Abstract
This paper presents a systematic review of the quantitative HIV research that assessed the relationships between religion, spirituality, HIV syndemics, and individual HIV syndemics-related health conditions (e.g. depression, substance abuse, HIV risk) among men who have sex with men (MSM) in the United States. No quantitative studies were found that assessed the relationships between HIV syndemics, religion, and spirituality. Nine studies, with 13 statistical analyses, were found that examined the relationships between individual HIV syndemics-related health conditions, religion, and spirituality. Among the 13 analyses, religion and spirituality were found to have mixed relationships with HIV syndemics-related health conditions (6 nonsignificant associations; 5 negative associations; 2 positive associations). Given the overall lack of inclusion of religion and spirituality in HIV syndemics research, a conceptual model that hypothesizes the potential interactions of religion and spirituality with HIV syndemics-related health conditions is presented. The implications of the model for MSM’s health are outlined.
Keywords: HIV/AIDS, Syndemics, Religion, Spirituality, Men who have sex with men
Introduction
HIV is a major public health concern and continues despite decades of research and prevention initiatives. Men who have sex with men (MSM) continue to be disproportionately affected by HIV in the United States [1]. In 2011 MSM comprised 79 % of new HIV infections among men [1], although they only accounted for 4 % of the male population. Furthermore, among MSM, Black and Latino men have been found to be disproportionately affected by HIV as they represented 39 and 29 % of new HIV infections, respectively, in 2011 [2]. Several decades into the HIV epidemic, MSM are still overwhelmingly burdened by this disease.
Initially, HIV prevention research focused on individual risk factors (e.g. condomless sex, drug use, sexual stigma) but has progressed to studying the influence of syndemics [3]. Syndemics are conceptualized as two or more co-occurring, mutually enhancing risk factors (e.g. poverty, racism, homonegativity) or health conditions (substance use, depression, sexual compulsivity) that intersect to increase the likelihood of disease development [4].The inclusion of syndemics in HIV prevention research has advanced the literature and increasingly examines the effect of the interplay of cultural factors (e.g. racism and homonegativity) and syndemics on HIV.
However, religion and spirituality are two important cultural factors that continue to be understudied in the HIV literature. Religion and spirituality are overlapping but distinct constructs that focus on one’s relationship with the sacred [5]. Whereas spirituality is most often defined as a, multidimensional, and transcendent relationship with the sacred that is free of boundaries, religion tends to be defined by its boundaries in its creation of specific rules and criteria for engagement with the sacred [6]. Religion also embraces nonspiritual, social concerns such as politics and economics, whereas spirituality is most often viewed as a unique experience that varies for each person. These factors have the potential to moderate, mediate, and directly influence how syndemics impact the overall health of MSM [7]. The broader epidemiology of religion literature [7–9] presents compelling evidence that religion and spirituality may influence health via several mechanisms: (1) the regulation of individual lifestyles and health behaviors, (2) provision of social resources (e.g. social ties, formal and informal support), (3) promotion of positive self-perceptions (e.g. self-esteem, feelings of personal mastery), (4) provision of specific coping resources (i.e. particular cognitive or behavioral responses to stress), (5) generation of other positive emotions (e.g. love, forgiveness), (6) promotion of health beliefs, and (7) “…healing bioenergy (and other supernatural influences)” [7].
The influences of religion and spirituality on health via these mechanisms have generally been studied using several models that propose that (1) religion and spirituality act as preventive agents for negative health outcomes, (2) religious and spiritual practices increase or decrease depending on the stressors one experiences in his environment, (3) religion and spirituality act as moderators for health behaviors and outcomes among people with high levels of stress, and (4) religion and spirituality provide counterbalancing, salutary effects on health outcomes [7]. While there is substantial evidence of these effects of religion and spirituality on the health of general populations (i.e. most often presumed heterosexual samples) [5–7, 9, 10], there is a dearth of research on this topic related specifically to MSM. Furthermore, there is no integrative theoretical model that addresses religion and spirituality’s influences on HIV syndemics among MSM. Such a model may prove useful in addressing HIV treatment and prevention among MSM.
Religion and spirituality are important factors in many LGBT people’s lives. The Pew Research Center [11] found that 51 % of LGBT adults reported being religiously affiliated and 17 % of those people reported that religion was very important in their lives. Among gay and bisexual men 52 and 51 %, respectively, reported having a religious affiliation [11]. These numbers indicated that religion is a highly salient factor in the lives of gay, bisexual, and other MSM. Spirituality is also an important factor in many LGBT people’s lives [12, 13] and encompasses one’s personal connection with her or his higher power(s). Religion and spirituality are also significantly associated with several mental and physical health outcomes [14] and can function as both risk and protective factors for negative health outcomes [15]. The duality of religion and spirituality is a significant aspect of these forces and more research is needed to understand how to maximize their health inducing qualities and minimize the deleterious ones.
Religion and spirituality may be particularly salient for MSM people of color and thus may influence their health in significantly different ways than their white counterparts. For example, Black MSM are more likely to report that religion and spirituality are very important to them compared to their counterparts of other races [16]. Furthermore, participating in religious rituals and attending religious services are activities that provide strong cultural bonds for many Black and Latino MSM with their racial and ethnic communities [17] as well as other MSM [18]. In addition, MSM of color have been found to use spirituality as a coping mechanism for homonegativity [18] and illness [19]. Given these findings, it might be expected that any associations of religion and spirituality with syndemics may be influenced by race.
This paper aims to examine the influences of religion and spirituality on the health of MSM and provide a conceptual framework for incorporating those factors into HIV research with MSM. Specifically, this paper will present a systematic review of the published, scholarly literature on religion, spirituality, and HIV syndemics and syndemics-related health conditions [3] (i.e. depression, substance use, intimate partner violence, childhood sexual abuse, and HIV risk behavior) among MSM. This paper also attempts to expand the HIV prevention literature by proposing a conceptual model of how religion and spirituality may impact the health of MSM. No such model currently exists and our model is unique in its conceptualization of various aspects of religion and spirituality at the structural, social and individual ecological levels [20] influencing each other and the health of MSM. It is hoped this paper will prove useful in (1) fostering a better understanding of the ways in which religion and spirituality are currently addressed in the HIV syndemics research and (2) providing a conceptual model to help advance HIV prevention scholarship at the intersection of religion, spirituality, and HIV syndemics.
