Abstract
[Purpose] This study investigated the effects of resistance exercise on cardiopulmonary functions in young sedentary subjects. [Subjects] Forty-two young and healthy subjects with a sedentary lifestyle were included in this study. [Methods] The subjects were randomly divided into 2 groups: control and experimental. The control group (n=21) received health education and continued with normal activities of daily living. The experimental group (n=21) underwent resistance training, health education, and continued with normal activities of daily living. The resistance exercise program consisted of 3 postural exercises: chest press, dumbbell pullover, and flat-bench dumbbell fly. The subjects received this intervention 3 times/week for 8 weeks. [Results] The baseline characteristics were comparable between the 2 groups. The 6-minute-walk test score, peak expiratory flow, forced vital capacity, forced expiratory volume in 1 second, maximal voluntary ventilation, and chest expansions were significantly improved post-intervention in the experimental group and between the 2 groups. [Conclusion] Cardiopulmonary functions in young sedentary subjects were significantly improved with the 8-week resistance exercise program.
Key words: Resistance exercise, Lung function, Sedentary lifestyle
INTRODUCTION
Resistance exercise involves continuous increase in resistance and duration. This type of exercise is used for improving strength, endurance, and muscle power. A previous study conducted by Fiatarone et al. involved 9 subjects with a mean age of 90 years (standard deviation [SD] 1 year)1). The program involved performance of the quadriceps exercise with resistance for 8 weeks. At the end of the study, the quadriceps muscles had improved in strength and balance. This resistance exercise is recommended in the elderly and is used widely in home care facilities in the United States. These data were limited only to the elderly.
A sedentary lifestyle is defined as a lack of regular exercise fewer than 25 minutes per day2). It is associated with obesity and metabolic syndrome, resulting in impaired cardiopulmonary function or increased risk of cardiovascular diseases1,2,3). Effects of resistance exercise in subjects with a sedentary lifestyle are limited. Here, we aimed to investigate the effects of resistance exercise on cardiopulmonary functions in young Thai adults with a sedentary lifestyle.
SUBJECTS AND METHODS
The study was conducted at the Khon Kaen University. The inclusion criteria were as follows: subjects over 15 years of age, who had no co-morbid diseases; those who did not take any medications or bronchodilators; and those who did not have a regular exercise schedule in the past 6 months.
The eligible subjects were randomly divided into control and experimental groups, using a simple random sampling method. The control group received basic instructions on health education, whereas the experimental group received the same health education as that given to the control group and resistance exercise for 8 consecutive weeks. The exercises were performed 3 times a week as per the recommendations in the 1998 American College of Sports Medicine guidelines. Each session consisted of 10 minutes of warm-up stretches, resistance exercise for 25 minutes, and 10 minutes of cool-down stretches.
The subjects in the experimental group participated in 3 types of exercises: chest press, dumbbell pullover, and flat-bench dumbbell fly4). Each exercise was carried out as a set of 10 repetitions, 3 sets/day, for 3 days/week. Each set consisted of 100% of 10 repetition maximum (RM), 75% of 10 RM, and 50% of 10 RM.
The baseline characteristics of all subjects were recorded at the beginning of the study, which included age, height, weight, blood pressure, and pulse rate. Cardiopulmonary outcomes were measured at the beginning and at the end of the study. These outcomes were a 6-minute walk test (6MWT) score, peak expiratory flow (PEF), forced vital capacity (FVC), forced expiratory volume in 1 second (FEV1), maximal voluntary ventilation (MVV), and chest expansions. The pulmonary function tests were performed using a spirometer (CONMED pony FX, Italy). The subjects were instructed to refrain from eating and drinking for at least 1 hour before the measurements. The details of each measurement were as follows:
6MWT: This test was used to measure cardiovascular endurance. For this test, the subjects walked in a square for 6 minutes, with no breaks; this was repeated twice. The longest distance was measured and recorded5, 6).
Lung function test7, 8): The volunteers were instructed in the operation of tools, related to the spirometer, which measured different values. Then, all components of the spirometer were checked to see if they were in a good condition. Each volunteer was asked to hold the flow sensor to enter data into the spirometer, which included the date, ID number, age, height, and gender.
