Summary
Background
Idiopathic hypoparathyroidism is an extremely rare endocrinal disorder with a prevalence of 37 per 100,000. Herein we presented a case of a 30-year-old male who came with symptoms of muscle weakness, carpopedal spasms and limitation of movement which gradually progressed over 8 years.
Case Report
A 30-year-old male patient presented in an outpatient department of a tertiary care centre with a complaint of severe pain in both hip joints. He had generalized muscle weakness, facial discomfort, recurrent episodes of carpopedal spasms and crampy abdominal pains. On clinical examination, the patient had Chvostek sign and Trousseau sign. Biochemical tests revealed hypocalcemia, hyperphosphatemia and hypomagnesemia with low plasma parathyroid hormone level. X-ray of the pelvis and spine revealed spondylarthropathic changes of long-standing hypoparathyroidism. Computed Tomography of the brain revealed bilateral basal ganglia calcifications. The patient was treated with intravenous calcium gluconate, magnesium and oral vitamin D3. On follow-up the patient showed improvement of muscle weakness and carpopedal spasm with near-normal biochemical parameters. However, there was no improvement in symptoms related to spondyloarthropathy.
Conclusions
Idiopathic hypoparathyroidism is a rare endocrine disorder with clinic and biochemical features of hypocalcemia. Long- standing hypoparathyroidism can cause spondyloarthropathic changes closely resembling ankylosing spondylitis and DISH. Skeletal changes of long-standing hypoparathyroidism are irreversible. If left untreated, life-threatening complications like cardiac arrhythmias and broncholaryngospasm may occur.
MeSH Keywords: Hypoparathyroidism; Pseudohypoparathyroidism; Spondylarthropathies; Spondylitis, Ankylosing
Background
Idiopathic hypoparathyroidism is an extremely rare endocrinal disorder with a prevalence of 37 per 100,000 [1]. Long-standing hypoparathyroidism can cause spondyloarthropathic changes closely resembling ankylosing spondylitis and DISH [2]. Herein we presented a case of long-standing hypoparathyroidism.
Case Report
A 30-year-old male patient presented in an outpatient department of a tertiary care centre with a complaint of severe pain in both hip joints. He had generalized muscle weakness, facial discomfort, recurrent episodes of carpopedal spasms and crampy abdominal pains. Symptoms were progressive over the last 8 years for which he was on injections of calcium gluconate. On clinical examination the patient had Chvostek sign (Video 1) and Trousseau sign (Video 2). The patient had also mild kyphotic deformity with limitation of extension. He had bilateral cataract and brittle nails. Biochemical tests revealed serum calcium, ionized of 2.4 mg/dL (low, normal − 4.5 to 5.3), serum phosphorus − 5.7 mg/dL (high, normal − 2.5 to 4.3), serum magnesium − 1.7 mg/dL (low, normal − 1.5 to 2.3), plasma parathyroid hormone − 2.5 pg/mL (low, normal − 8 to 51) and Vitamin D3 level of 55.8 ng/dL (within normal limit, normal − 30 to 100). [3] Ultrasonography of the thyroid gland was normal. No evidence of enlargement of parathyroid glands.
Video 1.
Chvostek sign.
Video 2.
Trousseau sign.
X-ray of the pelvis with both hips in antero-posterior view showed diffuse increase in bone density. Capsular ossification of both hip joints was found. Ossification of bilateral iliolumbar ligaments and subtle calcification of the right sacro-spinous ligament were present. There were broad irregular ossifications at lateral margins of the right acetabulum. Irregular bony excrescences were seen involving the right and left iliac bones just above the acetabulum and also involving the left ischial tuberosity and right superior pubic ramus. Entheseal erosions were present involving the lesser trochanters. Bilateral sacro-iliac joints were normal (Figure 1).
Figure 1.
