Abstract
Aims
A randomized controlled trial of brief intervention (BI), for drinking and related problems, using peer health promotion advocates (promotores), was conducted among at-risk and alcohol-dependent Mexican-origin young adult emergency department (ED) patients, aged 18–30.
Methods
Six hundred and ninety-eight patients were randomized to: screened only (n = 78), assessed (n = 310) and intervention (n = 310). Primary outcomes were at-risk drinking and Rapid Alcohol Problems Screen (RAPS4) scores. Secondary outcomes were drinking days per week, drinks per drinking day, maximum drinks in a day and negative consequences of drinking.
Results
At 3- and 12-month follow-up the intervention condition showed significantly lower values or trends on all outcome variables compared to the assessed condition, with the exception of the RAPS4 score; e.g. at-risk drinking days dropped from 2.9 to 1.7 at 3 months for the assessed condition and from 3.2 to 1.2 for the intervention condition. Using random effects modeling controlling for demographics and baseline values, the intervention condition showed significantly greater improvement in all consumption measures at 12 months, but not in the RAPS4 or negative consequences of drinking. Improvements in outcomes were significantly more evident for non-injured patients, those reporting drinking prior to the event, and those lower on risk taking disposition.
Conclusions
At 12-month follow-up this study demonstrated significantly improved drinking outcomes for Mexican-origin young adults in the ED who received a BI delivered by promotores compared to those who did not.
Trial Register
ClinicalTrials.gov.
Clinical Trial Registration Number
INTRODUCTION
Mexican-origin Hispanics are the largest minority group in the USA, constituting over half of those living in the 24 US counties bordering Mexico, among whom a high proportion are under 35 (United States Census Bureau, 2012). Young adults in the USA have the highest rates of alcohol consumption and alcohol-related problems, compared to other age groups, and those residing at the US–Mexico border may be especially vulnerable to at-risk drinking and related problems, due to alcohol advertising, and in Mexico, poor enforcement of drinking age (18) and greater availability of alcohol at low cost. While volume of consumption among Mexican-Americans living at the Texas–Mexico border is no greater than that for those living off the border, rates of alcohol use disorders (AUDs) are high (Wallisch and Spence, 2006), with 30% reporting one or more episodes of binge drinking (5 or more drinks on an occasion) during the previous month, and 23% reporting symptoms of alcohol dependence among those aged 18–25 (Wallisch, 1998; Wallisch and Spence, 2006), with El Paso, site of the present study, reporting the second highest rates in Texas (Lawrence, 1998). Despite elevated rates of at-risk drinking and AUD among Mexican-origin young adults living along the border, no studies have been reported on brief intervention (BI) in the emergency department (ED) for drinking and related problems in this age and ethnic group, although the ED is the main point of access for medical care for many of these individuals (de Cosío and Boadella, 1999).
Outcome studies of BI among ED patients have reported mixed results (Longabaugh et al., 2001; Rodríguez-Martos Dauer et al., 2003; Field and Caetano, 2010; D'Onofrio et al., 2013). In view of negative findings in several studies in ED settings, recommendations for future research have suggested the possible key role of specific types of ‘messengers’ delivering the intervention (Bernstein and Bernstein, 2008). One such ‘messenger’ is the trained Health Promotion Advocate (HPA) who is increasingly becoming an integral part of routine ED service (Bernstein et al., 2009). ‘Promotores’, who are community-based Mexican-origin peer HPAs, recruited based on their bilingual/bicultural skills, ethnic identification with the target population, communication skills and familiarity with local referral resources, have been used successfully in health promotion activities in Hispanic community settings (Warrick et al., 1992; Ramos and Ferreira-Pinto, 2006; Ramos et al., 2006) but there are no reports of their use to deliver BI for drinking and related problems. Protomores might be expected to be particularly effective in delivering BI to Mexican-origin young adults in the ED, given their long-established success in other health promotion and prevention activities in the Mexican-origin community.
The present study examines the efficacy of BI applied to Mexican-origin young adults in the ED at the US–Mexico border in El Paso, TX, using ‘promotores’ conversant in Spanish and English, and represents the first such randomized controlled clinical trial of BI using promotores. While existing ED staff have been shown to be effective providers of BI (D'Onofrio et al., 2013) they have limited time and competing priorities that present barriers to implementation of BI.
Reported here are findings from a 3- and 12-month follow-up assessment of drinking and related problems for those receiving only an assessment at baseline compared to those also receiving an intervention. We hypothesized that those in the intervention condition would report significantly greater reductions in primary outcomes of at-risk drinking and symptoms of alcohol dependence, and secondary outcomes of drinking days per week, drinks per drinking day, maximum drinks in a day, and negative consequences of drinking, compared to the assessed condition at 12-month follow-up.
Since ED admission for an injury has been thought to be a time when patients might be more inclined to change their drinking behavior (Conigrave et al., 1991; Monti et al., 1999), especially if they had been drinking prior to the injury event, and those more disposed to risk taking may be less inclined to behavioral change due to perceived lack of vulnerability (Donovan et al., 1988), we hypothesize in subgroup analysis that admission to the ED with an injury and self-reported drinking prior to the injury or illness event would positively predict efficacy of the intervention, while risk taking/impulsivity and sensation seeking dispositions would negatively predict efficacy.
METHODS
Patient screening, eligibility, recruitment and randomization
A cadre of interviewers were trained by the authors and supervised by survey research staff from Texas Tech University Health Sciences Center (TTUHSC) in El Paso to carry out patient screening, recruitment, assessment and randomization procedures.
Screening and eligibility
Patients aged 18–30 presenting to the ED at TTUHSC between 10:00 am and 10:00 pm 7 days a week, who self-identified as Mexican-origin and lived in El Paso County, were eligible for screening. Screening was based on questions about the usual quantity and frequency (Q-F) of drinking as a measure of at-risk drinking and the Rapid Alcohol Problems Screen (RAPS4) (Cherpitel, 2000) as a measure of alcohol dependence. Patients met eligibility criteria for the study if they were positive for at-risk drinking (reporting 15 or more drinks per week for males/8 or more for females, or 5 or more drinks in a day for males/4 or more for females, all over the past 28 days), or met criteria for Diagnostic and Statistical Manual 4th revision (DSM-IV) alcohol dependence (American Psychiatric Association, 1994) (positive on any one of the RAPS4 items during the last year: feeling of guilt or remorse after drinking, being told by a friend or family member about things said or did while drinking that could not be remembered, failed to do what was normally expected because of drinking, sometimes taking a drink in the morning when first get up). Eligibility criteria also included: (a) willingness to be randomized into one of three conditions: (i) screened only with 12-month assessment, (ii) screened plus baseline assessment with 3- and 12-month follow-up assessments, (iii) screened plus baseline assessment and receive the intervention with 3- and 12-month follow-up assessments; and (b) willingness to provide contact information for at least two individuals who would always know their whereabouts. Exclusion criteria included admitted to the hospital for inpatient treatment, currently in alcohol treatment, or planning to leave the El Paso metropolitan area.