Methods
This systematic review was conducted in accordance with the PRIMSA guidelines [21]. EBSCO Host (all databases described in the Appendix) and PubMed were searched in September and October 2014 for all articles related to syndemics, religion, and spirituality. Several search terms were used to find articles relevant to this systematic review. Exact search terms are described in the Appendix. A total of 36 searches in eight domains (i.e. syndemics, depression, substance use, intimate partner violence, childhood sexual abuse, sexual compulsivity, seroconversion, and HIV risk behavior) were conducted. An example of search terms include: (relig* AND gay AND syndemic); (spirit* AND gay AND syndemic); (relig* AND men who have sex with men AND syndemic); (spirit* AND men who have sex with men AND syndemic); (relig* AND bisexual AND syndemic); and (spirit* AND bisexual AND syndemic). We included the MeSH terms in the search only in the PubMed database. Reference lists of retrieved publications were also examined for any additional relevant publications. No limitations or exclusions were made based on publication date.
Article Selection
All records were reviewed for duplicates. Duplicate and irrelevant records were removed. Then abstracts were reviewed for relevance. They were deemed relevant if they mentioned “religion” “spirituality” and “syndemics” or a syndemics-related health conditions (i.e. depression, substance use, intimate partner violence, childhood sexual abuse, sexual compulsivity, seroconversion, and HIV risk behavior). Next, full articles were reviewed to assess their eligibility criteria. Eligibility criteria was (1) published studies only; (2) scholarly (peer-reviewed) only; (3) sample or subsample had to be comprised of US-residing MSM at time of study; (4) focused on gay or bisexual male/MSM sample or gay or bisexual male/MSM subsample; (5) quantitative methodology; and (6) must contain at least one statistical analysis of the relationship between a religion or spirituality variable and syndemics or a syndemics-related health condition. These inclusion criteria were chosen due to the authors’ desire to examine the relationship between syndemics and syndemics-related health conditions among US-residing MSM, which is consistent with Stall et al.’s [22] original syndemics theory that focused on US-residing MSM. Furthermore, while qualitative studies enrich the literature with personal accounts that uncover new or understudied phenomena and contextualize quantitative data, this study aimed to assess the quantitative relationships between religion, spirituality, and syndemics and syndemics-related health conditions. Therefore, only quantitative studies were included. Editorials, letters, technical reports, dissertations, and commentaries were excluded.
Data Collection Process
The data collection process was conducted in two phases. First, HIV syndemics articles that focused on MSM were assessed for their inclusion of religion or spirituality in their quantitative analyses. Second, studies that included at least one quantitative analysis of the relationship between a religion or spirituality variable and a syndemics-related health condition were assessed to determine the relationship (i.e. significant positive, significant negative, nonsignificant) between the religion or spirituality variable and the syndemics-related health condition. Data about the measures used to assess religion and spirituality was also collected. In addition, the percentage of racial and ethnic minorities and other demographic characteristics of the samples in each study were assessed.
Results
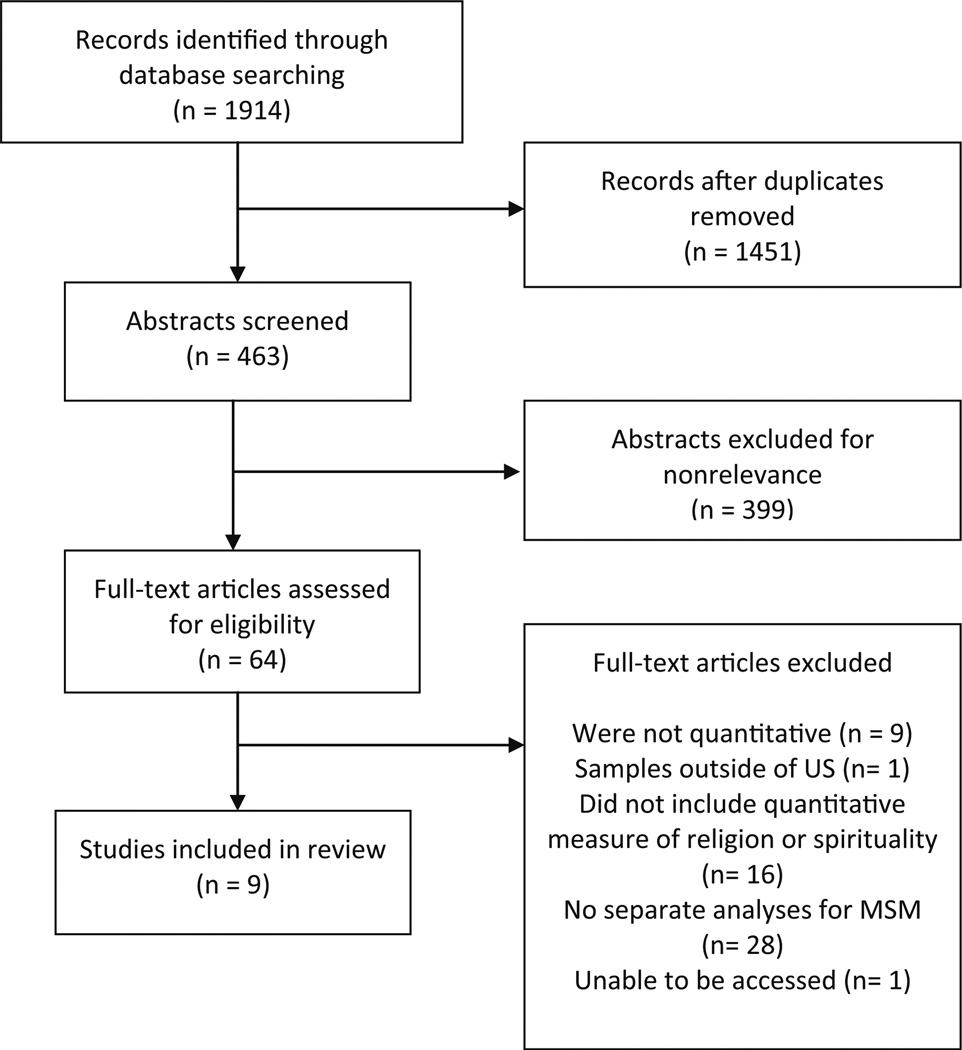
A summary of the article selection process is presented in Fig. 1. No studies that specifically assessed the direct or indirect quantitative relationships between syndemics, religion, and spirituality were found. There were nine studies that quantitatively examined the associations between syndemics-related health conditions, religion, and spirituality (see Table 1). These studies were published between 1992 and 2013. Most of the studies (N = 5) included mostly or only participants from the Western and Southwestern regions and men who identified as either gay or bisexual (N = 7). Four of the studies did not report participants HIV-serostatus, three included only persons living with HIV, and two included both HIV-positive and negative participants.
Fig. 1.
