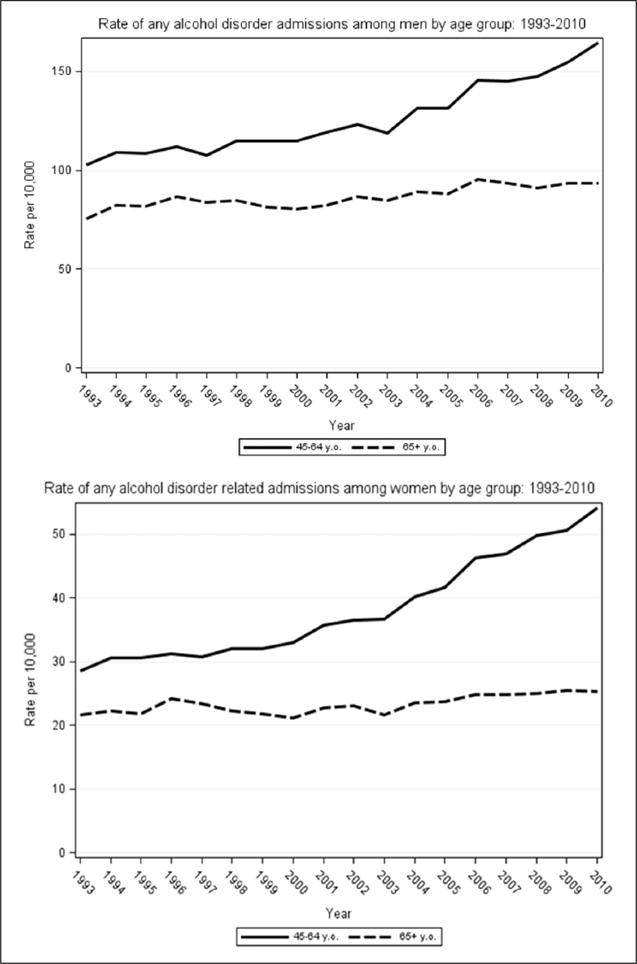
Rates of alcohol-related diagnoses by gender 1993–2010.
Table 1.
Statistical Tests of Trend by Gender and Race/Ethnicity.
| Rate of any alcohol-related diagnosis
|
||||
|---|---|---|---|---|
| b | SE | t | p | |
| Gender, n = 36a | ||||
| 45–64b | ||||
| Time | 3.25 | 0.205 | 15.87 | <.001 |
| Female | −72.44 | 2.89 | −25.04 | <.001 |
| Time × Female | −1.79 | 0.29 | −6.18 | <.001 |
| 65+b | ||||
| Time | 0.88 | 0.09 | 8.84 | <.001 |
| Female | −57.28 | 1.40 | −40.94 | <.001 |
| Time × Female | −0.68 | 0.14 | −4.82 | <.001 |
| Race/ethnicity, n = 55c | ||||
| 45–64b | ||||
| Time | 3.83 | 1.01 | 3.78 | <.001 |
| Black | 62.87 | 8.49 | 7.40 | <.001 |
| Hispanic | 22.30 | 8.49 | 2.63 | .012 |
| Asian/PI | −34.84 | 8.49 | −4.10 | <.001 |
| Native Amer. | −8.22 | 8.49 | −0.97 | .338 |
| Time × Black | 0.46 | 1.44 | 0.32 | .74 |
| Time × Hispanic | −2.65 | 1.44 | −1.85 | .071 |
| Time × Asian/PI | −3.10 | 1.44 | −2.16 | .036 |
| Time × Native | 3.15 | 1.44 | 2.20 | .033 |
| 65+b | ||||
| Time | 1.29 | 2.85 | 11.07 | <.001 |
| Black | 21.40 | 4.04 | 5.30 | <.001 |
| Hispanic | 14.99 | 4.04 | 3.71 | <.001 |
| Asian/PI | −22.60 | 4.04 | −5.60 | <.001 |
| Native Amer. | −0.44 | 4.04 | −3.74 | <.001 |
| Time × Black | −0.16 | 0.68 | 0.23 | .882 |
| Time × Hispanic | −0.45 | 0.68 | −1.31 | .1977 |
| Time × Asian/PI | −0.44 | 0.68 | −1.44 | .1566 |
| Time × Native | −0.04 | 0.68 | 4.18 | <.001 |
Note. SE = standard error; PI = Pacific Islander.
