Abstract
The U.S. criminal justice system refers more people to substance abuse treatment than any other system. Low treatment completion rates and high relapse rates among addicted offenders highlight the need for better substance use disorder treatment and recovery tools. Mobile health applications (apps) may fill that need by providing continuous support. In this pilot test, 30 participants in a Massachusetts drug court program used A-CHESS, a mobile app for recovery support and relapse prevention, over a four-month period. Over the course of the study period, participants opened A-CHESS on average of 62% of the days that they had the app. Social networking tools were the most utilized services. The study results suggest that drug court participants will make regular use of a recovery support app.
This pilot study sought to find out if addicted offenders in a drug court program would use a mobile application to support and manage their recovery.
Keywords: mobile health, drug court, substance use disorder, substance abuse, social networks
Introduction
Drug courts and treatment of substance use disorders
Substance use disorders (SUDs) are often chronic brain diseases characterized by cycles of relapse and remission.1 While medications are available to alleviate symptoms, such as craving, treatment usually includes counseling to facilitate behavior change.2 These treatments, like those for other chronic diseases requiring behavior change, are only moderately effective, with ~50% of patients relapsing within a year of ending treatment.3
When confronted with alcohol or drug use stimuli, either environmental or internally induced, a person recovering from an SUD must initiate a response to resist relapse. This response requires (1) cognitive override of cue-induced habitual response, (2) active engagement of newly learned, little-used skills, and/or (3) reaching out to newly established social supports at a vulnerable moment. Many people recovering from an SUD are unable to identify the trigger, use newly acquired skills to manage the trigger, or reach out to people they may not know well.4 In the United States, the criminal justice system refers more people for SUD treatment than any other referral source, making up 37% of treatment referrals.5 A growing number of addicted offenders receive treatment through drug courts. As of 2012, there were 2,734 drug courts,6 most of them being adult drug treatment courts, serving 136,000 people7 per year. Drug court participants experience greater scrutiny than the participants in other treatment populations. Key factors cited in the effectiveness of drug courts include SUD treatment along with random drug testing, unplanned home or work visits by case managers or probation officers, and frequent contact with the judge.8 Offenders with SUDs may show high motivation and ability to maintain sobriety in counseling sessions or when appearing before a judge. However, returning to settings that provide alcohol or drug use cues or create stress can reduce that motivation.9 Relapse is expected regardless of treatment modality.10
Using health information technology for SUD recovery
Health information technology is a vehicle for improving health outcomes through patient-centered communication mechanisms.11 Health-related smartphone applications (apps) have become ubiquitous in a short time.12 The most popular apps offer features, such as behavior tracking, social support, goal setting, and access to suggestions on improving performance, which may be effective for addressing SUDs.13,14 However, few apps offer all features or have a theoretical basis and clinical trial-based evidence for the features they include.15,16
SUD counseling generally occurs in an office setting separate from the daily environment that might precipitate relapse. Mobile phones offer an opportunity to support desired behavior change as never before, taking counseling out of the office and into everyday activities. Mobile apps have been proposed to reinforce skills learned in treatment, provide immediate access to social or professional support, and increase motivation.17–19 These may also help the user by tracking moods, behaviors, and risk factors, such as location, or protective factors, such as self-help group attendance.
A-CHESS
A-CHESS20,21 is a smartphone app (Fig. 1) developed specifically to help people with SUDs achieve and maintain recovery. To our knowledge, it is the only mobile app designed to address SUDs that has been demonstrated as effective in a randomized clinical trial so far.22 Self-determination theory (SDT)23 provided the basis for creating a suite of tools for interrupting the substance use relapse process as described by Marlatt and George.24 SDT is a theory of motivation to act or change. A-CHESS tools are designed to address the three conditions that SDT posits to foster positive behavior change: autonomous motivation [AM], competence in disease management (coping competence [CC]), and relatedness (RE) via social support. The tools are offered as needed to either maintain a drug-free lifestyle or interrupt the relapse process and prevent further harm.
Figure 1.
