Primary care providers refer patients to specialists when they need advice on the diagnosis or management of a particular condition; when a technical procedure, surgery, or specialized psychiatric intervention is required; or when additional expertise is needed for care of a complex chronic disease.1,2 In 2007, 3 million Canadians reported seeing a non–family physician specialist for a new condition in the preceding year.3
An effective referral-consultation process requires seamless transfer of complete, relevant information between providers. Inaccurate, incomplete, or delayed transfer of information might result in delayed access to care, duplicate testing, polypharmacy, inappropriate medication use, erosion of trust in the medical system, and increased costs.4,5 Referring physicians and consultants want medication lists and management plans to be included in communications between providers, yet there continues to be a gap in what is expected and what is provided.6 The potential for drug interactions, redundancies, or use of previously ineffective or not tolerated medications is substantial when there are failures in communication. Delays in initiating effective medications might occur when there is uncertainty about who is responsible for implementing and monitoring new therapies. Opportunity exists for innovative models to involve pharmacists in the referral-consultation process.
Assessing the gaps
According to a systematic review by Berta et al, the ideal referral note not only contains a list of current medications but also those relevant medications that have been previously tried and discontinued.7 Consultation letters should contain information about any therapy proposed or initiated, including all medications and their intended duration.8 These recommendations were incorporated into the joint College of Family Physicians of Canada and Royal College of Physicians and Surgeons of Canada statement.6
We completed a retrospective chart audit (n = 70) in a tertiary endocrinology clinic that provides more than 10 000 physician visits per year, from October 2013 to December 2013, to assess the accuracy and clarity of medication information in referral and consultation letters. Approval was obtained from the Ottawa Health Science Network Research Ethics Board. Medication lists were considered complete if the medication name, dose, and frequency were included. Clarity of the communication of medication changes made by the specialist was assessed: a primary care physician and a specialist assigned each case where a medication change was mentioned in the consultation letter as one of “medication change implemented by specialist,” “medication change recommended by specialist,” or “unclear.” Any case on which the first and second reader disagreed was considered unclear. We identified that 44% (31 of 70) of referral documents contained medication lists, of which 71% (22 of 31) were complete. Of the 96% (67 of 70) of consultation notes that contained a medication list, 48% (32 of 67) were complete. In the 46% (32 of 70) of consultation notes that contained a medication change, it was unclear 38% (12 of 32) of the time whether the change had been implemented or was only a recommendation. Median time between referral and consultation was 105 days. The long wait between referral and specialist visit might imply that the medication information sent is no longer accurate and suggests a potential need for updated medication profiles before the appointment.
Our findings are consistent with previous studies on completeness of medication lists in referral letters9,10 and consultation letters9,11 that show similar rates to our study of 33% to 38% and 75% to 80%, respectively. In an audit of 125 cases across 10 different medical specialties involving therapy as a key issue, 66% recommended changes in medication, of which only 55% indicated reasons for the change.12 One Australian study of 300 referral letters from primary care to tertiary ambulatory care for patients with type 2 diabetes identified that 80% of referral letters contained a medication discrepancy, with omission of a current medication being the most common inaccuracy. In this study the median time from the referral to the specialist visit was only 4 weeks.13
Opportunities to improve
Medication reconciliation is a systematic review of medications to ensure adequate communication at transition points, including transition to another service or provider, and is a recognized Canadian accreditation standard for hospitals.14 There are currently no programs or specific requirements in place to review the accuracy and completeness of medication information in the transitions between primary and specialty care.
