Abstract
Patients with serious mental illness (SMI) and diabetes often seek care in primary care settings and have worse health outcomes than patients who have either illness alone. Individual, provider, and system-level barriers present challenges to addressing both psychiatric and medical comorbidities. This article describes the feasibility, acceptability, and implementation of Targeted Training and Illness Management (TTIM), a self-management intervention delivered by trained nurse educators and peer educators to groups of individuals with SMI and diabetes to improve self-management of both diseases. TTIM is intended to be delivered in a primary care setting. Findings are intended to support the future development of nurse-led programs within the primary care setting that teach self-management to individuals with concurrent SMI and diabetes. This approach supports both adaptability and flexibility in delivering the intervention. Interventions such as TTIM can provide self-management skills, accommodate people with both SMI and diabetes in primary care settings such as patient-centered medical homes, and address known barriers to access.
Patients with both serious mental illness (SMI; e.g., schizophrenia/schizoaffective disorder, bipolar disorder, or severe major depressive disorder) and diabetes have disproportionately higher rates of poor outcomes compared to patients with either SMI or diabetes alone (1–8). Medical comorbidity reduces the life span of people with SMI by as much as 25–30 years (3,4). Contributing factors include widely prevalent unhealthy behaviors such as inactivity and poor diet (3,4,8). Professional groups have called for developing best practices to address the unique needs of patients with SMI for treatment of their comorbid general medical and psychiatric conditions (4,8). However, few studies have specifically addressed diabetes management among people with SMI, and fewer still have addressed concurrent management of diabetes and SMI (4).
Patients with SMI often rely on primary health care settings for the treatment of their comorbid physical illnesses (2). Diabetes education and self-management programs are commonly situated in primary care settings; however, people with SMI and diabetes may not access these services. One important reason patients with SMI do not attend diabetes education or self-management programs is that they are concerned about being stigmatized by other program participants (8,9).
A primary role of nurses is to care for patients with chronic illnesses and educate them about disease self-management (1,3,10–15). Examples of successful nurse-led self-management programs for chronic illness include osteoarthritis (16), asthma (10), and diabetes (1,3,7,13). This is the first study the authors are aware of that has examined the role of nurses in addressing the self-management needs of patients with both SMI and diabetes. This team of investigators conducted a pilot study of the Targeted Training and Illness Management (TTIM) intervention (including SMI and diabetes self-management, information sharing, psychoeducation, problem identification, goal setting, behavioral modeling, and care linkage) led by nurse educators in a primary care setting. TTIM features collaborative interdisciplinary involvement designed to empower historically underserved and marginalized patients to become actively engaged in their care. Promising results from the pilot study of the TTIM approach have been presented elsewhere (4,5).
The purpose of this article is to describe the nurse-led component of a randomized, controlled trial of the TTIM intervention, Improving Outcomes for Individuals with Serious Mental Illness and Diabetes (R01 MH085665), funded by the National Institute for Mental Health and conducted in a primary care setting. We report on the feasibility, acceptability, and implementation of nurse-led activities in the TTIM program. These findings are intended to support the future development of multidisciplinary programs within the primary care setting that improve self-management for individuals with concurrent SMI and diabetes, as well as other chronic conditions.