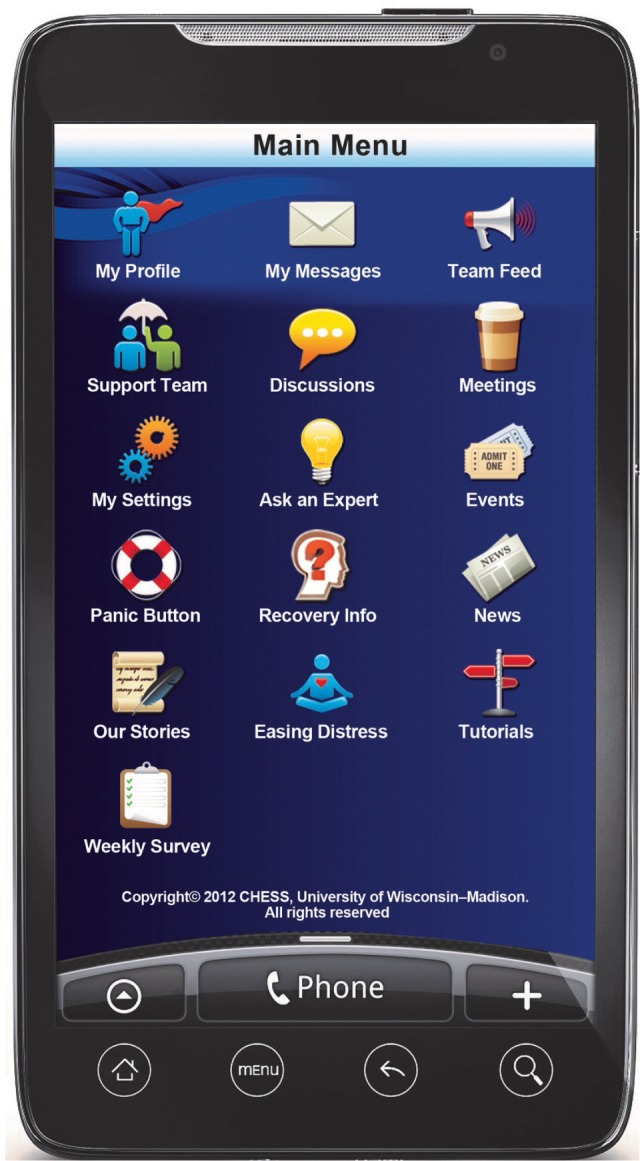
A-CHESS mobile app user interface.
A-CHESS tools include information services, such as recovery information, a self-help meetings list, news about substance use and recovery, activities such as games, guided relaxation recordings and podcasts about recovery, interactive communication, such as messaging and discussion boards, and assessment and feedback tools, such as the high-risk locator and the weekly survey based on the brief addiction monitor.25 Additionally, study participants received two instant messages per day: a “thought for the day,” which was designed to be motivational, and another that was designed to elicit use of the mobile app. This message asked the participant whether they could get through the day without using and directed them to the app or professional support in the event of a negative response.
Each tool within the app is designed to enhance motivation (thought for the day and feedback from survey and risk locator), provide skills or remind participants of skills they have learned in treatment (stories, recovery info, ask an expert, and news) or use skills (meetings, games, and easing distress) to increase competence, and quickly access social support and further develop RE within an online recovering community (my messages, discussions, and support team) based on the constructs of SDT. The version of the app used in this study was modified slightly from the version used in the clinical trial26 by adding more information on drug abuse in the recovery information and newsfeed sections.
A-CHESS has been demonstrated to be effective at decreasing the number of risky drinking days for people who have been recently discharged from residential treatment for an alcohol use disorder.26,27 It is under study with additional populations, including pregnant and postpartum women, veterans, people who are deaf or hard of hearing, and people identified in primary care settings as being in need of SUD treatment. However, studies on A-CHESS results in these populations have not yet been published. No other mobile phone app has been proven effective for addressing SUDs in a randomized clinical trial, though others have had promising pilot outcomes addressing both alcohol22,28 and tobacco use.29,30
Research Question
Will drug court participants, already closely monitored, use a tool that requires them to disclose information about their activities and feelings and to communicate with other drug court participants outside of the court and treatment settings?
A study of the Therapeutic Education System showed that a computerized substance abuse intervention could be implemented successfully in a prison population, which fill a significant treatment gap.31 Similarly, mobile technology may enhance both critical components of drug court – treatment and monitoring – if participants are willing to use it.
While theoretically a smartphone app tackles the problem of giving people with SUDs the health communication tools they need to change their behavior, will people who are already under scrutiny, who already have many additional supports, use a smartphone app and find it useful? Or, will it be perceived as an added burden or simply another mechanism for court monitoring? This pilot study sought to answer these questions by testing how frequently participants used the app and which features they elected to use.
