Abstract
A growing body of evidence has revealed that resident cells of the central nervous system (CNS), and particularly the glial cells, comprise a neuroimmune system that serves a number of functions in the normal CNS and during adverse conditions. Cells of the neuroimmune system regulate CNS functions through the production of signaling factors, referred to as neuroimmune factors. Recent studies show that ethanol can activate cells of the neuroimmune system, resulting in the elevated production of neuroimmune factors, including the cytokine interleukin-6 (IL-6). Here we analyzed the consequences of this CNS action of ethanol using transgenic mice that express elevated levels of IL-6 through increased astrocyte expression (IL-6-tg) to model the increased IL-6 expression that occurs with ethanol use. Results show that increased IL-6 expression induces neuroadaptive changes that alter the effects of ethanol. In hippocampal slices from non-transgenic (non-tg) littermate control mice, synaptically evoked dendritic field excitatory postsynaptic potential (fEPSP) and somatic population spike (PS) at the Schaffer collateral to CA1 pyramidal neuron synapse were reduced by acute ethanol (20 or 60 mM). In contrast, acute ethanol enhanced the fEPSP and PS in hippocampal slices from IL-6 tg mice. Long-term synaptic plasticity of the fEPSP (i.e., LTP) showed the expected dose-dependent reduction by acute ethanol in non-tg hippocampal slices, whereas LTP in the IL-6 tg hippocampal slices was resistant to this depressive effect of acute ethanol. Consistent with altered effects of acute ethanol on synaptic function in the IL-6 tg mice, EEG recordings showed a higher level of CNS activity in the IL-6 tg mice than in the non-tg mice during the period of withdrawal from an acute high dose of ethanol. These results suggest a potential role for neuroadaptive effects of ethanol-induced astrocyte production of IL-6 as a mediator or modulator of the actions of ethanol on the CNS, including persistent changes in CNS function that contribute to cognitive dysfunction and the development of alcohol dependence.
Keywords: synaptic plasticity, EEG, gamma frequency, glia, ethanol withdrawal hyperexcitability, neuroimmune, STAT3, long-term potentiation
1. Introduction
Neuroimmune factors play critical roles in homeostatic regulation of CNS function, neuronal development, defense against insult and infection, and repair mechanisms. Abnormal production of neuroimmune factors is considered an important contributing factor to many neuropsychiatric and neurologic condition, such as major depression (Sukoff Rizzo et al., 2012; Young et al., 2014), dementia (Trapero and Cauli, 2014), Alzheimer’s disease (Luterman et al., 2000), epilepsy (Li et al., 2011), schizophrenia (Schwieler et al., 2015), autism (Wei et al., 2013), sleep disturbances (Zhu et al., 2012), infection (Jurgens et al., 2012), and trauma (Lloyd et al., 2008). Importantly, recently studies have identified that excessive alcohol (ethanol) exposure, which is known to produce cognitive impairment, induces elevated glial production of IL-6 and other neuroimmune factors (Alfonso-Loeches et al., 2010; Doremus-Fitzwater et al., 2014). Excessive alcohol use is often co-morbid with neuropsychiatric and neurologic conditions, and is thought to impact negatively on these conditions (e.g., depression (Briere et al., 2014), epilepsy (Shield et al., 2013), trauma (Kachadourian et al., 2014), HIV infection (Silverstein et al., 2014)). Thus, insight into actions of IL-6 and interactions between IL-6 and ethanol are an important step toward an understanding CNS mechanism involved in the effects of ethanol on the brain and potential interactions with mechanisms underlying neuropsychiatric and neurologic conditions comorbid with alcohol use disorders.
A number of in vivo and in vitro studies have established that both acute and chronic ethanol alter CNS expression of IL-6 and other neuroimmune factors, primarily due to an action of ethanol on astrocytes and microglia. These neuroimmune factors include the proinflammatory cytokines IL-6, IL-1β and TNF-α and the chemokine CCL2 (Alfonso-Loeches et al., 2010; Blanco et al., 2005; He and Crews, 2008; Kane et al., 2013; Kane et al., 2014; Lippai et al., 2013; Qin and Crews, 2012; Tiwari et al., 2009; Valles et al., 2004; Vongvatcharanon et al., 2010; Ward et al., 2009; Zhang et al., 2014; Zhao et al., 2013). Ethanol-induced CNS expression of these neuroimmune factors appears to depend on brain region, cell type, and/or dose, duration and method of ethanol exposure. In recent studies acute ethanol (4 g/kg, i.p.) was shown to produce a prominent and prolonged increase (3–9 hrs) in the level of IL-6 mRNA in the hippocampus of rats, whereas the level of TNF-α mRNA was reduced, and the level of IL-1 β mRNA was unaffected (Doremus-Fitzwater et al., 2014). Chronic ethanol (6 g/kg per day for 10 days, by gavage) increased IL-6 mRNA levels in the CNS of adult mice, but only in cerebellum, whereas increased levels of CCL2 mRNA were observed in hippocampus, cerebellum and cortex, and TNF-α mRNA levels were not altered in any of these three CNS regions (Kane et al., 2014). Chronic ethanol consumption (13 g/kg per day for 5 months) induced a toll-like receptor 4 (TLR4) response in the cortex of mice that was associated with astrocyte activation and production of IL-6 mRNA, and IL-1 and TNF-α protein, an effect that was not observed in TLR4 knockout mice (Alfonso-Loeches et al., 2010). Increased levels of IL-6, IL-1β and TNF-α protein in the CNS of mice were also observed following three weeks of ethanol consumption using a two-bottle choice drinking paradigm (Zhang et al., 2014). Both acute (100 mM, 24 hr) and chronic (50 mM, 7 day) ethanol increased IL-6 production in primary cultures of cortical astrocytes, whereas there was no effect of ethanol on TNF-α production (Sarc et al., 2011). Ethanol (50–100 mM, 24 hr) also increased secretion of cytokines in primary cultures of cerebral microglia, including IL-6, TNF-α, MIP-1-α and MIP-2 (Boyadjieva and Sarkar, 2010).
While these and other studies have established that both acute and chronic ethanol alter CNS expression of neuroimmune factors, little is known about the consequences of this action of ethanol and underlying mechanisms. Fundamental to this issue is an understanding of how neuroimmune factors affect basic neuronal functions such synaptic transmission and cell excitability, which are target sites of ethanol action, and if or how the actions of neuroimmune factors and ethanol interact.
In the hippocampus, ethanol has been shown to alter hippocampal function through modifications of cellular mechanisms mediating synaptic transmission and plasticity (Peris et al., 1997; Weiner and Valenzuela, 2006; White and Swartzwelder, 2004; Zorumski et al., 2014). IL-6 and other proinflammatory cytokines (e.g. IL-1β and TNF-α also alter hippocampal synaptic transmission and plasticity (Beattie et al., 2002; Bellinger et al., 1993; Coogan and O'Connor, 1997; Ikegaya et al., 2003; Katsuki et al., 1990; Li et al., 1997; Nelson et al., 2012; O'Connor and Coogan, 1999; Pribiag and Stellwagen, 2013; Steffensen et al., 1994; Stellwagen and Malenka, 2006; Tancredi et al., 2000; Tancredi et al., 1992; Wheeler et al., 2009; Yang et al., 2005; Zhang et al., 2010). This commonality of ethanol and cytokine action raises the possibility that increased levels of proinflammatory cytokines produced by ethanol could result, either directly or indirectly, in transient or long-term neuroadaptive changes that then alter the effects of ethanol. Our studies focus on this possibility.
In the current studies, we utilized transgenic mice and their non-tg littermate controls to determine if elevated CNS expression of IL-6 can lead to neuroadaptive changes that alter the effects of acute ethanol on hippocampal synaptic function. The transgenic mice model the increased CNS expression of IL-6 that would occur with ethanol use. Expression of elevated levels of IL-6 in the CNS of the IL-6 tg mice was achieved through genetic manipulation of astrocyte expression (Campbell et al., 1993). Astrocytes are the most abundant cell type in the CNS and produce IL-6 both under physiological and pathological conditions (Gruol and Nelson, 1997). Ethanol has been shown to cause increased astrocyte production of IL-6 protein (Alfonso-Loeches et al., 2010; Sarc et al., 2011). Thus, the consequences of the increased astrocyte production of IL-6 in the IL-6 tg mice can inform on potential consequences of ethanol-induced increase in astrocyte production of IL-6.
Expression of IL-6 in the IL-6 tg mice is under control of the GFAP promoter. GFAP mRNA expression, which is regulated by IL-6 acting through STAT3, and GFAP protein do not become prominent until about 1 month postnatal, suggesting that IL-6 production is not prominent until about 1 month postnatal (Sanz et al., 2008). Thus, results from this model are likely to be most relevant to alcohol use that starts in the juvenile or adolescent stage of life, a pattern of alcohol use that has significant risk for developing alcohol dependence and is currently an important societal issue (Foltran et al., 2011; Hingson et al., 2006). Studies in animal models have shown that ethanol exposure increases IL-6 levels in the CNS of adolescents as well as adults (Doremus-Fitzwater et al., 2015).
The highest number of transgene-expressing astrocytes in the forebrain region of the IL-6 tg mice occurs in the hippocampus (Vallieres et al., 2002), making it likely that neuroadaptive effects on synaptic transmission will be evident in this CNS region. The hippocampus expresses one of the highest levels of mRNA for IL-6 receptors (IL-6R), which mediate cellular effects of IL-6, suggesting an important role for IL-6 in this CNS region (Gadient and Otten, 1994; Schobitz et al., 1993). Both neurons and glia cells of the hippocampus express IL-6R (Schobitz et al., 1993; Vollenweider et al., 2003). Astrocytes are a key regulator of synaptic function (Halassa et al., 2007) and astrocyte produced IL-6 or exogenously applied IL-6 has been shown to alter (i.e., depress) hippocampal synaptic plasticity at the Schaffer collateral to CA1 neuron synapse (Balschun et al., 2004; Li et al., 1997; Tancredi et al., 2000). Interestingly, synaptic plasticity at this synapse is also depressed by acute ethanol (Blitzer et al., 1990; Fujii et al., 2008; Izumi et al., 2005; Schummers et al., 1997; Sinclair and Lo, 1986), and these actions of ethanol are thought to contribute to the impairment in memory and learning produced by ethanol.
Our previous studies showed that synaptic transmission at the Schaffer collateral to CA1 pyramidal neuron synapse is enhanced in the IL-6 tg mice, consistent with the expression of persistent neuroadaptive changes in synaptic function in the IL-6 tg mice (Nelson et al., 2012). These neuroadaptive changes in synaptic function may be related to the enhanced susceptibility of the IL-6 tg mice to NMDA- and kainate-induced seizure activity (Samland et al., 2003). Ethanol exposure also results in increased susceptibility to seizure activity, as a consequence of transient or persistent ethanol-induced neuroadaptive changes that render the CNS dependent on the presence of ethanol. When ethanol exposure is terminated, a synaptic imbalance is created that results in hyperexcitability and increased susceptibility to seizure activity (Becker, 2000; Heilig et al., 2010). Thus, neuroadaptive changes in the CNS of the IL-6-tg mice could influence the effects of ethanol on synaptic function and susceptibility to ethanol-induced hyperexcitability/seizure activity, possibilities that we have assessed in the current studies. Results are consistent with interactions between the neuroadaptive changes in the CNS of IL-6 tg mice and the effects of ethanol, and suggest that ethanol-induced astrocyte production of IL-6 may play an important role as a mediator or modulator of CNS actions of ethanol, including persistent changes in CNS function that contribute to the cognitive dysfunction and development of dependence.
2. Materials and methods
2.1. Transgenic mice
The studies were carried out in IL-6-tg mice (heterozygote low expressor from the 167 line (Campbell et al., 1993)). These mice express moderately elevated levels of IL-6 in the CNS through increased astrocyte expression. Age-matched littermates that do not express the IL-6 transgene (non-tg) are used as controls. The methods used to engineer the transgenic mice have been described previously (Campbell et al., 1993). Briefly, IL-6 expression in the CNS was targeted to astrocytes by an expression vector derived from the murine glial fibrillary acidic protein (GFAP) gene. Full-length murine IL-6 cDNA was modified and inserted into the GFAP gene. The genes were then microinjected into fertilized eggs of F1 generation hybrid mice (C57BL/6J X SJL). The IL-6 line has been maintained for many years on a C57BL/6J background and is congenic. The phenotypic characteristics of the mice have remained stable and are comparable to that originally described (Campbell et al., 1993; Chiang et al., 1994; Giralt et al., 2013).
Transgenic mice with astrocyte-targeted elevated expression of CCL2 (CCL2 tg) were also used for one set of experiments. Non-transgenic littermates (CCL2 non-tg) served as controls. Construction of the mice has been described previously (Huang et al., 2002). Briefly, the murine CCL2 gene was placed under control of the huGFAP promoter and purified GFAP-CCL2 fusion gene fragment was injected into fertilized eggs of SWXJ (H-21q,s) mice. The line was later backcrossed onto a C57BL/6J background and maintained for several years by breeding heterozygous CCL2-tg mice with wild-type C57BL/6J mice.
All animals were genotyped by PCR analysis of tail DNA using standard methods. All animal procedures were performed in accordance with the National Institutes of Health Guideline for the Care and Use of Laboratory Animals. Animal facilities and experimental protocols were in accordance with the Association for the Assessment and Accreditation of Laboratory Animal Care.
2.2. Slice preparation and electrophysiological recordings
Electrophysiological recordings of synaptic function at the Schaffer collateral to CA1 pyramidal neuron synapse of the hippocampus were performed in vitro as described previously (Nelson et al., 2012). Non-tg (n=54) and IL-6 tg (n=61) mice 3–5 months of age were used (mean age in months: 4.5±0.1 for non-tg, n=31; 4.5±0.1 for IL-6 tg, n=44). The mice were weighed, anesthetized with isoflurane, and decapitated. Brains were rapidly removed and immersed in ice-cold artificial cerebrospinal fluid (ACSF). The ACSF was gassed continuously with 95% O2/5% CO2 (pH 7.2–7.4) to maintain cell viability. The composition of the ACSF was (in mM): 130.0 NaCl, 3.5 KCl, 1.25 NaH2PO4, 24.0 NaHCO3, 2.0 CaCl2, 1.3 MgSO4, and 10.0 glucose (all chemicals from Sigma-Aldrich, St. Louis, MO, USA). After cooling, the hippocampus was removed from the brain, cut into 400 µm slices using a McIlwain tissue chopper (Mickle Laboratory Engineering Co. Ltd., Surrey, UK), and the slices placed in a gas-fluid interface holding chamber maintained at ~33°C until used. The chamber was superfused continuously with ACSF (33° C) at rate of 0.55 ml/min. Slices from the mid-region of the hippocampus were used for experiments.
For recordings, a hippocampal slice was transferred to a gas-fluid recording chamber and allowed to stabilize for 30–60 minutes. The recording chamber was continuously superfused with ACSF or ACSF plus ethanol (20 or 60 mM) at a rate of 2 ml/min (33°C). Only one concentration of ethanol was tested on each slice studied. A concentric bipolar stimulating electrode (FHC Inc., Bowdoin, ME, USA) was placed in the Schaffer collaterals at the border of the CA2 and CA1 regions of the hippocampus and synaptic transmission was elicited by brief electrical stimulation of the Schaffer collaterals (50 µs duration; S88 Square Pulse Stimulator and PSIU6 Stimulus Isolation Unit, Grass Technologies, West Warwick, RI, USA). The resulting synaptic responses were recorded extracellularly as field potentials. One recording microelectrode (1–3 MΩ) filled with ACSF was placed in the stratum radiatum (dendritic region) of the CA1 region to record the field excitatory postsynaptic potential (fEPSP) and a second recording microelectrode was placed in the stratum pyramidale (somatic region) of CA1 region to record the population spike (PS), which was elicited by the fEPSP. The signals were amplified with an Axoclamp-2A amplifier and acquired using the pClamp software (both from Molecular Devices, Union City, CA, USA).
2.3. Ethanol concentrations tested
Two pharmacologically relevant concentrations of ethanol were tested, 20 mM (92 mg/dl) and 60 mM (276 mg/dl). The ethanol solutions (in ACSF) were prepared 10–15 min prior to use from 95% ethanol (Remet Alcohols Inc., La Mirada, CA). In humans, a blood ethanol concentration of 80 mg/dl is considered an intoxicating dose of ethanol, whereas in heavy drinkers and alcoholics blood ethanol concentrations can exceed 300 mg/dl (Perper et al., 1986). These concentrations of ethanol cause cognitive dysfunction including memory impairments in humans and animal models and, in animal models, altered synaptic function in the hippocampus and other brain regions (reviewed in (Tipps et al., 2014; White, 2003; Zorumski et al., 2014)). Brain levels of ethanol have been shown to correspond to blood levels in animal models (Gilpin et al., 2009; Smolen and Smolen, 1989).
2.4. Assessment of synaptic function
The effect of ethanol on synaptic transmission in the IL-6 tg and non-tg hippocampal slices was determined by a comparison of input-output (I/O) relationships for the EPSP or PS under control conditions (ACSF superfusion) and after exposure to ACSF containing ethanol. I/O data were generated by applying a series of stimuli of increasing intensity to the Schaffer collaterals while recording the EPSP and PS. Stimulation, at rate of 0.05 Hz, was started at the threshold intensity required to elicit a fEPSP or PS and increased in steps (typically 10–20 µA steps from 20 to 240 µA) until the maximum fEPSP or PS was reached. Ethanol was applied to the hippocampal slices by superfusion (flow rate of 1.0 – 2.0 ml/min) after baseline control data were collected. I/O measurements in the presence of ethanol were made ~30 min after the start of ethanol superfusion and new half-max values for the fEPSP and PS were identified and used in all subsequent protocols. Superfusion of ethanol was continued for the duration of the experiment, which included studies of I/O relationships, and short- and long-term forms of synaptic plasticity. Control data for studies of long-term synaptic plasticity were provided by an additional series of experiments that were carried out in slices exposed to vehicle only (ACSF) using the same protocol as used for the ethanol studies.