Design and Methods
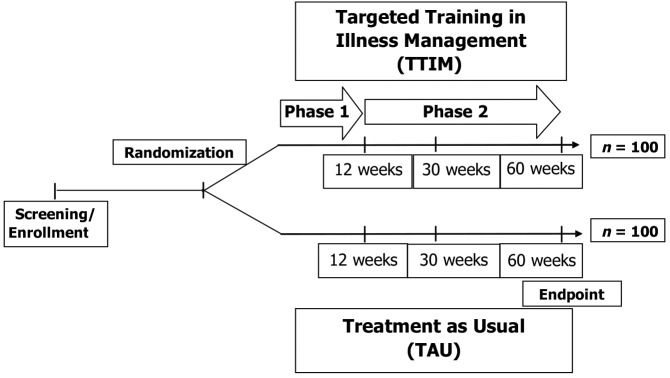
The intervention was conducted as part of a randomized controlled trial comparing TTIM to treatment as usual (TAU) in 200 individuals (n = 100 TTIM, n = 100 TAU) with concurrent SMI and diabetes. The primary aim of the project was to compare the two groups with regard to change from baseline in SMI symptoms, functional status, general health status, and diabetes outcomes. Figure 1 illustrates the overall study design, randomization, and research assessments. The study was approved by the local institutional review board (IRB), and all participants provided written informed consent to participate.
FIGURE 1.
Improving outcomes for individuals with SMI and diabetes: TTIM study design.
Treatment as Usual
Subjects randomized to TAU received their usual physical and mental health treatment without the TTIM intervention. Most study subjects were patients of this health care system and received their primary care within the study site clinical infrastructure staffed by general internal medicine and family medicine providers. In this health care system, patients with diabetes visit their primary care practitioner an average of five times per year. These practitioners are responsible for the primary management of diabetes and can refer their patients with diabetes to specialty care (e.g., endocrinology, ophthalmology, renal care, and podiatry) and educational resources (e.g., a diabetes nurse educator, the nutrition clinic, and diabetes group management). About one-fourth of patients of this system receive psychiatric care within the study site clinical infrastructure. The remaining three-fourths receive their psychiatric care at nonaffiliated community mental health clinics.
TTIM Intervention: Concept, Design, and Key Role of Nurses
The TTIM intervention is led by a nurse educator who delivers the manualized intervention. A manualized intervention is one that has been standardized through the creation of manuals and protocols so that participants all receive the same treatment. The nurse educator role is that of “content expert.” To enhance program effectiveness, trained peer educators, who are individuals with both SMI and diabetes, provide complementary support and structure as “experiential experts” in SMI and diabetes self-management. Interaction between nurse educators, peer educators, and program participants is a key feature of the TTIM intervention.
The TTIM intervention is delivered in two steps. Step 1 consists of 12 weekly group-based sessions. Step 2 consists of monthly follow-up contact, in person or by phone, over a 48-week period to support participants’ personal care plans (PC plans) regarding their self-management goals. In both steps, nurse educators address patient-specific factors regarding self-efficacy, outcome expectations, health knowledge, social support, cognitive skills, stigma, and substance abuse. Nurses address care facilitators and barriers by disseminating health information, facilitating group processes, minimizing logistic barriers, and coordinating interdisciplinary professional communications.
Nurse Educator Recruitment and Selection
Three nurse educators with broad experience in primary care nursing were selected from a safety-net medical system. The nurse educators were white, female, and bachelor’s degree–prepared. The nurses’ of experience were 28, 34, and 39 years. Two nurse educators were clinically experienced but not specialized in diabetes self-management or psychiatric nursing. One nurse educator had 11 years of experience as a CDE but was not specialized in psychiatric care.
Nurse Educator Training and Support Sessions
Nurse educator training involved general education in diabetes and SMI using a variety of methods and resources. Two days of initial intensive training with the principal investigators (PIs) and team members (i.e., co-investigators, research assistants, and peer educators) included an overview of the TTIM intervention and allowed the research team to get acquainted. The content for each of the 12 TTIM sessions was reviewed, and nurse educators were given a treatment manual for review and reference.
Communication skills, including group leading/co-leading, assistance with help-seeking pathways, and crisis management, were taught using role-play and repetition. Training was provided by the team psychiatrist. She was also available to respond to nurse educators’ questions and concerns and provide support related to participants’ mental health issues on an as-needed basis. Peer educators took an active part in the training, focusing on modeling SMI- and diabetes-related healthful behaviors and group processes. The psychiatrist PI met with nurse educators, peer educators, and research staff once weekly for the first month and has continued to meet with them every 1–2 months thereafter to conduct additional peer educator training and education.