Article selection process.
Table 1.
Summary of findings from studies examining relationship(s) between religion/spirituality and syndemics-related health outcomes for MSM (N = 9)
| Study | N | Health outcome [instrument(s)] |
Religion and/or spirituality included |
Instrument(s) used to study religion and/or spirituality |
Statistical analyses and association(s) between religion/spirituality and health outcome |
Percent of ethnic minorities in analytic sample |
Analytic sample characteristics |
|---|---|---|---|---|---|---|---|
| Leserman et al. [24] |
52 | Depression (Carroll depression scale, Hamilton depression scale, profile of mood states-depression subscale) |
Religion | COPE-turning to religion subscale |
Partial correlations; nonsignificant associations |
23.1a | Mean age: 30.0 Gender: male Geographic region: Southeastern Sexual orientation: gay HIV- serostatus: HIV-positive |
| Richards & Folkman [28] |
125 | Depression (Center for Epidemiological Studies Depression measure) |
Spirituality | Designations into spiritual or not spiritual group based on researcher’s qualitative coding |
T test; significant positive association with being in the spiritual group |
9.0a | Mean age: NR Gender: male Geographic region: Western Sexual orientation: gay HIV- serostatus: NR |
| Wilkerson et al. [25] |
889 | Depression (Center for epidemiological studies depression measure-short form) |
Religion | Duke religion index- attendance, activity, and intrinsic subscales |
Pearson correlations; nonsignificant associations with all three religious variables |
17.7 (Latino = 8.3 %, Black = 5.3 %, Asian = 2.9 %, Other = 9.5 %) |
Mean age: 38.4 Gender: male Geographic region: “16 Us metropolitan statistical areas” Sexual orientation: gay and other MSM HIV- serostatus: HIV-positive and HIV- negative |
| Woods et al. [26] |
106 | Depression (Beck depression inventory) |
Religion | Two instruments (COPE- religious coping subscale and religious service utilization schedule were factor analyzed to produce two factors: religious coping and religious behavior) |
Hierarchal multiple regressions; significant negative association with religious coping; nonsiginificant association with religious behavior |
45.0 (Latino = 30.0 %, Black = 6.0 %) |
Mean age: 35.4 Gender: male Geographic region: Southeastern Sexual orientation: gay or bisexual HIV- serostatus: HIV-positive |
| Eliason et al. [29] |
234 | Substance use (self-report of average number of alcohol drinks per week) |
Religion and spirituality |
Self-reported religious/ spiritual identity |
Moderation analyses via multiple regression; significant positive association |
Specific racial composition of MSM subsample not reported |
Mean age: NR Gender: male Geographic region: “90 % of” of participants “from California” Sexual orientation: gay HIV- serostatus: NR |
| Kipke et al. [30] |
496 | Substance use (self-report of club drug use) |
Religion | Self-reported religious identity |
Multiple logistic regression; Significant negative association |
64.0 (Latino = 40.0 %, Black = 24.0 %) |
Mean age: 20.1 Gender: Male Geographic region: Western Sexual orientation: MSM HIV- serostatus: NR |
| Folkman et al. [27] |
331 | HIV risk behavior (self-report of condomless anal sex in the previous month) |
Spirituality | Study-specific measure of spiritual beliefs and spiritual activities |
Discriminant analysis; nonsignificant association with spiritual beliefs; significant negative association with spiritual activities |
9.0a | Mean age: NR Gender: male Geographic region: Western Sexual orientation: gay and bisexual HIV- serostatus: HIV-positive and HIV- negative |
| Ross et al. [31] |
100 | HIV risk behavior (self-report of the likelihood of condomless anal sex) |
Religion | Self-report of church’s attitudes towards gay sex (from negative to positive) |
Multiple regression; significant negative association |
56.0 (Latino = 22.0 %, Black = 30.0 %, Asian = 1.0 %, Other = 3.0 %) |
Mean age: NR Gender: male Geographic region: Southwestern Sexual orientation: gay and bisexual HIV- serostatus: NR |
| Sikkema et al. [32] |
124 | HIV risk behavior (self-report of condomless oral, anal in the previous 4 months) |
Spirituality | Ways of coping-spiritual coping subscale |
Multiple logistic regression; significant negative association |
84.7 (Latino = 21.0 %, Black = 60.5 %, Other = 3.2 %) |
Mean age: 41.2 Gender: male Geographic region: Northeastern Sexual orientation: MSM HIV- serostatus: HIV-positive |
NR not reported, MSM men who have sex with men
These studies reported race and ethnicity as either “white” or “other” and did not provide details about the racial and ethnic composition of their study samples
Four of the studies focused on depression, two focused on substance use, and three were related to HIV risk behaviors. No studies were found that assessed the quantitative associations between religion or spirituality and intimate partner violence, childhood sexual abuse, sexual compulsivity, or seroconversion. Most of the studies (N = 8) focused on either religion or spirituality. Only one study focused on both religion and spirituality. Approximately half (N = 5) of the studies used some type of formal measure to assess religion or spirituality. Less than half (N = 3) of the studies examined more than one dimension of religion or spirituality in the participants’ lives. Dimensions of religion and spirituality that were examined included religious coping, religious attendance, religious activity, intrinsic religion, religious service utilization, subjective religious identity, spiritual beliefs, spiritual activities, spiritual coping, and churchs’ attitudes towards gay sex. Readers are referred to Idler et al. [23] for an explanation of the multiple dimensions of religion and spirituality as it is outside the scope of this paper.
Out of thirteen statistical tests (across the nine studies), six analyses were found to be nonsignificant [24–27]. There were two positive associations between religion, spirituality, and syndemics-related health conditions. Specifically, spirituality was found to be positively associated with depression [28] and self-reported religious/ spiritual identity was positively associated with alcohol and drug use [29]. There were five negative associations between religion, spirituality, and syndemics-related health conditions. Specifically, religious coping was negatively associated with depression [26], religious identity was negatively associated with club drug use [30], engaging in spiritual activities was negatively associated with condomless anal intercourse [27], one’s church’s positive attitudes towards gay sex were negatively associated with the likelihood of engaging in sex without condoms [31], and spiritual coping was negatively associated with the likelihood of engaging in sex without condoms [32]. There were no discernable differences in significance of results related to dimensions of religion or spirituality (e.g. religious coping versus spiritual activities) measured. Most of the studies (N = 6) used multivariate analyses (e.g. multiple regression, logistic regression). However, there were no discernable differences in significance of results related to whether statistical analyses were multivariate or univariate.
