Abstract
The provision of trauma care is a financial burden, continually associated with low reimbursement, and shifts the economic burden to major trauma centers and providers. Meanwhile, the volume of craniomaxillofacial (CMF) trauma and the number of surgically managed facial fractures are unchanged. Past financial analyses of cost and reimbursement for facial trauma are limited to mandibular and midface injuries, consistently revealing low reimbursement. The incurred financial burden also coincides with the changing landscape of health insurance. The goal of this study is to determine the opportunity cost of operative management of facial trauma at our institution. From our CMF database of greater than 3,000 facial fractures, the physician charges, collections, and relative value units (RVUs) for CMF trauma per year from 2007 to 2013 were compared with a general plastic surgery and otolaryngology population undergoing operative management during this same period. Collection rates were analyzed to assess if a significant difference exists between reimbursement for CMF and non-CMF cases. Results revealed a significant difference between the professional collection rate for operative CMF trauma and that for other operative procedures (17.25 vs. 29.61%, respectively; p < 0.0001). The average number of RVUs billed per provider for CMF trauma declines significantly, from greater than 700 RVUs to 300 over the study period, despite a stable volume. Surgical management of CMF trauma generates an unfavorable financial environment. The large opportunity cost associated with offering this service is a potential threat to the sustainability of providing care for this population.
Keywords: facial trauma, reimbursement, costs
The provision of trauma care is a financial burden, continually associated with low reimbursement, and shifts the economic burden to major trauma centers and providers.1 2 3 4 5 6 7 8 9 According to the Centers for Disease Control and the National Trauma Institute, trauma accounts for 41 million emergency department visits and 2.3 million hospital admissions across the United States. Data extracted from the National Trauma Database from 2008 to 2013 demonstrate that facial trauma represents 14 to 25% of trauma visits. The overall economic burden of trauma is estimated around $400 billion a year, including both health care costs and lost productivity.10 However, given the scope of craniomaxillofacial (CMF) trauma, the economic or financial impact remains less well defined. Previous studies have illustrated a financial burden that corresponds with the changing landscape of health insurance.3 4 6 7 Previous analyses of the financial aspect of CMF trauma have been limited to isolated facial fractures or specific subsites, such as the mandible or midface.3 4 5 Studies focusing on the financial aspects of management of mandibular trauma have revealed low reimbursement rates and lost income that was, in part, attributable to payer type, including those uninsured as well as those covered by federal agencies, such as Medicare, Medicaid, federal/state prisoners, and Veterans Administration.3 7 8 The study by Dillon et al focusing on mandibular trauma revealed an increase in patients with charity or unsponsored care from 6.7% in 1999 to 51.4% in 2010, while during the same time period the institution had excess of $15 million in unrecovered potential revenue.3 7 Additional studies have focused on management strategies, including adjustment of operative protocols, to assess the economic factors at play in operative management of isolated fractures.4 5 As a systematic analysis of the financial implications of operatively managed facial trauma was absent in the literature, Erdmann et al reviewed 202 patients from our institution that revealed a significantly lower reimbursement for surgical professional charges when compared with other professional services.8
Despite the previous studies investigating multiple aspects of operative facial fracture management, none have investigated the opportunity cost to the physician treating CMF trauma. Opportunity cost is defined by the third edition of the New Oxford American Dictionary as: “the loss of potential gain from other alternatives when one alternative is chosen over another,” such as choosing to include CMF trauma within one's scope of clinical practice. One study by Koenig and Lewis published in 1993 begins to comment on opportunity cost. The study compares not only reimbursement, but also litigation and clinic productivity lost due to missed appointments through a retrospective review of 50 consecutive facial trauma patients that were treated operatively and a sequential series of 20 patients with basal cell carcinoma (BCC) of the cheek treated by the same plastic surgeon at a university medical center.9 The trauma group only paid, on average, 57% of their charges, while the BCC group paid 90% (p < 0.01). There were also significant differences in compliance with follow-up with at least 46% missing one or more appointments in the trauma group, but only one missed appointment in the comparative group. Furthermore, litigation ensued in 30% of the trauma cases, while there were no reported incidents of litigation with the BCC patients.9 Koenig's study effectively identified not only the significant discrepancy in reimbursement, but also the added factors of lost productivity due to unfulfilled/missed clinic appointments and the underlying threat of litigation, highlighting the opportunity cost incurred by physicians associated with operative facial trauma management.