Sample is based on rate above 18 years (1993–2010) for each gender.
Models are stratified and run separately by age group.
Figure 3 displays trends in alcohol-related admissions for different racial categories. For race groups, we derived rates by age for 2000–2010, as population denominator data were not available from the Census Bureau stratified by age and race. Results of the models examining time (years), race, and race by time on admissions over time are reported in Table 1. Consistent with the gender models, there was an increasing linear trend rate of alcohol-related admissions among race groups within both age groups.
Figure 3.
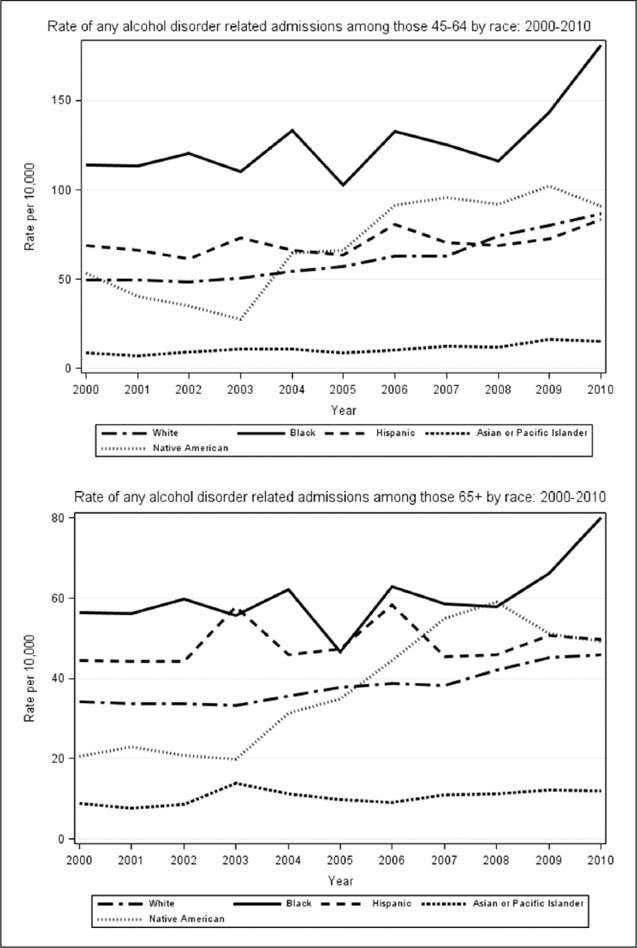
Rates of alcohol-related diagnoses by race and age group 2000–2010.
Racial differences were pronounced for alcohol-related admissions (see Table 1). Rates among African Americans (b = 62.87; t = 7.40; p < .001) and Hispanics (b = 22.30; t = 2.63; p = .012) were significantly higher than among Whites for those in the 45 to 64 age group. Rates among Asian/Pacific Islanders were lower (b = −34.84; t = −4.10; p < .001) within this same age group. Although there was no difference in the rate of alcohol-related admission between Whites and Native Americans, rates increased at a faster rate at ages 45 to 64 (b = 3.15; t = 2.20; p = .033). Among those aged 65 and older, rates were higher among African Americans (b = 21.40; t = 5.30; p < .001) and Hispanic individuals (b = 14.99; t = 3.71; p < .001), but lower in Asian/Pacific Islanders (b = −22.60; t = −5.60; p < .001) and Native Americans (b = −.44; t = 3.74; p < .001). Whereas there was a positive trend for alcohol-related admission among American Indians aged 45 to 64 years old, we found a slightly slower rate of increase in rates among American Indians aged 65 and older (b = −.04; t = 4.18; p < .001).
APC Model
Using rates for Years 1995, 2000, 2005, and 2010, we estimated APC models for alcohol-related admissions. These models were able to parse out the contributions of cohort membership, age, and time period in rates. Figure 4 provides graphical display of linear regression coefficients by age, period, and cohort. Model estimates are linear regression coefficients of rates, and the reference group for each variable (age, period, and cohort) is the mean for that variable. For instance, the reference category for age group would be the mean value across age categories.
Figure 4.