The effect of ethanol on short-term synaptic plasticity of the fEPSP and PS was assessed using standard paired-pulse ratio (PPR) protocols. The test stimulus intensities used elicited a response (fEPSP or PS) was equal to 50% of the maximal response determined from I/O protocols. Three paired-pulse responses (1 minute between acquisitions) were averaged for PPR in each slice. Plasticity of the fEPSP was determined by a stimulation protocol applied at paired-pulse intervals of 40, 100, and 200 ms. Plasticity of the PS was assessed by a paired-pulse stimulation protocol at short intervals (10 and 20 ms). Longer forms of synaptic plasticity elicited by high frequency stimulation (HFS) were also examined under control conditions and in the presence of ethanol including post-tetanic potentiation (PTP), short-term potentiation (STP), and long-term potentiation (LTP) of the fEPSP slope. The HFS protocol consisted of 100 pulses for 1 sec (100 Hz) repeated a total of three times with a 20 sec interval between trains. A test stimulus intensity that elicited a fEPSP equal to 50% of the maximal fEPSP, as determined from I/O protocols, was used. A slice was considered to exhibit successful LTP if the slope of the fEPSP remained at an elevated level of ≥25% of baseline for ≥60 minutes following HFS.
2.5. Analysis of electrophysiological data
Data analyses were conducted off-line using AxoGraph software program (Axograph Scientific, axograph.com). For I/O data, the magnitude of the fEPSP was quantified by the slope of the initial rising phase of the negative deflection over the 40–60% range of the peak. The magnitude of the PS was measured as the peak amplitude of the negative deflection from a baseline value. Baseline value was estimated from a tangent line fitted across the two positive peaks of the synaptic response recorded in the somatic region. To construct I/O curves, mean values for fEPSP slope or PS amplitude were plotted as a function of stimulus intensity. Threshold stimulus intensity for the fEPSP or PS varied across slices for both the IL-6 tg and non-tg hippocampus under baseline conditions. Therefore, for data analysis the stimulus intensity that elicited a threshold fEPSP (e.g., slope of ~0.15 mV/ms) or PS (e.g., amplitude of ~0.70 mV) under baseline conditions was standardized, by setting the threshold stimulus intensity for the fEPSP or PS under baseline conditions to the same value for all slices (e.g., 70 µA for fEPSP, 100 µA for PS). To construct graphs reflecting the I/O relationships, stimulus intensities values were incremented (e.g. 10 or 20 µA intervals) from the standardized threshold value according to the increments used during the experiment. Stimulus intensities for I/O curves generated in the presence of ethanol were correlated to stimulus intensities for I/O curves generated under baseline conditions in the same slice to retain baseline/ethanol I/O relationships.
For statistical analyses of I/O data, the data were first normalized. This normalization adjusted for differences in the amplitude of the synaptic responses within a genotype under baseline conditions. For normalization, fEPSP or PS values in the presence of ethanol were divided by fEPSP or PS values under baseline conditions for the same stimulus intensity measured in the same slice (Wei et al., 2004). The normalized data were compared statistically using repeated measures ANOVA to identify significant genotypic effects. In addition, a mean value for the normalized fEPSP or PS collapsed across the stimulus intensity range (e.g., 100–200 µA) was calculated for each slice. The mean normalized values were compared statistically to identify significant within genotype effects of treatment (i.e., baseline vs. ethanol, one group t-test) and dose (i.e., 20 vs. 60 mM ethanol, unpaired t-test). For this and all other statistical comparisons, p<0.05 was taken to indicate a significant difference.
For studies of short-term plasticity assessed by paired-pulse stimulation protocols, PPRs were determined from the ratio of the magnitude of the response to the second stimulation divided by the magnitude of the response to the first stimulation for each paired-pulse interval. Mean PPRs were compared statistically by ANOVA or the paired t-test. For studies of long-term plasticity, LTP, PTP, and STP, the slope of the fEPSP was expressed as a percentage of the mean for five baseline (pre-HFS) fEPSP slopes. Mean PTP was determined for each slice by averaging the first 3 measurements after HSF. Mean STP was determined for each slice by averaging the measurements from 15–25 min after HSF. Mean LTP was determined for each slice by averaging measurements from 50–60 min after HSF. Mean values for PTP, STP and LTP in IL-6 tg and non-tg slices were compared statistically by ANOVA. Compiled data are expressed as the mean ± SEM. Both females and males were used for these studies. Results showed no consistent gender differences and data from males and females were combined. For electrophysiological studies n = number of slices studied (one slice/animal).
2.6. IL-6 and Signal transduction
The relative level of IL-6 and activation of signal transduction molecules utilized by IL-6 was determined by ELISA or Western blot, respectively, in control and ethanol exposed hippocampal slices. Both the left and right hippocampi were obtained from the brain of each animal and cut into 400 µm slices following the same protocol as used for electrophysiological recordings. Approximately 6 slices were obtained from each hippocampus. The slices were pooled according to the hippocampus from which they were obtained. One set of hippocampal slices from each animal served as the control sample and the second set was used for ethanol treatment. The source (i.e., left or right hippocampus) for the control and ethanol samples was reversed in different experiments. The slices were placed in two recording chambers maintained at ~33°C and were continuously superfused with oxygenated ACSF at rate of 1 ml/min. The slices were incubated for 30–60 minutes to allow them to recover, and then one set of slices was superfused with 60 mM ethanol for 30 min and the second set of slices was superfused with ACSF. After 30 min, control and ethanol-treated slice sets were transferred to eppendorf tubes, snap frozen and stored at −80°C.
Protein samples for ELISA or Western blot were prepared from the IL-6 tg and non-tg hippocampal slices following protocols described previously (Gruol et al., 2014; Nelson et al., 2012). Proteins were extracted from the hippocampal samples by sonication in cold lysis buffer containing 50 mM Tris-HCl, pH 7.5, 150 mM NaCl, 2 mM EDTA, 1% Triton X-100, 0.5% NP-40, a Complete Protease Inhibitor Cocktail Tablet (Roche Diagnostics, Mannheim, Germany), and a cocktail of phosphatase inhibitors (Na+ pyrophosphate, β-glycerophosphate, NaF, Na+ orthovanadate; all from Sigma-Aldrich). The samples were incubated on ice for 30 minutes, centrifuged at 13,860g for 30 minutes at 4°C, and the supernatants were collected. Protein concentration in the supernatants was determined using the Bio-Rad Protein Assay Kit (Bio-Rad, Hercules, CA). Protein aliquots were stored at −80°C.
IL-6 levels in protein samples were determined by ELISA using the Mouse IL-6 ELISA Ready-SET-Go! Kit (eBioscience, Inc., San Diego, CA). Levels of other proteins were determined by Western blot. For Western blot, equal amounts of protein samples (25 µg) were subjected to SDS-PAGE using 4–12% Novex NuPAGE Bis-Tris gels (Invitrogen Life Technologies, Grand Island, NY). IL-6 tg and non-tg protein samples were run on the same gel. Samples were run in duplicate. Proteins were transferred to Immobilon-P membranes (Millipore, Billerica, MA) and uniform transfer was assessed by Ponceau S staining (Pierce, Rockford, IL). Membranes were washed and blocked in a 5% casein solution (Pierce) and then incubated in primary antibody overnight (4°C). After washing, the membranes were incubated (room temperature) in secondary antibody coupled to horseradish peroxidase (HRP). Protein bands were visualized by chemiluminescence and quantified by densitometry measurements using NIH Image software (http://rsb.info.nih.gov/nih-image/). Membranes were stripped and reprobed for β-actin. To adjust for possible loading errors, the density of each band was normalized to the density of the band for β-actin in the same lane. Normalized data from IL-6 tg slices were then normalized to the average normalized value for non-tg slices run on the same gel. Data were combined according to genotype and treatment and reported as mean ± SEM.
The following antibodies were used for Western blot studies: a monoclonal antibody to β-actin (#AC-15, 1:5000; Sigma, St. Louis, Missouri); a rabbit polyclonal antibody raised against p42/p44 mitogen-activated protein kinase (MAPK) (#61-7400; 1:5000, Zymed, Carlsbad, CA, USA); a purified rabbit polyclonal antibody raised against a synthetic phospho-peptide (KLH-coupled) corresponding to residues around Thr202/Tyr204 of human p42/p44 MAPK (#9101; 1:500; Cell Signaling Technologies, Danvers, MA; pp42/44 MAPK); a purified rabbit polyclonal antibody raised against a synthetic peptide (KLH-coupled) corresponding to the sequence of mouse signal transducer and activator of transcription 3 (STAT3) (AB#9132; 1:1000; Cell Signaling Technologies), a purified rabbit polyclonal antibody raised against a synthetic phospho-peptide (KLH-coupled) corresponding to the residues surrounding Tyr705 of mouse STAT3 (AB#9131; 1:1000; Cell Signaling Technologies).
2.7. Behavioral studies of acute ethanol withdrawal hyperexcitability
The ability of a single high dose of ethanol to induce a hyperexcitable state during the period of declining blood ethanol levels was assessed by scoring handling-induced convulsions and by recording the electroencephalograph activity. Male IL-6 tg and non-tg mice were used for these studies. n = number of animals tested. Compiled data are expressed as the mean ± SEM.
Ethanol treatment
All animals were ethanol naive before acute ethanol administration. A standard protocol for ethanol exposure was used, which involves a single i.p. injection of 4 g/kg ethanol (20%w/v in 0.9% saline) administered to mice two hours into the dark phase of the circadian rhythm. This protocol has been shown to increase CNS excitability during the period of declining ethanol levels following the acute high dose of ethanol (Crabbe, 1998; Crabbe et al., 1983; McQuarrie and Fingl, 1958; Roberts et al., 1992).
Recovery of righting reflex and blood ethanol levels
Potential differences in the pharmacokinetics of ethanol between IL-6 tg and non-tg mice were assessed by measurements of recovery of righting reflex and blood ethanol levels. The time to recovery of righting reflex reflects the sedative effects of ethanol and total sleeping time for each animal. Righting reflex was assessed by placing the animal on its back after the ethanol administered and recording the duration (in minutes) before it righted itself (all 4 paws touching the floor). Retro-orbital blood samples (50 µl) to determine blood ethanol levels were taken at the time of recovery of righting reflex. Plasma (5 µl) was used for blood ethanol measurement using an Analox GM 7 analyzer (Analox Instruments LTD, Lunenberg, MA). The reaction is based on the oxidation of ethanol by alcohol oxidase in the presence of molecular oxygen (ethanol + O2 → acetaldehyde +H2O2). The rate of oxygen consumption is directly proportional to the ethanol concentration. Single point calibrations are done for each set of samples with reagents provided by Analox Instruments (0.025–0.400 g%). A statistically significant difference was determined by the unpaired t-test.
Handling-induced Convulsions (HIC)
HIC were quantified using a scale developed by Goldstein and Pal (Goldstein and Pal, 1971), which is used extensively in the field (e.g., (Crabbe et al., 1980; Farook et al., 2008; Finn et al., 2007; Ghozland et al., 2005; Metten et al., 2010; Olive and Becker, 2008)). Briefly, this procedure involves lifting the mouse by the tail and observing it for possible convulsions. If none occur, the mouse is gently spun 180 degrees by rubbing the tail between the thumb and forefinger. Convulsions are scored on a 6 point scale ranging from facial grimace to severe tonic-clonic convulsions (higher numbers reflect more severe behavioral signs). Baseline HIC was assessed prior to ethanol injection. Mice were scored for HIC at 2, 4, 6, 8, 12 and 24 hours following ethanol administration by a single experimenter blind to the animals’ experimental history. A statistically significant genotypic difference was determined by repeated measures ANOVA).
Electroencephalogram (EEG)
EEG activity was measured in a separate cohort of animals before and after 4 g/kg ethanol administration (i.p.) to assess more quantitatively neuronal activity changes across the same time course used in HIC studies. EEG analysis was performed as previously described (Hedlund et al., 2005; Huitron-Resendiz et al., 2005; Huitron-Resendiz et al., 2004). EEG data were recorded from stainless steel screw electrodes implanted on the frontal and parietal bone over the hippocampus (coordinates: 2.0 mm posterior and 2.0 mm lateral to bregma according to The Mouse Brain in Stereotaxic Coordinates from Franklin and Paxinos, 1997) (Franklin and Paxinos, 1997). A fourth EEG electrode was implanted over the cerebellum and used to ground the animal to reduce signal artifacts. Insulated leads from the EEG electrodes were crimped to male pins (220-P02) and then cemented to the skull with dental acrylic. Following surgical implantation under general anesthesia (1–1.5% isoflurane), mice were allowed 2 weeks to recover prior to the study.
To record EEG, mice were connected to commutators (PlasticOne) with flexible recording cables allowing their unrestricted movements within the cage and habituated to the recording cages for 24h. Ethanol was administered as in HIC tests (4 g/kg, i.p.) and the EEG was recorded for an additional 12 hr. Electomyograph (EMG) signals were also recorded. EEG and EMG signals were amplified in a Grass Model 7D polygraph in a frequency range of 0.3 to 10 KHz. The EEG and EMG are displayed on a computer monitor and stored with a resolution of 128 Hz in the hard drive of a computer for the off-line spectral analysis and investigation of possible seizure activity using software supplied by Kissei Comptec. EEG power, a measure of EEG amplitude as a function of frequency (microvolts squared per Hz), was analyzed using 4-second epochs at delta (0.5–4.0 Hz), theta (4–9 Hz), alpha (6–12 Hz) and gamma (30–45 Hz and 45-1-100 Hz) frequencies. At some time points, records were inspected using 15-second epochs to obtain the total time spent in wakefulness, slow wave sleep (SWS) and rapid eye movement (REM) sleep. A statistically significant genotypic difference was determined by repeated measures ANOVA.
3. Results
3.1. Acute ethanol reduces synaptic responses in non-tg but not IL-6 tg hippocampal slices
To determine if the effect of acute ethanol on synaptic responses was altered in the IL-6-tg hippocampus, I/O relationships for the fEPSP (Fig. 1) and PS (Fig. 2) elicited by Schaffer collateral stimulation were studied in the CA1 region of IL-6-tg and non-tg hippocampal slices. Measurements of I/O relationships were made under baseline control conditions and in the presence of ethanol. Analysis involved a within slice comparison after normalization of the I/O data. For comparisons within a genotype, mean normalized data (collapsed across stimulus intensity) were used.
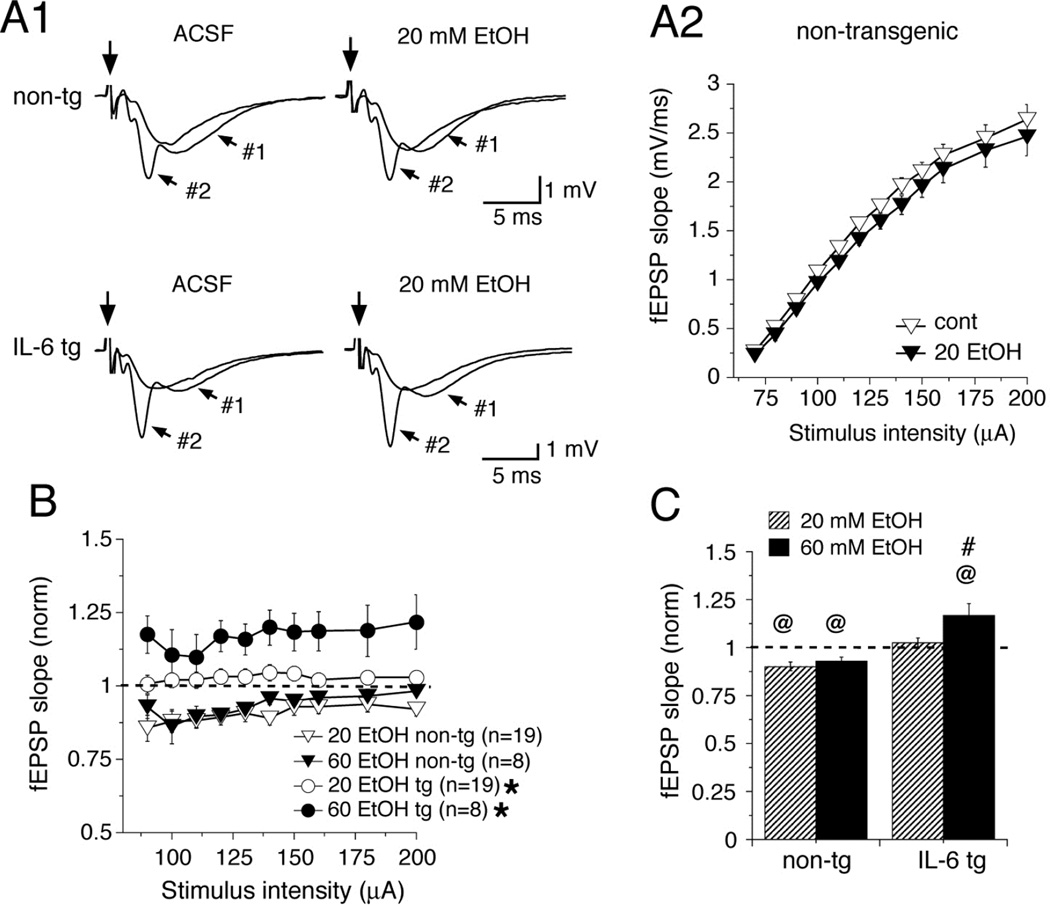
Figure 1.