When physicians choose, or are contractually obligated, to treat CMF trauma, variable potential opportunity costs exist. Opportunity cost is not limited to monetary or financial costs alone, although these factors may comprise a large portion of what is considered opportunity cost. The concept of opportunity cost also accounts for lost time (such as time away from a physician's standard practice), pleasure (time with family or not on call), or any benefit that provides utility.
The goal of this study is to investigate the opportunity cost of surgical management of CMF trauma as it relates to the financial burden of operative facial fracture management. The professional charges and collections for patients with operatively managed facial fractures were compared with professional charges and collections for general plastic surgery and otolaryngology patients at our institution undergoing operative management during the same period.
Patients and Methods
Collection of Patient Data
For each patient who underwent operative management of facial fractures between 2007 and 2013 at Duke University Medical Center, the following data were collected and entered into an electronic database (Microsoft Office Professional Plus 2010; Microsoft Corporation, Redmond, WA): date of initial encounter, date of initial procedure, diagnosis code, current procedural terminology code, physician billing, physician payments, number of relative value units (RVUs), and payor type. The physician (professional) charges included were limited to the operative surgeon only. For the payor type, these include private insurance, Medicaid, Medicare, Veteran's Affairs, Workers' Compensation, federal/state prison inmates, and no insurance/self-pay.
Professional charges and collections as well as RVUs for patients undergoing operative management of facial fractures were compared across the general Otolaryngology-Head and Neck Surgery, Facial Plastic Surgery, Oral & Maxillofacial Surgery, and general Plastic Surgery patient population for each of the five surgical attendings in the facial trauma call pool at Duke University Medical Center during the study years of 2007 to 2013. These charges and collections were compared against the nonfacial trauma operative charges and collections for the same attendings during the same time period.
Statistical Analysis
Data were organized and partially analyzed using Microsoft Excel. Full data analysis was completed using the SAS system (Statistical Analysis System 2013; SAS Institute Inc; Cary, NC).
Results
Between 2007 and 2013, there were 1,229 facial fractures evaluated by the CMF trauma team. Of these, 872 facial fractures were managed operatively, representing 764 patients with facial fracture subsites (Fig. 1). Only those managed operatively were included in the study. The sum of professional charges billed for CMF trauma was $3,735,027 with an average of $4,889 per patient. The collections totaled $644,141.86 with an average of $843 per patient. For operatively managed CMF trauma, the data yield an overall reimbursement rate of 17.39%. Of these patients, only 36% were uninsured, 36% were insured with private or commercial insurance, and 23% were insured with Medicare or Medicaid. The sum of professional charges for the non-CMF patients was $31,830,987 with total collections of $9,423,768 (Fig. 2). The total collection rate for the non-CMF patient population was 29.81%. There was a significant (p ≤ 0.0001) difference in collection rates between operatively managed CMF trauma and a non-CMF patient population.
Fig. 1.
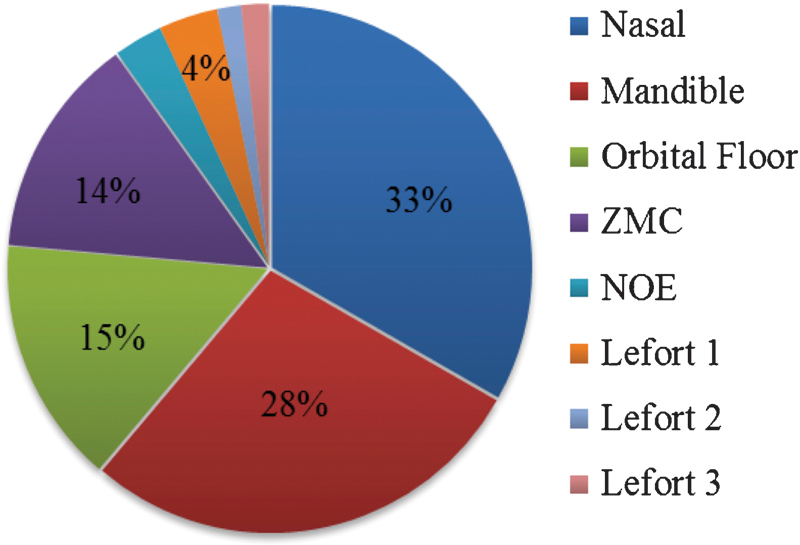
Operatively managed facial fractures by subsite.