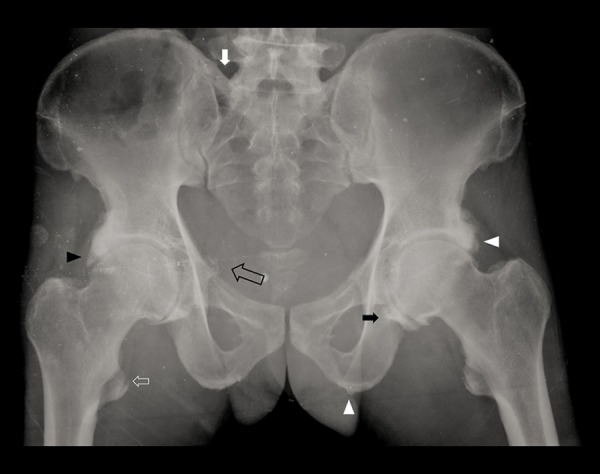
30-year-old man with idiopathic hypoparathyroidism. Anteroposterior radiograph of the pelvis shows diffuse osteosclerosis, capsular ossification around bilateral hip joints (black arrow), ossification of bilateral iliolumbar ligaments (white arrow), irregular bony excrescences (white arrowheads), subtle calcification of the right sacrospinous ligament (black open arrow), broad ossification at the lateral margin of the right acetabulum (black arrowhead), enthesopathy (white open arrow).
X-ray of the dorso-lumbar spine showed bridging osteophytes involving T7-T8, T8-T9, T9-T10 vertebrae. Subtle ossification of interspinous ligaments in the region of T5 to T7 with mild kyphotic deformity of the thoracic spine was present (Figures 2, 3).
Figure 2.

X Ray Dorso-lumbar AP view shows interspinous ligament calcification(arrow head).
Figure 3.

X Ray Dorso-lumbar Spine Lateral View shows bridging osteophytes (arrowheads) between T7–T8, T8–T9, T9–T10 vertebrae.
Computed Tomography of the brain (Figures 4, 5) revealed dense calcifications in bilateral lentiform nuclei and bilateral caudate nuclei. Linear transverse bands of calcification were seen in bilateral centrum semiovale.
Figure 4.
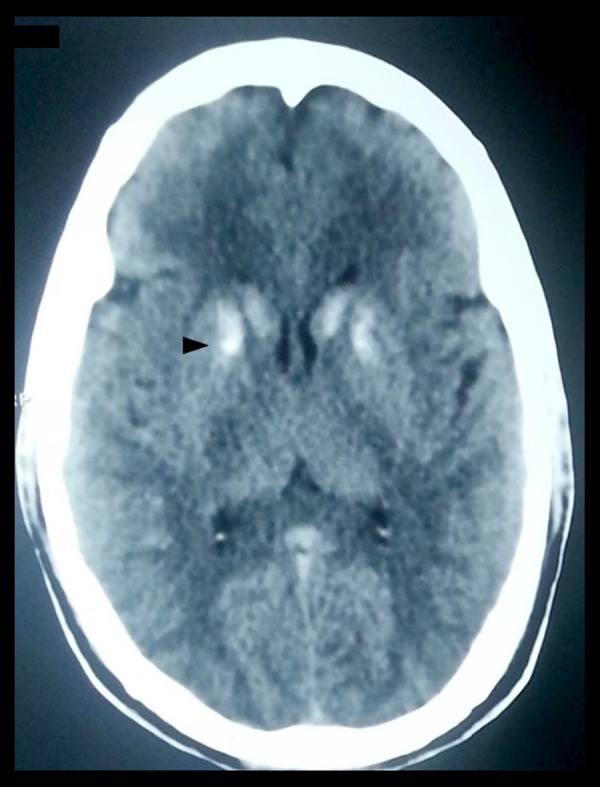
Computed Tomography of the Brain shows dense calcifications in bilateral lentiform nuclei and bilateral caudate nuclei (arrowhead).
Figure 5.