Recruitment, randomization and attrition
Eligible patients were provided an informed consent to participate, and once signed were randomized using a two-stage process. In the first stage patients who screened positive were randomized to whether or not they would receive a baseline assessment by the study interviewer who drew an envelope indicating if the assessment was to be given. Those who did not receive an assessment were assigned to the screened-only condition. The envelope of those receiving an assessment contained a second envelope, which was opened by the interviewer following assessment, to determine whether the patient was assigned to the intervention condition. Due to slower recruitment than anticipated, a decision was made after completing 12 months to discontinue the screened-only condition, so that all patients received the assessment and were then randomized to the intervention condition in order to assure adequate numbers for analysis in the assessment and intervention conditions.
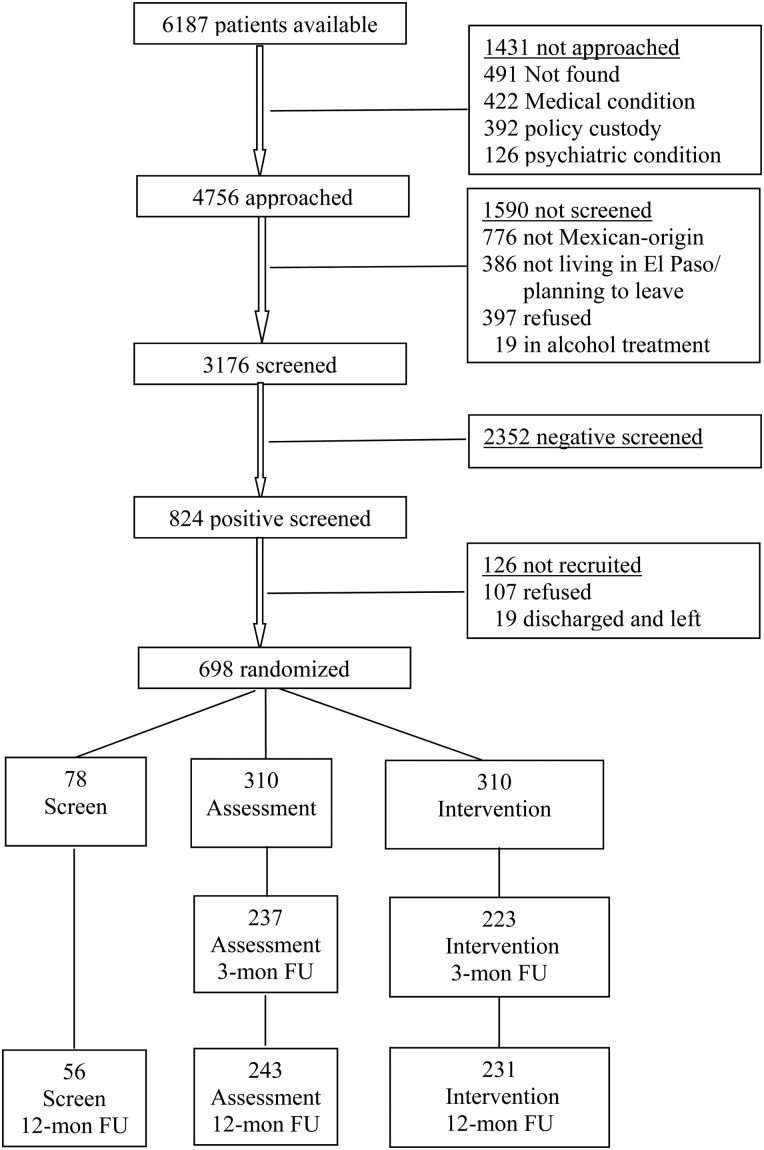
Patient recruitment continued over a 17-month period (November 2010–April 2012), and resulted in 3176 screened individuals. Figure 1 shows the CONSORT Diagram (Schulz et al., 2010) flow chart. Of those screened, 26% (n = 824) screened positive and of these, 85% (n = 698) were recruited into the study: 78 were randomized to the screened condition and 310 to each of the assessment and intervention conditions. Follow-up rates at 12 months were 72% for the screened condition (n = 56), 78% for the assessment condition (n = 243) and 75% for the intervention condition (n = 231). Patients in the screened-only condition received a list of Alcoholics Anonymous (AA) groups and specialized services for alcohol treatment and counseling.
Fig. 1.
Screening, recruitment and follow-up rates.
Baseline assessment
Patients randomized to the assessment and intervention conditions were asked questions regarding the reason for the ED visit, self-reported drinking within 6 h prior to the event bringing them to the ED, Q-F of usual drinking, negative consequences of drinking, and risk taking/impulsivity and sensation seeking disposition. Baseline assessment included the following standardized instruments.
The Timeline Followback (Sobell and Sobell, 1992) was used to assess Q-F of drinking over the last 28 days, including number of drinking days, number of drinks per drinking day and the maximum number of drinks per day.
The Short Inventory of Problems (SIPs + 6) (Miller et al., 1995), a brief version of the Drinking Inventory of Consequences, was used to assess negative consequences related to drinking over the last 3 months and includes 15 consequence items related to physical, social responsibility, intrapersonal, impulse control and interpersonal domains, with six additional questions from the original instrument on injury and drink driving.
Risk taking/impulsivity was assessed from five items adapted from Eysenck and Eysenck (1977) and Jackson (1974), and sensation seeking from four items on novelty and thrill seeking adapted from Zuckerman (1979). Each item for both dispositions was measured on a 4-point scale, summed across items for each disposition, separately, and then combined as a single measure (Cherpitel, 1993).
Instruments were translated into Spanish, verified by back-translation (Breslin, 1986) or expert attestation. Patients could choose whether they preferred to be interviewed in English (75%) or in Spanish (10%); 15% were conducted in both languages.
Patients randomized to the screening plus assessment condition received a list of AA groups and specialized services for alcohol treatment and counseling.