Fig. 2.
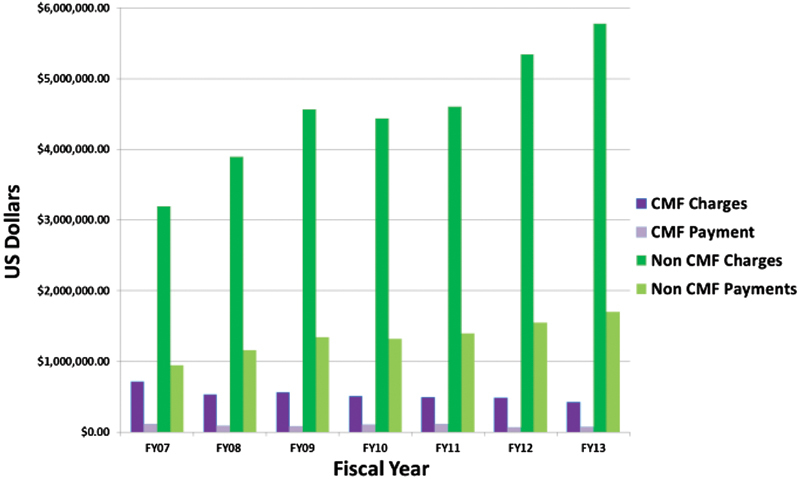
Professional charges and collections for patients undergoing operative management of facial fractures (CMF) and non-CMF patients.
Overall mean collection rates for the CMF group ranged from 14 to 22%, while for the non-CMF group the rates ranged from 29 to 31% (Fig. 3). The collection rate over the study period did not vary significantly on a year-to-year basis for either the CMF or non-CMF group. When exclusively comparing fiscal year 07–09 with fiscal year 12–13, which correspond to years when the number of physicians comprising the CMF call pool were three and five, respectively, there was no significant difference in the collection rate (p = 0.8522). These data reveal that the collection rate for CMF trauma does not fluctuate on an annual basis and is independent of the number of attending physician providers.
Fig. 3.
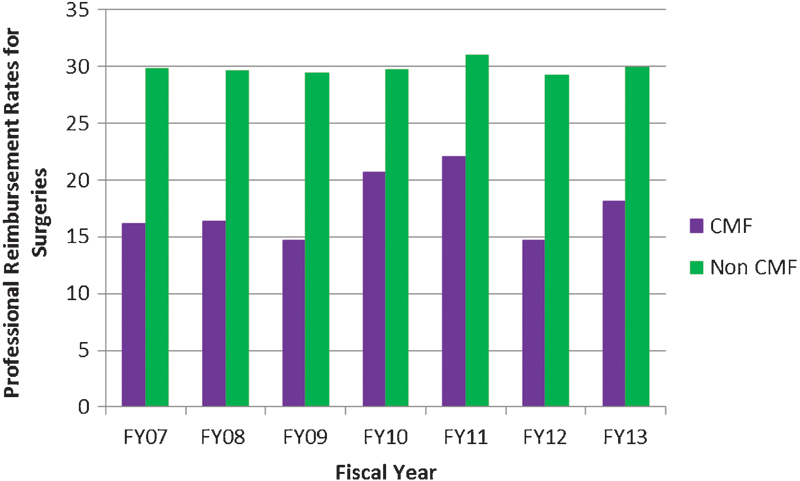
Professional reimbursement rates for surgeons in the following categories: operatively managed facial fractures (CMF) and Division of Otolaryngology/Head and Neck Surgery and Plastic, Reconstructive, Maxillofacial and Oral Surgery.