Methods
Recruitment and site information
The pilot site was a postadjudication outpatient drug court program in Massachusetts. A special court docket for drug-using offenders provides comprehensive supervision, drug testing, treatment services, and immediate sanctions and incentives. The target population for treatment was nonviolent adult drug offenders who resided within the court’s jurisdiction, who had been assessed as having an alcohol and/or other drug problem, and who had no record of violent offense. All participants were referred through the court and could be identified by the district attorney, probation department, police department, or defense attorney.
A private, nonprofit clinic oversees the clinical aspects of the drug court program, providing participants with individual, group, and family counseling. The same agency also provides comprehensive case management services to support the participants’ recovery from SUDs. The clinic’s drug court treatment program includes four phases of treatment with declining levels of supervision and support over a 52-week period.
Thirty participants were recruited for the four-month pilot. Participants had to be at least 18 years of age and consent to monitoring of their A-CHESS usage. Participants were offered smartphones with the app preloaded and an unlimited data plan for four months of the study. Participants were recruited by the drug court case managers, and all the drug court participants were invited to take part in the pilot. Only one person refused participation as he was leaving treatment early in the study period. New drug court members were invited to participate in the study when they were admitted to treatment. Twenty-five participants began the study at initiation and five participants were added during the study. The entire drug court population was invited to participate to avoid creating tension between those who obtained study phones and the rest of the population. The phones provided by the study were generally better phones with better service plans than the phones the participants already owned. Participants were offered $30 for completing an exit interview at the close of the study. This interview collected information on their perceptions of the mobile app and how they would improve it to better suit their needs.
Most of the participants were male (87%) and most were white (73%) non-Hispanic, with 10% black/African-American, 10% American Indian, and 7% white of Hispanic origin. It was a young population, with 52% participants in the 18–24 year-age range, 24% participants in the 25–34 year-age range, and 24% participants were of age 35 years or older. Participants received standard treatment plus a smart-phone with access to the A-CHESS system for a maximum of 121 days. During the initial recruitment and training session, participants entered personal information in the smartphone to improve the functioning of the app. They also entered the contact information of people in their support network, along with information on drug-free events and activities, important drug use triggers, and helpful interventions for dealing with those triggers. Participants created code names as instructed, to protect everyone’s privacy if the phones were lost or stolen, but because it was a small cohesive group, participants knew each other’s code names. Participants were also aware that staff, including case managers, probation officers, and the judge, would have access to the mobile app and any interaction that occurred within it. In addition, participants learned how to use the A-CHESS services, about the theory behind A-CHESS, and how it might help prevent relapse.
Nearly half (12) of the participants continued to carry the personal cell phones that they had used before receiving the study phones.
Data collection and analysis
A web server gathered data on each participant’s use of A-CHESS. The server tracked the date and time the participant logged in, the A-CHESS services selected, length of time the service was open, the number of pages viewed, and whether the participant sent or received messages. Overall and weekly A-CHESS use was analyzed by different types of services. (Data used for this analysis do not include the days participants received the phone and training on how to use it).
Social network analysis can help in describing how a group functions. Using data from the app, we could analyze who communicated with whom and how often. Communications between participants in the discussion board were used to create a numerical description of the network from identifying the sender, responders, and number of posts. The social network analysis conducted herein used NodeXL (V1.0.1.245) to calculate traditional social network measures, such as centrality (three types: closeness, betweenness, and eigenvector) and density of networks. These measures were used to draw diagrams of the network that highlight who is most central (eg, necessary to the network’s ongoing communication, either by sending or responding to communications), frequency of communications and how dense (eg, how many links or separate communications to different people each member has on average). For example, one person may initiate a discussion or a number of discussions. Others respond to the post. The network diagram graphically displays who most often initiates discussions and who responds to those initiated discussions. Graphs of two networks were drawn by using the force-directed Harel–Koren fast multiscale layout.32 To distinguish the influence of program staff and the research team, two separate network diagrams were prepared: first, a network that included participants and staff, and second, a network of participants only.
The study and all data collection and analysis were approved by the University of Wisconsin–Madison Social Sciences Institutional Review Board. Participant data were protected by a certificate of confidentiality. Participants signed written consent agreements. This study complied with the principles of the Declaration of Helsinki and was approved by the University of Wisconsin, Madison Education and Social Sciences Institutional Review Board.