Intervention
Patients randomized to the intervention condition received a brief motivational intervention by promotores who had been trained in BI using the Brief Negotiation Interviewing (BNI) protocol (Bernstein et al., 1997) which integrates the following elements with readiness to change (Prochaska and DiClemenmte, 1992): (a) establishing a relationship of empathy and trust with the patient and gaining permission to discuss drinking (engagement and permission), (b) providing the patient with feedback about their drinking based on safe drinking guidelines (feedback, information and norms), (c) asking the patient to discuss the pros and cons of their drinking (decisional balance), (d) assessing the patient's readiness to change their drinking behavior (readiness to change), (e) providing the patient with options regarding changing drinking behavior (menu of options) and (f) negotiating with the patient their goal for reducing drinking and strategies for achieving this (prescription for change, in which the promotore and the patient sign a plan of action for change in the patient's drinking). The intervention was designed to take about 20 min to complete and was generally provided in a private area near the waiting room while the patient was waiting for treatment, or in the treatment area. A list of AA groups, general resources, and specialized services for alcohol treatment and counseling was provided to the patient.
Training of promotores
A unique feature of this study was the use of community-based Mexican-origin peer HPAs, called promotores, to deliver the intervention. Training in BI was provided on-site by the project team, utilizing protocols established in training at all sites (Bernstein et al., 2007) in the Academic Emergency Medicine Collaborative SBIRT (Screening, Brief Intervention and Referral to Treatment) study (Academic ED SBIRT Research Collaborative, 2007). Four promotores received a 3-day training which included practice interventions with patients in the ED, in the presence of study staff, and two booster training sessions.
Monitoring fidelity to treatment and controlling potential threats to validity
As a measure of integrity, interventions were initially observed by supervisory staff with a patient's consent and immediate feedback provided to the promotore to assure high quality of the intervention. Additionally, with a patient's consent, interventions were taped and any deviation from the intervention protocol was discussed with the promotore. Brief exit interviews were conducted by interviewers regarding whether the promotore had talked with the patient about their drinking, patient satisfaction with the intervention and whether a contract agreement was reached.
Three- and twelve-month follow-up assessment
Those in the assessment and intervention conditions were assessed at 3 months and all three groups were assessed at 12 months via telephone by an interviewer blinded to group status, using the RAPS4, Timeline Followback and SIPS + 6. Patients were also asked whether they obtained treatment for their drinking in the last 3 months.
Data analysis
Chi-square and T-tests were used for bivariate comparisons. A random effects model was used to examine the intervention effect, which allows for unbalanced data due to loss to follow-up, issues related to missing data and potential bias, and accounts for correlation in errors resulting from repeated measures on the same individuals over time. The change in primary and secondary outcomes between the intervention and assessment conditions were compared, controlling for age, gender, country of birth (USA or Mexico), and baseline values for the total sample and, separately, by injury status, drinking prior to the event, and risk taking/impulsivity and sensation seeking.
Distributions of the continuous primary and secondary outcome measures demonstrated evidence of non-normality, indicated by large skewedness and kurtosis estimates, and were log-transformed. The specific model estimated was: yi,t = αi + β1·Gi + β2·t3 + β3·t12 + β4·Gi·t3 + β5·Gi·t12 + εi,t where t3 and t12 are indicator variables representing observations collected at 3- and 12-month interviews, and Gi = 0,1 if the ith case was assigned to the assessed and intervention conditions, respectively. The β2 coefficient represents change in drinking from baseline to the 3-month interview when G equals 0 (i.e. for the assessed condition); β3 represents the corresponding difference between baseline and the 12-month interview. The β1 estimate represents the difference in drinking variables between the assessed and intervention conditions at baseline. Last, β4 and β5 estimate the corresponding intervention effect at 3 and 12 months, which can be seen as the post-pre difference (i.e. 3-month or 12-month minus baseline) in outcomes for the intervention condition minus the analogous difference for the assessed condition (i.e. a difference in differences).
RESULTS
No significant differences were found in baseline variables between the assessed and intervention conditions, except for age, where the difference, while statistically significant due to the small age range (18–30), was minimal, suggesting randomization was achieved across conditions at baseline (Table 1).
Table 1.
Baseline comparison between the assessment and intervention groups
| Screen onlya | Assess | Intervene | Pb | |
|---|---|---|---|---|
| N | 78 | 310 | 310 | |
| Gender male, % | 52.6 | 54.4 | 58.3 | 0.330 |
| Age, mean (SDb) | 24.0 (3.4) | 24.3 (3.5) | 23.6 (3.5) | 0.009 |
| Born in the USA, % | N.A. | 81.9 | 77.3 | 0.156 |
| Injured, % | N.A. | 38.3 | 33.9 | 0.250 |
| Drinking before event, % | N.A. | 13.9 | 17.7 | 0.192 |
| Risk taking scale, mean (SD) | N.A. | 13.7 (7.5) | 13.3 (7.4) | 0.551 |
| Primary outcomes | ||||
| Days of 5+/4+ men/women last 28-day, mean (SD) | N.A. | 2.92 (4.15) | 3.16 (4.56) | 0.704 |
| Any RAPS4 positive last 3 months, % | 32.1 | 37.7 | 40.0 | 0.564 |
| Secondary outcomes | ||||
| No. of drinking days per week last 28-day, mean (SD) | 1.77 (1.60) | 1.06 (1.21) | 1.12 (1.24) | 0.394 |
| Drinks per drinking day last 28-day, mean (SD) | 5.86 (3.50) | 6.15 (4.83) | 5.99 (4.58) | 0.914 |
| Maximum drinks last 28-day, mean (SD) | 8.13 (3.76) | 8.53 (7.61) | 8.49 (7.16) | 0.695 |
| SIPs + 6 count last 3 months, mean (SD) | N.A. | 3.49 (4.01) | 3.51 (4.25) | 0.758 |
SD, standard deviation.
aScreen only group individuals were only asked the screening questions, thus not available (N.A.) for the assessment questions. In addition, other than the RASP4%, the three drinking outcomes shown for the screen only groups are from the screen items too, rather than from the time line follow-back questions used for Assess and Intervention groups, thus their estimates are not directly comparable. For example, the number of drinking days per week for the screen only group was based on the question: on average, how many days a week do you drink alcohol.
bP-values are based on tests between the Assess and the Intervention groups only, with t-tests for continuous measures and Chi-square tests for categorical measures; all continuous drinking outcomes were log-transformed due to their skewed distribution.