Ethanol differently altered the slope of the fEPSP in hippocampal slices from IL-6 tg vs. non-tg mice. (A1) Representative traces of the fEPSP before and after acute application of 20 mM ethanol (EtOH) in non-tg and IL-6 tg (hippocampal slices. For each genotype and treatment, two traces are overlaid showing fEPSP at low intensity (#1) and high intensity (#2) stimulation (applied at the arrow) within the respective I/O protocol. (A2) Representative graph showing I/O relationships for fEPSP slopes (mean ±SEM) over the range of stimulus intensities tested in non-tg hippocampal slices before (open symbols) and after (filled symbols) application of 20 mM ethanol. (B) Graph showing mean (±SEM) normalized values (ethanol/baseline) for fEPSP slopes at various stimulus intensities from 80 to 200 µA for non-tg (triangle) and IL-6 tg (circle) slices exposed to 20 mM (open symbols) or 60 mM (closed symbols) ethanol. Dashed line indicates control values (i.e., 1) for IL-6 tg and non-tg slices. (C) Mean (±SEM) values for normalized fEPSP slopes averaged on an individual slice basis over the range of stimulus intensities used for studies of 20 mM (stripped bar) and 60 mM (solid bar) ethanol in non-tg and IL-6 tg hippocampal slices. Dashed line indicates control values (i.e., 1) for IL-6 tg and non-tg slices. In non-tg slices, 20 mM and 60 mM ethanol significantly depressed the fEPSP slope. In the IL-6 tg slices, 20 ethanol had no effect on the fEPSP slope, whereas 60 mM ethanol enhanced the fEPSP slope. *Significant difference between IL-6 tg and non-tg slices for the same ethanol concentration (Repeated measures ANOVA, p<0.05). @Significant difference from baseline values (i.e., 1) for the same genotype (one sample t-test, p<0.05). #Significant difference between 20 mM vs. 60 mM ethanol for the same genotype (unpaired t-test, p<0.05).
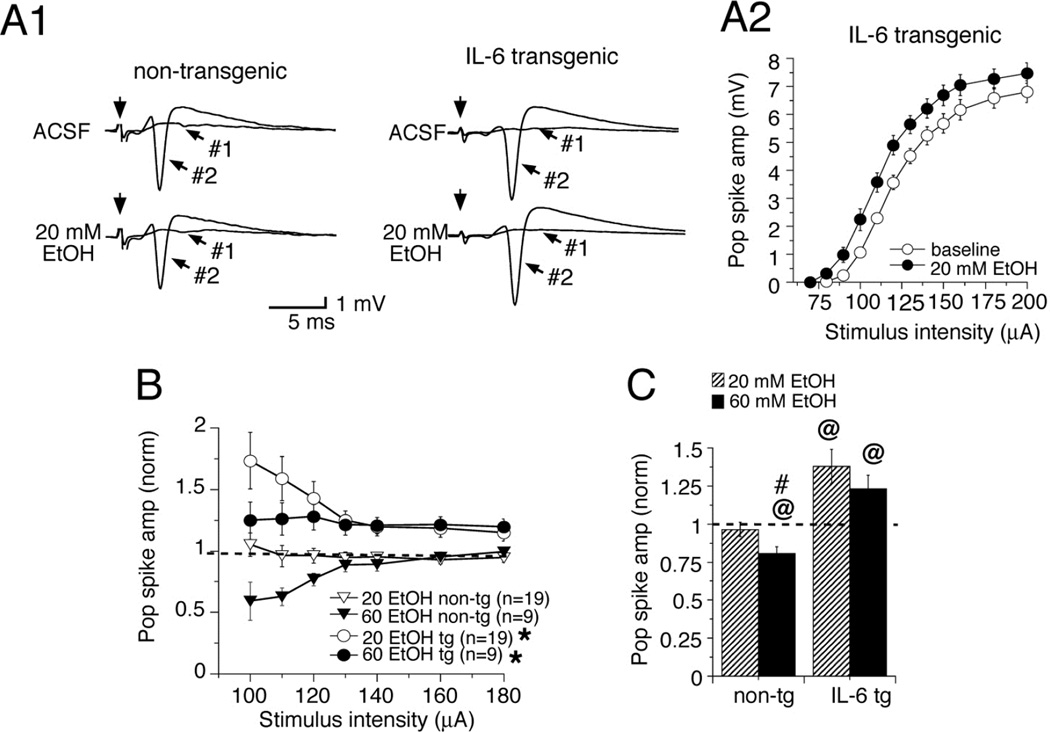
Figure 2.
Ethanol depresses the PS in non-tg hippocampal slices but enhances the PS in IL-6 hippocampal slices. (A1) Representative traces of PS evoked by Schaffer collateral stimulation (applied at the arrow) before and after acute application of 20 mM ethanol (EtOH) in non-tg and IL-6 tg slices. (A2) Representative graph showing I/O relationships for PS amplitudes mean (±SEM) over the range of stimulus intensities tested in IL-6 tg slices before ethanol (open symbols) and after ethanol (filled symbols) application of 20 mM ethanol. (B) Graph showing normalized (ethanol/control) values (mean±SEM) for PS amplitudes for the range of stimulus intensities studied (100 to 180 µA) for non-tg and IL-6 tg slices. Dashed line indicates control values (i.e., 1) for IL-6 tg and non-tg slices. (C) Mean normalized values (±SEM) for PS amplitudes averaged on an individual slice basis over the range of stimulus intensities used for studies of 20 (stripped bar) and 60 mM (solid bar) ethanol. Dashed line indicates control values (i.e., 1) for IL-6 tg and non-tg slices. Ethanol significantly depressed the PS amplitude in non-tg slices at 60 mM ethanol but not 20 mM ethanol, whereas the PS amplitude in IL-6 tg slices was increased by both 20 mM and 60 mM ethanol. *Significant difference between IL-6 tg and non-tg slices for the same ethanol concentration (Repeated measures ANOVA, p<0.05). @Significant difference from baseline values (i.e., 1) for the same genotype (one sample t-test, p<0.05). #Significant difference between 20 mM and 60 mM ethanol for the same genotype (unpaired t-test, p<0.05).
Results showed a significant genotypic difference (repeated-measures ANOVA) in the normalized fEPSP slopes for both 20 mM (F(1,36) = 15.02, p = 0.0004) and 60 mM ethanol (F(1,14) = 13.996, p = 0.0022), with ethanol producing a depression of the fEPSP slope in the non-tg slices, and an enhancement of the fEPSP slope in the IL-6 tg slices (Fig. 1A,B). Analysis of mean normalized data showed that the small depressions of the fEPSP slope produced by both 20 mM (~10%) and 60 mM (~7%) ethanol in the non-tg slices were significantly different from the respective baseline control values (i.e., 1; one group t-test, 20 mM, p = 0.0004; 60 mM, p = 0.0076) (Fig. 1C). The depressions of the fEPSP slope produced by 20 mM and 60 mM ethanol were not significantly different in the non-tg slices (p = 0.43, unpaired t-test), perhaps because the effect was maximal at 20 mM (Fig. 1C). In contrast, in the IL-6 tg slices 20 mM ethanol did not significantly alter the fEPSP slopes relative to control values (i.e., 1; p = 0.26, one group t-test), while 60 mM ethanol significantly increased (~17%) the fEPSP slopes relative to control values (p = 0.028, one group t-test)(Fig. 1C). The effects of 20 mM and 60 mM ethanol on the fEPSP slopes were significantly different in the IL-6 tg slices (p = 0.013, unpaired t-test) (Fig. 1C).
A significant genotypic difference (repeated measures ANOVA) was also observed for the effect of 20 mM (F(1,36) = 11.91, p = 0.0014) and 60 mM (F(1,16) = 18.29, p = 0.0006) ethanol on the normalized PS amplitude, with ethanol producing a depression of the PS in the non-tg slices and an enhancement of the PS in the IL-6 tg slices (Fig. 2A,B). Analysis of mean normalized data showed that in the non-tg slices, 20 mM ethanol did not significantly alter PS amplitude (~3% depression, p = 0.46, one group t-test) relative to control values (i.e., 1), whereas 60 mM ethanol produced a significant depression (~20%, p = 0.003, one group t-test) (Fig. 2C). The effects of 60 mM vs. 20 mM ethanol on the PS amplitude were significantly different in the non-tg slices (p = 0.042, unpaired t-test)(Fig. 2C). In contrast, in the IL-6 tg slices ethanol significantly enhanced the PS amplitude relative to control values (i.e., 1) at both 20 mM (p = 0.003, one group t-test) and 60 mM (p = 0.03, one group t-test) (Fig. 2C). The enhancement of the PS amplitude produced by 20 mM (~38%) and 60 mM (~23%) ethanol were not significantly different in the IL-6-tg slices (p = 0.41, unpaired t-test) (Fig. 2C). Thus, the depressive effect of acute ethanol on hippocampal synaptic responses in the non-tg slices was transform into an enhancement in the IL-6 tg slices.
3.2. Effects of ethanol on synaptic plasticity are altered in the IL-6 tg hippocampus
Experience-dependent changes in synaptic transmission, referred to as synaptic plasticity, play an important role in hippocampal functions such as learning and memory, and are known to be altered by ethanol (reviewed in (McCool, 2011; Zorumski et al., 2014)). Such changes can be identified experimentally by alterations in the magnitude of synaptic responses elicited by specific paired-pulse or high frequency stimulation protocols. Synaptic plasticity elicited by paired-pulse stimulation was determined using a standard protocol and quantified by the PPR. In both IL-6 tg and non-tg hippocampal slices, PPR of the fEPSP slope was greater than 1 (mean PPRs ~ 1.8 to 1.3) at all paired-pulse intervals tested (40, 100 and 200 ms) under both baseline and ethanol conditions, indicating paired-pulse facilitation (PPF). PPF is thought to result from an increased probability of transmitter release from presynaptic terminals (Zucker and Regehr, 2002). PPF was comparable in the IL-6 tg and non-tg slices in the presence and absence of 20 mM or 60 mM ethanol (not shown), indicating a lack of effect of ethanol or genotype on this form of synaptic plasticity.
A second form of plasticity assessed by paired-pulse stimulation (at 10 or 20 ms interpulse interval) is measured in the somatic region and reflects the level of excitability of the somatic region (Fig. 3). Excitability in the somatic region is a function of the actions of somatic/dendritic ion channels that mediate excitability in combination with the effects of recurrent GABAergic inhibitory synaptic transmission in the vicinity of the pyramidal cell layer. In our studies, PPR of the PS under baseline conditions was ≥1 for some hippocampal slices from both the IL-6 tg and non-tg mice, indicating no effect or a facilitation of the PS by paired-pulse stimulation in these slice (Fig. 3B). These data imply that inhibitory influences, which would produce inhibition of the second PS of the pair (i.e., PPR<1), were not prominent in those IL-6 tg and non-tg slices. However, genotypic differences in the effect of ethanol on PPR of the PS were independent of whether or not PPR of the PS showed inhibition or facilitation under baseline conditions. Facilitation vs. inhibition for the PPR of the PS presumably results from the angle at which the slices were cut, although regional differences in level of synaptic inhibition in the hippocampus could also contribute (Papatheodoropoulos et al., 2002; Petrides et al., 2007).
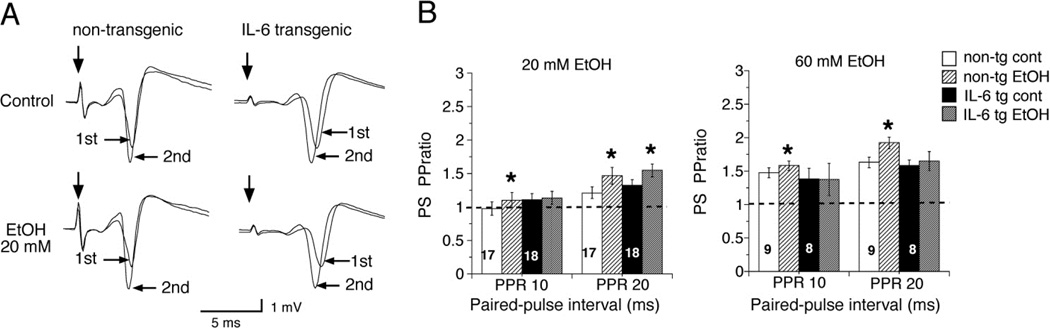
Figure 3.
The PPR for the PS amplitude showed genotypic differences. (A) Representative traces show PS evoked by 20 ms interval paired stimulation in non-tg and IL-6 tg hippocampal slices under control conditions and in the presence of 20 mM ethanol. (B) Graph shows mean values for the PS PPR for 10 and 20 ms paired pulse intervals under control conditions and in the presence of ethanol. Dashed line indicates control values (i.e., 1) for IL-6 tg and non-tg slices. In the non-tg hippocampal slices, 20 mM and 60 mM ethanol produced a small but significant increase in the PS PPR at 10 and 20 ms stimulus intervals. In the IL-6 tg hippocampal slices, 20 mM ethanol increased the PS PPR but only at the 20 ms stimulus interval, whereas 60 mM ethanol did not alter the PS PPR. 1st = response to first stimulus of the paired stimulation; 2nd = response to the second stimulus of the paired stimulation. *Significantly different from control PS PPR of the same genotype (paired t-test, p<0.05)
Exposure to both 20 mM and 60 mM ethanol produced a significant increase in the PPR for the PS in the non-tg slices at both the 10 and 20 ms paired-pulse intervals, indicating ethanol produced increased excitability during repetitive stimulation (Fig. 3). 20 mM ethanol also increased the PPR for the PS in the IL-6 tg slices, but only at the 20 ms paired-pulse interval (Fig. 3). There was no effect of 60 mM ethanol on PPR for the PS at either at 10 ms or 20 ms paired-pulse intervals in the IL-6 tg slices (Fig. 3B). Thus, ethanol consistently enhanced PPR of the PS in the non-tg slices, whereas the IL-6 tg slices were more resistant to this ethanol effect.
We also examined the effect of ethanol on long-term synaptic plasticity of the fEPSP induced by HFS of the Schaffer collaterals. HFS produced a prolonged increase in the fEPSP slope in both IL-6 tg and non-tg slices characterized by an initial peak (i.e., PTP) that occurred immediately after the termination of the HFS protocol and lasted for 2–3 min, a subsequent declining phase of the fEPSP slope that lasted ~30 min (i.e., STP), followed by a stable, enhancement of the fEPSP slope that lasted up to 60 min following the induction protocol (i.e., LTP) (Fig. 4). PTP is thought to result from a presynaptic enhancement of synaptic vesicle release from the reserve pool that lasts for seconds to minutes after HFS (Zucker, 1996). Both presynaptic and postsynaptic mechanisms appear to be involved in STP (Erickson et al., 2010; Lauri et al., 2007), which is thought to play a role in short-term memory (Erickson et al., 2010). LTP primarily results from increased membrane expression of AMPA receptors and is considered to be an important cellular model for memory and learning (Miyamoto, 2006; Peng et al., 2011).
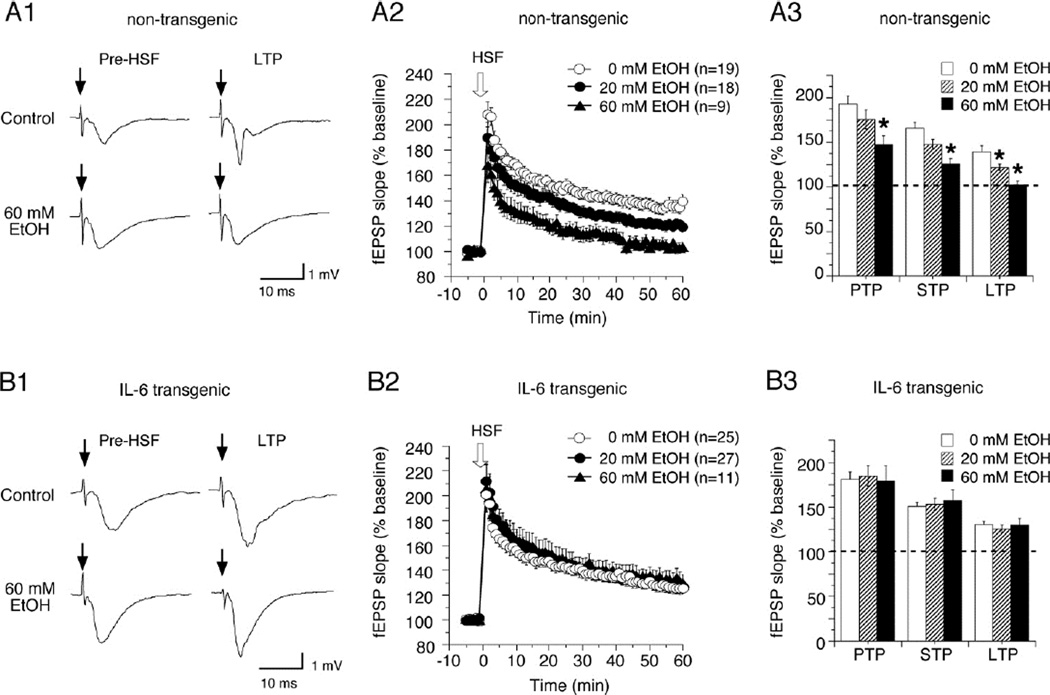
Figure 4.