Results
Participant use of A-CHESS
Participants’ length of time participating in the study varied. The longest possible period of time in the study was 121 days; the shortest period of time in the study was 4 days. The average amount of time in the study was 95 days. By eliminating the one person who was on study for only four days and was an outlier, the average time on study increases to 98 days. The average percentage of days using A-CHESS (ie, the number of days each individual used A-CHESS divided by the number of days that individual was in the study) was 62%, with a range of 23%–98%. All data analyzed exclude the first day that the participant received the phone to eliminate upward bias created by heavy use during training. Of the people who used the app on <50% of the days they had it, three individuals discontinued all use early and three individuals continued to use it at a low level through the entire study period (Fig. 2).
Figure 2.
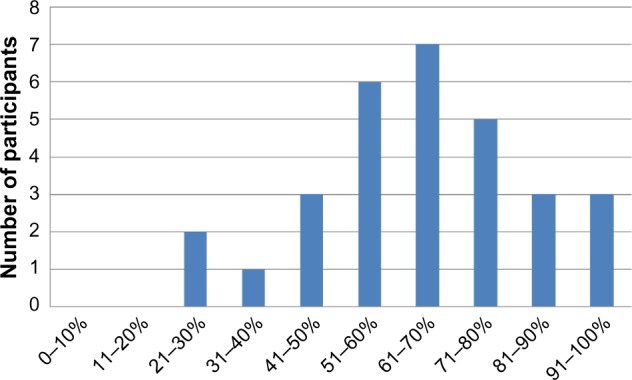
Percentage of days in which participants used A-CHESS.
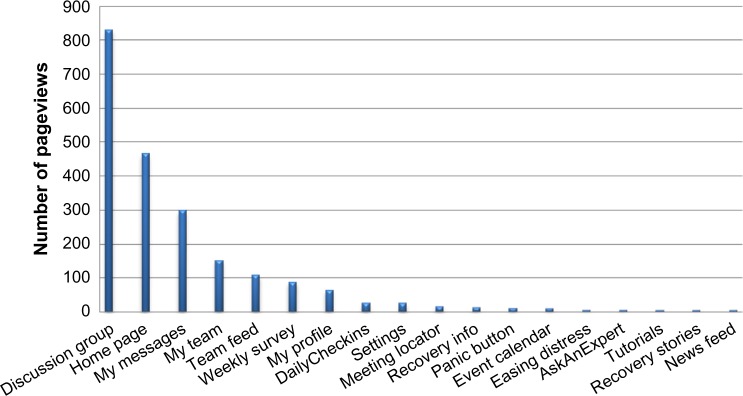
As shown in Figure 3, the top four services used were those designed to enhance social support. Messaging via group discussions was the most used service. The home page or landing page indicates the number of times A-CHESS was used in general. Multiple returns to discussions within one A-CHESS session explain why the Discussions service ranks higher than Home.
Figure 3.
Average number of times participants who used each service used it over the total study period.
A-CHESS services are based on three elements of the SDT theory: those that enhance CC, those that increase RE, and those that improve AM. All participants used the RE tools. By the end of the pilot, 46% of participants were still using the RE tools. The other two types of tools were used at a slightly lower initial rate. Use declined at a linear pace for all three types of tools through the course of the study period (Fig. 4).
Figure 4.
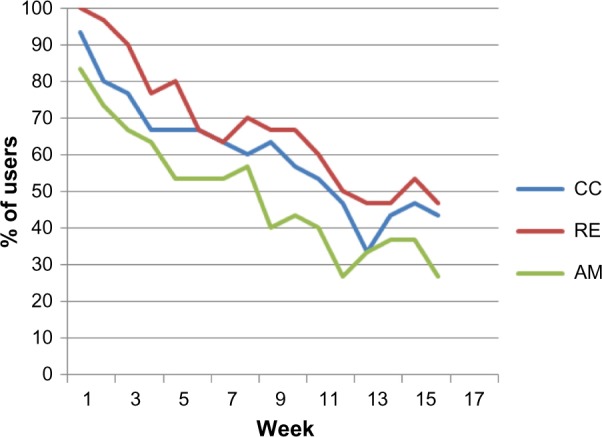
Frequency of use over a study period.