The studies included in this review had varying levels of racial and ethnic diversity in their analytic samples. These percentages ranged from 9 to 84.7 %. Studies that reported higher percentages of racial and ethnic minorities (N = 4) found more significant negative associations between religion, spirituality, and syndemics-related health conditions than studies that did not have high percentages of racial and ethnic minorities (N = 4).
Discussion
Summary of Findings
No published peer-reviewed articles that quantitatively examined the relationships between religion, spirituality, and HIV syndemics among MSM were found in this systematic review. Furthermore, only nine published peer-reviewed articles that quantitatively examined the relationships between religion, spirituality, and HIV syndemics-related health conditions (i.e. depression, substance use, intimate partner violence, childhood sexual abuse, sexual compulsivity, seroconversion, and HIV risk behavior) among MSM were found. Studies with more racially and ethnically diverse samples reported positive effects of religion and spirituality on the health of MSM more than those with mostly white samples. This suggests that religion and spirituality may be more beneficial for the health of MSM of color than for white MSM. Overall the findings suggest that religion and spirituality have mixed effects on the HIV syndemics-related health conditions of MSM.
Implications of Findings
The findings of this study reveal two significant facts. First, the incorporation of religion and spirituality in HIV syndemics quantitative research focused on MSM is nonexistent. Second, the inclusion of religion and spirituality in quantitative HIV syndemics-related health conditions research that is focused on MSM is sparse. This paucity of research related to religion, spirituality, HIV syndemics, and HIV syndemics-related health conditions represents an area for growth in the HIV prevention literature and larger MSM-focused health disparities literature. While qualitative studies focused on MSM [18, 33–36] and quantitative studies focused on LGBT people in general [37–39] have addressed the intersection of religion and spirituality with HIV and other health outcomes, HIV syndemics and HIV syndemics-related health conditions research focused on MSM have yet to do so.
HIV syndemics and other health disparities research with MSM could benefit from a more comprehensive and theoretically driven incorporation of religion and spirituality. Religion has been found to be associated with positive health outcomes and behaviors such as HIV medication adherence [40], quality of life, social support, effective coping strategies and less psychological distress [41]. Positive health effects for persons living with HIV, in general, have been linked to spirituality. Specifically, spirituality has been found to be associated with greater preservation of CD4 cells, lower viral loads [42] and lower salivary cortisol levels [37] in HIV-positive individuals as well as effective coping during difficult times [43] in MSM. Religion and spirituality also have their drawbacks. Homonegative religious experiences have been linked to higher levels of internalized homophobia [12, 44] and can contribute to cognitive dissonance regarding sexual and religious identities [45, 46], feeling isolated from one’s church [47], and decreased sexual orientation disclosure [44]. Of note, is that even in the midst of homonegative and oppressive forces, religion and spirituality can serve as a source of resiliency [48, 49]. For example, religious faith has been found to significantly contribute to resiliency (participants’ ability to handle changes or misfortunes in their lives) [49] among Black LGBT emerging adults even when they had high levels of internalized homonegativity. These findings highlight the multifaceted influences religion and spirituality could have on the health of MSM.
At the end of Stall et al.’s [22] chapter on syndemics, they encouraged the development of a program of research that seriously investigates the health concerns of racial and ethnic minority and low-SES MSM. A focus on MSM of color is especially important, given the disproportionate HIV rates among them [2]. Religion and spirituality have historical importance and significant present-day influences in the lives of racial and ethnic minority MSM [50–52] and the incorporation of these factors into syndemics research may be even more important for this population. Research has found that MSM of color are more likely to consider themselves religious, identify as spiritual, and engage in private prayer [12] as well as attend church [12, 34, 35] more than their white counterparts. Furthermore, MSM of color are likely to be attending non same-sex affirming churches [43, 47, 50] and are thus more susceptible to the negative influences of religion. Any HIV prevention and MSM health disparities research that incorporates religion and spirituality must also seriously consider how these factors intersect with race, ethnicity, and racism.
Conceptual Model for the Influences of Religious and Spiritual Mechanisms on HIV Syndemics & Other Sexual and Mental Health Disparities
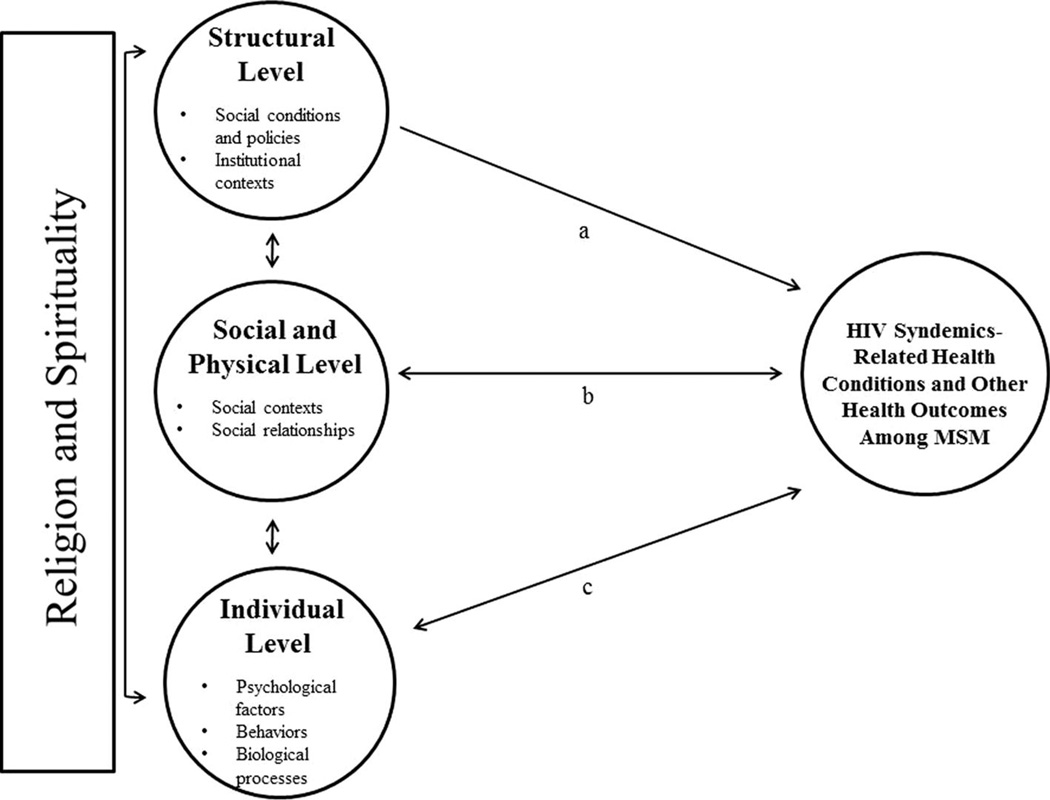
The lack of inclusion of religion and spirituality in quantitative research related to HIV syndemics among MSM, as found in this systematic review, may be due to a lack of a comprehensive framework for thinking about how religion and spirituality may influence the health of MSM. Thus, we propose a conceptual model informed by social ecological theory [53–55], the findings from this systematic review, and findings from religion, spirituality, and health related studies in the broader epidemiology of religion [7, 8, 10, 56, 57] and public health [58, 59] fields. This model highlights the ways in which religion and spirituality may influence the health of MSM (see Fig. 2). We propose that religion and spirituality manifest across three different ecological levels: structural, social and physical, and individual. Religion and spirituality may influence the health of MSM via one of these three levels independently. In addition, the manifestation of religion and spirituality at one level may influence their effects on another level and this multi-level interaction may combine to influence the health of MSM. For example, policies at the structural level (e.g. religious freedom laws that allow private business owners to discriminate against gay customers) that are often supported by homonegative religious beliefs (e.g. “Gays are an abomination against God”) may influence the individual spiritual beliefs of MSM, which combined may contribute to psychological processes that put them at risk for negative health outcomes such as depression.