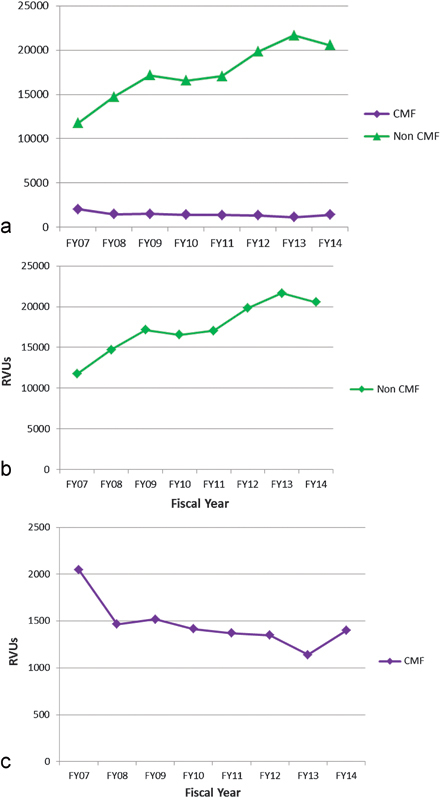
Total RVUs from fiscal year 2007 to fiscal year 2013 for CMF trauma were 10,307 RVUs. The number of RVUs associated with the non-CMF surgical group totaled 118,697. An analysis of the average RVUs for the CMF group in comparison to the non-CMF group revealed a significant difference between the two groups (p = 0.0002). Over time, the RVUs billed for the CMF group declined significantly in a logarithmic fashion (p ≤ 0.0001).
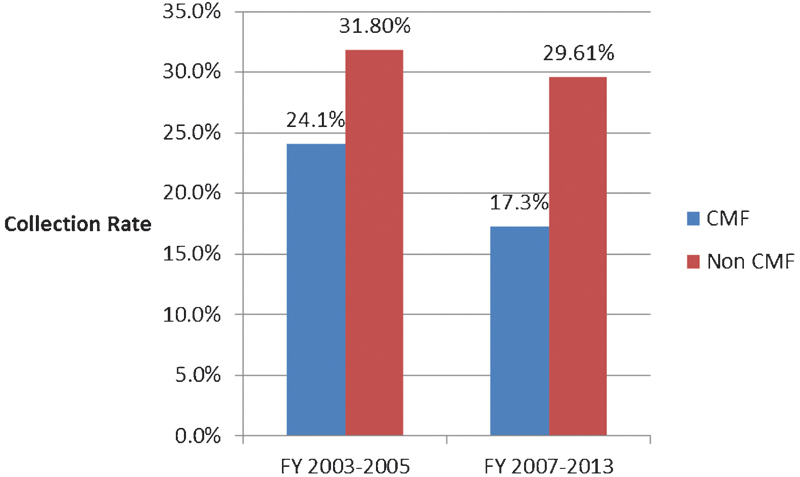
The collection rates at Duke University Medical Center for operatively managed CMF trauma have declined from 24.1% (2003–2005) to 17% (2007–2013), a statistically significant finding (p < 0.05), while the collection rates for the control group of non-CMF surgical procedures remain constant at 31.8% (2003–2005) to 29% (2007–2013).8
Discussion
CMF trauma affects ∼10 million individuals in the United States annually.10 Necessary evaluation, and management thereof, generates an unfavorable economic environment and at times is costly to those physicians and hospital systems providing the care.3 7 Thus far, literature analyses of charges, payments, and reimbursements have focused on particular types of facial fractures, mainly limited to operative and/or conservative management of mandible fractures. Additional studies have focused on the financial aspect of inpatient hospitalization associated with the operative management of limited or isolated facial fractures. In a recent survey of junior practicing otolaryngologists, insufficient reimbursement was cited by 52% as deterrent for treating CMF trauma, which is a direct risk to the sustainability of providing CMF trauma care.11
The data presented in Fig. 4 support the hypothesis that there is a lower professional collection rate (17%) for operatively managed facial trauma in a tertiary medical center when compared with the overall professional collection rates (29%) of these same providers from different surgical subspecialties. In comparison to the Duke University Medical Center data from 2003 to 2005, there has been a significant decline in the collection rate for operatively managed facial trauma from 24 to 17%.8 A recent survey of 57 Level-I trauma centers revealed that plastic surgeons comprise 40% of the call coverage for facial trauma, with maxillofacial surgeons responsible for 36%, followed by otolaryngologists (23%).12 The participation of each specialty in CMF trauma care is in addition to their primary consultative, outpatient, and surgical practices. Operative management alone, aside from clinic responsibilities associated with these patients, can easily interfere and derail regularly scheduled elective surgeries and clinic schedules.13
Fig. 4.