Ethanol significantly depressed long-term synaptic plasticity of the fEPSP in the non-tg hippocampal slices but not in the IL-6 tg hippocampal slices. (A1,B1) Representative traces of fEPSPs evoked by Schaffer collateral stimulation (at the arrow) from non-tg (A1) and IL-6 tg (B1) hippocampal slices before HSF was applied and 60 min after HFS, when LTP was established, under control conditions (0 mM EtOH) and in the presence of 60 mM ethanol. (A2,B2). Graphs show mean values for the fEPSP slopes during the LTP experiments in non-tg (A2) and IL-6 tg (B2) hippocampal slices under control conditions and in the presence of 20 or 60 mM ethanol. fEPSP slopes are expressed as a percentage of mean baseline fEPSP slope prior to HSF. HSF was delivered at the arrow. (A3,B3) Mean values for PTP, STP and LTP in the non-tg (A3) and IL-6 tg (B3) hippocampal slices under control conditions and in the presence of ethanol. Mean PTP was determined for each slice by averaging the first 3 measurements after HSF. Mean STP was determined for each slice by averaging the measurements from 15–25 min after HSF. Mean LTP was determined for each slice by averaging measurements from 50–60 min after HSF. *Significantly different from 0 ethanol values (ANOVA followed by Fisher’s PLSD, p<0.05).
Under control conditions (ACSF superfusion), the increase in the fEPSP slope induced by HFS was similar for IL-6 tg and non-tg slices for time periods that reflect PTP, STP and LTP. In non-tg slices, exposure to acute ethanol (20 mM and 60 mM) significantly reduced LTP in a dose-dependent manner (Fig. 4A), as expected based on previous studies of ethanol actions on synaptic plasticity (reviewed in (McCool, 2011; Zorumski et al., 2014)). For example, 60 mM ethanol completely blocked LTP in the non-tg slices, consistent with studies by others (Ramachandran et al., 2015). Exposure to 60 mM ethanol also significantly reduced PTP (~45%) and STP (~40%) in the non-tg slices (Fig. 4A2,3). In contrast, these concentrations of ethanol had no effect on LTP, PTP or STP in the IL-6 tg slices (Fig. 4B). Thus, in the IL-6 tg slices several forms of synaptic plasticity mediated by presynaptic or postsynaptic mechanisms showed a resistance to the effects of ethanol. Results from these electrophysiological studies are summarized in Table 1, and support the proposal that increased expression of astrocyte produced IL-6 can lead to altered effects of ethanol on synaptic function.
Table 1.
Summary of effects of ethanol on electrophysiological properties.
| Parameter measured |
Non-tg | IL-6 tg | ||
|---|---|---|---|---|
| 20 mM EtOH | 60 mM EtOH | 20 mM EtOH | 60 mM EtOH | |
| fEPSP slope | ↓ | ↓ | no Δ | ↑ |
| PS | no Δ | ↓ | ↑ | ↑ |
| PPF | no Δ | no Δ | no Δ | no Δ |
| PPR | ↑ | ↑ | ↑ | no Δ |
| PTP | no Δ | ↓ | no Δ | no Δ |
| STP | no Δ | ↓ | no Δ | no Δ |
| LTP | ↓ | ↓ | no Δ | no Δ |
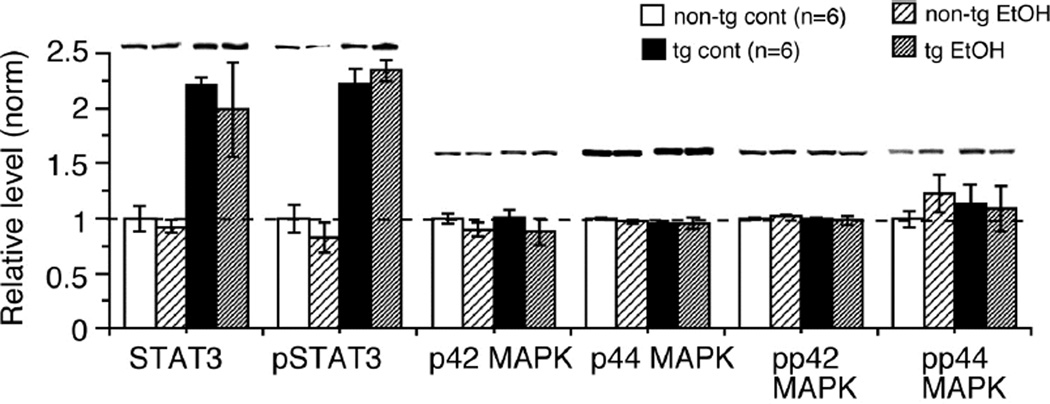
3.3. Acute ethanol does not result in STAT3 or p42/44 MAPK activation
Acute ethanol (4 g/kg, i.p.) has been reported to increase (~350%) IL-6 mRNA in the hippocampus of rats when measured 3–9 hrs post ethanol administration (earlier times not measured) (Doremus-Fitzwater et al., 2014). Acute ethanol (100 mM, 24 hour treatment) has also been reported to induce secretion of IL-6 (~ 5 fold) from rat cortical astrocytes in primary cultures, from ~ 50 pg/mg cell protein under control conditions to ~ 250 pg/mg cell protein (Sarc et al., 2011). These data raised the possibility that ethanol exposure of the hippocampal slices induced IL-6 (i.e., acute IL-6) production by astrocytes or other cell types, in which case differences in effects of the acute IL-6 could contribute to the observed genotypic differences in the effects of ethanol on synaptic function reported above. The acute IL-6 would presumably activate IL-6Rs on nearby cells and cause functional changes through downstream signaling. IL-6Rs are expressed on several cell types in the hippocampus, including neurons and glia (Gruol, 2014). To assess this possibility we carried out two types of experiment: (a) we measured by ELISA the levels of IL-6 in a separate group of IL-6 tg and non-tg hippocampal slices treated with control saline (ACSF) or 60 mM ethanol for 30 min, and (b) we measured the relative level of activation of downstream signal transduction molecules activated by IL-6.
As reported previously, levels of IL-6 in slices studied in vitro were higher than in samples from whole hippocampus immediately snap frozen after dissection (Gruol et al., 2014). In addition, levels of activated p42/44 MAPK were not higher in the IL-6 tg slices compared with the non-tg slices, as was observed for the samples from whole hippocampus (Nelson et al., 2012). These differences could result from the in vitro protocol used to prepare the slices (Jankowsky et al., 2000). To adjust for potential effects of the in vitro protocol on IL-6 levels in the slices and potential differences in the levels of IL-6 across animals of the same genotype, IL-6 levels in ethanol-treated slices were normalized to IL-6 levels in control slices obtained from the same animal and exposed to ACSF rather than ethanol. IL-6 levels varied across the slices for both IL-6 tg and non-tg slices, ranging from 12–80 pg/ml for both IL-6 tg and non-tg slices under control conditions. Normalization (ethanol/control) showed that in the non-tg slices, ethanol exposure significantly increased (one sample t-test) IL-6 levels by approximately 50% (mean normalized value = 1.50±0.11, n=3) compared to non-tg slices exposed to control saline. A similar increase was produced by ethanol in the IL-6 tg slices (mean normalized value = 1.49±0.09, n=3) compared to IL-6 tg slices exposed to control saline. These results are consistent with studies showing that ethanol causes an increase in IL-6 levels in CNS cells.
IL-6 produces its biological effects through several different signal transduction pathways linked to IL-6R, the primary pathway being STAT3 but also p42/44 MAPK. Measurement of the activated forms of these proteins (i.e., phosphorylated forms; pSTAT3, pp42/44 MAPK) in hippocampal slices exposed to control saline or ethanol (60 mM) for 30 min showed no significant effect of ethanol in either the non-tg or IL-6 tg slices (Fig. 5). These results make it unlikely that the differences in the effects of ethanol on synaptic function between IL-6 tg and non-tg hippocampal slices are due to differences in the actions of ethanol-induced acute IL-6 production between the IL-6 tg and non-tg hippocampus. However, the potential involvement of other ethanol-induced factors in the differential effects of ethanol in IL-6 tg and non-tg hippocampus cannot be eliminated at this time.
Figure 5.
Level of activation of signal transduction molecules associated with IL-6R activation was not altered by acute exposure of hippocampal slices to ethanol (60 mM, 30 min). Graph shows mean (±SEM) values for the relative level of the activated form and total (activated plus non-activated) STAT3 and p42/44 MAPK measured by Western blot in non-tg and IL-6 tg hippocampal slices. For each gel, measurements were normalized to the mean value for the non-tg hippocampus run on the same gel. Normalized values were then averaged according to genotype and protein. Representative Western blots are shown above the corresponding bars in the graph. Six slices were studied for each condition. Dotted line shows mean values for non-tg hippocampal slices (i.e., 1).
3.4. Ethanol withdrawal hyperexcitability is enhanced in the IL-6 tg mice
The enhanced synaptic responses in the IL-6 tg hippocampal slices produced by acute ethanol and the increased susceptibility of the IL-6 tg mice to seizure activity (Campbell et al., 1993; Sallmann et al., 2000), raised the possibility that IL-6 tg mice may be more susceptible to ethanol-induced withdrawal symptoms such as hyperexcitability than the non-tg mice. To test this possibility, we examined the behavioral effects of a single exposure to a high dose (4 g/kg, i.p.) of ethanol, an ethanol exposure protocol that can produce a mild state of ethanol dependence that increases susceptibility to a hyperexcitable state as blood ethanol levels decline toward zero. We used both the HIC test (Crabbe et al., 1991) and EEG recordings, which provided more quantitative data, to assess the effects of ethanol exposure/withdrawal on CNS activity in the IL-6 tg and non-tg mice. A high dose of ethanol (4 g/kg, i.p.) has been associated with increased seizure thresholds 8 hrs following ethanol injection (McQuarrie and Fingl, 1958) and increased HIC, albeit mild, in C57BL/6J mice 6–12 hr following ethanol injection (Crabbe, 1998; Crabbe et al., 1983; Roberts et al., 1992). A high dose of ethanol (4 g/kg, i.p.) has also been shown to produce elevated levels of IL-6 mRNA (~100 % increase) in the hippocampus at 3–9 hrs following ethanol injection (Doremus-Fitzwater et al., 2014).
Pharmacokinetics
Administration of the high dose of ethanol (4.0 g/kg, i.p.) caused a period of sedation in both the IL-6 tg and non-tg mice characterized by a loss of righting reflex. Time to recovery of righting reflex was similar (unpaired t-test) for the IL-6 tg and non-tg mice (IL-6 tg = 107±17 min, n=8; non-tg = 94±12 min, n=13). Blood ethanol levels were also similar (unpaired t-test) for the IL-6 tg (408±10 mg/dl, n=7) and non-tg (411±10, n=9) mice. These measures indicate that the pharmacokinetics of ethanol, which could influence results, were comparable in the IL-6 tg and non-tg mice. Blood ethanol levels were estimated to return to zero approximately 8–12 hours after ethanol administration.
HIC
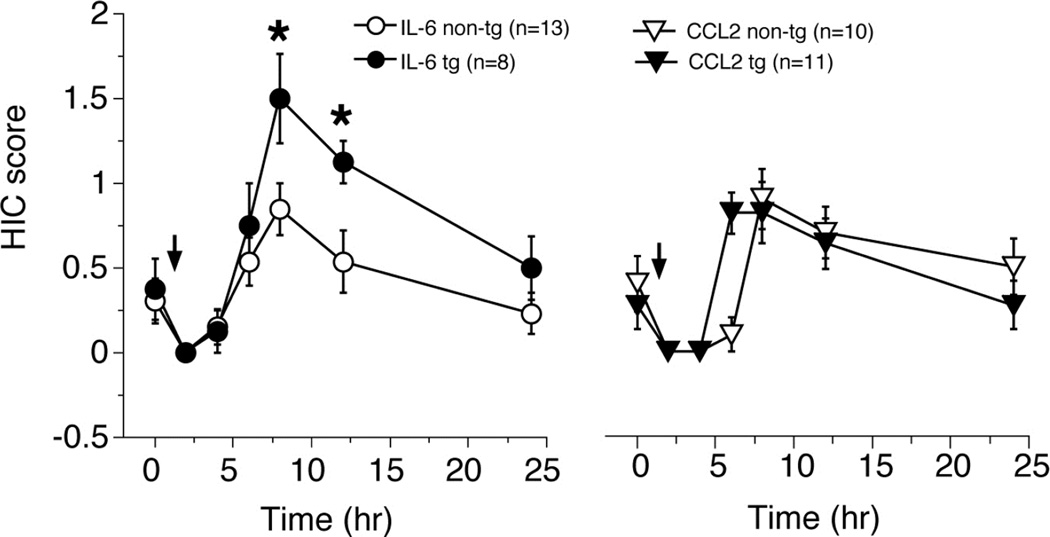
IL-6 tg and non-tg mice were scored for HIC during a baseline period and at 2, 4, 6, 8, 12 and 24 hours following administration of a single high dose of ethanol (4.0 g/kg, i.p.). HIC scores at baseline prior to ethanol administration were not significantly different for IL-6 tg and non-tg mice (unpaired t-test). HIC scores following ethanol administration were modestly increased for both the IL-6 tg and non-tg mice (Fig. 6). The increases at 6–24 hrs were significantly larger for IL-6 tg than the non-tg mice (repeated measures ANOVA, F(1,19) = 4.928, p = 0.038), indicating a higher level of CNS activity in the IL-6 tg mice. A significant increase (unpaired t-test) above baseline occurred at the 8 and 12 hrs in IL-6 tg mice, but only at 8 hrs in the non-tg mice (Fig. 6), consistent with a higher level of CNS activity in the IL-6 tg mice.
Figure 6.
IL-6 tg mice showed a higher level of CNS excitability during withdrawal from acute ethanol as measured by HIC assay. Graph showing mean values (±SEM) for HIC scores measured over a 24 hr period in IL-6 tg (closed circles) and non-tg (open circles) mice and CCL2 tg (closed triangle) and CCL2-non-tg (open triangle) mice. Mice were given a high dose of ethanol (4 gm/kg, i.p.) and tested at several different time points. The IL-6 tg mice showed significantly higher peak HIC scores than their non-tg littermates. No genotypic difference was observed for the CCL2 tg and non-tg mice. Baseline HIC scores were similar for all genotypes, as were the scores for initial time points (2,4, and 6 hr) following ethanol administration (arrow). *Significantly different from non-tg mice (Repeated measure ANOVA with post hoc Fisher’s PLSD, p<0.05). @Significantly different from baseline values for the same genotype (paired t-test, p<0.05).
We also measured HIC in similar studies of CCL2 transgenic (CCL2 tg) mice and their non-transgenic littermate control (CCL2 non-tg) mice. Like the IL-6 tg mice, the CCL2 tg mice express elevated levels of CCL2 through increased astrocyte expression. The CCL2 tg and non-tg mice showed no genotypic difference in the effects of a single high dose of ethanol (4.0 g/kg, i.p.) on HIC scores (Fig. 6). These results indicate specificity for the effects of IL-6 on ethanol-induced CNS activity during ethanol withdrawal.
EEG
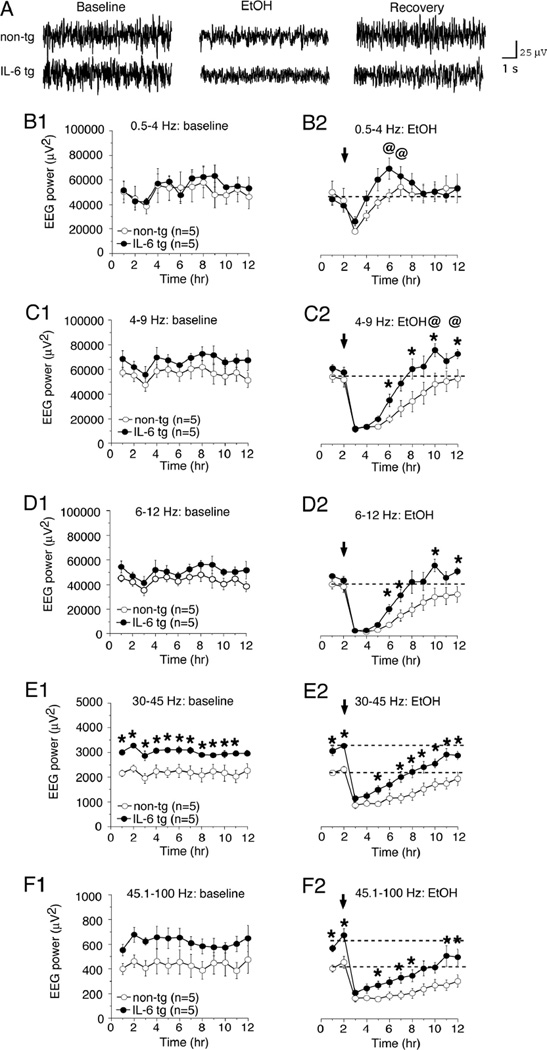
CNS activity in EEG recordings (Fig. 6A) was quantified by EEG power at delta (0.5–4.0 Hz), theta (4–9 Hz), alpha (6–12 Hz), and gamma (30–45 Hz and 45.1–100 Hz) frequencies. In general, the slow-wave activities (1–4 Hz) of the EEG are associated with sleep, less attentive conditions and drowsiness, while the faster-wave activities (12–50 Hz) are associated with arousal and attentive states (Pian et al., 2008).