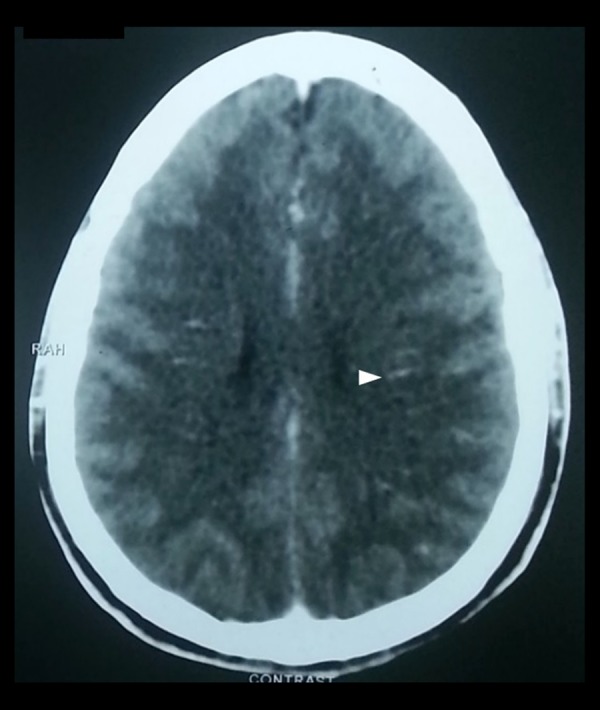
CT of the brain shows linear transverse bands of calcification in bilateral centrum semiovale (arrowhead).
On the basis of clinical, biochemical and radiological findings the patient was diagnosed with long-standing hypoparathyroidism. The patient was treated with intravenous calcium gluconate, magnesium and oral vitamin D3. On follow-up the patient showed improvement of muscle weakness and carpopedal spasm with near-normal biochemical parameters. However, there was no improvement in symptoms related to spondyloarthropathy.
Discussion
Hypoparathyroidism is an endocrinal disorder caused by deficiency of parathyroid hormone which in turn results in decreased serum calcium levels and raised serum phosphorus levels.
Epidemiological estimates of hypoparathyroidism in the literature are scarce. A study conducted with the population-based Rochester Epidemiology Project identified a prevalence of hypoparathyroidism of 37 per 100,000, with most cases caused by surgery [1].
It is most often acquired from head and neck surgery. It can also be congenital, idiopathic, genetic or associated with autoimmune disorders [4]. Pseudohypoparathyroidism is due to tissue insensitivity to parathyroid hormone. Symptoms of hypoparathyroidism are paraesthesia, muscle cramps, tetany, cataract, malformed teeth, and brittle nails.
General radiological features include generalised osteosclerosis, calvarial thickening, soft tissue calcifications and hypoplastic dentition.
Brain calcifications can occur in bilateral basal ganglia, most commonly in the globus pallidus, as in this case. Other sites are dentate nucleus, corona radiata, subcortical white matter and thalamus. Mechanism of brain calcification has been linked to long duration of hyperphosphetemia which tends to induce calcification [5]. A similar type of bilateral symmetrical calcification is also seen in Fahr’s disease, but in the latter the patient has neuropsychiatric symptoms and a normal biochemical profile [6].
Long-standing hypoparathyroidism can cause spondyloarthropathy [2]. There may be ossification of spinal ligaments and bridging osteophytes. Pelvis shows ossification of iliolumbar, sacrospinous and sacrotuberous ligaments and ossification of acetabular margins. These features may closely resemble ankylosing spondylitis and Diffuse Idiopathic Skeletal Hyperostosis (DISH). However, sacroilitis is usually absent and there is no erosive arthropathy in hypoparathyroidism [7]. Tetany, muscle cramps and other features of hypocalcaemia help to differentiate as well.
A rare complication of hypoparathyroidism is enthesopathy [8] which may occur at lesser and greater trochanters, ischial tuberosities and iliac crests.