Comparison of collection rates for operatively managed facial trauma at our institution in comparison to study by Erdmann et al.
Reimbursement rate has been closely linked to patient health care coverage in previous studies and this same variation in coverage type was seen at our institution. Dillon et al at Harborview Medical Center noted a decline in reimbursement for operatively managed mandible fractures that correlated with an increase in the number of uninsured patients (6.7–51.4%) over their study period.3 This overall change in payor mix resulted in greater than $15 million of unrecovered revenue. Duke University Medical Center has also seen an increase in self-pay patients with an increase from 26 (prior to the study period) to 36%.3 14 At a national level, most trauma centers had an average of 21% commercial coverage over the past 6 years and the number of uninsured patients with CMF trauma has increased substantially from 25% in 2007 to as high as 51% in 2010, suggesting a national decline in reimbursement based on payor type alone, as the economic burden is shifted to the hospitals and their providers.3 14 15
As reimbursement relates to opportunity cost for the provider, whether by choice alone, stipend provision, or contractual obligation to participate in CMF trauma care, our data strongly support that there is financial opportunity cost incurred when treating this patient population. In comparison to one's own subspecialty non–trauma-related surgical practice, participation in facial trauma care appears uneconomical and therefore participation may be less desirable to the specialty surgeon. This opportunity cost extends beyond monetary costs alone as it also includes additional time on call with nights and weekends that may otherwise be spent with family or other activity outside of the health care setting. There is also a loss of potential gain in the clinic setting when clinic appointments for potential patients are occupied by CMF trauma patients that historically are poorly compliant.9
RVU trends associated with operatively managed facial trauma care are not well defined. Over our study period, there is a significant decline in the number of RVUs billed for CMF trauma during fiscal years 2007 to 2013 (Fig. 5). In comparison to recently published data from another Level-I trauma center encompassing a similar time period, the annual operative RVUs for our CMF population ranged per surgeon from 558 in 2007 to 328 in 2013, with an overall average of 461, as compared with a range of 235 to 426 with average of 309 described by Osman et al.13 This comparison of recent data suggests that our CMF trauma experience is similar to, or greater than, that of other Level-I trauma centers. However, the data presented by Osman et al include a trend analysis that most of the annual RVUs were nonoperative until 2011, when the operative RVUs surpassed the nonoperative counterpart, the opposite of which is true at our institution.13 Furthermore, the overall decline in RVUs experienced from years 2007 to 2013 occurred despite a stable case volume, that is, no significant change in number of operative cases corresponding with a decline in the number of RVUs. Possible explanations include annual scheduled changes to the RVUs, more judicious use of conservative approaches, and/or increase in closed reduction techniques based on biases of the attending staff surgeon. Additionally, attending oversight may have increased and, that with attending oversight, a resultant increase in nonoperative management and corresponding decrease in the number of RVUs billed. For example, addressing certain facial fractures in the emergency room with more conservative measures, such as arch bars, with the oversight of an attending, as opposed to an invasive, procedure in the operating room, generates different billable RVUs. Another potential explanation is an overall shift toward conservative management when treating CMF trauma; however, this general trend is not isolated to this study period. With the inclusion of fiscal year 2014 following our initial results, there is an increase in RVUs as compared with the initial study period. It is unclear if this upward trend in RVUs will be isolated to fiscal year 2014 or is the beginning of an overall return to previous RVU amounts experienced in earlier years.
Fig. 5.
RVUs billed per fiscal year for operatively managed facial fractures. (a) RVUs for facial and nontrauma CMF. (b) RVUs for nontrauma. (c) RVUs for facial trauma.