Pharmacists are ideally situated to ensure continuity of medication information in the outpatient setting. In one study, a single consultant implemented sending copies of discharge summaries to practice-based pharmacists and demonstrated that patients were more likely to get the treatment recommended at discharge (83% vs 51% of patients) after the implementation. The study also demonstrated high satisfaction among the primary care physicians and pharmacists.15 The incorporation of practice-based pharmacists into the primary care of patients with an identified need for medication optimization has been shown to improve medication nonadherence (86% vs 40%), untreated indications (73% vs 11%), suboptimal medication choices (60% vs 6%), and cost-ineffective drug therapies (72% vs 7%) for patients in 2 community-based primary care internal medicine practices in the United States.16
We believe that there is an opportunity to link pharmacists into the communication channels between primary care physicians and specialists. Current models of care include integration of pharmacists into clinical teams (there are now 111 family health teams in Ontario with pharmacists), as well as enhanced, reimbursable clinical services provided by community pharmacists.17,18
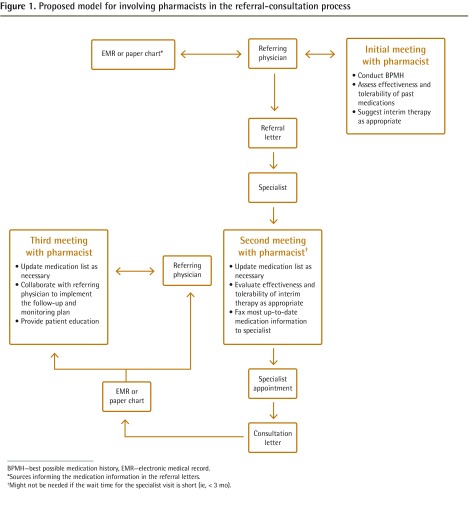
In the proposed model, both community pharmacists and those working within family physician practices could intervene up to 3 times in the referral process (Figure 1). The initial meeting would take place before the referral letter is sent to the consultant. The goal of this meeting between the patient and pharmacist is to collaborate in generating an accurate medication history, including past medications tried and their effectiveness and tolerability, before the specialist appointment. The outcome is to provide the specialist with a more complete picture to better guide optimal therapy. A secondary outcome of this appointment might be to aid the referring physician in determining which medication can be tried in the interim, particularly if a long wait time is anticipated. In Canada, the median wait time from primary care referral to specialist appointment was 8.6 weeks in 2013.19 If there is a substantial delay before the specialist appointment, a second meeting is then scheduled 1 to 2 weeks before the appointment date. The goal of this meeting is to reconcile the patient’s medications to provide the most up-to-date medication history and list possible. The need for this second appointment would be determined based on the clinical status of the patient and the length of time between the initial medication reconciliation and specialist consultation. The third appointment is immediately after the specialist appointment. The goal of this meeting is to reconcile any newly added or discontinued medication, to identify medication recommendations that were not initiated, and to provide the appropriate education and monitoring plan for changes made. The pharmacist would communicate the most up-to-date care plan back to the referring physician and specialist after each visit.
Figure 1..
Proposed model for involving pharmacists in the referral-consultation process
BPMH—best possible medication history, EMR—electronic medical record.
*Sources informing the medication information in the referral letters.
†Might not be needed if the wait time for the specialist visit is short (ie, < 3 mo).
Is this model feasible?
As with any new quality improvement or change in health care delivery, our model would need to be tested in a proof-of-concept trial to determine feasibility. This service model does have some limitations, as it is not designed for urgent referrals. As part of the proof-of-concept trial it would be important to determine whether the increased number of visits required is acceptable to patients, whether the need for clear communication between providers to prevent errors or misunderstandings can be achieved, and whether reimbursement models are satisfactory for pharmacists to provide the service. A systematic review of pharmacy clinical services by Houle et al18 identified several barriers to new services, including cost-effectiveness, time constraints, lack of patient and physician buy-in, cumbersome billing processes, and lack of privacy. Thus, the model we have proposed would need to be vetted and pilot tested with community pharmacists, pharmacists working within primary care teams, primary care providers, and specialists to assess its feasibility and determine structures and processes that would support its successful implementation. In recent years, a number of changes have occurred in community pharmacy practice that facilitate provision of this type of clinical service. These include regulation of pharmacy technicians, expanded scope of pharmacist practice, and new reimbursement models. The latter provides reimbursement for pharmacists to spend time with patients to review and provide up-to-date medication lists, and to make recommendations to prescribers if drug-related problems are identified. All provinces in Canada reimburse community pharmacists for some form of comprehensive medication review or assessment.20 In addition to yearly medication reviews, in some provinces, such as Ontario and Alberta, pharmacists can be reimbursed for follow-up medication review assessments if the patient is referred by another health care professional (eg, a physician).20 This might help contribute to the sustainability of this model. However, since reimbursement models and requirements differ across provinces, clinicians are encouraged to refer to their respective provincial reimbursement guidelines for pharmacist clinical services.