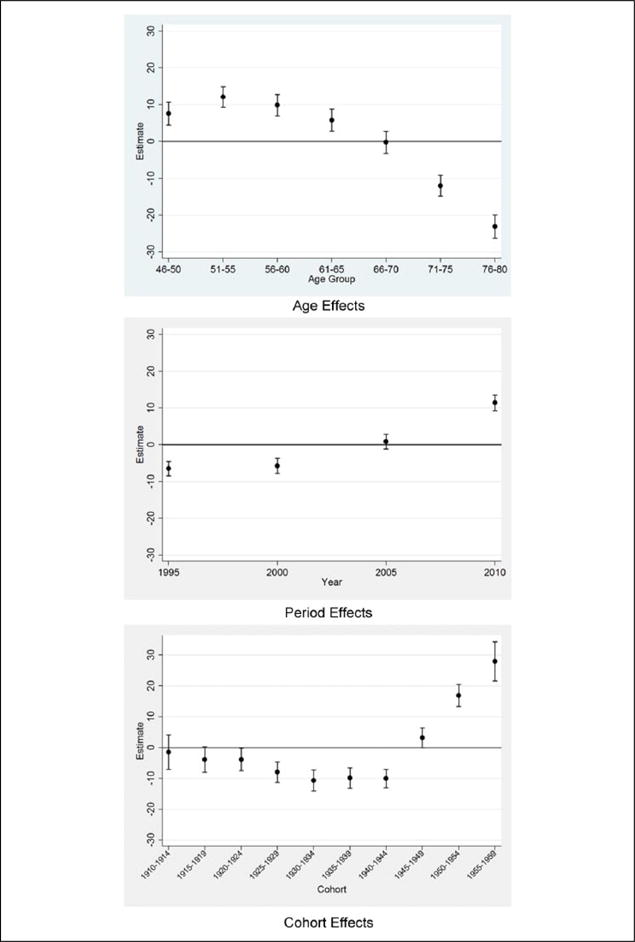
Age–period–cohort model.
Note. The reference group for age, period, and cohort coefficients is the mean rate of age, period, and cohort, respectively.
Age effects for alcohol-related admissions were also present. Age groups under age 65 demonstrated significantly higher rates of alcohol-related admission, and age groups above 70 demonstrated significantly lower rates. We also found a positive cohort effect for alcohol-related admission, as individuals in later post-war cohorts (1950–1954–1955–1959, and 1960–1964) showed significantly higher rates of admission, and those born in prewar and World War II cohorts (1920–1924–1925–1929–1930–1934–1935–1939–1940–1944) had significantly lower rates. Alcohol-related admission rates displayed a positive time trend, with the Years 1995 and 2000 significantly lower than the mean rate and 2010 significantly greater than the mean rate.
Discussion
This study adds to evidence that younger cohorts who are aging may have greater morbidity related to alcohol and other substance use and provides support for the notion that increasing disorder and service use are not simply a function of growing numbers of older adults, but of the rate of diagnosis in the population. Rates of alcohol-related hospitalizations were higher among individuals born in later cohorts (i.e., baby boom) and lower than average among individuals during World War II or before (1945 or earlier). Age effects were present with rates of hospitalizations decreasing in older age groups, consistent with longitudinal research on heavy episodic drinking (Keyes & Miech, 2013) and cross-sectional surveys (Moore et al., 2009). Among middle-aged and older adults, we found evidence for period effects in alcohol-related admissions. An increasing period effect was present, in that estimates of period effect went from negative for 1995 and 2000 to positive for 2010 (see Figure 4).
Cohort Effects
Our findings dovetail with research focused on increased diagnosis of substance use disorder (Han et al., 2009) and need for services (Gfroerer et al., 2003) among cohorts reaching older adulthood in coming years. Research by Keyes and colleagues (Keyes, Li, & Hasin, 2011) concluded that post–World War II generations are more likely to drink heavily and develop alcohol disorders. Evidence from this study suggests this pattern is present for alcohol-related hospitalizations as well. This is especially troublesome given the unprecedented numbers of people in the baby boom generation that may strain the health care system.
These ballooning rates add to a sense of urgency to prepare the mental health and substance abuse workforce to meet the needs of older adults (Eden, Maslow, Le, & Blazer, 2012; Institute of Medicine, 2008) and to support geriatric service providers in developing competency (Jeste et al., 1999) in working with patients for whom alcohol or other substances may be a critical aspect of their health. Such effort may be aided by the diffusion of evidence-based practices (e.g., Screening, Brief Intervention, and Referral for Treatment [SBIRT]; Schonfeld et al., 2009) aimed at identifying and treating older adults at risk of alcohol-related harm. Given the solid body of evidence suggesting that older adults achieve gains in treatment that are similar to younger groups (Kuerbis & Sacco, 2013), these efforts may have a positive impact on the health and well-being of aging Americans.