Vital capacity measurement (VC): The VC and start buttons were pressed by the researcher so that the graph correlated to the VC. The mouthpiece was held by the volunteer in his mouth; the volunteer also had a clip on his nose. The volunteer then inhaled and exhaled normally 3 times, which was followed by deep inhalation and exhalation. The results were observed, and the FVC, FEV1, and PEF were recorded. Finally, the MVV was measured7, 8).
MVV measurement: Each volunteer was asked to breathe into the spirometer as deeply and rapidly as possible for 15 seconds. This value, which indicated the strength of breathing muscles, was recorded. A reproducible test was accepted according to the American Thoracic Society regulations8). The value was expressed as a percentage of the predicted normal values according to the European Respiratory Society (ERS) criteria9).
Chest expansion4) was measured in centimeters with a tape measure placed circumferentially around the chest wall at the second, fourth, and sixth intercostal spaces.
This study protocol was approved by the Human Research Ethics Committee, Khon Kaen University and was based on the Declaration of Helsinki and Good Clinical Practices (ICHGCP) [No. HE562040]. Informed consent was obtained from all subjects prior to study participation.
Data are presented as means (SD). The final 6MWT scores, lung function test scores, and all outcome results of the 2 groups were compared using the Wilcoxon rank sum test. The signed rank test was used to compare the differences in all outcome variables between the baseline and the end of the study in each group. The analyses were performed using the STATA software, version 10.1 (College station, Texas, USA). P<0.05 was considered statistically significant.
RESULTS
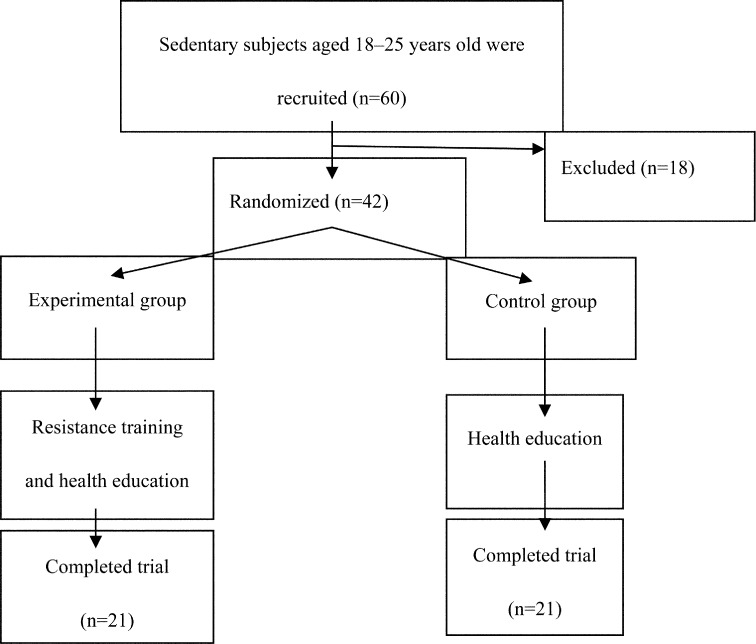
A total of 60 subjects were screened for this study. Of these, 42 subjects met the study criteria, who were divided into 2 groups of 21 subjects each. The other 18 subjects were excluded because of hypertension (6 subjects), wrist injury (4 subjects), smoking (3 subjects), and inconvenient participation (5 subjects). The data on baseline characteristics including age, weight, height, body mass index, blood pressure, and heart rate of the 2 groups were comparable (Table 1). The average age of the subjects in the control group (n=21) was 18.1±0.4 years, whereas that in the experimental group or resistance exercise group (n=21) was 18.2±0.4 years (Fig. 1).