Table 2 shows drinking outcomes at 3 and 12 months for the assessed compared to the intervention condition. At both follow-ups the intervention condition showed significantly or marginally significantly lower values on all outcome variables compared to the assessed condition, with the exception of the RAPS4 score.
Table 2.
Drinking outcomes at 3- and 12-month follow-up, for assessment and intervention groups, separately
| 3-month |
12-month |
|||||
|---|---|---|---|---|---|---|
| Assessed | Intervention | P-valuea | Assessed | Intervention | P-valuea | |
| N | 237 | 223 | 243 | 231 | ||
| Primary outcomes | ||||||
| Days of 5+/4+ men/women last 28-day, mean (SD) | 1.66 (3.32) | 1.17 (2.12) | 0.087 | 2.43 (4.19) | 1.46 (2.95) | 0.001 |
| Any RAPS4 positive last 3 months, % | 23.6 | 19.7 | 0.311 | 14.4 | 14.3 | 0.971 |
| Secondary outcomes | ||||||
| No. of drinking days per week last 28-day, mean (SD) | 0.72 (1.06) | 0.56 (0.92) | 0.066 | 1.13 (1.31) | 0.82 (1.21) | 0.003 |
| Drinks per drinking day last 28-day, mean (SD) | 3.90 (4.51) | 3.10 (3.88) | 0.065 | 3.08 (3.02) | 2.65 (3.13) | 0.040 |
| Maximum drinks last 28-day, mean (SD) | 5.08 (5.91) | 3.90 (4.87) | 0.044 | 4.75 (5.20) | 4.06 (5.50) | 0.035 |
| SIPs + 6 count last 3 months, mean (SD) | 1.55 (2.95) | 0.91 (2.02) | 0.011 | 1.35 (2.46) | 1.10 (2.46) | 0.047 |
aAll continuous measures (all variables except for RASP4 positive) were log-transformed for t-test; Chi-square test was used for RAPS4 positive.
Using random effects modeling, differences in improvement in outcomes between the intervention and assessed conditions are examined at 3- and 12-month follow-up (Table 3). For each drinking outcome, the table shows the coefficient estimates of the difference between assessed and intervention conditions at baseline (the group effect at baseline), the differences between baseline and 3 or 12 months for the assessed group (the time effect), and changes in drinking from baseline to 3 or 12 months for the intervention group vs the assessed group (the intervention effect as measured by interaction). Negative time effects were seen for almost all drinking variables at both 3 and 12 months, indicating decline in drinking from baseline. For estimates of intervention effects, at 3 months the intervention condition showed greater improvement than the assessed condition only in maximum drinks on an occasion, while at 12 months the intervention condition, compared to the assessed condition, showed greater improvement in all outcome variables with the exception of the RAPS4 and SIPs + 6 score.
Table 3.
Random effect model coefficients for change in drinking between baseline and 3- and 12-month follow-up for the total sample (N = 620 at baseline)a
| Interceptb (assess at baseline) | Group effect at baseline (intervention vs assess) | Time effect (3-month vs baseline) | Time effect (12-month vs baseline) | Interaction (3-month × intervention) | Interaction (12-month × intervention) | |
|---|---|---|---|---|---|---|
| Primary outcomes | ||||||
| Days of 5+/4+ men/women last 28-day | 0.69 (0.11) | 0.03 (0.06) | −0.43 (0.06)*** | −0.26 (0.06)*** | −0.12 (0.08) | −0.27 (0.08)*** |
| Any RAPS4 positive last 3 months | −1.15 (0.42) | 0.14 (0.23) | −0.95 (0.23)*** | −1.74 (0.27)*** | −0.36 (0.34) | −0.12 (0.37) |
| Secondary outcomes | ||||||
| No. of drinking days per week last 28-day | 0.40 (0.06) | 0.03 (0.04) | −0.19 (0.03)*** | −0.01 (0.03) | −0.09 (0.05)† | −0.17 (0.05)*** |
| Drinks per drinking day last 28-day | 1.36 (0.11) | 0.001 (0.07) | −0.55 (0.06)*** | −0.63 (0.06)*** | −0.17 (0.09)† | −0.18 (0.09)* |
| Maximum drinks last 28-day | 1.56 (0.12) | 0.02 (0.07) | −0.64 (0.07)*** | −0.65 (0.07)*** | −0.22 (0.10)* | −0.24 (0.10)* |
| SIPs + 6 count last 3 months | 1.02 (0.11) | −0.03 (0.06) | −0.58 (0.06)*** | −0.60 (0.06)*** | −0.12 (0.08) | −0.11 (0.08) |
aAll drinking outcome variable were log-transformed, except for any RAPS4 positive.
bSignificant tests not shown for intercepts.
†P < 0.10, *P < 0.05, ***P < 0.001.
Subgroup analysis was performed to investigate potential differential intervention effects by ED admission injury status (injured vs not-injured, Table 4), by drinking within 6 h prior to the injury or medical event (Table 5), and by patients' risk taking/impulsivity and sensation seeking disposition (Table 6). Improvement in outcomes was more evident, especially at 12 months, for non-injured patients, those who reported drinking prior to the event that precipitated the ED visit, and those lower on risk taking disposition. For example, while greater improvement at 12 months for the intervention condition compared to the assessed condition was observed in 5+/4+ days and number of drinking days for both injured and non-injured patients, significant additional reduction was also seen in drinks per drinking day and maximum drinks for the non-injured patients (the last column of Table 4), proving stronger evidence of the intervention effect for this subgroup compared to the injured patients. When the intervention effects were estimated separately for those who reported drinking before the event and those who did not (Table 5), four out of six 12-month outcomes were significant (P < 0.05) among those who reported drinking, while only one 12-month outcome was significant for those who did not report drinking. This 12-month intervention effect for those who reported drinking is even more evident considering its sample size is much smaller (n = 98) than for those who did not report drinking (n = 521), and thus having less power in significant testing. Lastly, the intervention effect appeared to be more evident for those lower on risk taking disposition compared to those higher, with a larger number of significant intervention effects observed for both 3- and 12-month outcomes (Table 6).
Table 4.