Nurse educators, peer educators, the psychiatrist PI, and research coordinators met as a group for follow-up training approximately monthly for the first 6 months and approximately every 2 months for the next 6 months. Quarterly training sessions provided an opportunity to discuss and update overall study progress, review TTIM content, address concerns, practice skills for managing questions, discuss follow-up contact, and provide ongoing support and encouragement.
Nurse educators were encouraged to call the study PIs or other study staff if they had any concerns they felt were too urgent to wait until the next scheduled training session. Ongoing training and support was conducted via meetings, phone calls, and e-mail with TTIM investigators. The psychiatrist PI was available for informal support related to participants’ mental health issues.
Description of TTIM Nurse Educator Manual Content
The TTIM nurse educators’ instructor’s manual consists of two parts. Part 1 provides an overview of the program, a list of needed supplies and equipment, a time schedule, and objectives and materials to be covered in each session. Home practice exercises facilitating information-building from week to week are also included and distributed to participants by the nurses. Table 1 summarizes the 12 weekly group sessions provided in step 1 of the program.
TABLE 1.
TTIM Topics
| Session | Description |
|---|---|
| 1 | Orientation and introductions, emphasis on ground rules, establishment of a therapeutic relationship, discussion of facts and misconceptions about SMI, introduction of diabetes topics |
| 2 | The challenge of having both SMI and diabetes, the stigma of SMI and strategies to cope with stigma, relationship of SMI symptoms and functioning in response to stress and diabetes, an introduction to personal goal-setting |
| 3 | Personal SMI profile (what does worsening illness look like for you), triggers of SMI relapse, personal action plan for coping with SMI relapse |
| 4 | Carbohydrate and blood glucose monitoring |
| 5 | Problem-solving skills, talking with medical and mental health care providers, role-playing communication with care providers |
| 6 | Nutrition for best physical and emotional health, reading nutrition labels |
| 7 | Replacing unhealthy sugar and fat, substance use and its effects on SMI and diabetes, problem-solving to eat healthfully |
| 8 | Effects of exercise on physical and emotional health, importance of daily routine and good sleep habits |
| 9 | Medications and psychological treatments for SMI, creation of a personal care plan to take care of the mind and the body |
| 10 | Social support and using available supports, types of physical activity, and community resources |
| 11 | Taking care of your feet, staying on track with medication treatments |
| 12 | Illness management as a lifestyle, acknowledgment of group progress |
Part 2 of the manual, “Follow Up,” includes instructions for nurse educator and peer educator telephone follow-ups. Step 2 of the program lasts for 48 weeks and includes monthly follow-up contacts, in person or by phone, by the nurse educator. Peer educators call twice each month for the first 3 months and monthly for the next 5 months. At each follow-up, nurse educators ask about how things are going in general, progress on mental health and diabetes goals, and follow-up with primary care and mental health care providers and then request permission to call again in 1 month. Follow-ups are meant to be brief, lasting 15 minutes at most.
Communication with participants’ medical providers, through scheduled clinical linkages, is implemented early in the program. Each participant’s primary care and mental health providers are sent notification of the patient’s participation in TTIM and an overview of the TTIM program at around week 2. The second clinical linkage is sent when the participant completes a PC plan, usually at week 9. Clinical linkages are sent to providers at least once between weeks 13 and 29 of the program and at least once between weeks 30 and 59. Additional communications are sent to mental health or primary care providers as needed. Clinical linkages content includes anticipated completion dates, copies of the participants’ PC plans, updated information on the study participants’ progress relative to the PC plan, and any information pertinent to the participant’s health.
