Abstract
EDITOR’S NOTE: This article is adapted from the address of the American Diabetes Association (ADA) President, Health Care and Education, given in June 2015 at the Association’s 75th Scientific Sessions in Boston, Mass. A webcast of this speech is available for viewing at the ADA website (http://professional.diabetes.org/webcasts).
I have lived with type 1 diabetes for 39 years. Today, I would like to talk about how research has affected my life as a person with diabetes. Now, before you say, “Great, another ADA talk extolling the importance of funding research,” I want to be clear: although I do want to mention the amazing advances we have made, I also want to discuss what I believe what we have failed to do and, in this context, what research needs to focus upon in the future.
In the past four decades, I have seen many changes in how my disease has been treated, almost all of which have been the result of research and clinical trials. When I was diagnosed, my therapeutic options were limited. There was only animal-species insulin, and there were only two choices for basal insulin and one for short-acting insulin. In type 2 diabetes, there was only one oral medication. Home glucose monitoring did not exist to assess daily control—only urine testing, which was imprecise, to say the least. There were no A1C assessments to evaluate the adequacy of therapy. Disposable syringes had just become available, and the needles were about the gauge of a threepenny nail. There were few effective treatments for complications.
So, what changes have occurred in the clinical treatment of diabetes in the past 40 years? New insulins and new drugs have become available, allowing much better glycemic control today than was achievable a few short decades ago. The advent of self-monitoring of blood glucose occurred. Early meters were amazing but plagued by issues of user error and unreliable accuracy. Today’s meters are faster, smaller, and more accurate. They allow users to really know what is happening with their therapy and meal decisions. Lancet devices have improved. We used to prick our fingers by hand, a literal act of willpower to overcome the body’s natural avoidance of sticking sharp objects into itself. Recognizing this limitation, the Bayer company introduced an automated device that many users nicknamed “the guillotine.” Today, there are several models that make a painful process more tolerable. More recently, continuous glucose monitoring allowed me to see for the first time real-time responses to changes in my medication, diet, and activity and even to anticipate glucose lows and highs before they happened and take action to avoid them. Accurate A1C tests are now available—even ones I can do at home. Very-small-gauge needles are now common, and I can use insulin pens instead of vials and syringes. Alternatively, I can use an insulin infusion pump. These devices more accurately mimic the body’s natural delivery of insulin and allow for greater flexibility in daily diabetes management.
We’ve come a long way, and ongoing, innovative research is what got us here. But we still have a long way to go. Even with all of these innovative medications and technologies, my biggest obstacle to maintaining good control of my diabetes is me. I am the one who has to check my blood glucose several times each day to determine my insulin doses and make sure I’m not going to hit the floor. Every time I eat or exercise, I have to determine how that will affect my blood glucose. When I go to bed at night, it’s hard not to wonder if I’m going to actually wake up in the morning.
And I am one of the lucky ones. I am around “diabetes people” all the time, both at work and when I am collaborating with colleagues at the American Diabetes Association (ADA). I am not alone with my diabetes; I have support, and I have immediate access to the best diabetes experts in the country. Most people are not so lucky.
It has been estimated that individuals with diabetes spend almost 9,000 hours each year managing their diabetes on their own. My friend Manny Hernandez, formally of the Diabetes Hands Foundation, put together an image to illustrate the relationship between the time spent self-managing diabetes and time spent with a health care provider (Figure 1). The blue in this circle can be seen as how often we don’t see a doctor or a diabetes educator, and the white as the time spent with a health care professional. In the course of a whole year, we are in the company of a medical professional for our diabetes only ∼0.1% of the time. This is very much a condition we have to manage on our own, and it is not easy. Imagine for a second how it must feel not to have anyone else to talk with or share this thing with that you live with 24/7.
FIGURE 1.
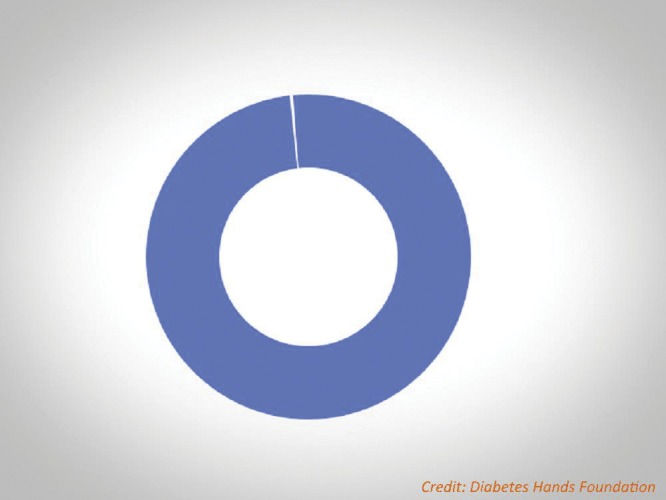
Image illustrating the relationship between the time spent self-managing diabetes (blue) and time spent with a health care provider (white). Credit: Diabetes Hands Foundation, www.diabeteshandsfoundation.org.