Random effect model coefficients for change in drinking between baseline and 3- and 12-month follow-up, by injury statusa
| Interceptb (assess at baseline) | Group effect at baseline (intervention vs assess) | Time effect (3-month vs baseline) | Time effect (12-month vs baseline) | Interaction (3-month × intervention) | Interaction (12-month × intervention) | |
|---|---|---|---|---|---|---|
| Injured patients (N = 223 at baseline) | ||||||
| Primary outcomes | ||||||
| Days of 5+/4+ men/women last 28-day | 0.98 (0.19) | 0.03 (0.11) | −0.49 (0.10)*** | −0.18 (0.10)† | −0.09 (0.14) | −0.27 (0.14)* |
| Any RAPS4 positive last 3 months | −0.56 (0.66) | 0.24 (0.38) | −1.33 (0.39)*** | −1.95 (0.45)*** | 0.14 (0.55) | −0.01 (0.61) |
| Secondary outcomes | ||||||
| No. of drinking days per week last 28-day | 0.49 (0.10) | 0.06 (0.06) | −0.21 (0.06)*** | 0.05 (0.06) | −0.09 (0.09) | −0.18 (0.09)* |
| Drinks per drinking day last 28-day | 1.59 (0.18) | −0.05 (0.11) | −0.65 (0.10)*** | −0.63 (0.10)*** | 0.03 (0.14) | −0.06 (0.14) |
| Maximum drinks last 28-day | 1.84 (0.21) | −0.03 (0.13) | −0.75 (0.11)*** | −0.67 (0.11)*** | −0.02 (0.16) | −0.07 (0.16) |
| SIPs + 6 count last 3 months | 1.20 (0.18) | 0.00 (0.11) | −0.72 (0.09)*** | −0.57 (0.10)*** | −0.07 (0.14) | −0.14 (0.14) |
| Non-injured patients (N = 395 at baseline) | ||||||
| Primary outcomes | ||||||
| Days of 5+/4+ men/women last 28-day | 0.52 (0.13) | 0.05 (0.08) | −0.38 (0.07)*** | −0.30 (0.07)*** | −0.14 (0.10) | −0.28 (0.10)** |
| Any RAPS4 positive last 3 months | −1.51 (0.55) | 0.14 (0.30) | −0.71 (0.30)* | −1.55 (0.33)*** | −0.70 (0.43) | −0.27 (0.46) |
| Secondary outcomes | ||||||
| No. of drinking days per week last 28-day | 0.35 (0.08) | 0.02 (0.05) | −0.17 (0.04)*** | −0.04 (0.04) | −0.10 (0.06)† | −0.17 (0.06)** |
| Drinks per drinking day last 28-day | 1.18 (0.13) | 0.06 (0.08) | −0.48 (0.08)*** | −0.62 (0.08)*** | −0.29 (0.11)* | −0.26 (0.11)* |
| Maximum drinks last 28-day | 1.34 (0.15) | 0.08 (0.09) | −0.56 (0.09)*** | −0.62 (0.09)*** | −0.35 (0.13)** | −0.35 (0.13)** |
| SIPs + 6 count last 3 months | 0.93 (0.14) | −0.04 (0.08) | −0.50 (0.07)*** | −0.62 (0.07)*** | −0.15 (0.10) | −0.10 (0.10) |
aAll drinking outcome variable were log-transformed, except for any RAPS4 positive.
bSignificant tests not shown for intercepts.
†P < 0.10, *P < 0.05, **P < 0.01, ***P < 0.001.
Table 5.
Random effect model coefficients for change in drinking between baseline and 3- and 12-month follow-up, by drinking prior to the eventa
| Interceptb (assess at baseline) | Group effect at baseline (intervention vs assess) | Time effect (3-month vs baseline) | Time effect (12-month vs baseline) | Interaction (3-month × intervention) | Interaction (12-month × intervention) | |
|---|---|---|---|---|---|---|
| Drinking before event (N = 98 at baseline) | ||||||
| Primary outcomes | ||||||
| Days of 5+/4+ men/women last 28-day | 0.92 (0.29) | 0.27 (0.17) | −0.53 (0.18)** | −0.29 (0.18) | −0.28 (0.25) | −0.78 (0.24)** |
| Any RAPS4 positive last 3 months | −0.54 (1.05) | 0.18 (0.59) | −1.56 (0.67)* | −2.72 (0.78)*** | 0.27 (0.86) | −0.03 (0.94) |
| Secondary outcomes | ||||||
| No. of drinking days per week last 28-day | 0.55 (0.17) | 0.18 (0.11)† | −0.26 (0.11)* | 0.00 (0.11) | −0.16 (0.15) | −0.48 (0.15)*** |
| Drinks per drinking day last 28-day | 1.56 (0.25) | 0.10 (0.16) | −0.54 (0.17)** | −0.63 (0.16)*** | −0.10 (0.23) | −0.44 (0.22)* |
| Maximum drinks last 28-day | 1.83 (0.29) | 0.15 (0.18) | −0.72 (0.19)*** | −0.72 (0.18)*** | −0.16 (0.25) | −0.59 (0.24)* |
| SIPs + 6 count last 3 months | 1.41 (0.30) | 0.19 (0.17) | −0.85 (0.17)*** | −0.82 (0.17)*** | −0.21 (0.23) | −0.40 (0.22)† |
| No drinking before event (N = 521 at baseline) | ||||||
| Primary outcomes | ||||||
| Days of 5+/4+ men/women last 28-day | 0.67 (0.11) | −0.04 (0.07) | −0.41 (0.06)*** | −0.26 (0.06)*** | −0.07 (0.09) | −0.16 (0.08)† |
| Any RAPS4 positive last 3 months | −1.18 (0.46) | 0.07 (0.26) | −0.89 (0.26) *** | −1.60 (0.29)*** | −0.44 (0.37) | −0.09 (0.40) |
| Secondary outcomes | ||||||
| No. of drinking days per week last 28-day | 0.39 (0.06) | −0.01 (0.04) | −0.18 (0.03) *** | −0.01 (0.03) | −0.07 (0.05) | −0.10 (0.05)* |
| Drinks per drinking day last 28-day | 1.34 (0.12) | −0.03 (0.07) | −0.55 (0.07) *** | −0.63 (0.07)*** | −0.17 (0.10)† | −0.13 (0.10) |
| Maximum drinks last 28-day | 1.53 (0.13) | −0.02 (0.08) | −0.63 (0.08) *** | −0.64 (0.08)*** | −0.22 (0.11)* | −0.16 (0.11) |
| SIPs + 6 count last 3 months | 0.95 (0.11) | −0.10 (0.07) | −0.54 (0.06) *** | −0.57 (0.06)*** | −0.08 (0.09) | −0.03 (0.08) |
aAll drinking outcome variable were log-transformed, except for any RAPS4 positive.
bSignificant tests not shown for intercepts.