Clinical linkages assist in communication between providers caring for patients with comorbid SMI and diabetes. It is important to note that, unlike more “wrap-around” care systems such as the Collaborative Care Model (17), the TTIM linkages are intended to keep providers informed but do not require an intensive coordination effort on the part of providers. A focus of the TTIM intervention is to empower patients to communicate effectively with providers and to more actively engage in care. An example of how this has been operationalized is that nurse educators suggest that TTIM participants make and keep appointments with care providers but do not make the appointments for them.
Role of Peer Educators in TTIM
Peer educators were identified from individuals receiving care at an urban safety-net primary care setting located in the midwest region of the United States or self-referred in response to an IRB-approved study advertisement. All peer educators were research subjects and provided informed consent to participate. They included five women and three men ranging in age from 45 to 64 years (median 56 years). Two participants were non-Hispanic white, four were non-Hispanic black, and two were Hispanic white. In addition to having diabetes, five of the peer educators had a diagnosis of depression, two of schizophrenia, and one of bipolar disorder.
Peer interaction in TTIM was used to empower participants by disseminating patient-level self-care innovations. In both steps of the program, the peer educators shared their personal expertise about diabetes and mental illness and modeled self-management. TTIM participants viewed the peer educators as someone who has “walked in their shoes,” fostering an understanding from a perspective other than that of a health care professional. Working closely with the nurse educator, the peer educator often came to sessions early or met with the nurse educator after class to address any concerns that might have been helpful to TTIM participants. Peer educators similarly met with the nurse educator regarding step 2 follow-up phone calls as needed.
TTIM Group Participant Characteristics
TTIM intervention group sizes ranged from 8 to 10 individuals. Among the 200 individuals in the study, 64% were female and 36% were male. Of these, 53% identified themselves as African American, 10% as Hispanic, and 37% as white. Ages ranged from 25 to 73 years (mean 54, SD 9.4 years). Mean level of education was 13 years (SD 2.7 years). All individuals had a diagnosis of diabetes and the mean time since diagnosis was 10 years (SD 7.8 years). Regarding SMI, 95 (48.0%) had a diagnosis of depression, 49 (24%) had a diagnosis of schizophrenia, and 56 (28%) had a diagnosis of bipolar disorder. The mean time since SMI diagnosis was 18 years (SD 12.6 years).
Results
The study recently completed enrollment of 200 participants, evenly randomized between TTIM and TAU. Study follow-up and data analysis will be completed over the next 12 months. Results for TTIM group attendance, retention, and nursing personnel fidelity to the TTIM intervention provide preliminary information on the feasibility, practical implementation, and general acceptability of TTIM to participants with SMI.
Participant Attendance
There were a total of 11 TTIM group cohorts. Of the 100 participants randomized to TTIM, 80 (80%) attended at least one session. Of those who attended at least one session, the mean number of sessions attended was 8 (SD 3.5) of 12. Nurses conducted “make-up” sessions when logistic factors such as acute medical illness prevented an individual from attending a session. However, most of the participation was in the group sessions; the mean number of makeup sessions was 0.7. Forty-nine participants (61%) completed all 12 sessions, including group attendance or individual make-up sessions.
Fidelity to the Process
Fidelity to the TTIM process was established by research assistants observing and documenting on checklists adherence to the manual during TTIM sessions. Each of the TTIM step 1 group cohorts was observed on two different, randomly determined occasions to establish fidelity. Research assistants documented nearly complete fidelity to the manualized content and process, with the exception of a few of the sessions going ∼15 minutes beyond the allotted time frame of 90 minutes.
Clinical outcomes data for the study are being collected at weeks 13, 30, and 60 and will be reported in future articles.
TTIM Nurse Educator Experience
Overall, the nurse educators’ experiences were very positive. As one nurse educator stated, “. . . to be able to work with individuals who have two serious illnesses and helping them effectively manage both was a highlight.”
Table 2 illustrates the variety of resources and approaches used by the nurse educators to disseminate health information to TTIM participants. The use of a standardized TTIM manual, individualized PC plans, flexible scheduling for make-up sessions, question-and-answer periods, teach-back methods to allow patients to explain what they understand, and coaching of participants to follow up with their providers all helped nurse educators to meet participants’ learning needs.