Where does research need to focus in the future? What advances have not been made that would improve the lives of those with diabetes? What is the next research frontier? To address this question, let’s go back again to 40 years ago, when I was first diagnosed.
I was in graduate school at the time. Naturally, the diagnosis of type 1 diabetes was quite a shock, requiring rather drastic changes in my lifestyle. Like any good graduate student in psychology, I went to the library to see what had been written about coping with this disease. I was shocked to discover that there were hardly any articles about the mental health issues I found myself experiencing. Those that did exist had been mostly written in the 1940s and ’50s and mainly focused on “the Freudian personality and diabetes.”
Although it was tempting to blame my diabetes on my mother, I realized that this was not going to be productive. Equally disturbing was that the sparse available literature seemed to depict patients as being either “good” or “bad,” a distinction that was defined by factors such as “compliance,” “adherence,” and “listening to the doctor.” There were no studies that even attempted to understand the behavioral demands of diabetes, and little research or scholarly attention had been paid to coping and mental health in people with diabetes.
When I complained to my advisor about the sorry state of scholarship and understanding in this area, he suggested that I focus my dissertation on coping with diabetes because my training in psychology provided me with the skills to do this. I elected to study adolescents with a history of very poor control, most of whom had had at least three hospital admissions for diabetic ketoacidosis (DKA) per year. I spent a year interviewing a group of 27 adolescents and their families, all united by a history of multiple annual hospitalizations for DKA. They were all viewed by their physicians as “bad patients” who were fated to die an early and unpleasant death.
First, I quickly learned that these individuals knew what was needed to maintain glycemic control. Indeed, with each hospitalization, the basic response of the care team was to “reeducate” them. This was coupled by their physicians telling them, yet again, how they were going to go blind, lose their feet, and die a slow and miserable death. Not one of these kids was offered any psychological counseling. They also taught me that the reasons for their apparent noncompliance were complex, multifaceted, and steeped in behavioral, rather than clinical, issues.
Where are we today with understanding the behavioral aspects of diabetes? Has research transformed the behavioral and mental health areas over the past four decades as it has done in the clinical arena? It is clear that diabetes remains unique among chronic conditions in the extent to which therapy is controlled by the patient and the factors that shape behavior. It is also clear that how people deal with diabetes is more than simply personal decisions or “acts of will” that control outcomes. Rather, we have become increasingly aware of several factors that affect therapy, including health literacy, education level, socioeconomic status, environmental factors, and mental health status.
We are also increasingly aware that people with diabetes suffer from mental health issues more than their brethren without diabetes. Indeed, we now know that people with diabetes are more than twice as likely as others to face depression or varying degrees of mental health issues. However, this is something that, traditionally, has not been talked about very much and has not received adequate attention.
The World Health Organization (WHO) reported that mental illnesses are the leading causes of disability-adjusted life-years worldwide, accounting for 37% of healthy years lost from noncommunicable diseases (NCDs) (1). Depression alone accounts for one-third of this disability (2,3). WHO estimated the global cost of mental illness at nearly $2.5 trillion (two-thirds in indirect costs) in 2010, with a projected increase to over $6 trillion by 2030.
The WHO report (1) also provided comparisons across NCDs to give some sense of the drivers of global economic burden. Mental health costs are the largest single source—larger than cardiovascular disease, chronic respiratory disease, cancer, or diabetes. Mental illness alone will account for more than half of the projected total economic burden from NCDs in the next two decades and for 35% of the global lost output. The report concluded that, worldwide, mental illnesses are the largest single driver of these costs. Importantly, these costs can be controlled.
The National Institutes of Health (NIH) has addressed mental health issues in diabetes specifically (4), stating:
Studies show that depression and diabetes may be linked, but scientists do not yet know whether depression increases the risk of diabetes or diabetes increases the risk of depression. Current research suggests that both cases are possible.
In addition to possibly increasing your risk for depression, diabetes may make symptoms of depression worse. The stress of managing diabetes every day and the effects of diabetes on the brain may contribute to depression (5,6) In the United States, people with diabetes are twice as likely as the average person to have depression (7).
At the same time, some symptoms of depression may reduce overall physical and mental health, not only increasing your risk for diabetes but making diabetes symptoms worse. Studies have shown that people with diabetes and depression have more severe diabetes symptoms than people who have diabetes alone.”