Future areas of focus for this study population will include the effect of closed versus open management of CMF trauma on collection rates. With closed versus open techniques, one would infer that with closed reduction techniques there is decreased time in the operating room as well as decreased capital outlays for equipment, with a reflexive effect on overall charges and facility costs.16 17 Acceptance of this perspective, however, may result in exorbitant future and secondary charges to the health care system due to the significant costs associated with surgical management of complications such as malocclusion, trismus, and functional deficits.18 The delayed costs associated with repair of iatrogenic or pathologic complications may well exceed the overall costs associated with definitive rigidly fixed primary repair. Other well-established criteria for cost containment in CMF trauma management is to discharge the stable patient from the emergency room and schedule the operative procedure as an elective outpatient.4 5 While some patients may wish to pursue hospitalization and immediate treatment, this choice alleviates the need for an inpatient hospital charge, significantly decreasing health care costs, as well as improving the opportunity cost for the operative surgeon by scheduling the case at a more convenient time.4 5 The dichotomy of what to do with the “unfunded” patient should become less prevalent with maturation of the Affordable Care Act. Another important consideration for future studies includes the financial implications of transferred patients. This represents a lost opportunity to cost to not only treating physicians, but also receiving hospitals, as the “primary” institution is able to charge for the initial evaluation and stabilization and the receiving institution does not necessarily get reimbursed by Medicaid or Medicare for those transfers.
Our 7-year data in operative management of facial fractures represent a consistently stable volume of CMF trauma and the conclusions therein reliably support the notion that the current processes of providing facial trauma care are not sustainable. There are, however, self-identified limitations to the study. Inconsistent CMF trauma consultation in the emergency department will lead to an under-reporting of facial fractures; also, the study does not address the financial implications of hospital transfers, which undoubtedly may have affected this tenuous financial balance. Variations between the treatment protocols preferences of the various surgical attending staff impact significantly the scope, and ultimate costs, of treatment provided.
Lastly, the impact of the Affordable Care Act continues to be unclear as there are multiple levels that could theoretically affect reimbursement rates for hospitals and physicians. Regarding trauma care, and particularly CMF trauma, while one may anticipate an increase in the insured care we provide, many of the patients cared for are below the poverty level. For these patients, the emergency room may remain their primary modality for medical care, as they cannot be turned away and, given their financial situation, have no money for which to be billed or otherwise penalized. Nonetheless, the effect of the newly implemented Affordable Care Act will have far-reaching impacts and must be considered in future financial analyses.
Conclusion
There is a significant difference between the physician professional collection rate for surgical management of CMF trauma and that for a matched non-CMF surgical patient population. This difference represents a direct opportunity cost to physicians treating CMF trauma. While our study does not include the financial implications of missed appointments and potential litigation, these factors must also be considered as they relate to the overall opportunity cost incurred by physicians. Additionally, the RVUs for CMF trauma show a general decline over this 7-year study period, which may represent a change in attending oversight or management principles. This is a retrospective financial and productivity analysis from a Level-I trauma center. The study confirms that surgical management of CMF trauma generates an unfavorable financial environment. The large opportunity cost associated with offering this service is a potential threat to the sustainability of providing care for this population.
In light of these circumstances, the future management of CMF trauma may ultimately become a subspecialty managed through financial arrangements within the representative health care system subsidizing, or effectively employing, specialists in this arena much like orthopedic trauma, trauma surgery, and neurosurgical trauma.