Conclusion
Medication information is present in referrals less than half of the time. When medication lists are present in referrals and consultation notes, information is frequently incomplete. Combined with the delay between referral and consultation, as well as lack of clarity regarding medication changes, this is a considerable concern for patient safety. Physicians might not be the best suited for providing detailed medication histories and reconciliation during this process. The pharmacist has not been traditionally involved in the referral process from primary to specialty care in the outpatient setting. By systematically including pharmacists (working within the primary care team or in the community pharmacy) in the referral-consultation process, they will ensure prescribers are working with up-to-date and accurate information to facilitate the best decision making possible. This will also help identify if patients experience problems or successes with medication changes made by consultants.
Acknowledgments
Mr Tsang completed the chart audit and contributed to preparing the article while on a co-op placement at the Bruyère Research Institute at the University of Ottawa in Ontario.
Footnotes
This article has been peer reviewed.
La traduction en français de cet article se trouve à www.cfp.ca dans la table des matières du numéro de février 2016 à la page e52.
Competing interests
None declared
The opinions expressed in commentaries are those of the authors. Publication does not imply endorsement by the College of Family Physicians of Canada.
References
- 1.Forrest CB. A typology of specialists’ clinical roles. Arch Intern Med. 2009;169(11):1062–8. doi: 10.1001/archinternmed.2009.114. [DOI] [PubMed] [Google Scholar]
- 2.Piterman L, Koritsas S. Part II. General practitioner-specialist referral process. Intern Med J. 2005;35(8):491–6. doi: 10.1111/j.1445-5994.2005.00860.x. [DOI] [PubMed] [Google Scholar]
- 3.Carriere G, Sanmartin C. Waiting time for medical specialist consultations in Canada, 2007. Vancouver, BC: Health Analysis Division at Statistics Canada; 2010. [PubMed] [Google Scholar]
- 4.Lin CY. Improving care coordination in the specialty referral process between primary and specialty care. N C Med J. 2012;73(1):61–2. [PubMed] [Google Scholar]
- 5.O’Malley AS, Reschovsky JD. Referral and consultation communication between primary care and specialist physicians: finding common ground. Arch Intern Med. 2011;171(1):56–65. doi: 10.1001/archinternmed.2010.480. [DOI] [PubMed] [Google Scholar]
- 6.College of Family Physicians of Canada. Royal College of Physicians and Surgeons of Canada . Guide to enhancing referrals and consultations between physicians. Mississauga, ON: College of Family Physicians of Canada; 2009. Available from: www.cfpc.ca/uploadedFiles/Resources/Resource_Items/Health_Professionals/Guide%20to%20enhancing%20referrals%20and%20consultations%20between%20physicians.pdf. Accessed 2015 Dec 18. [Google Scholar]
- 7.Berta W, Barnsley J, Bloom J, Cockerill R, Davis D, Jaakkimainen L, et al. Enhancing continuity of information. Essential components of a referral document. Can Fam Physician. 2008;54:1432–3.e1–6. Available from: www.cfp.ca/content/54/10/1432.full.pdf+html. Accessed 2015 Dec 18. [PMC free article] [PubMed] [Google Scholar]