Potential differences in baseline EEG activity were evaluated during a 12 hour period (in the dark) one day prior to testing the effects of ethanol. There were no significant differences between the IL-6 tg and non-tg mice in the EEG power for delta, theta and alpha frequency ranges during the baseline period (Fig. 7B1–D1). In contrast, a significant increase in EEG power for the 30–45 Hz gamma frequency range (~38% increase; repeated measures ANOVA, F(1,8) = 12.798, p = 0.007) was observed during the baseline period for IL-6 tg mice compared to the non-tg mice (Fig. 7E1). EEG power for the 45.1–100 Hz frequency range was not significantly increased in the IL-6 tg mice, although it did show a trend (0.1>p>0.05) for an increase (repeated measures ANOVA, F(1,8) = 3.914, p = 0.08) (Fig. 7F1).
Figure 7.
EEG analysis revealed differences in power spectra between IL-6 tg and non-tg mice before and after ethanol administration. (A) Representative EEG recordings from IL-6 tg and non-tg mice under baseline conditions, after ethanol administration and during the phase of declining blood ethanol levels (Recovery). (B1–F1). Graphs show mean values (±SEM) of EEG power for different frequency ranges recorded in IL-6 tg (closed circle) and non-tg (open circle) mice during a baseline control period. The IL-6 tg mice showed a significantly higher level of EEG power for the gamma frequency ranges (E1,F1) than the non-tg mice. This difference was significant for the 30–45 Hz frequency band (E1). (B2-F2) Graphs showing mean values (±SEM) of EEG power at different frequencies obtained during a 12 hr recording period that included a baseline period (2 hr), injection of a high dose of ethanol (arrow; 4 gm/kg, i.p.) and during the period of declining blood ethanol levels (4–12 hr). The IL-6 tg mice consistently showed higher EEG power than the non-tg mice for all EEG frequencies during the period of declining blood ethanol levels. However, significant differences in EEG power between IL-6 tg and non-tg mice were not observed for the gamma frequency bands when the data were expressed as a percent of baseline (not shown). *Significant difference between IL-6 tg and non-tg mice (Repeated measures ANOVA with post hoc Fisher’s PLSD, p<0.05). @Significant increase over baseline level for the same genotype (paired t-test, p<0.05). Dotted lines indicate baseline levels.
On the following day, EEG power was measured at hourly intervals during a 12 hour period (in the dark). After 2 hours of baseline recording, ethanol was administered (4 g/kg, i.p.). EEG power for all measured frequencies declined precipitously after ethanol administration, to a similar extent for IL-6 tg and non-tg mice (Fig. 7B2–F2). Similar administration of saline does not alter EEG power (unpublished). Recovery of EEG power occurred during the next 12 hours that EEG activity was recorded, with the IL-6 tg mice showing faster recovery from the depressive effects of ethanol than non-tg mice (Fig. 7B2–F2). Repeated measures ANOVA confirmed a significant main effect of genotype for EEG power in the alpha (F(1,8) = 6.306, p = 0.033) and gamma (30–45 Hz, F(1,8) = 11.891, p = 0.009; 45.1–100 Hz, F(1,8) = 8.453, p = 0.02) frequency ranges of the EEG, and also a significant time × genotype interaction for EEG power in the alpha (F(1,11) = 3.363, p = 0.0007) and gamma (30–45 Hz, F(1,11) = 3.089, p = 0.002; 45.1–100 Hz, F(1,11) = 2.306, p = 0.016) frequency ranges. No significant genotype effect was observed for EEG power in delta (F(1,8) = 0.487, p = 0.51) or theta (F(1,8) = 4.784, p = 0.06) frequency ranges, although there was a significant genotype × time interaction for EEG power for both the delta (F(1,11) = 2.476, p = 0.009) and theta (F(1,11) =3.571, p = 0.0004) frequency ranges. Also, EEG power for the delta and theta frequency ranges exceeded baseline levels (paired t-test) at some recovery time points in the IL-6 tg mice, an effect that was not observed in non-tg mice (Fig. 7B2,C2).
When differences in baseline levels of EEG power were taken into consideration, by expressing the EEG activity at time points after ethanol administration as a percent of the average baseline value before ethanol administration for each mouse, EEG power for the gamma frequency ranges no longer showed a significant genotypic effect (repeated measures ANOVA for hours 4–12; 30–45 Hz, F(1,8) = 0.689, p = 0.43; 45.1–100 Hz, F(1,8) = 0.570, p = 0.47) or genotype × time interactions (30–45 Hz, F(1,11) = 1.245, p = 0.29; 45.1–100 Hz, F(1,11) = 0.992, p = 0.45). These results indicate that the effects of ethanol on EEG gamma power was proportional to baseline levels, which were higher in the IL-6 tg mice. Differences between the IL-6 tg and non-tg mice in the timecourse of recovery of EEG power, and the increase in EEG power over baseline levels observed for other EEG frequencies were not evident for EEG gamma frequencies (Fig. 7B2–F2). Taken together, these results show that IL-6 tg mice differ significantly from non-tg mice with respect to both baseline activities of CNS circuits as well as the effect of acute ethanol on these circuits.
To determine if differences in wakefulness contribute to genotypic differences in EEG power, an analysis of sleep time was carried out for a one hour interval starting at the 10 hour time point, when significant differences were observed in EEG power between the IL-6 tg and non-tg mice. This time point correlates with the 8 hour time point in the HIC studies. There was no significant difference in the percent of time spent in wakefulness (~60% for IL-6 tg vs. 44% for non-tg), slow wave sleep (~39% for IL-6 tg vs. 54% for non-tg) or REM sleep (~1% for IL-6 tg vs. 2% for non-tg) between the IL-6 tg and non-tg mice (p>0.05, unpaired t-test). Thus, differences in wakefulness or sleep time during ethanol withdrawal do not appear to contribute to the genotypic differences in EEG power observed between the IL-6 tg and non-tg mice.
4. Discussion
Results from the current studies show that transgenic mice genetically engineered to produce increased astrocyte expression of IL-6 show altered responses to acute ethanol. The altered responses were demonstrated in electrophysiological studies on the effects of acute ethanol on synaptic transmission and plasticity in hippocampal slices from the IL-6 tg and non-tg mice, and in behavioral studies of ethanol withdrawal hyperactivity in the CNS of IL-6 tg and non-tg mice. These results raise the possibility that ethanol consumption will produce similar neuroadaptive changes in the CNS as a consequence of ethanol-induced increases in astrocytes production of IL-6, an action that could result in persistent alterations in CNS function, contribute to mechanisms involved in the development of alcohol dependence, and confound disorders that are co-morbid with alcohol dependence.
4.1. Ethanol and synaptic responses
Our previous studies identified neuroadaptive changes in the hippocampus of IL-6 tg mice that enhanced the fEPSP and the PS (Gruol et al., 2014; Nelson et al., 2012). Here we show that neuroadaptive changes in the IL-6 tg hippocampus also alter the effects of acute ethanol on these synaptic responses. Thus, in the IL-6 tg hippocampal slices ethanol enhanced the fEPSP and PS, whereas in non-tg hippocampal slices ethanol reduced the fEPSP and PS, consistent with the known depressive actions of ethanol. In contrast, neuroadaptive changes in synaptic plasticity were not evident in ethanol naïve IL-6 tg hippocampus but were revealed by ethanol. Thus, there were no significant differences in the PPR of the PS or the magnitude of PTP, STP and LTP between the non-tg and IL-6 tg hippocampal slices from ethanol naïve mice (Nelson et al., 2012). Acute ethanol enhanced PPR of the PS in the non-tg hippocampal slices, but the IL-6 tg slices were more resistant to this effect of ethanol. Ethanol reduced PTP, STP, and LTP in a dose-dependent manner in the non-tg slices, consistent with the known depressive effects of acute ethanol on these forms of synaptic plasticity (McCool, 2011; Zorumski et al., 2014). However, In the IL-6 tg hippocampal slices, there was no effect of ethanol on PTP, STP, or LTP.
The neuroadaptive changes that are responsible for the differences in the effects of ethanol on synaptic function between the IL-6 tg and non-tg hippocampus remain to be determined in future studies. However, several sites of ethanol action could be involved. For example, the magnitude of the PPR of the PS is a function of the action of recurrent GABAergic inhibition to the pyramidal neuron and somatic/dendritic ion channels that mediate pyramidal neuron excitability. Ethanol has been shown to alter recurrent GABAergic inhibition of CA1 neurons (Weiner and Valenzuela, 2006). Inhibitory interneurons that provide recurrent GABAergic inhibition to CA1 neurons and express parvalbumin (PAV), a Ca2+ binding protein, show morphological alterations at 2 months of age and cell loss at 6 months of age in the IL-6 tg mice (Campbell et al., 1993; Heyser et al., 1997; Samland et al., 2003). Therefore, functional changes in recurrent GABAergic inhibition in the IL-6 tg hippocampus could contribute to differences between non-tg and IL-6 tg hippocampus in the effects of ethanol on the PPR of the PS.
Neuroadaptive changes that affect the activity/expression of ethanol-sensitive ion channels could also contribute to differences in the effects of ethanol between the IL-6 tg and non-tg hippocampus. For example, ethanol has been shown to reduce the activity/expression of K+ channels (e.g., KCa2, Kv4), an effect that increases excitability (Mulholland et al., 2009; Mulholland et al., 2014). K+ channels control excitability in both the somatic and dendritic region of hippocampal neurons by setting the resting membrane potential and repolarizing the membrane potential following the depolarizing phase of synaptic responses and action potentials. If functional expression of ethanol-sensitive K+ channels was altered in the IL-6 tg hippocampus, this difference could contribute to differences in the effects of ethanol on fEPSP, PS and/or PPR of the PS. Neuroadaptive changes in NMDA receptor (NMDAR)-mediated synaptic responses could also contribute to the altered effects of ethanol in the IL-6 tg hippocampus. Our previous studies showed that the peak amplitude of the NMDAR-mediated fEPSP was larger in the IL-6 tg slices than in the non-tg slices (Nelson et al., 2012). Ethanol is known to reduce responses mediated by NMDARs (Lovinger et al., 1990; Wirkner et al., 1999). A larger NMDAR component of the synaptic response in the IL-6 tg slices could lead to a smaller net effect of ethanol, both with respect to the fEPSP and LTP. Interestingly, our studies of cultured cerebellar granule neurons showed that chronic treatment with IL-6 results in reduced levels of Kv4.2 protein (Gruol et al., 2011) and increased NMDAR-mediated responses (Qiu et al., 1995; Qiu et al., 1998) in the granule neurons. These findings raise the possibility that astrocyte production of IL-6 in the IL-6 tg hippocampus could result in similar changes in the CA1 pyramidal neurons and, consequently, enhanced excitability and altered response to ethanol. Alternatively or in addition, neuroadaptive effects of IL-6 could alter the sensitivity of NMDAR- or Kv4.2-mediated events to ethanol, a possibility to be pursued in future studies.
Neuroadaptive changes in the level or activation of signal transduction molecules utilized by IL-6 including STAT3 and p42/44 MAPK could also play a role in the altered effects of acute ethanol on synaptic plasticity in the IL-6 tg hippocampus. STAT3 and p42/44 MAPK are known to be involved in the induction of hippocampal synaptic plasticity (Nicolas et al., 2012; Sweatt, 2001). Ethanol has been shown to alter p42/44 MAPK and STAT3 activation in CNS tissue, effects that can vary across brain regions (Bachtell et al., 2002; Chandler and Sutton, 2005; Fujita et al., 2003; Kalluri and Ticku, 2002; Roberto et al., 2003). Thus, multiple ethanol-sensitive targets could be involved in the neuroadaptive changes produced in the IL-6 tg CNS and, consequently, in the altered effects of ethanol.
4.2. Acute ethanol-induced IL-6 production
Measurement of IL-6 levels in hippocampal slices showed that acute ethanol increased the level of IL-6 in both the IL-6 tg and non-tg hippocampal slices. However, there were no corresponding changes in the levels of activated STAT3 and p42/44 MAPK, suggesting that IL-6 signal transduction was not activated in the hippocampal slices, at least at the 30 min time period tested. Previous studies have shown that effects of IL-6 on these signal transduction molecules evident with a 30 min IL-6 exposure period (Schumann et al., 1999; Tancredi et al., 2000). Studies of cultured astrocytes showed that exposure to 50 mM ethanol (24 hr exposure) did not induce increased secretion of IL-6 protein from the astrocytes (Sarc et al., 2011). These results make it unlikely that ethanol-induced production/release of acute IL-6 contributed to the differences in the effects ethanol on synaptic function between the IL-6 tg and non-tg slices. Consistent with this interpretation, acute application of IL-6 does not alter the fEPSP or PS evoked by Schaffer collateral stimulation in CA1 pyramidal neurons, (Li et al., 1997; Tancredi et al., 2000), making it unlikely that acute IL-6 contributed to the effects of ethanol on the fEPSP or PS in the IL-6 tg or non-tg slices. Acute application of IL-6 does reduce long-term synaptic plasticity (PTP, STP and LTP)(Li et al., 1997; Tancredi et al., 2000). Thus, IL-6 could have played a role in the depressive effects of ethanol on long-term synaptic plasticity in the non-tg slices but not the IL-6 tg slices, which did not show a similar ethanol-induced depression of long-term synaptic plasticity.
Ethanol effects on IL-6 signaling could explain the lack of changes in the level of activation of STAT3 or p42/44 MAPK in our studies of hippocampal slices. The effect of acute ethanol on STAT3 activation has not been reported for CNS tissue, but in other cell types (i.e., liver cells, monocytes) acute ethanol reduces IL-6 activation of STAT3 (Chen et al., 1999; Norkina et al., 2008). Acute ethanol has been reported to inhibit p42/44 MAPK activation in cortical and hippocampal tissue (Kalluri and Ticku, 2002, 2003; Spanos et al., 2012).
Although ethanol-induced production of acute IL-6 did not appear to contributed to differences in the effects ethanol on synaptic function between the IL-6 tg and non-tg hippocampal slices, acute IL-6 could play a role in genotypic differences observed In the behavioral studies (HIC and EEG). In these studies, blood ethanol levels were in the 400 mg/dl range (~90 mM), a range where astrocytes have been shown to secrete IL-6 (Sarc et al., 2011). A high dose of ethanol (4 g/kg, i.p.) has been shown to produce elevated levels of IL-6 mRNA (~100 % increase) in the hippocampus at 3–9 hrs following ethanol injection (Doremus-Fitzwater et al., 2014). Therefore, ethanol-induced release of IL-6 from astrocytes could play a role in the effects of ethanol on the EEG activity in the IL-6 and non-tg mice.
4.3. Ethanol and HIC
The action of acute ethanol to increase the fEPSP and PS in the IL-6 tg hippocampus could extended to other CNS regions and contribute to the greater CNS excitability of the IL-6 tg mice observed in the HIC test and EEG recordings. The increased ethanol withdrawal excitability was specific to the IL-6 tg mice in that similar studies of CCL2 transgenic (CCL2-tg) mice and their non-transgenic littermate control (CCL2-non-tg) mice showed no genotypic difference in the effects of a single high dose of ethanol (4.0 g/kg, i.p.) on HIC scores (unpublished). Like the IL-6 tg mice, the CCL2-tg mice express elevated levels of CCL2 in the CNS through increased astrocyte expression (Bray et al., 2013; Huang et al., 2002). Also like IL-6 tg mice, CCL2 levels are increased in the CNS by ethanol (He and Crews, 2008; Kane et al., 2013). HIC scores for CCL2 null mice were similar to scores for wildtype mice when the mice were tested after exposure to ethanol in a two-bottle choice drinking paradigm (Blednov et al., 2005), supporting a lack of involvement of CCL2 in ethanol withdrawal hyperexcitability.
4.4. Ethanol and EEG activity
Acute ethanol-induced alterations in CNS activity during ethanol withdrawal were also demonstrated by a comparison of EEG activity in the IL-6 tg and non-tg mice. EEG power for theta and alpha frequencies showing a faster recovery from the depressive effects of ethanol, and the delta and theta frequencies showed an overshoot of baseline levels in the IL-6 tg mice compared with non-tg mice, consistent with greater activity in these frequency ranges in the IL-6 tg mice. Thus, neuroadaptive effects in the IL-6 tg mice, although not evident under baseline conditions, were revealed for the delta, theta, and alpha frequency range when ethanol was on board.
In contrast, a genotypic difference was observed for EEG power in the gamma frequency range during baseline recordings and after ethanol administration. However, no genotypic difference in gamma frequency levels was observed after ethanol administration when adjustments were made for baseline differences in gamma frequency levels. Thus, the effect of acute ethanol on activity in the gamma frequency range was proportional to baseline levels, which were higher in the IL-6 tg mice. In addition, the timecourse of acute ethanol action for the gamma frequency range was similar for the IL-6 tg and non-tg mice. These results suggest that neuroadaptive effects in the IL-6 tg mice and actions of acute ethanol overlap to some extent with mechanisms responsible for generation or regulation of gamma frequency activity.
The higher EEG power in the gamma frequency range in the IL-6 tg mice under baseline conditions indicates a higher level of CNS activity than in the non-tg mice, a condition that could contribute to the increased susceptibility of the IL-6 tg mice to kainate- and NMDA-induce seizure activity (Samland et al., 2003). Consistent with this possibility, systemic administration of kainate has been shown to cause generalized non-convulsive discharges characterized by increased gamma activity (30–40 Hz) in the hippocampus and neocortex of rats prior to the expression of seizure activity (Medvedev et al., 2000).