†P < 0.10, *P < 0.05, **P < 0.01, ***P < 0.001.
Table 6.
Random effect model coefficients for change in drinking between baseline and 3- and 12-month follow-up, by dispositional variablesa
| Interceptb (assess at baseline) | Group effect at baseline (intervention vs assess) | Time effect (3-month vs baseline) | Time effect (12-month vs baseline) | Interaction (3-month × intervention) | Interaction (12-month × intervention) | |
|---|---|---|---|---|---|---|
| Higher risk takingc (N = 205 at baseline) | ||||||
| Primary outcomes | ||||||
| Days of 5+/4+ men/women last 28-day | 0.80 (0.20) | 0.13 (0.12) | −0.46 (0.11)*** | −0.33 (0.11)** | −0.23 (0.16) | −0.35 (0.16)* |
| Any RAPS4 positive last 3 months | −1.09 (0.64) | 0.44 (0.39) | −1.04 (0.37)** | −1.65 (0.41)*** | −0.36 (0.54) | −0.53 (0.58) |
| Secondary outcomes | ||||||
| No. of drinking days per week last 28-day | 0.43 (0.12) | 0.12 (0.07) | −0.18 (0.07)** | −0.03 (0.07) | −0.15 (0.10) | −0.22 (0.10)* |
| Drinks per drinking day last 28-day | 1.53 (0.19) | −0.06 (0.12) | −0.64 (0.11)*** | −0.80 (0.11)*** | −0.03 (0.16) | −0.05 (0.16) |
| Maximum drinks last 28-day | 1.79 (0.22) | −0.01 (0.14) | −0.76 (0.13)*** | −0.83 (0.13)*** | −0.12 (0.18) | −0.16 (0.18) |
| SIPs + 6 count last 3 months | 1.46 (0.20) | 0.09 (0.12) | −0.75 (0.10)*** | −0.88 (0.10)*** | −0.25 (0.15) | −0.22 (0.15) |
| Lower risk taking (N = 414 at baseline) | ||||||
| Primary outcomes | ||||||
| Days of 5+/4+ men/women last 28-day | 0.59 (0.12) | −0.01 (0.07) | −0.42 (0.07)*** | −0.23 (0.06)*** | −0.05 (0.09) | −0.24 (0.09)* |
| Any RAPS4 positive last 3 months | −1.34 (0.55) | 0.01 (0.29) | −0.97 (0.31)** | −1.82 (0.35)*** | −0.32 (0.44) | 0.14 (0.48) |
| Secondary outcomes | ||||||
| No. of drinking days per week last 28-day | 0.35 (0.07) | 0.00 (0.04) | −0.20 (0.04)*** | 0.00 (0.04) | −0.06 (0.05) | −0.15 (0.05)** |
| Drinks per drinking day last 28-day | 1.23 (0.13) | 0.03 (0.08) | −0.52 (0.08)*** | −0.55 (0.07)*** | −0.22 (0.11)* | −0.25 (0.11)* |
| Maximum drinks last 28-day | 1.38 (0.15) | 0.04 (0.09) | −0.60 (0.08)*** | −0.56 (0.08)*** | −0.25 (0.12)* | −0.28 (0.12)* |
| SIPs + 6 count last 3 months | 0.74 (0.12) | −0.06 (0.07) | −0.50 (0.07)*** | −0.46 (0.06)*** | −0.05 (0.09) | −0.06 (0.09) |
aAll drinking outcome variable were log-transformed, except for any RAPS4 positive.
bSignificant tests not shown for intercepts.
cIncludes impulsivity and sensation seeking.
*P < 0.05, **P < 0.01, ***P < 0.001.
The assessed condition was also compared to the screened-only condition to examine potential biases related to assessment reactivity (not shown). No difference was found between the two conditions at baseline, while at 12-month follow-up the direction of differences in the observed effects varied across outcome measures, and, except for RAPS4, none of the comparisons were significant.
DISCUSSION
In this BI study of young adult Mexican-origin ED patients residing in the Texas–Mexico border city of El Paso, 25% of those screened met criteria for at-risk or dependent drinking, which was similar to the proportion screening positive in other BI studies (Longabaugh et al., 2001; Academic ED SBIRT Research Collaborative, 2007; Daeppen et al., 2007; Cherpitel et al., 2010). Both the assessment and intervention conditions showed decreases in all primary and secondary outcomes from baseline to the 12-month follow-up, with the intervention condition showing significantly or marginally significantly lower values on outcome variables except the RAPS4 score. Controlling for gender, age, nativity and baseline drinking values, the intervention condition showed greater improvement than the assessed condition only in maximum drinks on an occasion at 3 months, while at 12 months the intervention condition showed greater improvement in all consumption variables, but not in problem variables (RAPS4 measuring dependence and SIPs + 6 measuring negative consequences of drinking). Unlike those studies which have found positive results for BI in the short-term deteriorating on longer-term follow-up (Nilsen et al., 2008), findings here suggest long-term effects of the intervention, also reported elsewhere (Monti et al., 1999; Longabaugh et al., 2001; Cherpitel et al., 2010).
In subgroup analysis, improvement in outcomes was significantly more evident for non-injured patients, those who reported drinking prior to the event that precipitated the ED visit and those lower on risk taking disposition. We hypothesized that injured patients would demonstrate greater improvement in outcomes over non-injured patients due to the injury event being viewed as a ‘teachable moment’, at which time patients may be more receptive to an intervention (Conigrave et al., 1991; Monti et al., 1999), but findings here did not support this. Drinking prior to the injury or medical event was found to be a significant moderator of effectiveness of the intervention, as hypothesized and found elsewhere (Barnett et al., 2010), presumably due to the increased salience of alcohol's role in the event as a motivator to change drinking behavior. Likewise we hypothesized that those low on risk taking/impulsivity and sensation seeking would also show improved outcomes compared to those higher on these dispositions who may be least susceptible to behavioral change due to perceived lack of vulnerability and differences in information processing (Donovan et al., 1988), and findings here support this hypothesis.
Improved outcomes from baseline to 12 months for both the assessed and intervention condition may be due, in part, to regression to the mean, operant where those recruited based on a given level of criteria may be at a peak for the criteria at the time of recruitment. Likewise, assessment reactivity, where the impact of assessment may be nearly as strong as the impact of the intervention in changing drinking behavior, has been thought to account for improved outcomes for the assessment condition, but little evidence of this was apparent in this study. Comparison between the screened and assessed condition at the 12-month follow-up found the direction of differences in the effects observed varied across outcome measures, and except for RAPS4, none of the comparisons were significant.