- 8.Berta W, Barnsley J, Bloom J, Cockerill R, Davis D, Jaakkimainen L, et al. Enhancing continuity of information. Essential components of consultation reports. Can Fam Physician. 2009;55:624–5.e1–5. Available from: www.cfp.ca/content/55/6/624.full.pdf+html. Accessed 2015 Dec 18. [PMC free article] [PubMed] [Google Scholar]
- 9.Stille CJ, Mazor KM, Meterko V, Wasserman RC. Development and validation of a tool to improve paediatric referral/consultation communication. BMJ Qual Saf. 2011;20(8):692–7. doi: 10.1136/bmjqs.2010.045781. [DOI] [PubMed] [Google Scholar]
- 10.Dupont C. Quality of referral letters. Lancet. 2002;359(9318):1701. doi: 10.1016/S0140-6736(02)08583-5. [DOI] [PubMed] [Google Scholar]
- 11.Fox AT, Palmer RD, Crossley JG, Sekaran D, Trewavas ES, Davies HA. Improving the quality of outpatient clinic letters using the Sheffield Assessment Instrument for Letters (SAIL) Med Educ. 2004;38(8):852–8. doi: 10.1111/j.1365-2929.2004.01898.x. [DOI] [PubMed] [Google Scholar]
- 12.Scott IA, Mitchell CA, Logan E. Audit of consultant physicians’ reply letters for referrals to clinics in a tertiary teaching hospital. Intern Med J. 2004;34(1–2):31–7. doi: 10.1111/j.1444-0903.2004.00424.x. [DOI] [PubMed] [Google Scholar]
- 13.Azzi M, Constantino M, Pont L, Mcgill M, Twigg S, Krass I. Medication safety: an audit of medication discrepancies in transferring type 2 diabetes mellitus (T2DM) patients from Australian primary care to tertiary ambulatory care. Int J Q Health Care. 2014;26(4):397–403. doi: 10.1093/intqhc/mzu051. [DOI] [PubMed] [Google Scholar]
- 14.Accreditation Canada, Canadian Institute for Health Information. Canadian Patient Safety Institute. Institute for Safe Medication Practices Canada . Medication reconciliation in Canada: raising the bar—progress to date and the course ahead. Ottawa, ON: Accreditation Canada; 2012. Available from: www.accreditation.ca/sites/default/files/med-rec-en.pdf. Accessed 2015 Dec 18. [Google Scholar]
- 15.Gray S, Urwin M, Woolfrey S, Harrington B, Cox J. Copying hospital discharge summaries to practice pharmacists: does this help implement treatment plans? Qual Prim Care. 2008;16(5):327–34. [PubMed] [Google Scholar]
- 16.Altavela JL, Jones MK, Ritter M. A prospective trial of a clinical pharmacy intervention in a primary care practice in a capitated payment system. J Manag Care Pharm. 2008;14(9):831–43. doi: 10.18553/jmcp.2008.14.9.831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jorgenson D, Dalton D, Farrell B, Tsuyuki RT, Dolovich L. Guidelines for pharmacists integrating into primary care teams. Can Pharm J (Ott) 2013;146(6):342–52. doi: 10.1177/1715163513504528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Houle SK, Grindrod KA, Chatterley T, Tsuyuki RT. Paying pharmacists for patient care: a systematic review of remunerated pharmacy clinical care services. Can Pharm J (Ott) 2014;147(4):209–32. doi: 10.1177/1715163514536678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barua B, Esmail N. Waiting your turn: wait times for health care in Canada. Vancouver, BC: The Fraser Institute; 2013. [Google Scholar]
- 20.Pammett R, Jorgenson D. Eligibility requirements for community pharmacy medication review services in Canada. Can Pharm J (Ott) 2014;147(1):20–4. doi: 10.1177/1715163513514006. [DOI] [PMC free article] [PubMed] [Google Scholar]