Fig. 2.
Conceptual model for the influence of religion and spirituality on HIV syndemics-related health conditions and other health outcomes among MSM. Pathway a illustrates the influence of religion and spirituality at the structural level on MSM’s health. No literature in the systematic review provided evidence for this relationship. Pathway b illustrates the influence of religion and spirituality at the social and physical level on MSM’s health. Two analyses out of 13 from the systematic review provided evidence for this relationship [27, 31]. Pathway c illustrates the influence of religion and spirituality at the individual level on MSM’s health. Five analyses out of 13 from the systematic review provided evidence for this relationship [26, 28–30, 32]
The structural level of our conceptual model highlights the impact of religion and spirituality on social conditions and policies and institutional contexts. Little research has specifically investigated the influences of religion and spirituality at the structural level on the health of MSM. While none of the studies found in our systematic review examined the associations between health outcomes and religion or spirituality at the structural level, there has been some evidence to support this relationship. One study found that LGB youth who lived in a county with a religious climate that was supportive of homosexuality had significantly fewer alcohol abuse symptoms and sexual partners [60]. More research is needed to assess how religious and spiritual factors at the structural level may relate to health behaviors and outcomes for MSM.
The social and physical level of our model focuses on the interplay of religion and spirituality with social contexts, social relationships, and physical contexts. Religious and spiritual factors at this level include such factors as religious and spiritual group cohesion and beliefs, religious and spiritual participation, and access to religious and spiritual resources. Four of the studies [25–27, 31] that were found in our systematic review defined religion or spirituality at this level. Two out of 13 analyses (15 %) yielded significant associations between religious variables at this level and health outcomes; thus, providing support for the proposed pathway in the conceptual model [27, 31]. For example, Folkman et al. [27] found that higher levels of participation in spiritual activities were significantly associated with reporting no condomless anal sex in the previous month. HIV research would benefit from investigating how social and physical level religious and spiritual factors (e.g. religious and spiritual economic initiatives and physical spiritual resources) may impact the health of MSM.
The individual level highlights the impact of religion and spirituality on individual psychological factors, behaviors, and biological processes. Eight studies in our review measured religion or spirituality at this level [24– 30, 32]. Religious and spiritual factors at the individual level, such as religious identity, have been linked to both positive and negative health outcomes for MSM. Our review found five out of 13 analyses (38 %) that provided evidence to support the relationship between religion and spirituality at the individual level with health outcomes for MSM [26, 28–30, 32]. For example, Woods et al. [26] found that religious coping was significantly associated with fewer depressive symptoms in a sample of HIV-positive MSM. There is a growing body of research examining religion and spirituality’s influences on individual level psychological and behavioral processes in MSM. However, there has been no research, to date, that has examined religion and spirituality’s impact on the biological processes of MSM specifically. Yet, findings from research in the epidemiology of religion field suggest that religion and spirituality are associated with biological functioning in the general population. Studies have found that religion and spirituality have effects on people’s health via biological processes such as lowering blood pressure [61], oxidative stress [62], and stress hormone levels and reactivity [9]. Among persons living with HIV, in general, religion and spirituality have been found to improve immunological functioning [42]. More research that focuses on religion and spirituality’s influences on the biological processes of MSM is needed. Overall, our review found a higher percentage of analyses with significant associations between religion, spirituality, and health outcomes at the individual level. This finding may be a factor of religion and spirituality actually having stronger influences at the individual level or a byproduct of the higher percentage of studies examining religion, spirituality, and health outcomes at the individual level versus the structural and social and physical levels. More research is needed to determine the primary contributor to this finding.
It should be noted that religious and spiritual factors at all levels in this model are not static but interact with each other in complex ways. While no research studies in our review examined the interplay of religion and spirituality across ecological levels, the larger epidemiology of religion literature provides evidence of bidirectional and mutually influential relationships between levels. For example, religious doctrine may dictate a religious organization’s perspective on homonegativity and thereby influence a gay or bisexual man’s feelings about his personal relationship with the sacred [63]. The studies in our systematic review reported on the unidirectional associations between religion, spirituality, and health outcomes. However, there have been studies that found that certain health outcomes (i.e. HIV seroconversion) are associated with increases in religion and spirituality at the social and physical level and individual level [42]. Thus, there is evidence of a bidirectional relationship between religion and spirituality and health.
Investigators who choose to utilize this model to inform their research are encouraged to measure more than one religious and spiritual factor in their research and take a comprehensive approach that assesses the multidimensional and multilevel influences of religion and spirituality on the health of MSM. For example, instead of only measuring religious and spiritual participation’s (at the social and physical level) effect on HIV risk in MSM, researchers may find it more beneficial to examine how religious and spiritual climate (at the structural level) is associated with religious and spiritual group cohesion (at the social and physical level) and how religious and spiritual group cohesion impacts HIV risk via religious and spiritual identity. In addition, it should be noted that religious and spiritual factors at all levels can have positive, negative, neutral, or mixed associations with the health of MSM. The strengths of these associations are likely influenced (i.e. mediated or moderated) by several factors including lifespan developmental stage, time, sociodemographic factors (e.g. race), and which level the religious or spiritual factor resides in the conceptual model (i.e. factors at the structural level may have less direct impact on the health of MSM than factors at the individual level).