Race and Gender Differences
Our estimates of race and gender differences are in line with current understanding of alcohol-related problems from other data sources, including the National Hospital Discharge Survey (Chen & Yi, 2010, 2014). Specifically, rates of alcohol-related admissions were higher among middle-aged and older adult men than women in the same age groups. Among racial groups, rates of alcohol-related disorders were significantly higher among Blacks than Whites and lower among Asians than Whites. Still, we did not identify large differences in the trend of alcohol-related admissions by gender or racial group as measured by time by race interaction terms, suggesting little differences in trend based on gender and race.
Data from this study also shed light on racial disparities in alcohol-related hospital admissions. Rates of admission were significantly higher among middle-aged and older adult African Americans, and were also higher among middle-aged Hispanics. Asian American middle-aged and older adults had consistently lower rates. These findings are congruent with those of McDonald, Wang, and Camargo (2004), who identified higher rates of alcohol-related admissions to the emergency department among Blacks compared with Whites between the years 1992 and 2000. Similarly, a review by Keyes and colleagues (2011) concluded that rates of alcohol-attributable injury were high for both Blacks and Hispanics in relation to estimates of use. Blacks and Hispanics display greater risk of specific alcohol-related conditions (Chartier & Caetano, 2010) including liver disease (Flores et al., 2008), cirrhosis (Stinson, Grant, & Dufour, 2001; Yoon, Yi, & Grant, 2008), and alcohol-related cancers (Polednak, 2007). Racial/ethnic differences in rates could also be a result of differences in life course trajectories related to alcohol use by race (Caetano & Clark, 1998).
Although this study benefits from the comprehensiveness of the NIS data, it has several limitations. The accuracy of administrative data is reliant on documentation of alcohol-related conditions for billing purposes. It is possible that diagnosis of alcohol-related conditions was not documented in the NIS, or that trends in alcohol-related admissions are a function of improved detection through uptake of interventions such as SBIRT. Moreover, diagnostic codes may be influenced by confounding changes in reimbursement, such as the addition of new reimbursement codes. The sampling frame of the NIS is limited to community hospitals, so conclusions may not be generalizable to other settings, such as Veterans Administration hospitals or Federal hospitals. APC analysis is limited by the number of time points (1995, 2000, 2005, and 2010) used in the analysis and limited number of measurements for the youngest and oldest age groups.
In the interest of clinical practice, future research should explore potential changes in the profile of alcohol-related hospital admissions with a focus on comorbid conditions and older adult populations at high risk. Future research should consider the impact of alcohol-related diagnosis on morbidity and mortality to provide insights into the impact of alcohol-related conditions on clinical outcomes for older adults. Recent research also suggests that the substance use profile of older adults is moving away from alcohol alone and will include greater use of illicit and prescription drugs (Lay, King, & Rangel, 2008; Lofwall, Schuster, & Strain, 2008; Sacco et al., 2013). This may contribute to the hospitalization of older adults for substance-related conditions other than alcohol, and as such, more knowledge is needed about co-morbidity and mortality related to those substances as well. This research adds to the evidence that training of health care professionals who care for older adults should include an understanding of alcohol-related conditions and their treatment. From the standpoint of specialty care providers, addiction treatment needs to become aging-informed, as the demographic make-up of unhealthy drinkers reflects the graying of our nation.
Acknowledgments
We gratefully acknowledge the Healthcare Cost and Utilization Project (HCUP) data partners for their contribution to the HCUP (http://www.hcup-us.ahrq.gov/db/hcupdatapartners.jsp) and Agency for Healthcare Research and Quality for making these data available for research.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: ‘This research was supported with funding from the National Institute on Alcohol Abuse and Alcoholism (K24 AA15957) and from the National Institute of Aging (P30AG10415 and P30AG028748).’