Social network analysis
Because social networking tools were the most utilized services, we further examined how the communication tools were used, ie, who was communicating with whom and in what frequency. In the network, the red circles represent the drug court participants. Blue diamonds represent program and research staff. The size of each vertex (ie, circle or diamond representing an individual) is mapped to eigenvector centrality, where the larger vertices indicate connections to more members and other members who have more connections.33 The size of the vertex is a measure of the influence of that individual. The opacity of each vertex was mapped to betweenness centrality, so that darker vertices indicate the importance of that individual in integrating the network.34 These two centrality measures are different. An individual could have a few links to other well-connected people and be portrayed as a large but not very dark circle or diamond. An individual linked to many, not very well-connected people, would appear as a small but dark circle or diamond. Eigenvector centrality measures influence by the number of connections to other members who have many connections, and betweenness centrality measures influence by the ability of the member to link other members who would not be linked otherwise. The width of the lines connecting individuals is based on the number of messages sent between each vertex.
The two social network maps that were created are pictured in Figures 5 and 6. Of interest is how highly central one staff person was (both eigenvector and betweenness type) and how the network without that individual has many more isolates (Fig. 6). Other authors have suggested that facilitation of online discussion groups is important in keeping participants active, preventing dropout, and promoting positive communication.35 The analysis in our study supports this conclusion.
Figure 5.
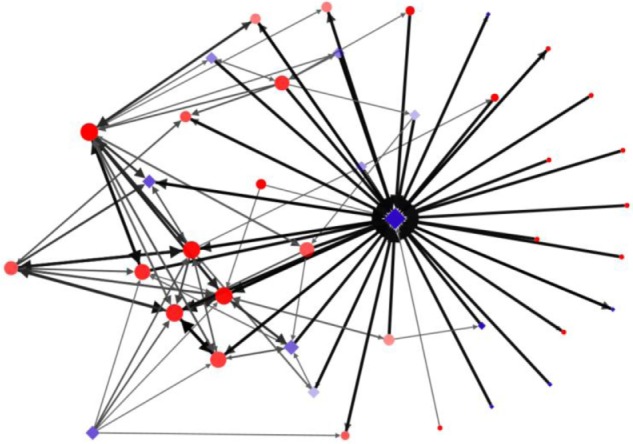
Social network map of all participants including staff.
Figure 6.
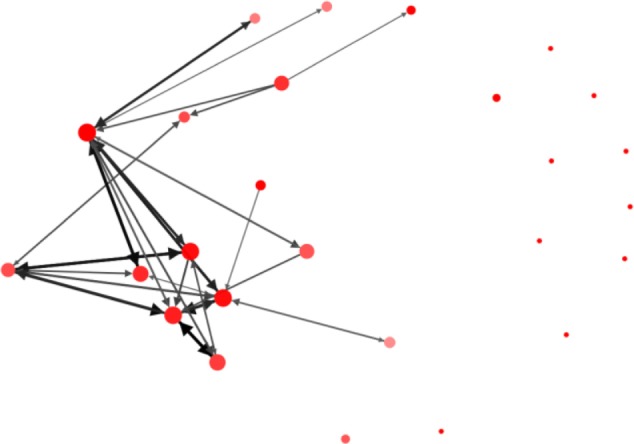
Social network map of drug court participants.
Limitations
This study is a pilot and accepted every participant in the drug court, and so there is no comparison group. Where comparisons were necessary, we used a different group in a previously published study. The study group was too small (n = 31) to draw any conclusions about whether different types of participants might behave differently, such as whether men and women used the app differently or whether people who used different types of drugs might have different use patterns. We did not collect information about specific drugs of abuse or participants’ diagnosis, but collected only basic demographic information and that they were participants in a drug court program.
Because of the brevity of the study period (four months), 12 participants kept their own mobile phones. It is likely that this reduced the use of the phone provided for the study. The study was completed at a time when most people did not have smartphones, so we could not download the app onto the participants’ own phones. Future studies may need to consider the difficulty of subjects maintaining both a personal and a study phone.
Social network analysis is a way of quantifying the relationships based on the communications between participants, but does not describe the quality of the communication and whether it was supportive of recovery. Future research using content analysis might provide more insight into how the discussion group was used and why participants in this study used it more than in the previously published study with a different population.
Discussion
Mobile health apps have become widely available in a short time despite lack of research on their effectiveness. A-CHESS has been demonstrated to be effective in reducing substance use in a clinical trial.26 However, its efficacy was demonstrated in people with a diagnosis of alcohol dependence who had completed residential treatment, which is an intensive level of care. The drug court pilot study asked a preliminary question about people whose diagnosis included a high prevalence of drug abuse/dependence, as opposed to alcohol dependence, and who were actively in treatment in a highly structured treatment and oversight environment. Would they be interested in using a recovery support app, and if so, how would they use it?