Furthermore, the protective and positive relationships between the health of MSM and religion and spirituality are understudied. Given the homonegative tone of several western religious traditions (i.e. Christianity, Islam, and Judaism), most research has focused on the negative aspects of religion in the lives of MSM. Yet, religion has also been found to be a positive force for many MSM, especially MSM of color. It has been found to be a protective factor against racism [64, 65] and a resilience factor in the face of internalized homonegativity [49]. Furthermore, religious institutions have traditionally been bastions of economic and social support for poor community members [66] including those who are LGBT. Scholarship that expands the knowledgebase about religion and spirituality to the positive psychology spheres can have beneficial implications for the health of MSM.
Limitations
There were some limitations to this study. We only focused on peer-reviewed scholarly literature and did not include editorials, letters, technical reports, theses, dissertations, or commentaries in our review. These excluded publications, while not necessarily scholarly, may have presented more in-depth discourse about religion, spirituality, HIV syndemics, and HIV for MSM. Also, only two databases using specific search terms were used to identify publications for inclusion in this review. The review is most likely to be exhaustive; however, it is possible more publications could have been identified if more databases were searched. To the extent that negative and nonsignificant findings are less likely to be published, there may exist a larger body of data indicating a lack of association between religion, spirituality, HIV syndemics, and HIV syndemics-related health conditions than is evident from the scholarly literature reviewed in this paper.
Readers are encouraged to use caution in generalizing the findings of this review. MSM residing in the US were the target population for this review; therefore, it may be inappropriate to generalize these findings to MSM outside of the US. In addition, most of these studies were conducted with men who openly (at least for the purposes of being included in the studies) identified as gay or bisexual. The influences of religion and spirituality on HIV-syndemics and HIV syndemics-related health conditions may differ for MSM who do not disclose their sexual orientations.
Conclusions
This paper has highlighted the lack of inclusion of religion and spirituality in HIV syndemics research with MSM. It has also provided a conceptual model to help HIV researchers and public health policy makers begin to understand how religion and spirituality may impact the health of MSM. The need for the inclusion of religion and spirituality in HIV and health disparities research with MSM is clearly supported by this systematic review and ways to address that gap are outlined in the conceptual model. HIV researchers and public health policy makers are encouraged to begin to critically examine how religion and spirituality may influence health among MSM and how to use these factors to promote positive health outcomes.
Supplementary Material
Acknowledgments
This project was supported by a supplement to a research grant from the National Institute of Mental Health (R01-DA036466; Jeffrey T. Parsons and Christian Grov, Principal Investigators). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Electronic supplementary material The online version of this article (doi:10.1007/s10461-015-1173-0) contains supplementary material, which is available to authorized users.
References
- 1.Johnson A, Hall H, Hu X, Lansky A, Holtgrave D, Mermin J. Trends in diagnoses of HIV infection in the United States, 2002–2011. JAMA. 2014;312:432–434. doi: 10.1001/jama.2014.8534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.CDC. [Accessed 10 Oct 2014];HIV among African American gay and bisexual men. 2014 Available from: http://www.cdc.gov/hiv/pdf/black_msm_fact_sheet_rev_final.pdf.
- 3.Stall R, Mills TC, Williamson J, Hart T, Greenwood G, Paul J, Pollack L, Binson D, Osmond D, Catania JA. Association of co-occurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. Am J Public Health. 2003;93:939–942. doi: 10.2105/ajph.93.6.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Singer M, Clair S. Syndemics and public health: reconceptualizing disease in bio-social context. Med Anthropol Q. 2003;17:423–441. doi: 10.1525/maq.2003.17.4.423. [DOI] [PubMed] [Google Scholar]
- 5.Zinnbauer B, Pargament K, Cole B, Rye M, Butter M, Belavich T, Hipp K, Scott A, Kadar J. Religion and spirituality: unfuzzying the fuzzy. J Sci Study Relig. 1997;36:549–564. [Google Scholar]
- 6.Miller W, Thoresen C. Spirituality, religion, and health. An emerging research field. Am Psychol. 2003;58:24–35. doi: 10.1037/0003-066x.58.1.24. [DOI] [PubMed] [Google Scholar]
- 7.Ellison C, Levin J. The religion-health connection: evidence, theory, and future directions. Health Educ Behav. 1998;25:700–720. doi: 10.1177/109019819802500603. [DOI] [PubMed] [Google Scholar]
- 8.Aldwin C, Park C, Jeong Y, Nath R. Differing pathways between religiousness, spirituality, and health: a self-regulation perspective. Psycholog Relig Spirit. 2014;6:9–21. [Google Scholar]
- 9.Seeman T, Dubin L, Seeman M. Religiosity/spirituality and health: a critical review of the evidence for biological pathways. Am Psychol. 2003;58:53–63. doi: 10.1037/0003-066x.58.1.53. [DOI] [PubMed] [Google Scholar]
- 10.Powell L, Shahabi L, Thoresen C. Religion and spirituality: linkages to physical health. Am Psychol. 2003;58:36–52. doi: 10.1037/0003-066x.58.1.36. [DOI] [PubMed] [Google Scholar]
- 11.Pew RC. A survey of LGBT Americans attitudes, experiences and values in changing times. Washington, DC: Pew Research Center; 2013. [Google Scholar]
- 12.Barnes DM, Meyer IH. Religious affiliation, internalized homophobia, and mental health in lesbians, gay men, and bisexuals. Am J Orthopsychiatry. 2012;82:505–515. doi: 10.1111/j.1939-0025.2012.01185.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tan P. The importance of spirituality among gay and lesbian individuals. J Homosex. 2005;49:135–144. doi: 10.1300/J082v49n02_08. [DOI] [PubMed] [Google Scholar]
- 14.Swartz C, Bunting M, Fruhauf C, Orel N. The meaning of spirituality in end-of-life decisions among LGBT older adults. In: Orel N, Fruhauf C, editors. The Lives of LGBT older adults: understanding challenges and resilience. Washington, DC: American Psychological Association; 2014. pp. 91–109. [Google Scholar]