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Adams WL, Zhong Y, Barboriak JJ, Rimm AA. Alcohol-related hospitalizations of elderly people: Prevalence and geographic variation in the United States. Journal of the American Medical Association. 1993;270:1222–1225. [PubMed] [Google Scholar]
- Blow FC, Brockmann LM, Barry KL. Role of alcohol in late-life suicide. Alcoholism: Clinical and Experimental Research. 2004;28:48S–56S. [PubMed] [Google Scholar]
- Caetano R, Clark CL. Trends in alcohol consumption patterns among Whites, Blacks, and Hispanics: 1984 and 1995. Journal of Studies on Alcohol and Drugs. 1998;59:659–668. doi: 10.15288/jsa.1998.59.659. [DOI] [PubMed] [Google Scholar]
- Chartier K, Caetano R. Ethnicity and health disparities in alcohol research. Alcohol Health and Research World. 2010;33(1–2):152–160. [PMC free article] [PubMed] [Google Scholar]
- Chen CM, Yi H. Trends in alcohol-related morbidity among short-stay community hospital discharges, United States, 1979–2007. Washington, DC: U.S. Department of Health and Human Services, Public Health Service, National Institutes of Health; 2010. [Google Scholar]
- Chen CM, Yi H. Trends in alcohol-related morbidity among community hospital discharges, United States, 2000–2012. Washington, DC: U.S. Department of Health and Human Services, Public Health Service, National Institutes of Health; 2014. [Google Scholar]
- Durnas C, Loi CM, Cusack B. Hepatic drug metabolism and aging. Clinical Pharmacokinetics. 1990;19:359–389. doi: 10.2165/00003088-199019050-00002. [DOI] [PubMed] [Google Scholar]
- Eden J, Maslow K, Le M, Blazer D. The mental health and substance use workforce for older adults: In whose hands? Washington, DC: National Academies Press; 2012. [PubMed] [Google Scholar]
- Elixhauser A, McCarthy E. Clinical classifications for health policy research, version 2: Hospital inpatient statistics. Rockville, MD: Agency for Health Care Research and Quality; 1996. [Google Scholar]
- Flores YN, Yee HF, Leng M, Escarce JJ, Bastani R, Salmeron J, Morales LS. Risk factors for chronic liver disease in Blacks, Mexican Americans, and Whites in the United States: Results from NHANES IV, 1999–2004. The American Journal of Gastroenterology. 2008;103:2231–2238. doi: 10.1111/j.1572-0241.2008.02022.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gfroerer J, Penne M, Pemberton M, Folsom R. Substance abuse treatment need among older adults in 2020: The impact of the baby-boom cohort. Drug and Alcohol Dependence. 2003;69:127–135. doi: 10.1016/s0376-8716(02)00307-1. [DOI] [PubMed] [Google Scholar]
- Han B, Gfroerer J, Colliver JD, Penne MA. Substance use disorder among older adults in the United States in 2020. Addiction. 2009;104:88–96. doi: 10.1111/j.1360-0443.2008.02411.x. [DOI] [PubMed] [Google Scholar]
- Healthcare Cost and Utilization Project. Nationwide Inpatient Sample Trends (NIS-Trends) files. Rockville, MD: Agency for Healthcare Research and Quality; 1993–2010. [Google Scholar]
- Healthcare Cost and Utilization Project. Introduction to the Nationwide Inpatient Sample (NIS) Rockville, MD: Agency for Healthcare Research and Quality; 2012. [Google Scholar]
- Institute of Medicine. Retooling for an aging America: Building the health care workforce. Washington, DC: National Academies Press; 2008. [PubMed] [Google Scholar]
- Jeste DV, Alexopoulos GS, Bartels SJ, Cummings JL, Gallo JJ, Gottlieb GL, Lebowitz BD. Consensus statement on the upcoming crisis in geriatric mental health. Archives of General Psychiatry. 1999;56:848–853. doi: 10.1001/archpsyc.56.9.848. [DOI] [PubMed] [Google Scholar]
- Johnson RA, Gerstein DR. Age, period, and cohort effects in marijuana and alcohol incidence: United States females and males, 1961–1990. Substance Use & Misuse. 2000;35:925–948. doi: 10.3109/10826080009148427. [DOI] [PubMed] [Google Scholar]