4.5. Gamma frequency activity
Gamma frequency activity is observed in many brain areas during different behavioral states and is thought to arise through local circuit activity involving excitatory, glutamate containing pyramidal neurons, and inhibitory, GABAergic interneurons that express PAV (Buzsaki and Wang, 2012; Ferando and Mody, 2013; Mann and Mody, 2010). Thus, neuroadaptive effects on local circuit activity could contribute the increased gamma frequency activity observed under baseline conditions in the IL-6 tg mice. The alterations in GABAergic interneurons that express PAV observed in the hippocampus and cortex of IL-6 tg mice are consistent with altered local circuit activity in the IL-6 tg hippocampus (Campbell et al., 1993; Heyser et al., 1997; Samland et al., 2003). Also, our Western blot analysis of the level of GAD65/67, the synthetic enzyme for GABA, showed reduced levels in the IL-6-tg hippocampus compared to the non-tg hippocampus, although no genotypic difference was observed in PAV levels (Gruol et al., 2014; Nelson et al., 2012). Thus, effects on inhibitory interneurons could contribute to the increased EEG power in the gamma frequency range in the IL-6 tg mice.
4.6. IL-6 expression in the IL-6 tg mice
Although the neuroadaptive changes in the IL-6 tg mice that underlie the altered response to ethanol have yet to be identified, several lines of evidence indicate that the changes are directly or indirectly related to the biologic actions of transgene derived IL-6. For example, the highest number of astrocytes expressing the transgene in the forebrain region of the IL-6 tg mice occurs in the hippocampus (Vallieres et al., 2002), where IL-6 transgene expression in astrocytes was demonstrated by expression of the lacZ reporter gene and immunohistochemical detection of β-gal (Vallieres et al., 2002). Studies of supernatant from astrocytes cultured from the CNS of IL-6 tg mice showed that IL-6 tg astrocytes secrete significant IL-6 protein (Campbell et al., 1993). Immunohistochemical studies showed increased levels of activated STAT3 (i.e., pSTAT3), primarily in astrocytes and microglia of the IL-6 tg CNS, indicative of activation of IL-6R and consistent with elevated levels of IL-6 in the IL-6 tg CNS (Sanz et al., 2008). The IL-6 tg CNS shows increase expression of IL-6 regulated genes (e.g., GFAP, eb22, Socs3), increased levels of GFAP, and increased levels of activated STAT3 (pSTAT3), the signal transduction molecule through which IL-6 acts to increase GFAP (Gruol et al., 2014; Herrmann et al., 2008; Nelson et al., 2012; Sanz et al., 2008; Shu et al., 2011). The increased sensitivity to seizure activity observed in the IL-6 tg mice was specific for IL-6 in that a similar sensitivity was not observed in transgenic mice that express elevated levels of TNF-α in the CNS through astrocyte expression (Samland et al., 2003). However, the link to IL-6 could be indirect and result from actions of secondary effectors such as other cytokines under the control of IL-6 or other downstream factors activated by IL-6.
Although astrocytes are a primary producer of IL-6 in the IL-6 tg CNS, microglia or other cell types that are responders and/or producers of IL-6 could also play a secondary role. Astrocytes are present at a higher density than microglia in the hippocampus (~50% fewer microglia) (Long et al., 1998; Savchenko et al., 2000), making it likely that they play a more prominent role than microglia as IL-6 producers in the IL-6 tg hippocampus. Moreover, microglial production of IL-6 is typically associated with prolonged exposure to high doses of ethanol rather than the acute ethanol exposure used in our studies (Marshall et al., 2013; Ward et al., 2014; Zhang et al., 2014; Zhao et al., 2013).
4.7. Summary
Our studies show that neuroadaptive changes in the IL-6 tg mice significantly alter the CNS actions of ethanol at both the synaptic and behavioral levels. The neuroadaptive changes resulted in an ethanol-induced increase in hippocampal synaptic responses rather than a depression, a resistance of long-term synaptic plasticity to the depressive effects of ethanol, and enhanced ethanol withdrawal hyperexcitability. Although it is unknown if the neuroadaptive changes in the IL-6 tg mice result from direct or indirect effects of IL-6, these results support the idea that ethanol-induced increases in the levels of IL-6 in the CNS could play a critical role in the CNS actions of ethanol and in the severity of ethanol-induced withdrawal symptoms, which is a contributing factor to the risk for developing alcohol dependence (Becker and Mulholland, 2014). A role for IL-6 as a risk factor for developing alcohol dependence has also been noted in other studies. Blednov et al (Blednov et al., 2012) showed that mice that lack IL-6 (IL-6 null) exhibited lower ethanol preference and consumption than wildtype control mice in a two-bottle choice behavioral paradigm, suggesting a role for IL-6 in the regulation of ethanol consumption. Genomic studies of alcohol-preferring rats and mice also identified IL-6 signaling as a candidate contributor to alcohol preference (Mulligan et al., 2006).
Interestingly, chronic ethanol exposure/withdrawal reduces the number of neurons that immunostain for PAV (Smiley et al., 2015; Udomuksorn et al., 2011; Vongvatcharanon et al., 2010), increases expression of GFAP (Chiang et al., 1994; Vongvatcharanon et al., 2010), increases EEG gamma power in the CNS (Cheaha et al., 2014), increases NMDAR-mediated synaptic responses (Carpenter-Hyland et al., 2004; Hendricson et al., 2007; Nelson et al., 2005), and reduces Kv4.2 expression (Mulholland et al., 2014). Thus, chronic ethanol exposure/withdrawal can produce some of the same characteristics as observed in ethanol-naïve IL-6 tg mice or CNS cultures chronically treated with IL-6. These similarities raise the possibility that ethanol-induced IL-6 production could, directly or indirectly, play a role in these neuroadaptive effects of chronic ethanol exposure/withdrawal, in which case the long-term effects of IL-6 are an important consideration and could provide alternative targets for therapeutic intervention. An understanding of interactions between neuroadaptive effects of IL-6 and ethanol is also an important consideration for conditions where CNS injury (e.g., traumatic brain injury (Teng and Molina, 2014)) or disease (e.g., depression (Neupane et al., 2014)), is comorbid with alcohol use disorders, as both conditions produce increased levels of IL-6 in the CNS.
Highlights.
Effects of ethanol are altered in mice with increased astrocyte expression of IL-6.
Ethanol depression of the fEPSP and PS is not observed in IL-6 tg hippocampus.
Long-term synaptic plasticity is resistant to ethanol in the IL-6 tg hippocampus.
EEG activity during ethanol withdrawal is enhanced in IL-6 transgenic mice.
Acknowledgements
Supported by NIAAA Grant AA019261 and the Integrated Neuroscience Initiative on Alcoholism (INAI)-West grant AA020893.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest
The authors have no conflict of interest to declare.
References
- Alfonso-Loeches S, Pascual-Lucas M, Blanco AM, Sanchez-Vera I, Guerri C. Pivotal role of TLR4 receptors in alcohol-induced neuroinflammation and brain damage. Journal of Neuroscience. 2010;30:8285–8295. doi: 10.1523/JNEUROSCI.0976-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bachtell RK, Tsivkovskaia NO, Ryabinin AE. Alcohol-induced c-Fos expression in the Edinger-Westphal nucleus: pharmacological and signal transduction mechanisms. Journal of Pharmacology and Experimental Therapeutics. 2002;302:516–524. doi: 10.1124/jpet.102.036046. [DOI] [PubMed] [Google Scholar]
- Balschun D, Wetzel W, Del Rey A, Pitossi F, Schneider H, Zuschratter W, Besedovsky HO. Interleukin-6: a cytokine to forget. FASEB Journal. 2004;18:1788–1790. doi: 10.1096/fj.04-1625fje. [DOI] [PubMed] [Google Scholar]
- Beattie EC, Stellwagen D, Morishita W, Bresnahan JC, Ha BK, Von Zastrow M, Beattie MS, Malenka RC. Control of synaptic strength by glial TNFalpha. Science. 2002;295:2282–2285. doi: 10.1126/science.1067859. [DOI] [PubMed] [Google Scholar]
- Becker HC. Animal models of alcohol withdrawal. Alcohol Res Health. 2000;24:105–113. [PMC free article] [PubMed] [Google Scholar]
- Becker HC, Mulholland PJ. Neurochemical mechanisms of alcohol withdrawal. Handbook of Clinical Neurology. 2014;125:133–156. doi: 10.1016/B978-0-444-62619-6.00009-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellinger FP, Madamba S, Siggins GR. Interleukin 1 beta inhibits synaptic strength and long-term potentiation in the rat CA1 hippocampus. Brain Research. 1993;628:227–234. doi: 10.1016/0006-8993(93)90959-q. [DOI] [PubMed] [Google Scholar]
- Blanco AM, Valles SL, Pascual M, Guerri C. Involvement of TLR4/type I IL-1 receptor signaling in the induction of inflammatory mediators and cell death induced by ethanol in cultured astrocytes. Journal of Immunology. 2005;175:6893–6899. doi: 10.4049/jimmunol.175.10.6893. [DOI] [PubMed] [Google Scholar]
- Blednov YA, Bergeson SE, Walker D, Ferreira VM, Kuziel WA, Harris RA. Perturbation of chemokine networks by gene deletion alters the reinforcing actions of ethanol. Behavioural Brain Research. 2005;165:110–125. doi: 10.1016/j.bbr.2005.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blednov YA, Ponomarev I, Geil C, Bergeson S, Koob GF, Harris RA. Neuroimmune regulation of alcohol consumption: behavioral validation of genes obtained from genomic studies. Addiction Biology. 2012;17:108–120. doi: 10.1111/j.1369-1600.2010.00284.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blitzer RD, Gil O, Landau EM. Long-term potentiation in rat hippocampus is inhibited by low concentrations of ethanol. Brain Research. 1990;537:203–208. doi: 10.1016/0006-8993(90)90359-j. [DOI] [PubMed] [Google Scholar]
- Boyadjieva NI, Sarkar DK. Role of microglia in ethanol's apoptotic action on hypothalamic neuronal cells in primary cultures. Alcoholism, Clinical and Experimental Research. 2010;34:1835–1842. doi: 10.1111/j.1530-0277.2010.01271.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bray JG, Reyes KC, Roberts AJ, Ransohoff RM, Gruol DL. Synaptic plasticity in the hippocampus shows resistance to acute ethanol exposure in transgenic mice with astrocyte-targeted enhanced CCL2 expression. Neuropharmacology. 2013;67:115–125. doi: 10.1016/j.neuropharm.2012.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briere FN, Rohde P, Seeley JR, Klein D, Lewinsohn PM. Comorbidity between major depression and alcohol use disorder from adolescence to adulthood. Comprehensive Psychiatry. 2014;55:526–533. doi: 10.1016/j.comppsych.2013.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buzsaki G, Wang XJ. Mechanisms of gamma oscillations. Annual Review of Neuroscience. 2012;35:203–225. doi: 10.1146/annurev-neuro-062111-150444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell IL, Abraham CR, Masliah E, Kemper P, Inglis JD, Oldstone MB, Mucke L. Neurologic disease induced in transgenic mice by cerebral overexpression of interleukin 6. Proceedings of the National Academy of Sciences of the United States of America. 1993;90:10061–10065. doi: 10.1073/pnas.90.21.10061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter-Hyland EP, Woodward JJ, Chandler LJ. Chronic ethanol induces synaptic but not extrasynaptic targeting of NMDA receptors. Journal of Neuroscience. 2004;24:7859–7868. doi: 10.1523/JNEUROSCI.1902-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandler LJ, Sutton G. Acute ethanol inhibits extracellular signal-regulated kinase, protein kinase B, adenosine 3':5'-cyclic monophosphate response element binding protein activity in an age- and brain region-specific manner. Alcoholism, Clinical and Experimental Research. 2005;29:672–682. doi: 10.1097/01.alc.0000158935.53360.5f. [DOI] [PubMed] [Google Scholar]
- Cheaha D, Sawangjaroen K, Kumarnsit E. Characterization of fluoxetine effects on ethanol withdrawal-induced cortical hyperexcitability by EEG spectral power in rats. Neuropharmacology. 2014;77:49–56. doi: 10.1016/j.neuropharm.2013.09.020. [DOI] [PubMed] [Google Scholar]
- Chen J, Kunos G, Gao B. Ethanol rapidly inhibits IL-6-activated STAT3 and C/EBP mRNA expression in freshly isolated rat hepatocytes. FEBS Letters. 1999;457:162–168. doi: 10.1016/s0014-5793(99)01031-5. [DOI] [PubMed] [Google Scholar]
- Chiang CS, Stalder A, Samimi A, Campbell IL. Reactive gliosis as a consequence of interleukin-6 expression in the brain: studies in transgenic mice. Developmental Neuroscience. 1994;16:212–221. doi: 10.1159/000112109. [DOI] [PubMed] [Google Scholar]
- Coogan A, O'Connor JJ. Inhibition of NMDA receptor-mediated synaptic transmission in the rat dentate gyrus in vitro by IL-1 beta. Neuroreport. 1997;8:2107–2110. doi: 10.1097/00001756-199707070-00004. [DOI] [PubMed] [Google Scholar]
- Crabbe JC. Provisional mapping of quantitative trait loci for chronic ethanol withdrawal severity in BXD recombinant inbred mice. Journal of Pharmacology and Experimental Therapeutics. 1998;286:263–271. [PubMed] [Google Scholar]
- Crabbe JC, Janowsky JS, Young ER, Rigter H. Handling induced convulsions in twenty inbred strains of mice. Substance and Alcohol Actions/Misuse. 1980;1:159–163. [PubMed] [Google Scholar]
- Crabbe JC, Jr, Young ER, Kosobud A. Genetic correlations with ethanol withdrawal severity. Pharmacology, Biochemistry and Behavior. 1983;18(Suppl 1):541–547. doi: 10.1016/0091-3057(83)90233-2. [DOI] [PubMed] [Google Scholar]
- Crabbe JC, Merrill C, Belknap JK. Acute dependence on depressant drugs is determined by common genes in mice. Journal of Pharmacology and Experimental Therapeutics. 1991;257:663–667. [PubMed] [Google Scholar]
- Doremus-Fitzwater TL, Buck HM, Bordner K, Richey L, Jones ME, Deak T. Intoxication- and withdrawal-dependent expression of central and peripheral cytokines following initial ethanol exposure. Alcoholism, Clinical and Experimental Research. 2014;38:2186–2198. doi: 10.1111/acer.12481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doremus-Fitzwater TL, Gano A, Paniccia JE, Deak T. Male adolescent rats display blunted cytokine responses in the CNS after acute ethanol or lipopolysaccharide exposure. Physiology and Behavior. 2015;148:131–144. doi: 10.1016/j.physbeh.2015.02.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erickson MA, Maramara LA, Lisman J. A single brief burst induces GluR1-dependent associative short-term potentiation: a potential mechanism for short-term memory. Journal of Cognitive Neuroscience. 2010;22:2530–2540. doi: 10.1162/jocn.2009.21375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farook JM, Krazem A, Lewis B, Morrell DJ, Littleton JM, Barron S. Acamprosate attenuates the handling induced convulsions during alcohol withdrawal in Swiss Webster mice. Physiology and Behavior. 2008;95:267–270. doi: 10.1016/j.physbeh.2008.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferando I, Mody I. Altered gamma oscillations during pregnancy through loss of delta subunit-containing GABA(A) receptors on parvalbumin interneurons. Front Neural Circuits. 2013;7:144. doi: 10.3389/fncir.2013.00144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finn DA, Snelling C, Fretwell AM, Tanchuck MA, Underwood L, Cole M, Crabbe JC, Roberts AJ. Increased drinking during withdrawal from intermittent ethanol exposure is blocked by the CRF receptor antagonist D-Phe-CRF(12-41) Alcoholism, Clinical and Experimental Research. 2007;31:939–949. doi: 10.1111/j.1530-0277.2007.00379.x. [DOI] [PubMed] [Google Scholar]
- Foltran F, Gregori D, Franchin L, Verduci E, Giovannini M. Effect of alcohol consumption in prenatal life, childhood, and adolescence on child development. Nutrition Reviews. 2011;69:642–659. doi: 10.1111/j.1753-4887.2011.00417.x. [DOI] [PubMed] [Google Scholar]
- Franklin K, Paxinos G. The Mouse Brain in Stereotaxic Coordinates. San Diego: Academic Press; 1997. [Google Scholar]
- Fujii S, Yamazaki Y, Sugihara T, Wakabayashi I. Acute and chronic ethanol exposure differentially affect induction of hippocampal LTP. Brain Research. 2008;1211:13–21. doi: 10.1016/j.brainres.2008.02.052. [DOI] [PubMed] [Google Scholar]