- 15.Lassiter J. Extracting dirt from water: a strengths-based approach to religion for African American same-gender-loving men. J Relig Health. 2014;53:178–189. doi: 10.1007/s10943-012-9668-8. [DOI] [PubMed] [Google Scholar]
- 16.O’Leary A, Fisher H, Purcell D, Pilgrim S, Gomez C. Correlates of risk patterns and race/ethnicity among HIV-positive men who have sex with men. AIDS Behav. 2007;11:706–715. doi: 10.1007/s10461-006-9205-4. [DOI] [PubMed] [Google Scholar]
- 17.Williams J, Wyatt G, Resell J, Peterson J, Asuan-O’Brien A. Psychosocial issues among gay- and non-gay-identifying HIV-seropositive African American and Latino MSM. Cultur Divers Ethnic Minor Psychol. 2004;10:268–286. doi: 10.1037/1099-9809.10.3.268. [DOI] [PubMed] [Google Scholar]
- 18.Jeffries WL, Dodge B, Sandfort TG. Religion and spirituality among bisexual Black men in the USA. Cult Health Sex. 2008;10:463–477. doi: 10.1080/13691050701877526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Miller R. Look at what God can do: African American gay men, AIDS, and spirituality. J HIV AIDS Soc Serv. 2005;4:25–46. [Google Scholar]
- 20.Bronfenbrenner U. Ecological models of human development. In: Gauvain M, Cole M, editors. Readings on the development of children. 2nd Ed. NY: Freeman; 1993. pp. 37–43. [Google Scholar]
- 21.Liberati A, Altman D, Tetzlaff J, Mulrow C, Gøtzsche P, Ioan-nidis J, Clarke M, Devereaux P, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. Ann Intern Med. 2009;151:65–94. doi: 10.7326/0003-4819-151-4-200908180-00136. [DOI] [PubMed] [Google Scholar]
- 22.Stall R, Friedman M, Catania J. Interacting epidemics and gay men’s health: a theory of syndemic production among urban gay men. In: Wolitski J, Stall R, Valdiserri R, editors. Unequal opportunity: health disparities affecting gay and bisexual men in the United States. New York: Oxford University Press; 2008. pp. 251–274. [Google Scholar]
- 23.Idler E, Musick M, Ellison C, George L, Krause N, Ory M, Pargament K, Powell L, Underwood L, Williams D. Measuring multiple dimensions of religion and spirituality for health research: conceptual background and findings from the 1998 General Social Survey. Res Aging. 2003;25:327–65. [Google Scholar]
- 24.Leserman J, Perkins DO, Evans DL. Coping with the threat of AIDS: the role of social support. Am J Psychiatry. 1992;149:1514–1520. doi: 10.1176/ajp.149.11.1514. [DOI] [PubMed] [Google Scholar]
- 25.Wilkerson JM, Smolensk DJ, Brady SS, Rosser BR. Performance of the Duke Religion Index and the spiritual well-being scale in online samples of men who have sex with men. J Relig Health. 2013;52:610–621. doi: 10.1007/s10943-012-9594-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Woods T, Antoni M, Ironson G, Kling D. Religiosity is associated with affective and immune status in symptomatic HIV-in-fected gay men. J Psychosom Res. 1999;46:165–176. doi: 10.1016/s0022-3999(98)00078-6. [DOI] [PubMed] [Google Scholar]
- 27.Folkman S, Chesney M, Pollack L, Phillips C. Stress, coping, and high-risk sexual behavior. Health Psychol. 1992;11:218–222. doi: 10.1037//0278-6133.11.4.218. [DOI] [PubMed] [Google Scholar]
- 28.Richards T, Folkman S. Spiritual aspects of loss at the time of a partner’s death from AIDS. Death Stud. 1997;21:527–552. doi: 10.1080/074811897201769. [DOI] [PubMed] [Google Scholar]
- 29.Eliason M, Burke A, van Olphen J, Howell R. Complex interactions of sexual identity, sex/gender, and religious/spiritual identity on substance use among college students. Sex Res Soc Policy. 2011;8:117–125. [Google Scholar]
- 30.Kipke MD, Weiss G, Ramirez M, Dorey F, Ritt-Olson A, Iverson E, Ford W. Club drug use in los angeles among young men who have sex with men. Subst Use Misuse. 2007;42:1723–1743. doi: 10.1080/10826080701212261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ross M, Henry D, Freeman A, Caughy M, Dawson A. Environmental influences on safer sex in young gay men: a situational presentation approach to measuring influences on sexual health. Arch Sex Behav. 2004;33:249–257. doi: 10.1023/B:ASEB.0000026624.69223.5f. [DOI] [PubMed] [Google Scholar]
- 32.Sikkema K, Hansen NB, Meade C, Kochman A, Fox A. Psychosocial predictors of sexual HIV transmission risk behavior among HIV-positive adults with a sexual abuse history in childhood. Arch Sex Behav. 2009;38:121–134. doi: 10.1007/s10508-007-9238-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Balaji AB, Oster AM, Viall AH, Heffelfinger JD, Mena LA, Toledo CA. Role flexing: how community, religion, and family shape the experiences of young black men who have sex with men. AIDS Patient Care STDS. 2012;26:730–737. doi: 10.1089/apc.2012.0177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jeffries WLt, Okeke JO, Gelaude DJ, Torrone EA, Gasiorowicz M, Oster AM, McCree DH, Bertolli J. An exploration of religion and spirituality among young, HIV-infected gay and bisexual men in the USA. Cult Health Sex. 2014;16:1070–1083. doi: 10.1080/13691058.2014.928370. [DOI] [PubMed] [Google Scholar]
- 35.Garcia DI, Gray-Stanley J, Ramirez-Valles J. “The priest obviously doesn’t know that I’m gay”: the religious and spiritual journeys of Latino gay men. J Homosex. 2008;55:411–436. doi: 10.1080/00918360802345149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kubicek K, McDavitt B, Carpineto J, Weiss G, Iverson E, Kipke MD. “God made me gay for a reason”: young men who have sex with men’s resiliency in resolving internalized homophobia from religious sources. J Adolesc Res. 2009;24:601–633. doi: 10.1177/0743558409341078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bormann JE, Aschbacher K, Wetherell JL, Roesch S, Redwine L. Effects of faith/assurance on cortisol levels are enhanced by a spiritual mantram intervention in adults with HIV: a randomized trial. J Psychosom Res. 2009;66:161–171. doi: 10.1016/j.jpsychores.2008.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Szaflarski M, Ritchey PN, Leonard AC, Mrus JM, Peterman AH, Ellison CG, McCullough ME, Tsevat J. Modeling the effects of spirituality/religion on patients’ perceptions of living with HIV/ AIDS. J Gen Intern Med. 2006;21(Suppl 5):S28–S38. doi: 10.1111/j.1525-1497.2006.00646.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vance DE, Brennan M, Enah C, Smith GL, Kaur J. Religion, spirituality, and older adults with HIV: critical personal and social resources for an aging epidemic. Clin Interv Aging. 2011;6:101–109. doi: 10.2147/CIA.S16349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nightingale VR, Sher TG, Thilges S, Niel K, Rolfsen N, Hansen NB. Non-conventional practices and immune functioning among individuals receiving conventional care for HIV. J Health Psychol. 2011;16:1241–1250. doi: 10.1177/1359105311405350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Suzuki-Crumly J, Ackerman M, Vance D, Antia L, Blanshan S, Smith B, Bodner E, Hiers K. The roel of religiosity in mediating biopsychosocial outcome in homosexual and heterosexual with HIV: a structural equation modeling comparision study. J Spirit Mental Health. 2010;12:209–223. [Google Scholar]