Additionally, patients expecting a follow-up contact may have reduced their drinking under both conditions, or may claim to have reduced consumption to meet perceived expectation of the interviewers. This social desirability bias may be especially relevant for this population of Mexican-origin patients among whom there is a strong cultural emphasis on harmony in interpersonal relationships and respect and obedience for authority figures (Marín, 1996; Marín and Marín, 1997).
The present study employed peer educator HPAs, licensed as community health workers, who were able to spend more time with the patient and conduct the intervention in a private area, addressing some of the observed shortcomings of BI in the ED setting (Daeppen et al., 2007), and may account for the long-term effects of BI found here. While the use of promotores has reached widespread success as a low-cost, culturally appropriate prevention model in clinical settings among ethnic populations (Warrick et al., 1992; Williams, 2001; Ramos and Ferreira-Pinto, 2006; Ramos et al., 2006), they have not previously been used to deliver BI for drinking and related problems. It was hypothesized, and substantiated by our findings, that promotores would be particularly effective in delivering BI to Mexican-origin young adults, given their long-established success in other health promotion and prevention activities in the Mexican-origin community. Additionally, ethnic matching between patient and interventionist has been found to be an important factor in efficaciousness of BI (Marín, 1989; Marín et al., 1995; Casas et al., 2002; Comas-Días, 2006; Vasquez, 2007; Field and Caetano, 2010), especially among those less acculturated who may be more distrustful and less comfortable discussing their alcohol use with a stranger (Field and Caetano, 2010).
Limitations
Findings here may be influenced by the low severity of drinking of those recruited into this study. Patients reported drinking on average about 1 day a week, but consuming six drinks per drinking day and over eight drinks on a maximum drinking occasion, reflecting a pattern of heavy episodic drinking characteristic of a fiesta drinking culture typical in this Mexican-origin population. BI directed toward patients in the mild range of drinking severity is less likely to show improvement in drinking outcomes (Bernstein and Bernstein, 2008), and findings based on this drinking style may not be generalizable to other cultures or populations with more frequent heavy drinking patterns.
Also potentially effecting study findings is attrition at follow-up. While no significant differences were observed between those followed and those not followed in the assessed condition, those not followed in the intervention condition were heavier drinkers at baseline. One possible explanation for this is that those with a more serious drinking problem who undergo an intervention may find it more difficult to change their drinking behavior than those with a less severe problem, and therefore less inclined to participate at follow-up, due to the strong cultural emphasis on respect and obedience for authority figures in this ethnic group (Marín, 1996; Marín and Marín, 1997).
Lastly, findings here pertain only to one ED in El Paso, TX, and may not be generalizable to other border settings either in Texas, or in the three other states that border Mexico, or to other more rural border areas.
Despite these limitations, main findings related to both primary and secondary outcomes were similar to those from other BI studies, and intervention may have added benefits above assessment for specific subgroups of patients in the ED, an area that warrants additional study in the ED setting. Data also suggest the efficacy of promotores in delivering BI in this population of young adult Mexican-origin patients in the ED.
FUNDING
This work was supported by a grant from the U.S. National Institute on Alcohol Abuse and Alcoholism (R01 AA018119).
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- Academic ED SBIRT Research Collaborative. (2007) The impact of screening, brief intervention, and referral for treatment on Emergency Department patients’ alcohol use. Ann Emerg Med 50:699–710. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (1994) Diagnostic and Statistical Manual of Mental Disorders (DSM-IV). Washington, DC: American Psychiatric Association. [Google Scholar]
- Barnett NP, Apodaca TR, Magill M et al. (2010) Moderators and mediators of two brief interventions for alcohol in the emergency department. Addiction 105:452–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein E, Bernstein J (2008) Effectiveness of alcohol screening and brief motivational intervention in the emergency department setting. Ann Emerg Med 51:751–4. [DOI] [PubMed] [Google Scholar]
- Bernstein E, Bernstein J, Levenson S (1997) Project ASSERT: an ED-based intervention to increase access to primary care, preventive services, and the substance abuse treatment system. Ann Emerg Med 30:181–9. [DOI] [PubMed] [Google Scholar]
- Bernstein E, Bernstein J, Feldman J et al. (2007) An evidence-based alcohol screening, brief intervention and referral to treatment (SBIRT) curriculum for emergency department (ED) providers improves skills and utilization. Subst Abus 28:79–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein E, Topp D, Shaw E et al. (2009) A preliminary report of knowledge translation: lessons from taking screening and brief intervention techniques (SBI) from the research setting into regional systems of care. Acad Emerg Med 16:1225–33. [DOI] [PubMed] [Google Scholar]
- Breslin RW. (1986) The wording and translation of research instruments. In Lonner WJ, Berry JW (eds). Field Methods in Cross-Cultural Research, Vol. 8 Newbury Park, CA: SAGE Publications, 137–65. [Google Scholar]
- Casas JM, Vasquez MJT, Ruiz de Esparza CA (2002) Counseling the Latina/o: a guiding framework for a diverse population. In Pederson PB, Draguns JG, Lonner WJ, Trimble JE (eds). Counseling Across Cultures. Thousand Oaks, CA: SAGE Publications, Inc., 133–60. [Google Scholar]
- Cherpitel CJ. (1993) Alcohol, injury and risk taking behavior: data from a national sample. Alcohol Clin Exp Res 17:762–6. [DOI] [PubMed] [Google Scholar]
- Cherpitel CJ. (2000) A brief screening instrument for problem drinking in the emergency room: the RAPS4. J Stud Alcohol 61:447–9. [DOI] [PubMed] [Google Scholar]