We evaluated two measures of A-CHESS utilization: frequency and quantity. We were interested in knowing the number of days the app was accessed and whether that changed over the course of the study period. In addition, we were interested in understanding quantity – how often specific services were accessed. As in some earlier studies,8,36,37 social support services were the most utilized, with the discussion forum being used most frequently. However, this was different from the clinical trial for A-CHESS, where the discussion forum page was accessed less than half as often as individual messaging.26
One explanation for this difference is that the drug court cohort includes people who know each other and communicate as a group. In contrast, participants in the clinical trial came from two different areas of the country, were recruited over a year-long period, and were unlikely to know others on the discussion boards. The network analysis offers a second explanation. A few participants communicated with each other regularly via the group discussion. However, one staff person supported the network, communicating with everyone; this person used the discussion board rather than private messaging to ask questions and provide feedback to all participants. Removing that staff person from the analysis leaves a third of the group as isolates.
This group’s use of A-CHESS also differed from that of the clinical trial group in the rapid decline in their use of the app over the course of the study period. The percentage of participants accessing each type of service decreased by more than half over the four-month period. In the first 16 weeks of the clinical trial, only the CC services decreased at that rate.27 Because of the short duration of the drug court pilot, participants continued to use personal cell phones as their primary phone rather than adopting the study phone. Twelve participants reported maintaining another phone as their primary mobile phone. It is possible that once the novelty wore off, they were less likely to carry two phones, reducing their immediate access to the A-CHESS phone.
A final interesting difference is that the drug court group was more likely to use tools designed to increase competence than tools to increase motivation, which was the inverse of the clinical trial group.26 The difference may be a result of the population (drug-addicted criminal offenders vs primarily alcohol-dependent nonoffenders), or it may be a result of the difference in where and when A-CHESS was offered in the individual’s recovery process. Drug court participants may not have had as much prior treatment at the time they received A-CHESS and may have had a greater need for tools for developing CC. They may have had a lesser need for tools to enhance motivation, given the multiple external motivators built into the drug court program. Training in how to use the app was not standardized between studies. An emphasis on different resources during training and setup may also have influenced their use during the study. Crises that arose for participants during the course of the drug court study reinforced their perception of A-CHESS as a communication tool. An instance of domestic violence and another involving a drug overdose were both resolved with the aid of A-CHESS communication tools.
This pilot points to interesting differences between the frequency and type of use of the A-CHESS app by this population, when compared with the population in a previously published study.26 It appears that the answer to the study question is yes, drug court participants will use a recovery support app. How their use of such a tool may differ from that of nonoffenders or people who are not involved in a drug court and the effectiveness of such tools in reducing drug use deserves additional study.
Acknowledgments
The authors acknowledge the funder, SAMHSA, and also thank Maureen Fitzgerald for contributing to the editing and organi zation of the paper, and Judy Ganch for help with references.
Footnotes
ACADEMIC EDITOR: Gregory Stuart, Editor in Chief
PEER REVIEW: Six peer reviewers contributed to the peer review report. Reviewers’ reports totaled 2002 words, excluding any confidential comments to the academic editor.
FUNDING: This pilot was funded by SAMHSA purchase order: HHSP233201000663P. The authors confirm that the funder had no influence over the study design, content of the article, or selection of this journal.
COMPETING INTERESTS: Two authors, Kimberly Johnson and David Gustafson, are shareholders in a company, CHESS Mobile Health, which has a license to market A-CHESS, the mobile application used in this study.
Paper subject to independent expert blind peer review. All editorial decisions made by independent academic editor. Upon submission manuscript was subject to anti-plagiarism scanning. Prior to publication all authors have given signed confirmation of agreement to article publication and compliance with all applicable ethical and legal requirements, including the accuracy of author and contributor information, disclosure of competing interests and funding sources, compliance with ethical requirements relating to human and animal study participants, and compliance with any copyright requirements of third parties. This journal is a member of the Committee on Publication Ethics (COPE). Provenance: the authors were invited to submit this paper.
Author Contributions
Conceived and designed the experiments: KJ. Analyzed the data: M-YC, TJM. Wrote the first draft of the manuscript: KJ. Contributed to the writing of the manuscript: SR, HC, DHG. Agreed with manuscript results and conclusions: KJ, M-YC, TJM, SR, HC, DHG. Jointly developed the structure and arguments for the paper: KJ, M-YC, TJM, SR, HC, DHG. Made critical revisions and approved the final version: KJ, M-YC, TJM, SR, HC, DHG. All the authors reviewed and approved the final manuscript.