What is our current research investment? Let’s start by looking at the NIH portfolio. Of the 5,046 grants currently funded by the National Institute of Diabetes and Digestive and Kidney Diseases, 40 dealt with mental health or any behavioral focus, regardless of whether they focused on diabetes. That is 0.8% of the total funding. How about the National Institute of Mental Health, the agency whose name reflects its charge to address mental health issues? Of its current 3,648 grants, although many deal with depression, only 35 have any mention of diabetes in their titles. That is 0.9% of its total funding.
How is ADA doing in this regard? Table 1 shows the number of behavioral or psychosocial grants submitted since 2012. As shown in the table, a very small percentage of these grants focus on behavioral or psychological issues, with only 3% receiving funding. Although this is still significantly better than federal research funding sources, behavioral and mental health research is still woefully underrepresented.
TABLE 1.
Number of Behavioral or Psychosocial Grants Submitted to ADA Since 2012
| Year | Total Submissions | Behavioral/Psychosocial Submissions | Percentage of Total Submissions |
|---|---|---|---|
| 2012 | 887 | 18 | 2 |
| 2013 | 860 | 30 | 3.5 |
| 2014 | 927 | 36 | 3.8 |
| 2015 | 571 | 17 | 3 |
Where does this leave us in considering mental health issues in diabetes? Despite the clear role behavioral factors and mental health play in diabetes treatment, they have not received the attention they deserve with regard to research and research funding. Clearly, given the magnitude of the problem, the next frontier of research in diabetes needs to focus more on behavior and mental health if we are going to continue the success in the clinical treatment and management of diabetes that we have seen in the past 40 years. We need significant increases in funding for research that will help identify the best strategies for integrating chronic illness services with care for a broad range of mental health conditions. We need to turn more of our attention to which behavioral interventions are most effective and how they can be appropriately scaled up.
Some of our specific needs include:
An increase in the number of highly trained people who can effectively address the mental health issues associated with adapting to and coping with diabetes treatment
More research into the behavioral aspects of diabetes care to guide health care providers in addressing and supporting the emotional needs of their patients as part of routine care
Guidance for policymakers who control health care spending to ensure that all individuals with diabetes have unfettered access to the quality care, medications, and management tools they need to effectively control their diabetes
How is ADA responding to these needs? We are entering into collaboration with the American Psychological Association to develop training programs for psychologists, focusing specifically on the unique needs of people with diabetes. In addition, the U.S. Food and Drug Administration has initiated a patient-focused drug development initiative to incorporate patient preferences and patient-reported outcomes into the review process for drugs and devices, and it has asked ADA to provide recommendations about best assessment techniques for measuring patient-reported outcomes and how new treatments affect quality of life. This initiative will allow ADA to make a meaningful contribution to FDA decisions about the acceptability of new treatments to the patients who will be using them.
Depression and related mental health disorders are so common in people with diabetes that they should be viewed as comorbid conditions. Unfortunately, they have not received the attention by the health care system that other comorbid conditions have. This is unfortunate in that mental health conditions can exact a considerable toll on both quality of life and treatment outcomes. Clearly, it is time to focus on this so that we can continue to make strides in the optimal treatment of people with diabetes.
Duality of Interest
No potential conflicts of interest relevant to this article were reported.
References
- 1.Bloom DE, Cafiero ET, Jané-Llopis E, et al. The Global Economic Burden of Noncommunicable Diseases. Geneva, Switzerland, World Economic Forum, 2011 [Google Scholar]
- 2.World Health Organization The Global Burden of Disease: 2004 Update. Geneva, Switzerland, World Health Organization, 2008 [Google Scholar]
- 3.World Health Organization Global Status Report on Non-Communicable Diseases, 2010. Geneva, Switzerland, World Health Organization, 2011 [Google Scholar]
- 4.National Institute of Mental Health Depression and diabetes. Bethesda, Md, National Institutes of Health (NIH Publication No. 11–5003), 2011 [Google Scholar]
- 5.Golden SH, Lazo M, Carnethon M, et al. Examining a bidirectional association between depressive symptoms and diabetes. JAMA 2008;299:2751–2759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kumar A, Gupta R, Thomas A, Ajilore O, Hellemann G. Focal subcortical biophysical abnormalities in patients diagnosed with type 2 diabetes and depression. Arch Gen Psychiatry 2009;66:324–330 [DOI] [PubMed] [Google Scholar]
- 7.Egede LE, Zheng D, Simpson K. Comorbid depression is associated with increased health care use and expenditures in individuals with diabetes. Diabetes Care 2002;25:464–470 [DOI] [PubMed] [Google Scholar]