- Cherpitel CJ, Korcha R, Moskalewicz J et al. (2010) Screening, brief intervention and referral to treatment (SBIRT): 12-month outcomes of a randomized controlled clinical trial in a Polish emergency department. Alcohol Clin Exp Res 34:1922–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comas-Días L. (2006) Cultural variation in the therapeutic relationship. In Goodheart CD, Kazdin AE, Sternberg RJS (eds). Evidence-Based Psychotherapy: Where Practice and Research Meet. Washington, DC: American Psychological Association, 81–105. [Google Scholar]
- Conigrave KM, Burns FH, Reznik RB et al. (1991) Problem drinking in emergency department patients: the scope for early intervention. Med J Aust 154:801–5. [DOI] [PubMed] [Google Scholar]
- D'Onofrio GD, Fiellin DA, Pantalon MV et al. (2013) A brief intervention reduces hazardous and harmful drinking in emergency department patients. Ann Emerg Med 60:181–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daeppen J-B, Gaume J, Bady P et al. (2007) Brief alcohol intervention and alcohol assessment do not influence alcohol use in injured patients treated in the emergency department: a randomized controlled clinical trial. Addiction 102:1224–33. [DOI] [PubMed] [Google Scholar]
- de Cosío FG, Boadella A (1999) Demographic factors affecting the U.S.–Mexico border health status. In Loustaunau MO, Sánchez-Bane M (eds). Life, Death, and In-between on the U.S.–Mexico Border. Así es la vida. Wesport, CT: Bergin & Garvey, 1–22. [Google Scholar]
- Donovan DM, Umlauf RL, Salzberg PM (1988) Derivation of personality subtypes among high-risk drivers. Alcohol Drugs Driving 4:233–44. [Google Scholar]
- Eysenck SBG, Eysenck HJ (1977) The place of impulsiveness in a dimensional system of personality description. Br J Soc Clin Psychol 16:57–68. [DOI] [PubMed] [Google Scholar]
- Field CA, Caetano R (2010) The role of ethnic matching between patient and provider on the effectiveness of brief alcohol interventions with Hispanics. Alcohol Clin Exp Res 34:262–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson DN. (1974) JPI Jackson Personality Inventory Manual. Goshen, NY: Psychologists Press. [Google Scholar]
- Lawrence PA. (1998) Psychological risk factors and substance abuse among young adults. A comparison of non-Hispanic Whites and Mexican Americans. In Power JG, Byrd T (eds). U.S.–Mexico Border Health. Issues for Regional and Migrant Populations. Thousand Oaks, CA: SAGE Publications, 32–51. [Google Scholar]
- Longabaugh R, Woolard RF, Nirenberg TD et al. (2001) Evaluating the effects of a brief motivational intervention for injured drinkers in the emergency department. J Stud Alcohol 62:806–16. [DOI] [PubMed] [Google Scholar]
- Marín G. (1989) AIDS prevention among Hispanics: needs, risk behaviors, and cultural values. Public Health Rep 104:411–5. [PMC free article] [PubMed] [Google Scholar]
- Marín G. (1996) Expectancies for drinking and excessive drinking among Mexican Americans and non-Hispanic whites. Addict Behav 21:491–507. [DOI] [PubMed] [Google Scholar]
- Marín G, Marín MA (1997) Differential perception of drinkers of alcoholic beverages by Mexican-Americans and non-Hispanic whites. Subst Use Misuse 32:1369–84. [DOI] [PubMed] [Google Scholar]
- Marín G, Burhansstipanov L, Connell CM et al. (1995) A research agenda for health education among underserved populations. Health Educ Q 22:346–63. [DOI] [PubMed] [Google Scholar]
- Miller WR, Tonigan JS, Longabaugh R (1995) The Drinker Inventory of Consequences (DrInC): An Instrument for Assessing Adverse Consequences of Alcohol Abuse [NIH Pub. No. 95–3911]. Rockville, MD: National Institute on Alcohol Abuse and Alcoholism, National Institutes of Health. [Google Scholar]
- Monti PM, Colby SM, Barnett NP et al. (1999) Brief intervention for harm reduction with alcohol-positive older adolescents in a hospital emergency department. J Consult Clin Psychol 67:989–94. [DOI] [PubMed] [Google Scholar]
- Nilsen P, Baird J, Mello MJ et al. (2008) A systematic review of emergency care brief alcohol interventions for injury patients. J Subst Abuse Treat 35:184–201. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, DiClemente CC (1992) Stages of change in the modification of problem behaviors. Prog Behav Modif 28:183–218. [PubMed] [Google Scholar]
- Ramos RL, Ferreira-Pinto JB (2006) A transcultural case management model for HIV/AIDS care and prevention. J HIV AIDS Soc Serv 5:139–57. [Google Scholar]
- Ramos RL, Hernandez A, Ferreira-Pinto JB et al. (2006) Promovisión: designing a capacity-building program to strengthen and expand the role of promotores in HIV prevention. Health Promot Pract 7:444–9. [DOI] [PubMed] [Google Scholar]
- Rodríguez-Martos Dauer A, Santamariña Rubio E, Martínez Gómez X et al. (2003) Identificación precoz e intervención breve en lesionades de tráfico con presencia de alcohol: primeros resultados [Early identification and brief intervention in alcohol-related traffic casualties: preliminary results]. Adicciones 15:191–202. [Google Scholar]
- Schulz KF, Altman DG, Moher D (2010) CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. Ann Intern Med 152:726–32. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB (1992) Timeline Follow-Back: a technique for assessing self-reported alcohol consumption. In Litten RZ, Allen JP (eds). Measuring Alcohol Consumption: Psychosocial and Biological Methods. Totowa, NJ: Humana Press, 41–72. [Google Scholar]
- United States Census Bureau. (2012) American Community Survey. Archived by WebCite® at http://www.webcitation.org/69ifuxgD2 (6 August 2012, date last accessed), Washington, DC. [Google Scholar]
- Vasquez MJT. (2007) Cultural differences and the therapeutic alliance: an evidence-based analysis. Am Psychol 62:878–85. [DOI] [PubMed] [Google Scholar]
- Wallisch LS. (1998) 1996 Survey of Substance Use on the Texas–Mexico Border and in Colonias. Full Report. Austin, TX: Texas Commission on Alcohol and Drug Abuse. [Google Scholar]
- Wallisch LS, Spence RT (2006) Alcohol and drug use, abuse, and dependence in urban areas and colonias of the Texas–Mexico border. Hisp J Behav Sci 28:286–307. [Google Scholar]
- Warrick LH, Wood AH, Meister JS et al. (1992) Evaluation of peer health worker prenatal outreach program for Hispanic farm worker families. J Community Health 17:13–26. [DOI] [PubMed] [Google Scholar]
- Williams DM. (2001) La promotora: linking disenfranchised residents along the border to the U.S. health care system. Health Aff (Millwood) 20:212–8. [DOI] [PubMed] [Google Scholar]
- Zuckerman M. (1979) Sensation Seeking: Beyond the Optimal Level of Arousal. Hillsdale, NJ: Lawrence Erlbaum Associates. [Google Scholar]