REFERENCES
- 1.Leshner AI. Addiction is a brain disease, and it matters. Science. 1997;278(5335):45–7. doi: 10.1126/science.278.5335.45. [DOI] [PubMed] [Google Scholar]
- 2.Glasner-Edwards S, Rawson R. Evidence-based practices in addiction treatment: review and recommendations for public policy. Health Policy. 2010;97(2–3):93–104. doi: 10.1016/j.healthpol.2010.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.DiClemente CC, Holmgren MA, Rounsaville D. Relapse prevention and recycling in addiction. In: Johnson Bankole A., editor. Addiction Medicine. New York, NY: Springer; 2011. pp. 765–82. [Google Scholar]
- 4.Schwabe L, Dickinson A, Wolf OT. Stress, habits, and drug addiction: a psychoneu-roendocrinological perspective. Exp Clin Psychopharmacol. 2011;19(1):53–63. doi: 10.1037/a0022212. [DOI] [PubMed] [Google Scholar]
- 5.Substance Abuse and Mental Health Services Administration (SAMHSA) The TEDS Report: Substance Abuse Treatment Admissions, Referred by the Criminal Justice System. Rockville, MD: Substance Abuse and Mental Health Administration, Office of Applied Studies; 2009. Available at: http://www.samhsa.gov/data/2k9/211/211CJadmits2k9.pdf. [Google Scholar]
- 6.National Drug Court Resource Center Drug Courts Today. 2012. [Accessed February 20, 2014]. Available at: http://www.ndcrc.org/content/how-many-drug-courts-are-there.
- 7.National Association of Drug Court Professionals Types of Drug Courts. 2013. [Accessed February 20, 2014]. Available at: http://www.nadcp.org/learn/what-are-drug-courts/types-drug-courts.
- 8.Goldkamp JS, White MD, Robinson JB. Do drug courts work? Getting inside the drug court black box. J Drug Issues. 2001;31(1):27–72. [Google Scholar]
- 9.Weiss F, Ciccocioppo R, Parsons LH, et al. Compulsive drug-seeking behavior and relapse. Neuroadaptation, stress, and conditioning factors. Ann N Y Acad Sci. 2001;937:1–26. doi: 10.1111/j.1749-6632.2001.tb03556.x. [DOI] [PubMed] [Google Scholar]
- 10.Shaffer DK. Looking inside the black box of drug courts: a meta-analytic review. Justice Q. 2011;28(3):493–521. [Google Scholar]
- 11.Finney Rutten LJ, Agunwamba AA, Greene SM, et al. Enabling patient-centered communication and care through health information technology. J Commun Healthc. 2014;7(4):255–61. [Google Scholar]
- 12.Klasnja P, Pratt W. Healthcare in the pocket: mapping the space of mobile-phone health interventions. J Biomed Inform. 2012;45(1):184–98. doi: 10.1016/j.jbi.2011.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fox S, Duggan M. Mobile health 2012. Pew Internet and American Life Project. 2012. Available at: http://www.pewinternet.org/files/old-media//Files/Reports/2012/PIP_MobileHealth2012_FINAL.pdf.