TABLE 2.
Nurses Disseminate Health Information: Overcoming Challenges and Promoting Interaction
| Nurses’ Role | Challenges | Highlights | Interactive Opportunities |
|---|---|---|---|
| Using the TTIM manual | Adherence to manual to ensure research fidelity | Manualized curriculum and detailed timeline ensure consistency of information provided to different groups | Participants have a manual; each session includes a PowerPoint presentation |
| Encouraging attendance in a 12-week program | Absenteeism limits weekly assimilation of material; goal is to complete a missed session before the next class | Participants and nurse arrange make-up times for anticipated absences | Nurse educators provide opportunities for small-group and individual make-up sessions as needed |
| Addressing nurse educators’ knowledge base | Questions about personal health conditions are outside the scope of the TTIM program | Curriculum does not require nurse specialization in diabetes management or mental health and includes strategies to enhance participants’ communication with providers | Nurse educators and curriculum provide tips for more effectively communicating with health care providers |
| Ensuring participants’ comprehension of class material | Participants’ learning limitations include literacy, primary language, and sensory impairments | Participants are encouraged to participate in discussion of presented material and share relevant experiences; materials were developed for low-literacy participants; participants express excitement about mastering new (“I never knew that”) | Sessions include time for questions and answers, discussion, role-playing, and teach-back opportunities; nurse educators reinforce key concepts from the previous class, posing open-ended questions such as “How was your week?” to engage group discussion of home practice exercises |
| Assisting participants in writing a personal care plan (PC plan) for their diabetes and mental health management | Writing a PC plan can be challenging depending on participants’ diabetes and SMI disease severity and educational limitations | Goals are based on the information learned about diabetes and SMI management | Nurse educators coach participants in writing goals; copies of PC plans are provided to participants and peer educators and to care providers as clinical linkages |
As shown in Table 3, nurse educators facilitated group processes to maximize a therapeutic environment. Providing clear ground rules, using peer educators as models, and adopting a nurse/peer team approach encouraged TTIM participants to openly share their concerns and personal experiences. The unique roles of the nurse and peer educators contributed to the success of each session. As one TTIM participant noted, “. . . I learned to trust to share my mental illness . . . .”
TABLE 3.
Nurses Facilitate Group Processes for Individuals With Comorbid SMI and Diabetes
| Nurses’ Role | Experience Challenges | Experience Highlights | Interactive Opportunities |
|---|---|---|---|
| Openly discussing stigma about mental illness | Establishing a welcoming, nonjudgmental environment for participants to self-identify shared health conditions and concerns | Session 1 includes time for participants to tell their “story” and state desired class outcomes; participants are encouraged to share their feelings; participants are empowered through shared experiences to see that others have similar emotions | Use of structured prompts; ground rules for confidentiality, respect, and positive support; ground rules for discussion include “the same time for all;” positive reinforcement for appropriate self-disclosure and support of others |
| Managing attrition | Inconsistent attendance alters group process and opportunities to learn | Consistent attendance fosters development of informal relationships and concern when participants are absent | Promotional activities include confirmation letter and welcome gift; weekly reminder calls; follow-up hand-written letters and phone calls; door prizes at each session; peer educator phone calls to encourage attendance; refreshments consistent with American Diabetes Association dietary guidelines provided at each class |
| Adhering to class start and end times | Disruptions: arriving late and leaving early affected group discussion; difficult for group members who struggle with attention difficulties | Detailed timeline for each class session helps keep sessions on track (social isolation and relationship-building among participants could contribute to digression from session schedule) | Welcome of late-arriving participants; nurse educators summarize session information referring to the page in the manual and use interruptions as an opportunity to review and refocus the group |
| Employing a nurse/peer educator team approach | Diversity among peer educators in SMI and diabetes severity; peer educators sometimes struggled with modeling behaviors consistent with class materials | Peer educators responsibility included modeling; participants see that peer educators struggle to manage illnesses as they do; open discussion increases participant comfort with the peer educator and class | Participants volunteer and are called on to give others an opportunity to speak; participants show positive regard toward peer educators for their willingness to share their struggles and setbacks and how they overcome them; nurse and peer educators review content before and after class to support understanding; when peer educators provide information inconsistent with material, nurse educators facilitate participant discussion, leading them to modify solutions |
Table 4 displays the strategies used by nurse educators to help manage logistic barriers common for TTIM group participants, including transportation issues, some class times, inconsistent classroom locations, and difficulties contacting participants.