References
- 1.Lanzarotti S, Cook C S, Porter J M, Judkins D G, Williams M D. The cost of trauma. Am Surg. 2003;69(9):766–770. [PubMed] [Google Scholar]
- 2.Lee L N, Bhattacharyya N. Contemporary trends in procedural volume for adult facial trauma, 1996-2006. Otolaryngol Head Neck Surg. 2012;146(2):226–229. doi: 10.1177/0194599811427825. [DOI] [PubMed] [Google Scholar]
- 3.Dillon J K, Christensen B, McDonald T, Huang S, Gauger P, Gomez P. The financial burden of mandibular trauma. J Oral Maxillofac Surg. 2012;70(9):2124–2134. doi: 10.1016/j.joms.2012.04.048. [DOI] [PubMed] [Google Scholar]
- 4.David L R, Bisseck M, Defranzo A, Marks M, Molnar J, Argenta L C. Cost-based analysis of the treatment of mandibular fractures in a tertiary care center. J Trauma. 2003;55(3):514–517. doi: 10.1097/01.TA.0000025319.71666.2D. [DOI] [PubMed] [Google Scholar]
- 5.Sanger C Argenta L C David L R Cost-effective management of isolated facial fractures J Craniofac Surg 2004154636–641., discussion 642 [DOI] [PubMed] [Google Scholar]
- 6.van den Bergh B, Heymans M W, Duvekot F, Forouzanfar T. Treatment and complications of mandibular fractures: a 10-year analysis. J Craniomaxillofac Surg. 2012;40(4):e108–e111. doi: 10.1016/j.jcms.2011.05.015. [DOI] [PubMed] [Google Scholar]
- 7.Abubaker A O Lynam G T Changes in charges and costs associated with hospitalization of patients with mandibular fractures between 1991 and 1993 J Oral Maxillofac Surg 1998562161–167., discussion 167–168 [DOI] [PubMed] [Google Scholar]
- 8.Erdmann D, Follmar K E, Debruijn M. et al. A retrospective analysis of facial fracture etiologies. Ann Plast Surg. 2008;60(4):398–403. doi: 10.1097/SAP.0b013e318133a87b. [DOI] [PubMed] [Google Scholar]
- 9.Koenig W J, Lewis V L Jr. The physician cost of treating maxillofacial trauma. Plast Reconstr Surg. 1993;91(5):778–782. doi: 10.1097/00006534-199304001-00004. [DOI] [PubMed] [Google Scholar]
- 10.Finkelstein E A, Corso P S, Miller T R. New York: Oxford University Press; 2006. The Incidence and Economic Burden of Injuries in the United States. [Google Scholar]
- 11.McCusker S B, Schmalbach C E. The otolaryngologist's cost in treating facial trauma: American Academy of Otolaryngology—Head and Neck Surgery survey. Otolaryngol Head Neck Surg. 2012;146(3):366–371. doi: 10.1177/0194599811429007. [DOI] [PubMed] [Google Scholar]
- 12.Bagheri S C, Dimassi M, Shahriari A, Khan H A, Jo C, Steed M B. Facial trauma coverage among level-1 trauma centers of the United States. J Oral Maxillofac Surg. 2008;66(5):963–967. doi: 10.1016/j.joms.2008.01.020. [DOI] [PubMed] [Google Scholar]
- 13.Osman M F, Baugh R F, Baugh A D, Welch M C, Sferra J J, Williams M. Relative value units and payer mix analysis of facial trauma coverage at a level 1 trauma center: is the current model sustainable? Surgery. 2014;156(4):995–1000. doi: 10.1016/j.surg.2014.06.046. [DOI] [PubMed] [Google Scholar]
- 14.National and Regional Statistics from the NIS United States Department of Health and Human Services Agency for Healthcare Research and Quality Available at: http://hcup.ahrq.gov/HCUPnet.jsp. Accessed March 23, 2015
- 15.Holahan J, Cook A. Changes in economic conditions and health insurance coverage, 2000–2005. Health Aff (Millwood) 2005;5:498–508. doi: 10.1377/hlthaff.w5.498. [DOI] [PubMed] [Google Scholar]
- 16.Schmidt B L Kearns G Gordon N Kaban L B A financial analysis of maxillomandibular fixation versus rigid internal fixation for treatment of mandibular fractures J Oral Maxillofac Surg 200058111206–1210., discussion 1210–1211 [DOI] [PubMed] [Google Scholar]
- 17.Jurić M, Novakovic J, Carapina M, Kneiević E. Treatment cost of patients with maxillofacial fractures at the University Hospital in Mostar 2002-2006. Coll Antropol. 2010;34(1) 01:199–203. [PubMed] [Google Scholar]
- 18.Dodson T B, Pfeffle R C. Cost-effectiveness analysis of open reduction/nonrigid fixation and open reduction/rigid fixation to treat mandibular fractures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;80(1):5–11. doi: 10.1016/s1079-2104(95)80008-5. [DOI] [PubMed] [Google Scholar]