- 14.Johnson K, Isham A, Shah DV, Gustafson DH. Potential roles for new communication technologies in treatment of addiction. Curr Psychiatry Rep. 2011;13(5):390–7. doi: 10.1007/s11920-011-0218-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.West JH, Hall PC, Hanson CL, Barnes MD, Giraud-Carrier C, Barrett J. There’s an app for that: content analysis of paid health and fitness apps. J Med Internet Res. 2012;14(3):e72. doi: 10.2196/jmir.1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Becker S, Miron-Shatz T, Schumacher N, Krocza J, Diamantidis C, Albrecht UV. mHealth 2.0: experiences, possibilities, and perspectives. JMIR Mhealth Uhealth. 2014;2(2):e24. doi: 10.2196/mhealth.3328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gravenhorst F, Muaremi A, Bardram J, et al. Mobile phones as medical devices in mental disorder treatment: an overview. Pers Ubiquit Comput. 2015;19(2):335–53. [Google Scholar]
- 18.Morris ME, Aguilera A. Mobile, social, and wearable computing and the evolution of psychological practice. Prof Psychol Res Pr. 2012;43(6):622. doi: 10.1037/a0029041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Marsch LA. Leveraging technology to enhance addiction treatment and recovery. J Addict Dis. 2012;31(3):313–8. doi: 10.1080/10550887.2012.694606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gustafson DH, Boyle MG, Shaw BR, et al. An e-health solution for people with alcohol problems. Alcohol Res Health. 2011;33(4):327–37. [PMC free article] [PubMed] [Google Scholar]
- 21.Gustafson DH, Shaw BR, Isham A, Baker T, Boyle MG, Levy M. Explicating an evidence-based, theoretically informed, mobile technology-based system to improve outcomes for people in recovery for alcohol dependence. Subst Use Misuse. 2011;46(1):96–111. doi: 10.3109/10826084.2011.521413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Quanbeck A, Chih M-Y, Isham A, Johnson R, Gustafson D. Mobile delivery of treatment for alcohol use disorders. Alcohol Res. 2014;36(1):111. [PMC free article] [PubMed] [Google Scholar]
- 23.Ryan RM, Deci EL. Intrinsic and extrinsic motivations: classic definitions and new directions. Contemp Educ Psychol. 2000;25(1):54–67. doi: 10.1006/ceps.1999.1020. [DOI] [PubMed] [Google Scholar]
- 24.Marlatt GA, George WH. Relapse prevention: introduction and overview of the model. Br J Addict. 1984;79(3):261–73. doi: 10.1111/j.1360-0443.1984.tb00274.x. [DOI] [PubMed] [Google Scholar]
- 25.Cacciola JS, Alterman AI, Dephilippis D, et al. Development and initial evaluation of the brief addiction monitor (BAM) J Subst Abuse Treat. 2013;44(3):256–63. doi: 10.1016/j.jsat.2012.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gustafson DH, McTavish FM, Chih MY, et al. A smartphone application to support recovery from alcoholism: a randomized clinical trial. JAMA Psychiatry. 2014;71(5):566–72. doi: 10.1001/jamapsychiatry.2013.4642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McTavish FM, Chih MY, Shah D, Gustafson DH. How patients recovering from alcoholism use a smartphone intervention. J Dual Diagn. 2012;8(4):294–304. doi: 10.1080/15504263.2012.723312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dulin PL, Gonzalez VM, Campbell K. Results of a pilot test of a self-administered smartphone-based treatment system for alcohol use disorders: usability and early outcomes. Subst Abus. 2014;35(2):168–75. doi: 10.1080/08897077.2013.821437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ubhi HK, Michie S, Kotz D, Wong WC, West R. A mobile app to aid smoking cessation: preliminary evaluation of SmokeFree28. J Med Internet Res. 2015;17(1):e17. doi: 10.2196/jmir.3479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bricker JB, Mull KE, Kientz JA, et al. Randomized, controlled pilot trial of a smartphone app for smoking cessation using acceptance and commitment therapy. Drug Alcohol Depend. 2014;143:87–94. doi: 10.1016/j.drugalcdep.2014.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chaple M, Sacks S, McKendrick K, et al. Feasibility of a computerized intervention for offenders with substance use disorders: a research note. J Exp Criminol. 2014;10:105–27. doi: 10.1007/s11292-013-9187-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Harel D, Koren Y. A fast multi-scale method for drawing large graphs. In: Marks J, editor. Graph Drawing. Heidelberg: Springer; 2001. pp. 183–96. [Google Scholar]
- 33.Bonacich P. Some unique properties of eigenvector centrality. Soc Networks. 2007;29(4):555–64. [Google Scholar]
- 34.Freeman LC. A set of measures of centrality based on betweenness. Sociometry. 1977;40(1):35–41. [Google Scholar]
- 35.O’Grady L, Bender J, Urowitz S, Wiljer D, Jadad AR. Promoting and participating in online health forums: a guide to facilitation and evaluation for health professionals. J Commun Healthc. 2010;3(3–4):246–57. [Google Scholar]
- 36.Awoyinka I, Atwood AK, Shanovich KK, Sorkness C, McTavish F, Gustafson DH. The effects of a mhealth intervention on asthma symptom control in inner-city teens. J Mob Technol Med. 2012;1(4S):27. [Google Scholar]
- 37.Han JY, Wise M, Kim E, et al. Factors associated with use of interactive cancer communication system: an application of the comprehensive model of information seeking (CMIS) J Comput Mediat Commun. 2010;15(3):367–88. doi: 10.1111/j.1083-6101.2010.01508.x. [DOI] [PMC free article] [PubMed] [Google Scholar]