TABLE 4.
Nurses Minimize Logistical Barriers for Individuals With Comorbid SMI and Diabetes
| Barrier | Challenges | Highlights | Interactive Opportunities |
|---|---|---|---|
| Limited transportation resources | Various and unreliable modes of transportation affect reliability | Various transportation methods are used to get to and from class including personal vehicles, public transportation, specialty transportation for disabled participants, rides from friends/family, and bicycles | Reimbursement is provided for parking and bus passes |
| Inconsistent class location | Inconsistent attendance alters group process and opportunities to learn | Consistent attendance fosters development of informal relationships and concern when participants are absent | Promotional activities include confirmation letter and welcome gift; weekly reminder calls; follow-up hand-written letters and phone calls; door prizes at each session; peer educator phone calls to encourage attendance; refreshments consistent with American Diabetes Association dietary guidelines provided at each class |
| Class times | Morning classes are difficult | Feedback and experience helps to identify what times work best | Mid-afternoon classes allow participants time to manage morning challenges |
| Participant contact | Some participants’ phones are disconnected, their numbers are changed, or they have only limited minutes | Participants provide a secondary contact the nurse can call if needed | Electronic medical records are a resource for finding alternate contact information when necessary; participants are sent hand-written notes to their last known address |
A variety of approaches were employed to facilitate clinical linkages to providers (Table 5). Based on provider preference, fax, phone, or secure e-mail was used to coordinate communication of structured program information. Provider turnover was a frequent challenge, and nurse educators coach participants to identify and establish appointments with a new provider when necessary.
TABLE 5.
Nurses Coordinate Interdisciplinary Communication for Individuals With Comorbid SMIand Diabetes: Overcoming Challenges and Promoting Interaction
| Communication Issues | Challenges | Highlights | Interactive Opportunities |
|---|---|---|---|
| Clinical linkages | Establishing contact and preferred mode of contact with participants’ providers | Primary and mental health care providers are informed of participants’ enrollment and provided regular updates regarding their patients’ progress in the program | Participants provide mental health care and primary care provider information at session 1; nurse educators establish liaison from a variety of health systems and settings; communication is provided per provider preference by fax, electronic medical record, or phone |
| Primary and mental health care provider turnover | Turnover hinders consistent communication regarding patients’ participation | Participants have opportunities to give updated provider contact information | Nurse educators become aware of provider turnover via electronic medical record; participants are encouraged to notify nurse educators of changes in providers; TTIM encourages participants to have a provider and to keep appointments |
| Participants' lack of an identified mental health provider or consistent mental health care | Some participants do not recognize their need for mental health care and minimizing their SMI; some think having a mental health care provider adds to their stigma | Nurse educators encourage participants to develop a relationship with a mental health provider throughout the sessions | Nurse educators facilitate referral to a mental health professional when participants come to understand the role or purpose of having a mental health provider |
Nurse educators completed follow-up contacts with TTIM participants to support progress relative to their PC plan and to check on their follow-up with their primary and mental health care providers. Many TTIM participants reported looking forward to the contacts. As participants’ goals were achieved, changed, or modified, these were communicated to their providers.