- 42.Ironson G, Stuetzle R, Fletcher MA. An increase in religiousness/ spirituality occurs after HIV diagnosis and predicts slower disease progression over 4 years in people with HIV. J Gen Intern Med. 2006;21(Suppl 5):S62–S68. doi: 10.1111/j.1525-1497.2006.00648.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Foster M, Arnold E, Rebchook G, Kegeles S. ‘It’s my inner strength’: spirituality, religion and HIV in the lives of young African American men who have sex with men. Cult Health Sex. 2011;13:1103–1117. doi: 10.1080/13691058.2011.600460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wilkerson JM, Smolenski DJ, Brady SS, Rosser BR. Religiosity, internalized homonegativity, and outness in Christian men who have sex with men. Sex Relat Ther. 2012;27:122–132. doi: 10.1080/14681994.2012.698259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lassiter J. Reconciling sexual orientation and Christianity: black same-gender loving men’s experiences. Ment Health Relig Cult. 2015 doi: 10.1080/13674676.2015.1056121. [Google Scholar]
- 46.Pitt R. ‘Still looking for my Jonathan’: gay Black men’s management of religious and sexual identity conflicts. J Homosex. 2010;57:39–53. doi: 10.1080/00918360903285566. [DOI] [PubMed] [Google Scholar]
- 47.Rhodes SD, Hergenrather KC, Vissman AT, Stowers J, Davis AB, Hannah A, Alonzo J, Marsiglia FF. Boys must be men, and men must have sex with women: a qualitative CBPR study to explore sexual risk among African American, Latino, and White gay men and MSM. Am J Mens Health. 2011;5:140–151. doi: 10.1177/1557988310366298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chaudoir S, Norton W, Earnshaw V, Moneyham L, Mugavero M, Hiers K. Coping with HIV stigma: do proactive coping and spiritual peace buffer the effect of stigma on depression? AIDS Behav. 2012;16:2382–2391. doi: 10.1007/s10461-011-0039-3. [DOI] [PubMed] [Google Scholar]
- 49.Walker JJ, Longmire-Avital B. The impact of religious faith and internalized homonegativity on resiliency for black lesbian, gay, and bisexual emerging adults. Dev Psychol. 2013;49:1723–1731. doi: 10.1037/a0031059. [DOI] [PubMed] [Google Scholar]
- 50.Boykin K. One more river to cross: Black and gay in America. New York: Anchor Books; 1996. [Google Scholar]
- 51.Miller R. Legacy denied: African American gay men, AIDS, and the black church. Soc Work. 2007;52:51–61. doi: 10.1093/sw/52.1.51. [DOI] [PubMed] [Google Scholar]
- 52.Webb J. In broad daylight. In: James G, Moore L, editors. Spirited: affirming the soul and Black gay/lesbian identity. Washington, DC: Redbone Press; 2006. [Google Scholar]
- 53.Baral S, Logie C, Grosso A, Wirtz A, Beyrer C. Modified social ecological model: a tool to guide the assessment of the risks and risk contexts of HIV epidemics. BMC Public Health. 2013;13:1–8. doi: 10.1186/1471-2458-13-482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bekalu M, Eggermont S. The role of communication inequality in mediating the impacts of socioecological and socioeconomic disparities on HIV/AIDS knowledge and risk perception. Int J Equity Health. 2014;13(1):1–14. doi: 10.1186/1475-9276-13-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Naar-King S, Montepie dra G, Garvie P, Kammerer B, Malee K, Sirois P, Aaron L, Nichols S, Team PPs. Social ecological predictors of longitudinal HIV treatment adherence in youth with perinatally acquired HIV. J Pediatr Psychol. 2013;38:664–674. doi: 10.1093/jpepsy/jst017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Aukst-Margetic B, Margetic B. Religiosity and health outcomes: review of literature. Coll Antropol. 2005;29:365–371. [PubMed] [Google Scholar]
- 57.Masters K, Spielmans G. Prayer and health: review, meta-analysis, and research agenda. J Behav Med. 2007;30:329–338. doi: 10.1007/s10865-007-9106-7. [DOI] [PubMed] [Google Scholar]
- 58.Levin J. Spiritual determinants of health and healing: an epidemologic perspective on salutogenic mechanisms. Altern Ther Health Med. 2003;9:48–57. [PubMed] [Google Scholar]
- 59.Van Ness P. Religion and public health. J Relig Health. 1999;38:15–26. [Google Scholar]
- 60.Hatzenbuehler ML, Pachankis JE, Wolff J. Religious climate and health risk behaviors in sexual minority youths: a population-based study. Am J Public Health. 2012;102:657–663. doi: 10.2105/AJPH.2011.300517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Schneider R, Staggers F, Alexander C, Sheppard W, Rainforth M, Kondwani K, Smith S, King C. A randomized controlled trial of stress reduction for hypertension in older African Americans. Hypertension. 1995;26:820–827. doi: 10.1161/01.hyp.26.5.820. [DOI] [PubMed] [Google Scholar]
- 62.Schneider R, Nidich S, Salerno J, Sharma H, Robinson C, Nidich R, Alexander C. Lower lipid peroxide levels in practitioners of the transcendental meditation program. Psychosom Med. 1998;60:38–41. doi: 10.1097/00006842-199801000-00008. [DOI] [PubMed] [Google Scholar]
- 63.Griffin H. Their own receive them not: Black American lesbians and gays in Black churches. Cleveland, OH: Pilgrim Press; 2006. [Google Scholar]
- 64.Bowleg L, Huang J, Brooks K, Black A, Burkholder G. Triple jeopardy and beyond: multiple minority stress and resilience among Black lesbians. J Lesbian Stud. 2003;7(4):87–108. doi: 10.1300/J155v07n04_06. [DOI] [PubMed] [Google Scholar]
- 65.Brown D. African American resiliency: examining racial socialization and social support as protective factors. J Black Psychol. 2008;34:32–48. [Google Scholar]
- 66.Harrison H, Wobbenhorst W, Waits M, Hurt A. The role of the Black church in economic and community development efforts: a workforce development case study. Soc Work Christ. 2006;33:288–305. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.