- Keyes KM, Li G, Hasin DS. Birth cohort effects and gender differences in alcohol epidemiology: A review and synthesis. Alcoholism: Clinical and Experimental Research. 2011;35:2101–2112. doi: 10.1111/j.1530-0277.2011.01562.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes KM, Miech R. Age, period, and cohort effects in heavy episodic drinking in the US from 1985 to 2009. Drug and Alcohol Dependence. 2013;132:140–148. doi: 10.1016/j.drugalcdep.2013.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuerbis A, Sacco P. A review of existing treatments for substance abuse among the elderly and recommendations for future directions. Substance Abuse: Research and Treatment. 2013;7:13–37. doi: 10.4137/SART.S7865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lay K, King LJ, Rangel J. Changing characteristics of drug use between two older adult cohorts: Small sample speculations on baby boomer trends to come. Journal of Social Work Practice in the Addictions. 2008;8:116–126. [Google Scholar]
- Lofwall MR, Schuster A, Strain EC. Changing profile of abused substances by older persons entering treatment. The Journal of Nervous and Mental Disease. 2008;196:898–905. doi: 10.1097/NMD.0b013e31818ec7ee. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald AJ, Wang N, Camargo JCA. US emergency department visits for alcohol-related diseases and injuries between 1992 and 2000. Archives of Internal Medicine. 2004;164:531–537. doi: 10.1001/archinte.164.5.531. [DOI] [PubMed] [Google Scholar]
- Moore AA, Karno MP, Grella CE, Lin JC, Warda U, Liao DH, Hu P. Alcohol, tobacco, and nonmedical drug use in older U.S. adults: Data from the 2001/02 National Epidemiologic Survey of alcohol and related conditions. Journal of the American Geriatrics Society. 2009;57:2275–2281. doi: 10.1111/j.1532-5415.2009.02554.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore AA, Whiteman EJ, Ward KT. Risks of combined alcohol/medication use in older adults. American Journal of Geriatric Pharmacotherapy. 2007;5:64–74. doi: 10.1016/j.amjopharm.2007.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson TL, Jeste DV. The potential impact of the baby boom generation on substance abuse among elderly persons. Psychiatric Services. 1999;50:1184–1188. doi: 10.1176/ps.50.9.1184. [DOI] [PubMed] [Google Scholar]
- Polednak AP. Secular trend in U.S. Black–White disparities in selected alcohol-related cancer incidence rates. Alcohol and Alcoholism. 2007;42:125–130. doi: 10.1093/alcalc/agl121. [DOI] [PubMed] [Google Scholar]
- Rehm J, Room R, Graham K, Monteiro M, Gmel G, Sempos CT. The relationship of average volume of alcohol consumption and patterns of drinking to burden of disease: An overview. Addiction. 2003;98:1209–1228. doi: 10.1046/j.1360-0443.2003.00467.x. [DOI] [PubMed] [Google Scholar]
- Sacco P, Kuerbis A, Goge N, Bucholz KK. Help seeking for drug and alcohol problems among adults age 50 and older: A comparison of the NLAES and NESARC surveys. Drug and Alcohol Dependence. 2013;131:157–161. doi: 10.1016/j.drugalcdep.2012.10.008. [DOI] [PubMed] [Google Scholar]
- SAS Institute Inc. SAS 9.2 help and documentation. Cary, NC: Author; 2008. [Google Scholar]
- Schonfeld L, King-Kallimanis BL, Duchene DM, Etheridge RL, Herrera JR, Barry KL, Lynn N. Screening and brief intervention for substance misuse among older adults: The Florida BRITE project. American Journal of Public Health. 2009;100:108–114. doi: 10.2105/AJPH.2008.149534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorock GS, Chen LH, Gonzalgo SR, Baker SP. Alcohol-drinking history and fatal injury in older adults. Alcohol. 2006;40:193–199. doi: 10.1016/j.alcohol.2007.01.002. [DOI] [PubMed] [Google Scholar]
- Statacorp. Stata Statistical Software: Release 13. College Station, TX: Author; 2013. [Google Scholar]
- Stinson FS, Grant BF, Dufour MC. The critical dimension of ethnicity in liver cirrhosis mortality statistics. Alcoholism: Clinical and Experimental Research. 2001;25:1181–1187. [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. The TEDS report: Older adult admissions reporting as a substance of abuse: 1992 and 2009 2011 [Google Scholar]
- Yang Y, Schulhofer-Wohl S, Fu WJ, Land KC. The intrinsic estimator for age–period–cohort analysis: What it is and how to use it. American Journal of Sociology. 2008;113:1697–1736. [Google Scholar]
- Yoon YH, Yi H-Y, Grant B. Surveillance report 83, liver cirrhosis mortality in the United States, 1970–2005. Arlington, VA: National Institute on Alcohol Abuse and Alcoholism; 2008. [Google Scholar]