- Fujita N, Sakamaki H, Uotani S, Takahashi R, Kuwahara H, Kita A, Oshima K, Yamasaki H, Yamaguchi Y, Eguchi K. Acute effects of ethanol on feeding behavior and leptin-induced STAT3 phosphorylation in rat hypothalamus. International Journal of Obesity and Related Metabolic Disorders. 2003;27:55–59. doi: 10.1038/sj.ijo.0802194. [DOI] [PubMed] [Google Scholar]
- Gadient RA, Otten U. Expression of interleukin-6 (IL-6) and interleukin-6 receptor (IL-6R) mRNAs in rat brain during postnatal development. Brain Research. 1994;637:10–14. doi: 10.1016/0006-8993(94)91211-4. [DOI] [PubMed] [Google Scholar]
- Ghozland S, Chu K, Kieffer BL, Roberts AJ. Lack of stimulant and anxiolytic-like effects of ethanol and accelerated development of ethanol dependence in mu-opioid receptor knockout mice. Neuropharmacology. 2005;49:493–501. doi: 10.1016/j.neuropharm.2005.04.006. [DOI] [PubMed] [Google Scholar]
- Gilpin NW, Smith AD, Cole M, Weiss F, Koob GF, Richardson HN. Operant behavior and alcohol levels in blood and brain of alcohol-dependent rats. Alcoholism, Clinical and Experimental Research. 2009;33:2113–2123. doi: 10.1111/j.1530-0277.2009.01051.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giralt M, Ramos R, Quintana A, Ferrer B, Erta M, Castro-Freire M, Comes G, Sanz E, Unzeta M, Pifarre P, Garcia A, Campbell IL, Hidalgo J. Induction of atypical EAE mediated by transgenic production of IL-6 in astrocytes in the absence of systemic IL-6. Glia. 2013;61:587–600. doi: 10.1002/glia.22457. [DOI] [PubMed] [Google Scholar]
- Goldstein DB, Pal N. Alcohol dependence produced in mice by inhalation of ethanol: grading the withdrawal reaction. Science. 1971;172:288–290. doi: 10.1126/science.172.3980.288. [DOI] [PubMed] [Google Scholar]
- Gruol DL. IL-6 regulation of synaptic function in the CNS. Neuropharmacology. 2014 doi: 10.1016/j.neuropharm.2014.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruol DL, Nelson TE. Physiological and pathological roles of interleukin-6 in the central nervous system. Molecular Neurobiology. 1997;15:307–339. doi: 10.1007/BF02740665. [DOI] [PubMed] [Google Scholar]
- Gruol DL, Puro A, Hao C, Blakely P, Janneke E, Vo K. Neuroadaptive changes in cerebellar neurons induced by chronic exposure to IL-6. Journal of Neuroimmunology. 2011;239:28–36. doi: 10.1016/j.jneuroim.2011.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruol DL, Vo K, Bray JG. Increased astrocyte expression of IL-6 or CCL2 in transgenic mice alters levels of hippocampal and cerebellar proteins. Frontiers in Cellular Neuroscience. 2014;8:234. doi: 10.3389/fncel.2014.00234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halassa MM, Fellin T, Haydon PG. The tripartite synapse: roles for gliotransmission in health and disease. Trends in Molecular Medicine. 2007;13:54–63. doi: 10.1016/j.molmed.2006.12.005. [DOI] [PubMed] [Google Scholar]
- He J, Crews FT. Increased MCP-1 and microglia in various regions of the human alcoholic brain. Experimental Neurology. 2008;210:349–358. doi: 10.1016/j.expneurol.2007.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedlund PB, Huitron-Resendiz S, Henriksen SJ, Sutcliffe JG. 5-HT7 receptor inhibition and inactivation induce antidepressantlike behavior and sleep pattern. Biological Psychiatry. 2005;58:831–837. doi: 10.1016/j.biopsych.2005.05.012. [DOI] [PubMed] [Google Scholar]
- Heilig M, Egli M, Crabbe JC, Becker HC. Acute withdrawal, protracted abstinence and negative affect in alcoholism: are they linked? Addiction Biology. 2010;15:169–184. doi: 10.1111/j.1369-1600.2009.00194.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendricson AW, Maldve RE, Salinas AG, Theile JW, Zhang TA, Diaz LM, Morrisett RA. Aberrant synaptic activation of N-methyl-D-aspartate receptors underlies ethanol withdrawal hyperexcitability. Journal of Pharmacology and Experimental Therapeutics. 2007;321:60–72. doi: 10.1124/jpet.106.111419. [DOI] [PubMed] [Google Scholar]
- Herrmann JE, Imura T, Song B, Qi J, Ao Y, Nguyen TK, Korsak RA, Takeda K, Akira S, Sofroniew MV. STAT3 is a critical regulator of astrogliosis and scar formation after spinal cord injury. Journal of Neuroscience. 2008;28:7231–7243. doi: 10.1523/JNEUROSCI.1709-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heyser CJ, Masliah E, Samimi A, Campbell IL, Gold LH. Progressive decline in avoidance learning paralleled by inflammatory neurodegeneration in transgenic mice expressing interleukin 6 in the brain. Proceedings of the National Academy of Sciences of the United States of America. 1997;94:1500–1505. doi: 10.1073/pnas.94.4.1500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hingson RW, Heeren T, Winter MR. Age of alcohol-dependence onset: associations with severity of dependence and seeking treatment. Pediatrics. 2006;118:e755–e763. doi: 10.1542/peds.2006-0223. [DOI] [PubMed] [Google Scholar]
- Huang D, Tani M, Wang J, Han Y, He TT, Weaver J, Charo IF, Tuohy VK, Rollins BJ, Ransohoff RM. Pertussis toxin-induced reversible encephalopathy dependent on monocyte chemoattractant protein-1 overexpression in mice. Journal of Neuroscience. 2002;22:10633–10642. doi: 10.1523/JNEUROSCI.22-24-10633.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huitron-Resendiz S, Kristensen MP, Sanchez-Alavez M, Clark SD, Grupke SL, Tyler C, Suzuki C, Nothacker HP, Civelli O, Criado JR, Henriksen SJ, Leonard CS, de Lecea L. Urotensin II modulates rapid eye movement sleep through activation of brainstem cholinergic neurons. Journal of Neuroscience. 2005;25:5465–5474. doi: 10.1523/JNEUROSCI.4501-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huitron-Resendiz S, Sanchez-Alavez M, Wills DN, Cravatt BF, Henriksen SJ. Characterization of the sleep-wake patterns in mice lacking fatty acid amide hydrolase. Sleep. 2004;27:857–865. doi: 10.1093/sleep/27.5.857. [DOI] [PubMed] [Google Scholar]
- Ikegaya Y, Delcroix I, Iwakura Y, Matsuki N, Nishiyama N. Interleukin-1beta abrogates long-term depression of hippocampal CA1 synaptic transmission. Synapse. 2003;47:54–57. doi: 10.1002/syn.10154. [DOI] [PubMed] [Google Scholar]
- Izumi Y, Nagashima K, Murayama K, Zorumski CF. Acute effects of ethanol on hippocampal long-term potentiation and long-term depression are mediated by different mechanisms. Neuroscience. 2005;136:509–517. doi: 10.1016/j.neuroscience.2005.08.002. [DOI] [PubMed] [Google Scholar]
- Jankowsky JL, Derrick BE, Patterson PH. Cytokine responses to LTP induction in the rat hippocampus: a comparison of in vitro and in vivo techniques. Learning and Memory. 2000;7:400–412. doi: 10.1101/lm.32600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jurgens HA, Amancherla K, Johnson RW. Influenza infection induces neuroinflammation, alters hippocampal neuron morphology, and impairs cognition in adult mice. Journal of Neuroscience. 2012;32:3958–3968. doi: 10.1523/JNEUROSCI.6389-11.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kachadourian LK, Pilver CE, Potenza MN. Trauma, PTSD, and binge and hazardous drinking among women and men: findings from a national study. Journal of Psychiatric Research. 2014;55:35–43. doi: 10.1016/j.jpsychires.2014.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalluri HS, Ticku MK. Ethanol-mediated inhibition of mitogen-activated protein kinase phosphorylation in mouse brain. European Journal of Pharmacology. 2002;439:53–58. doi: 10.1016/s0014-2999(01)01599-0. [DOI] [PubMed] [Google Scholar]
- Kalluri HS, Ticku MK. Regulation of ERK phosphorylation by ethanol in fetal cortical neurons. Neurochemical Research. 2003;28:765–769. doi: 10.1023/a:1022822119560. [DOI] [PubMed] [Google Scholar]
- Kane CJ, Phelan KD, Douglas JC, Wagoner G, Johnson JW, Xu J, Drew PD. Effects of ethanol on immune response in the brain: region-specific changes in aged mice. Journal of Neuroinflammation. 2013;10:66. doi: 10.1186/1742-2094-10-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kane CJ, Phelan KD, Douglas JC, Wagoner G, Johnson JW, Xu J, Phelan PS, Drew PD. Effects of ethanol on immune response in the brain: region-specific changes in adolescent versus adult mice. Alcoholism, Clinical and Experimental Research. 2014;38:384–391. doi: 10.1111/acer.12244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katsuki H, Nakai S, Hirai Y, Akaji K, Kiso Y, Satoh M. Interleukin-1 beta inhibits long-term potentiation in the CA3 region of mouse hippocampal slices. European Journal of Pharmacology. 1990;181:323–326. doi: 10.1016/0014-2999(90)90099-r. [DOI] [PubMed] [Google Scholar]
- Lauri SE, Palmer M, Segerstrale M, Vesikansa A, Taira T, Collingridge GL. Presynaptic mechanisms involved in the expression of STP and LTP at CA1 synapses in the hippocampus. Neuropharmacology. 2007;52:1–11. doi: 10.1016/j.neuropharm.2006.06.017. [DOI] [PubMed] [Google Scholar]
- Li AJ, Katafuchi T, Oda S, Hori T, Oomura Y. Interleukin-6 inhibits long-term potentiation in rat hippocampal slices. Brain Research. 1997;748:30–38. doi: 10.1016/s0006-8993(96)01283-8. [DOI] [PubMed] [Google Scholar]
- Li G, Bauer S, Nowak M, Norwood B, Tackenberg B, Rosenow F, Knake S, Oertel WH, Hamer HM. Cytokines and epilepsy. Seizure. 2011;20:249–256. doi: 10.1016/j.seizure.2010.12.005. [DOI] [PubMed] [Google Scholar]
- Lippai D, Bala S, Csak T, Kurt-Jones EA, Szabo G. Chronic alcohol-induced microRNA-155 contributes to neuroinflammation in a TLR4-dependent manner in mice. PloS One. 2013;8:e70945. doi: 10.1371/journal.pone.0070945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lloyd E, Somera-Molina K, Van Eldik LJ, Watterson DM, Wainwright MS. Suppression of acute proinflammatory cytokine and chemokine upregulation by post-injury administration of a novel small molecule improves long-term neurologic outcome in a mouse model of traumatic brain injury. Journal of Neuroinflammation. 2008;5:28. doi: 10.1186/1742-2094-5-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long JM, Kalehua AN, Muth NJ, Calhoun ME, Jucker M, Hengemihle JM, Ingram DK, Mouton PR. Stereological analysis of astrocyte and microglia in aging mouse hippocampus. Neurobiology of Aging. 1998;19:497–503. doi: 10.1016/s0197-4580(98)00088-8. [DOI] [PubMed] [Google Scholar]
- Lovinger DM, White G, Weight FF. NMDA receptor-mediated synaptic excitation selectively inhibited by ethanol in hippocampal slice from adult rat. Journal of Neuroscience. 1990;10:1372–1379. doi: 10.1523/JNEUROSCI.10-04-01372.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luterman JD, Haroutunian V, Yemul S, Ho L, Purohit D, Aisen PS, Mohs R, Pasinetti GM. Cytokine gene expression as a function of the clinical progression of Alzheimer disease dementia. Archives of Neurology. 2000;57:1153–1160. doi: 10.1001/archneur.57.8.1153. [DOI] [PubMed] [Google Scholar]
- Mann EO, Mody I. Control of hippocampal gamma oscillation frequency by tonic inhibition and excitation of interneurons. Nature Neuroscience. 2010;13:205–212. doi: 10.1038/nn.2464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall SA, McClain JA, Kelso ML, Hopkins DM, Pauly JR, Nixon K. Microglial activation is not equivalent to neuroinflammation in alcohol-induced neurodegeneration: The importance of microglia phenotype. Neurobiology of Disease. 2013;54:239–251. doi: 10.1016/j.nbd.2012.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCool BA. Ethanol modulation of synaptic plasticity. Neuropharmacology. 2011;61:1097–1108. doi: 10.1016/j.neuropharm.2010.12.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McQuarrie D, Fingl E. Effects of single doses and chronic administration of ethanol on experimental seizures in mice. Journal of Pharmacology and Experimental Therapeutics. 1958;124:264–271. [PubMed] [Google Scholar]
- Medvedev A, Mackenzie L, Hiscock JJ, Willoughby JO. Kainic acid induces distinct types of epileptiform discharge with differential involvement of hippocampus and neocortex. Brain Research Bulletin. 2000;52:89–98. doi: 10.1016/s0361-9230(00)00239-2. [DOI] [PubMed] [Google Scholar]
- Metten P, Sorensen ML, Cameron AJ, Yu CH, Crabbe JC. Withdrawal severity after chronic intermittent ethanol in inbred mouse strains. Alcoholism, Clinical and Experimental Research. 2010;34:1552–1564. doi: 10.1111/j.1530-0277.2010.01240.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyamoto E. Molecular mechanism of neuronal plasticity: induction and maintenance of long-term potentiation in the hippocampus. Journal of Pharmacological Sciences. 2006;100:433–442. doi: 10.1254/jphs.cpj06007x. [DOI] [PubMed] [Google Scholar]
- Mulholland PJ, Hopf FW, Bukiya AN, Martin GE, Liu J, Dopico AM, Bonci A, Treistman SN, Chandler LJ. Sizing up ethanol-induced plasticity: the role of small and large conductance calcium-activated potassium channels. Alcoholism, Clinical and Experimental Research. 2009;33:1125–1135. doi: 10.1111/j.1530-0277.2009.00936.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulholland PJ, Spencer KB, Hu W, Kroener S, Chandler LJ. Neuroplasticity of A-type potassium channel complexes induced by chronic alcohol exposure enhances dendritic calcium transients in hippocampus. Psychopharmacology. 2014 doi: 10.1007/s00213-014-3835-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulligan MK, Ponomarev I, Hitzemann RJ, Belknap JK, Tabakoff B, Harris RA, Crabbe JC, Blednov YA, Grahame NJ, Phillips TJ, Finn DA, Hoffman PL, Iyer VR, Koob GF, Bergeson SE. Toward understanding the genetics of alcohol drinking through transcriptome meta-analysis. Proceedings of the National Academy of Sciences of the United States of America. 2006;103:6368–6373. doi: 10.1073/pnas.0510188103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson TE, Olde Engberink A, Hernandez R, Puro A, Huitron-Resendiz S, Hao C, De Graan PN, Gruol DL. Altered synaptic transmission in the hippocampus of transgenic mice with enhanced central nervous systems expression of interleukin-6. Brain, Behavior, and Immunity. 2012;26:959–971. doi: 10.1016/j.bbi.2012.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson TE, Ur CL, Gruol DL. Chronic intermittent ethanol exposure enhances NMDA-receptor-mediated synaptic responses and NMDA receptor expression in hippocampal CA1 region. Brain Research. 2005;1048:69–79. doi: 10.1016/j.brainres.2005.04.041. [DOI] [PubMed] [Google Scholar]
- Neupane SP, Lien L, Martinez P, Aukrust P, Ueland T, Mollnes TE, Hestad K, Bramness JG. High frequency and intensity of drinking may attenuate increased inflammatory cytokine levels of major depression in alcohol-use disorders. CNS Neuroscience & Therapeutics. 2014;20:898–904. doi: 10.1111/cns.12303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicolas CS, Peineau S, Amici M, Csaba Z, Fafouri A, Javalet C, Collett VJ, Hildebrandt L, Seaton G, Choi SL, Sim SE, Bradley C, Lee K, Zhuo M, Kaang BK, Gressens P, Dournaud P, Fitzjohn SM, Bortolotto ZA, Cho K, Collingridge GL. The Jak/STAT pathway is involved in synaptic plasticity. Neuron. 2012;73:374–390. doi: 10.1016/j.neuron.2011.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norkina O, Dolganiuc A, Catalano D, Kodys K, Mandrekar P, Syed A, Efros M, Szabo G. Acute alcohol intake induces SOCS1 and SOCS3 and inhibits cytokine-induced STAT1 and STAT3 signaling in human monocytes. Alcoholism, Clinical and Experimental Research. 2008;32:1565–1573. doi: 10.1111/j.1530-0277.2008.00726.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Connor JJ, Coogan AN. Actions of the pro-inflammatory cytokine IL-1 beta on central synaptic transmission. Experimental Physiology. 1999;84:601–614. [PubMed] [Google Scholar]
- Olive MF, Becker HC. Effects of the mGluR2/3 agonist LY379268 and the mGluR5 antagonist MPEP on handling-induced convulsions during ethanol withdrawal in mice. Alcohol. 2008;42:191–197. doi: 10.1016/j.alcohol.2008.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papatheodoropoulos C, Asprodini E, Nikita I, Koutsona C, Kostopoulos G. Weaker synaptic inhibition in CA1 region of ventral compared to dorsal rat hippocampal slices. Brain Research. 2002;948:117–121. doi: 10.1016/s0006-8993(02)02958-x. [DOI] [PubMed] [Google Scholar]