Discussion
Best-practice programs have been adapted using nurses to teach individuals with specific chronic diseases (1,3–5,13,18). Nurses working in primary care settings are ideally positioned to teach self-management to individuals with concurrent diabetes and SMI, and the TTIM approach supports both adaptability and flexibility in delivering the intervention in these settings. For the TTIM study, nurses with clinical experience who were not specialized in either diabetes self-management or psychiatric nursing effectively provided education and support related to both diabetes and SMI self-management. The nurse-lead TTIM approach was highly acceptable to individuals with SMI and diabetes. Eighty percent of individuals randomized to TTIM attended at least 1 session, and of those, the mean number of sessions attended was 8 of 12. This relatively high level of engagement is particularly notable considering barriers such as depression, paranoia, and stigma that people with SMI may encounter in completing activities that require sustained motivation.
Classes were highly participatory. Shared mutual support and success bolstered participants’ confidence. Challenges to the delivery of TTIM included inconsistent participant attendance, provider turnover, peer educators’ illness severity, participants’ symptoms impeding some group interactions, and inconsistent peer behavioral modeling. Nurse educators managed these by implementing strategies to enhance participant attendance, providing opportunities to make up missed sessions, supporting participants in cases of provider turnover, facilitating/maximizing group processes, considering participants’ diversity in disease severity, and capitalizing on teachable moments.
Nurse educators found the TTIM instructor’s manual to be user-friendly and effective. This manualized approach can be applied in all systems of care (e.g., cross-referral, bidirectional, or integrated [9]) by training nurses using existing resources to address the self-care needs of patients with complex comorbidities. Nurse educators’ activities addressing patient-specific factors facilitated participants’ self-management for both SMI and diabetes.
Future Implications
Mandersheid and Kathol (9) described the current status of primary care and behavioral health integration. They reported that nearly half of patients with chronic medical conditions also have comorbid behavioral health–related illnesses. They argue that 90% of such patients can be effectively managed in patient-centered medical homes and that patients with more severe behavioral health conditions (e.g., schizophrenia, bipolar disorder, and severe major depression—the specific illnesses for which the TTIM intervention was designed) will continue to be candidates for specialty behavioral health management. We believe that the enhanced self-management knowledge and skills available through the TTIM intervention would be useful to patients seen in primary care or specialty behavioral health care settings.
With emerging health system changes in the United States and implementation of the Affordable Care Act, more people with comorbid mental illness and diabetes will have access to providers under a single care system. We believe that nurse educators are ideally suited to deliver the TTIM intervention within the medical home model. The program’s manualized approach ensures that nurse educators have sufficient support to acquire needed knowledge and extends the scope and impact of nursing personnel.
Patients who might otherwise drop out of treatment because of perceived stigma may become engaged and communicate better with members of their health care team. Programs such as TTIM that increase self-management skills and use staff already embedded in primary care settings need to be implemented and further evaluated. This type of intervention could be embedded in medical homes and accountable care organizations as payment structures are redesigned in the context of health care reform.
Duality of Interest
No potential conflicts of interest relevant to this article were reported.