Chronic management includes supplementing oral calcium, vitamin D, thiazide diuretics and phosphate binders. Replacement therapy using synthetic human parathyroid hormone is also beneficial [9].
If untreated, the following complications are likely to occur: blocked airway due to severe laryngeal spasm, stunted growth, malformed teeth, calcium deposits in the brain leading to seizures and cardiac arrhythmia [10].
Conclusions
Idiopathic hypoparathyroidism is a rare endocrine disorder with clinical and biochemical features of hypocalcemia. Long-standing hypoparathyroidism can cause spondyloarthropathic changes closely resembling ankylosing spondylitis and DISH. Skeletal changes of long-standing hypoparathyroidism are irreversible. If left untreated, life threatening complications like cardiac arrhythmias and broncholaryngospasm may occur.
Learning points/take-home messages
X-ray findings of hypoparathyroidism are generalised osteosclerosis, calvarial thickening, hypoplastic dentition and soft tissue calcifications.
Computed Tomography of the brain may show bilateral symmetrical calcifications involving basal ganglia, corona radiata, subcortical white matter and thalamus.
Long-standing hypoparathyroidism can cause extensive spondyloarthropathy with ossification of spinal ligaments, bridging ostophytes, ligamental calcification and enthesopathy. These skeletal changes are irreversible.
Radiological features may closely mimic ankylosing spondylitis, fluorosis and diffuse idiopathic skeletal hyperostosis. However, sacroiliac joint is normal in hypoparathyroidism.
References
- 1.Powers J, Joy K, Ruscio A, Lagast H. Prevalence and incidence of hypoparathyroidism in the united states using a large claims database. J Bone Miner Res. 2013;28:2570–76. doi: 10.1002/jbmr.2004. [DOI] [PubMed] [Google Scholar]
- 2.Goswami R, Ray D, Sharma R, et al. Presence of spondyloarthropathy and its clinical profile in patients with hypoparathyroidism. Clin Endocrinol. 2008;68:258–63. doi: 10.1111/j.1365-2265.2007.03032.x. [DOI] [PubMed] [Google Scholar]
- 3.Longo DL, editor. Harrison’s principles of internal medicine. 18th ed. Vol. 2. Mc-Graw-Hill; 2012. Appendix: Reference Values of Laboratory Tests. Tables 2,4. [Google Scholar]
- 4.Martel J, Spriggs BB. Hypoparathyroidism. Healthline. 2012June [Google Scholar]
- 5.Jagtap S, Nair S, Harsha KJ. Primary Hypoparathyroidism. American Journal of Neuroradiology. 2012 Image Quiz. [Google Scholar]
- 6.Mittal A, Agrawal BK, Mittal A, et al. Fahr’s syndrome: A rare case of idiopathic basal ganglia calcification. Journal, Indian Academy of Clinical Medicine. 2010;11(3):239–41. [Google Scholar]
- 7.Jakkani RK, Sureka J, Mathew J. Spondyloarthropathy occurring in long-standing idiopathic hypoparathyroidism. Radiology Case Reports (Online) 2011;6:545. doi: 10.2484/rcr.v6i4.545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Davies M, Johnson K, Whitehouse RW. Technics and applications. Spinger-Verlag; Berlin Heidelberg: 2006. Imaging of the hip and bony pelvis. [Google Scholar]
- 9.Bilezikian JP, Khan A, Potts JT, et al. Hypoparathyroidism in the adult: Epidemiology, diagnosis, pathophysiology, target-organ involvement, treatment, and challenges for future research. J Bone Miner Res. 2011;26:2317–37. doi: 10.1002/jbmr.483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cunha JP, Felicetta J. Hypoparathyroidism. MedicineNet: Diseases & Conditions. [cited 2008 Sept 24, medically reviewed 2014 Apr 3], page 2. Available from: URL: http://www.medicinenet.com/hypoparathyroidism/page2.htm.