- Peng S, Zhang Y, Zhang J, Wang H, Ren B. Glutamate receptors and signal transduction in learning and memory. Molecular Biology Reports. 2011;38:453–460. doi: 10.1007/s11033-010-0128-9. [DOI] [PubMed] [Google Scholar]
- Peris J, Anderson KJ, Vickroy TW, King MA, Hunter BE, Walker DW. Neurochemical basis of disruption of hippocampal long term potentiation by chronic alcohol exposure. Frontiers in Bioscience. 1997;2:d309–d316. doi: 10.2741/a193. [DOI] [PubMed] [Google Scholar]
- Perper JA, Twerski A, Wienand JW. Tolerance at high blood alcohol concentrations: a study of 110 cases and review of the literature. Journal of Forensic Sciences. 1986;31:212–221. [PubMed] [Google Scholar]
- Petrides T, Georgopoulos P, Kostopoulos G, Papatheodoropoulos C. The GABAA receptor-mediated recurrent inhibition in ventral compared with dorsal CA1 hippocampal region is weaker, decays faster and lasts less. Experimental Brain Research. 2007;177:370–383. doi: 10.1007/s00221-006-0681-6. [DOI] [PubMed] [Google Scholar]
- Pian JP, Criado JR, Walker BM, Ehlers CL. Differential effects of acute alcohol on EEG and sedative responses in adolescent and adult Wistar rats. Brain Research. 2008;1194:28–36. doi: 10.1016/j.brainres.2007.11.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pribiag H, Stellwagen D. TNF-alpha downregulates inhibitory neurotransmission through protein phosphatase 1-dependent trafficking of GABA(A) receptors. Journal of Neuroscience. 2013;33:15879–15893. doi: 10.1523/JNEUROSCI.0530-13.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qin L, Crews FT. Chronic ethanol increases systemic TLR3 agonist-induced neuroinflammation and neurodegeneration. Journal of Neuroinflammation. 2012;9:130. doi: 10.1186/1742-2094-9-130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu Z, Parsons KL, Gruol DL. Interleukin-6 selectively enhances the intracellular calcium response to NMDA in developing CNS neurons. Journal of Neuroscience. 1995;15:6688–6699. doi: 10.1523/JNEUROSCI.15-10-06688.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu Z, Sweeney DD, Netzeband JG, Gruol DL. Chronic interleukin-6 alters NMDA receptor-mediated membrane responses and enhances neurotoxicity in developing CNS neurons. Journal of Neuroscience. 1998;18:10445–10456. doi: 10.1523/JNEUROSCI.18-24-10445.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramachandran B, Ahmed S, Zafar N, Dean C. Ethanol inhibits long-term potentiation in hippocampal CA1 neurons, irrespective of lamina and stimulus strength, through neurosteroidogenesis. Hippocampus. 2015;25:106–118. doi: 10.1002/hipo.22356. [DOI] [PubMed] [Google Scholar]
- Roberto M, Nelson TE, Ur CL, Brunelli M, Sanna PP, Gruol DL. The transient depression of hippocampal CA1 LTP induced by chronic intermittent ethanol exposure is associated with an inhibition of the MAP kinase pathway. European Journal of Neuroscience. 2003;17:1646–1654. doi: 10.1046/j.1460-9568.2003.02614.x. [DOI] [PubMed] [Google Scholar]
- Roberts AJ, Crabbe JC, Keith LD. Genetic differences in hypothalamic-pituitary-adrenal axis responsiveness to acute ethanol and acute ethanol withdrawal. Brain Research. 1992;579:296–302. doi: 10.1016/0006-8993(92)90064-g. [DOI] [PubMed] [Google Scholar]
- Sallmann S, Juttler E, Prinz S, Petersen N, Knopf U, Weiser T, Schwaninger M. Induction of interleukin-6 by depolarization of neurons. Journal of Neuroscience. 2000;20:8637–8642. doi: 10.1523/JNEUROSCI.20-23-08637.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samland H, Huitron-Resendiz S, Masliah E, Criado J, Henriksen SJ, Campbell IL. Profound increase in sensitivity to glutamatergic- but not cholinergic agonist-induced seizures in transgenic mice with astrocyte production of IL-6. Journal of Neuroscience Research. 2003;73:176–187. doi: 10.1002/jnr.10635. [DOI] [PubMed] [Google Scholar]
- Sanz E, Hofer MJ, Unzeta M, Campbell IL. Minimal role for STAT1 in interleukin-6 signaling and actions in the murine brain. Glia. 2008;56:190–199. doi: 10.1002/glia.20602. [DOI] [PubMed] [Google Scholar]
- Sarc L, Wraber B, Lipnik-Stangelj M. Ethanol and acetaldehyde disturb TNF-alpha and IL-6 production in cultured astrocytes. Human and Experimental Toxicology. 2011;30:1256–1265. doi: 10.1177/0960327110388533. [DOI] [PubMed] [Google Scholar]
- Savchenko VL, McKanna JA, Nikonenko IR, Skibo GG. Microglia and astrocytes in the adult rat brain: comparative immunocytochemical analysis demonstrates the efficacy of lipocortin 1 immunoreactivity. Neuroscience. 2000;96:195–203. doi: 10.1016/s0306-4522(99)00538-2. [DOI] [PubMed] [Google Scholar]
- Schobitz B, de Kloet ER, Sutanto W, Holsboer F. Cellular localization of interleukin 6 mRNA and interleukin 6 receptor mRNA in rat brain. European Journal of Neuroscience. 1993;5:1426–1435. doi: 10.1111/j.1460-9568.1993.tb00210.x. [DOI] [PubMed] [Google Scholar]
- Schumann G, Huell M, Machein U, Hocke G, Fiebich BL. Interleukin-6 activates signal transducer and activator of transcription and mitogen-activated protein kinase signal transduction pathways and induces de novo protein synthesis in human neuronal cells. Journal of Neurochemistry. 1999;73:2009–2017. [PubMed] [Google Scholar]
- Schummers J, Bentz S, Browning MD. Ethanol's inhibition of LTP may not be mediated solely via direct effects on the NMDA receptor. Alcoholism, Clinical and Experimental Research. 1997;21:404–408. doi: 10.1111/j.1530-0277.1997.tb03783.x. [DOI] [PubMed] [Google Scholar]
- Schwieler L, Larsson MK, Skogh E, Kegel ME, Orhan F, Abdelmoaty S, Finn A, Bhat M, Samuelsson M, Lundberg K, Dahl ML, Sellgren C, Schuppe-Koistinen I, Svensson C, Erhardt S, Engberg G. Increased levels of IL-6 in the cerebrospinal fluid of patients with chronic schizophrenia--significance for activation of the kynurenine pathway. Journal of Psychiatry and Neuroscience. 2015;40:126–133. doi: 10.1503/jpn.140126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shield KD, Parry C, Rehm J. Chronic diseases and conditions related to alcohol use. Alcohol Res. 2013;35:155–173. [PMC free article] [PubMed] [Google Scholar]
- Shu M, Zhou Y, Zhu W, Wu S, Zheng X, Yan G. Activation of a pro-survival pathway IL-6/JAK2/STAT3 contributes to glial fibrillary acidic protein induction during the cholera toxin-induced differentiation of C6 malignant glioma cells. Molecular Oncology. 2011;5:265–272. doi: 10.1016/j.molonc.2011.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverstein PS, Kumar S, Kumar A. HIV-1, HCV and alcohol in the CNS: potential interactions and effects on neuroinflammation. Current HIV Research. 2014;12:282–292. doi: 10.2174/1570162x12666140721122956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinclair JG, Lo GF. Ethanol blocks tetanic and calcium-induced long-term potentiation in the hippocampal slice. General Pharmacology. 1986;17:231–233. doi: 10.1016/0306-3623(86)90144-8. [DOI] [PubMed] [Google Scholar]
- Smiley JF, Saito M, Bleiwas C, Masiello K, Ardekani B, Guilfoyle DN, Gerum S, Wilson DA, Vadasz C. Selective reduction of cerebral cortex GABA neurons in a late gestation model of fetal alcohol spectrum disorder. Alcohol. 2015;49:571–580. doi: 10.1016/j.alcohol.2015.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smolen TN, Smolen A. Blood and brain ethanol concentrations during absorption and distribution in long-sleep and short-sleep mice. Alcohol. 1989;6:33–38. doi: 10.1016/0741-8329(89)90070-0. [DOI] [PubMed] [Google Scholar]
- Spanos M, Besheer J, Hodge CW. Increased sensitivity to alcohol induced changes in ERK Map kinase phosphorylation and memory disruption in adolescent as compared to adult C57BL/6J mice. Behavioural Brain Research. 2012;230:158–166. doi: 10.1016/j.bbr.2012.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steffensen SC, Campbell IL, Henriksen SJ. Site-specific hippocampal pathophysiology due to cerebral overexpression of interleukin-6 in transgenic mice. Brain Research. 1994;652:149–153. doi: 10.1016/0006-8993(94)90329-8. [DOI] [PubMed] [Google Scholar]
- Stellwagen D, Malenka RC. Synaptic scaling mediated by glial TNF-alpha. Nature. 2006;440:1054–1059. doi: 10.1038/nature04671. [DOI] [PubMed] [Google Scholar]
- Sukoff Rizzo SJ, Neal SJ, Hughes ZA, Beyna M, Rosenzweig-Lipson S, Moss SJ, Brandon NJ. Evidence for sustained elevation of IL-6 in the CNS as a key contributor of depressive-like phenotypes. Transl Psychiatry. 2012;2:e199. doi: 10.1038/tp.2012.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sweatt JD. The neuronal MAP kinase cascade: a biochemical signal integration system subserving synaptic plasticity and memory. Journal of Neurochemistry. 2001;76:1–10. doi: 10.1046/j.1471-4159.2001.00054.x. [DOI] [PubMed] [Google Scholar]
- Tancredi V, D'Antuono M, Cafe C, Giovedi S, Bue MC, D'Arcangelo G, Onofri F, Benfenati F. The inhibitory effects of interleukin-6 on synaptic plasticity in the rat hippocampus are associated with an inhibition of mitogen-activated protein kinase ERK. Journal of Neurochemistry. 2000;75:634–643. doi: 10.1046/j.1471-4159.2000.0750634.x. [DOI] [PubMed] [Google Scholar]
- Tancredi V, D'Arcangelo G, Grassi F, Tarroni P, Palmieri G, Santoni A, Eusebi F. Tumor necrosis factor alters synaptic transmission in rat hippocampal slices. Neuroscience Letters. 1992;146:176–178. doi: 10.1016/0304-3940(92)90071-e. [DOI] [PubMed] [Google Scholar]
- Teng SX, Molina PE. Acute alcohol intoxication prolongs neuroinflammation without exacerbating neurobehavioral dysfunction following mild traumatic brain injury. Journal of Neurotrauma. 2014;31:378–386. doi: 10.1089/neu.2013.3093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tipps ME, Raybuck JD, Lattal KM. Substance abuse, memory, and post-traumatic stress disorder. Neurobiology of Learning and Memory. 2014;112:87–100. doi: 10.1016/j.nlm.2013.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiwari V, Kuhad A, Chopra K. Suppression of neuro-inflammatory signaling cascade by tocotrienol can prevent chronic alcohol-induced cognitive dysfunction in rats. Behavioural Brain Research. 2009;203:296–303. doi: 10.1016/j.bbr.2009.05.016. [DOI] [PubMed] [Google Scholar]
- Trapero I, Cauli O. Interleukin 6 and cognitive dysfunction. Metabolic Brain Disease. 2014;29:593–608. doi: 10.1007/s11011-014-9551-2. [DOI] [PubMed] [Google Scholar]
- Udomuksorn W, Mukem S, Kumarnsit E, Vongvatcharanon S, Vongvatcharanon U. Effects of alcohol administration during adulthood on parvalbumin and glial fibrillary acidic protein immunoreactivity in the rat cerebral cortex. Acta Histochemica. 2011;113:283–289. doi: 10.1016/j.acthis.2009.11.001. [DOI] [PubMed] [Google Scholar]
- Valles SL, Blanco AM, Pascual M, Guerri C. Chronic ethanol treatment enhances inflammatory mediators and cell death in the brain and in astrocytes. Brain Pathology. 2004;14:365–371. doi: 10.1111/j.1750-3639.2004.tb00079.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vallieres L, Campbell IL, Gage FH, Sawchenko PE. Reduced hippocampal neurogenesis in adult transgenic mice with chronic astrocytic production of interleukin-6. Journal of Neuroscience. 2002;22:486–492. doi: 10.1523/JNEUROSCI.22-02-00486.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vollenweider F, Herrmann M, Otten U, Nitsch C. Interleukin-6 receptor expression and localization after transient global ischemia in gerbil hippocampus. Neuroscience Letters. 2003;341:49–52. doi: 10.1016/s0304-3940(03)00136-8. [DOI] [PubMed] [Google Scholar]
- Vongvatcharanon U, Mukem S, Udomuksorn W, Kumarsit E, Vongvatcharanon S. Alcohol administration during adulthood induces alterations of parvalbumin and glial fibrillary acidic protein immunoreactivity in rat hippocampus and cingulate cortex. Acta Histochemica. 2010;112:392–401. doi: 10.1016/j.acthis.2009.04.001. [DOI] [PubMed] [Google Scholar]
- Ward RJ, Colivicchi MA, Allen R, Schol F, Lallemand F, de Witte P, Ballini C, Corte LD, Dexter D. Neuro-inflammation induced in the hippocampus of 'binge drinking' rats may be mediated by elevated extracellular glutamate content. Journal of Neurochemistry. 2009;111:1119–1128. doi: 10.1111/j.1471-4159.2009.06389.x. [DOI] [PubMed] [Google Scholar]
- Ward RJ, Lallemand F, de Witte P. Influence of adolescent heavy session drinking on the systemic and brain innate immune system. Alcohol and Alcoholism. 2014;49:193–197. doi: 10.1093/alcalc/agu002. [DOI] [PubMed] [Google Scholar]
- Wei H, Alberts I, Li X. Brain IL-6 and autism. Neuroscience. 2013;252:320–325. doi: 10.1016/j.neuroscience.2013.08.025. [DOI] [PubMed] [Google Scholar]
- Wei W, Faria LC, Mody I. Low ethanol concentrations selectively augment the tonic inhibition mediated by delta subunit-containing GABAA receptors in hippocampal neurons. Journal of Neuroscience. 2004;24:8379–8382. doi: 10.1523/JNEUROSCI.2040-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiner JL, Valenzuela CF. Ethanol modulation of GABAergic transmission: the view from the slice. Pharmacology and Therapeutics. 2006;111:533–554. doi: 10.1016/j.pharmthera.2005.11.002. [DOI] [PubMed] [Google Scholar]
- Wheeler D, Knapp E, Bandaru VV, Wang Y, Knorr D, Poirier C, Mattson MP, Geiger JD, Haughey NJ. Tumor necrosis factor-alpha-induced neutral sphingomyelinase-2 modulates synaptic plasticity by controlling the membrane insertion of NMDA receptors. Journal of Neurochemistry. 2009;109:1237–1249. doi: 10.1111/j.1471-4159.2009.06038.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White AM. What happened? Alcohol, memory blackouts, and the brain. Alcohol Res Health. 2003;27:186–196. [PMC free article] [PubMed] [Google Scholar]
- White AM, Swartzwelder HS. Hippocampal function during adolescence: a unique target of ethanol effects. Annals of the New York Academy of Sciences. 2004;1021:206–220. doi: 10.1196/annals.1308.026. [DOI] [PubMed] [Google Scholar]
- Wirkner K, Poelchen W, Koles L, Muhlberg K, Scheibler P, Allgaier C, Illes P. Ethanol-induced inhibition of NMDA receptor channels. Neurochemistry International. 1999;35:153–162. doi: 10.1016/s0197-0186(99)00057-1. [DOI] [PubMed] [Google Scholar]
- Yang S, Liu ZW, Wen L, Qiao HF, Zhou WX, Zhang YX. Interleukin-1beta enhances NMDA receptor-mediated current but inhibits excitatory synaptic transmission. Brain Research. 2005;1034:172–179. doi: 10.1016/j.brainres.2004.11.018. [DOI] [PubMed] [Google Scholar]
- Young JJ, Bruno D, Pomara N. A review of the relationship between proinflammatory cytokines and major depressive disorder. Journal of Affective Disorders. 2014;169:15–20. doi: 10.1016/j.jad.2014.07.032. [DOI] [PubMed] [Google Scholar]
- Zhang R, Sun L, Hayashi Y, Liu X, Koyama S, Wu Z, Nakanishi H. Acute p38-mediated inhibition of NMDA-induced outward currents in hippocampal CA1 neurons by interleukin-1beta. Neurobiology of Disease. 2010;38:68–77. doi: 10.1016/j.nbd.2009.12.028. [DOI] [PubMed] [Google Scholar]
- Zhang Y, Wei G, Di Z, Zhao Q. miR-339-5p inhibits alcohol-induced brain inflammation through regulating NF-kappaB pathway. Biochemical and Biophysical Research Communications. 2014;452:450–456. doi: 10.1016/j.bbrc.2014.08.092. [DOI] [PubMed] [Google Scholar]
- Zhao YN, Wang F, Fan YX, Ping GF, Yang JY, Wu CF. Activated microglia are implicated in cognitive deficits, neuronal death, and successful recovery following intermittent ethanol exposure. Behavioural Brain Research. 2013;236:270–282. doi: 10.1016/j.bbr.2012.08.052. [DOI] [PubMed] [Google Scholar]
- Zhu B, Dong Y, Xu Z, Gompf HS, Ward SA, Xue Z, Miao C, Zhang Y, Chamberlin NL, Xie Z. Sleep disturbance induces neuroinflammation and impairment of learning and memory. Neurobiology of Disease. 2012;48:348–355. doi: 10.1016/j.nbd.2012.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zorumski CF, Mennerick S, Izumi Y. Acute and chronic effects of ethanol on learning-related synaptic plasticity. Alcohol. 2014;48:1–17. doi: 10.1016/j.alcohol.2013.09.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zucker RS. Exocytosis: a molecular and physiological perspective. Neuron. 1996;17:1049–1055. doi: 10.1016/s0896-6273(00)80238-x. [DOI] [PubMed] [Google Scholar]
- Zucker RS, Regehr WG. Short-term synaptic plasticity. Annual Review of Physiology. 2002;64:355–405. doi: 10.1146/annurev.physiol.64.092501.114547. [DOI] [PubMed] [Google Scholar]