Funding
Research reported in this publication was supported by the National Institute of Mental Health of the National Institutes of Health (NIH) under award number R01MH085665. The project described was also supported by the National Center for Research Resources, grant UL1RR024989, and is now at the National Center for Advancing Translational Sciences, grant UL1TR000439. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
References
- 1.Chiverton P, Lindley P, Tortoretti DM, Plum KC. Well balanced: 8 steps to wellness for adults with mental illness and diabetes. J Psychosoc Nurs Ment Health Serv 2007;45:46–56 [DOI] [PubMed] [Google Scholar]
- 2.Mental Health America Position statement 13: Integration of mental and general health care. Available from http://www.mentalhealthamerica.net/positions/integrated-care. Accessed 24 August 2015
- 3.Kahn LS, Fox CH, Carrington J, et al. . Telephonic nurse case management for patients with diabetes and mental illness: qualitative perspective. Chronic Illn 2009;5:257–267 [DOI] [PubMed] [Google Scholar]
- 4.Sajatovic M, Dawson NV, Perzynski AT, et al. . Optimizing care for people with serious mental illness and comorbid diabetes. Psychiatrc Serv 2011;62:1001–1003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Blixen C, Perzynski A, Sajatovic M, Dawson NV. Treating severe mental illnesses and comorbid medical conditions in the primary care setting: an idea whose time has come. Cut Edge Psychiatry Pract 2011;3:106–110 [Google Scholar]
- 6.Falck-Ytter C, Baskaran G, Sanders C, Newshutz L, Einstadter D. Continued benefit from a diabetes group clinic (DGC) in an urban population. Poster session presented at the 35th Annual Meeting of the Society for General Internal Medicine. Orlando, Fla., May 2012
- 7.Kahn LS, Pastore PA, Rodriguez EM, et al. . A community-academic partnership to adapt a curriculum for people with serious mental illnesses and diabetes. Prog Community Health Partnersh 2012;6:443–450 [DOI] [PubMed] [Google Scholar]
- 8.Scott D, Platania-Phung C, Happell B. Quality of care for cardiovascular disease and diabetes amongst individuals with serious mental illness and those using antipsychotic medications. J Healthc Qual 2012;34:15–21 [DOI] [PubMed] [Google Scholar]
- 9.Mandersheid R, Kathol R. Fostering sustainable integrated medical and behavioral health services in medical settings. Ann Intern Med 2013;160:61–65 [DOI] [PubMed] [Google Scholar]
- 10.van Os-Medendorp H, Eland-de Kok PC, Ros WJ, Bruijnzeel-Koomen CA, Grypdonck M. The nursing programme ‘Coping with Itch’: a promising intervention for patients with chronic pruritic skin diseases. J Clin Nurs 2007;16:1238–1246 [DOI] [PubMed] [Google Scholar]
- 11.Macdonald W, Rogers A, Blakeman T, Bower P. Practice nurses and the facilitation of self-management in primary care. J Adv Nurs 2008;62:191–199 [DOI] [PubMed] [Google Scholar]
- 12.Blixen CE, Murphy D, Ault V, Hammel J. Feasibility of a nurse-run asthma education program for urban African Americans: a pilot study. J Asthma 2004;38:23–32 [PubMed] [Google Scholar]
- 13.Leak A, Davis ED, Houchin LB, Marbrey M. Diabetes management and self-care education for hospitalized patients with cancer. Clin J Oncol Nurs 2009;13:205–210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Du S, Yuan C. Evaluation of patient self-management outcomes in health care: a systematic review. Int Nurs Rev 2010;57:159–167 [DOI] [PubMed] [Google Scholar]
- 15.Moriyama M, Nakano M, Kuroe Y, Nin K, Niitani M, Nakaya T. Efficacy of a self-management education program for people with type 2 diabetes: results of a 12 month trial. Japan J Nurs Sci 2009;6:51–63 [DOI] [PubMed] [Google Scholar]
- 16.Blixen CE, Bramstedt KA, Hammel JP, Tilley BC. Health education via a nurse-run telephone self-management program for older adults with osteoarthritis: a pilot study. J Telemed Telecare 2004;10:44–49 [DOI] [PubMed] [Google Scholar]
- 17.Bauer MS, McBride L, Williford WO, et al. . Collaborative care for bipolar disorder: part II. impact on clinical outcome, function, and costs. Psychiatr Serv 2006;57:937–945 [DOI] [PubMed] [Google Scholar]
- 18.Kahn LS, Glaser K, Fox CH, Patterson A. Diabetes Educators in Safety-Net Practices: a qualitative study. Diabetes Educ 2011;37:212–219 [DOI] [PubMed] [Google Scholar]