Table 1. Anthropometric and baseline characteristics of subjects.
| Data/Groups | CG (n=21) | EG (n=21) |
|---|---|---|
| Gender (male/female) | 13/8 | 15/6 |
| Age (years) | 18.1±0.4 | 18.2±0.4 |
| Weight (kg) | 64.2±7.7 | 65.5±6.3 |
| Height (cm) | 169±0.06 | 170±0.1 |
| BMI (kg/m2) | 22.4±1.3 | 22.3±1.0 |
| SBP (mmHg) | 113.8±5.3 | 119.1±5.9 |
| DBP (mmHg) | 80.2±6.1 | 82.2±6.5 |
| HR (beats/minute) | 81.4±5.6 | 86.8±5.8 |
Data are presented as mean±SD. CG: control group; EG: experimental group; kg: kilogram; cm: centimeter; m: meter; mmHg: millimeters of mercury; BMI: body mass index; SBP: systolic blood pressure; DBP: diastolic blood pressure; HR: heart rate
Fig. 1.
Recruitment and randomization of subjects
The 8 outcome variables, as shown in Tables 2, 3, and 4, included 6MWT, PEF, FVC, FEV1, MVV, and 3 chest expansions (upper, middle, and lower). All outcome values in the resistance exercise group at week 8 were significantly higher than the respective baseline values and those in the control group (Tables 2, 3, and 4). In the control group, the PEF and upper and middle chest expansions at the end of study were significantly lower than the respective baseline values (Tables 2 and 4).
Table 2. Lung function and 6 MWT in the control (n=21) and experimental (n=21) groups.
| Variables | Groups | Baseline | 8 weeks |
|---|---|---|---|
| 6MWT (m) | CG | 595.0±29.9 | 594.1±36.9 |
| EG | 599.3±42.3 | 637.9±41.9*# | |
| PEF (L) | CG | 11.3±0.7 | 10.8±0.9* |
| EG | 11.7±0.8 | 13.4±0.8*# | |
| FVC (L) | CG | 4.6±0.4 | 4.7±0.3 |
| EG | 4.5±0.5 | 4.8±0.5*# | |
| FEV1 (L) | CG | 4.2±0.3 | 4.2±0.4 |
| EG | 4.1±0.5 | 4.6±0.5*# | |
| MVV (L/min) | CG | 174.7±8.9 | 172.8±9.5 |
| EG | 172.1±10.3 | 189.0±9.5*# |
Data are presented as mean±SD. CG: control group; EG: experimental group; 6MWT: 6-minute walk test; PEF: peak expiratory flow; FVC: forced vital capacity; FEV1: forced expiratory volume in 1 second; MVV: maximal voluntary ventilation; m: meter; L: liter; min: minute. #Significantly different from corresponding control group (p<0.05). *Significantly different from corresponding before period (p<0.05)
Table 3. Lung function in the control (n=21) and experimental (n=21) groups.
| Variables | Group | Baseline | 8 weeks |
|---|---|---|---|
| PEF (%pred.) | CG | 82.9±6.7 | 83.0±5.6 |
| EG | 84.7±6.7 | 89.3±5.3*# | |
| FVC (%pred.) | CG | 91.0±5.6 | 90.9±4.8 |
| EG | 92.0±5.6 | 95.6±4.1*# | |
| FEV1 (%pred.) | CG | 90.0±4.2 | 88.4±4.8 |
| EG | 90.1±3.5 | 95.3±4.2*# | |
| MVV (%pred.) | CG | 85.1±7.6 | 84.3±5.7 |
| EG | 85.8±7.6 | 90.8 ±6.3*# |
Data are presented as mean±SD. CG: control group; EG: experimental group; 6MWT: 6-minute walk test; PEF: peak expiratory flow; FVC: forced vital capacity; FEV1: forced expiratory volume in 1 second; MVV: maximal voluntary ventilation; %: percent; m: meter; L: liter; min: minute. #Significantly different from corresponding control group (p<0.05). *Significantly different from corresponding before period (p<0.05)
Table 4. Chest expansion in the control (n=21) and experimental (n=21) groups.
| Variables | Group | Baseline | 8 weeks |
|---|---|---|---|
| Upper chest (cm) | CG | 2.9±0.4 | 2.8±0.3* |
| EG | 2.9±0.3 | 3.1±0.3*# | |
| Middle chest (cm) | CG | 3.1±0.4 | 3.0±0.4* |
| EG | 3.1±0.3 | 3.3±0.2*# | |
| Lower chest (cm) | CG | 3.4±0.5 | 3.3±0.5 |
| EG | 3.3±0.3 | 3.6±0.3*# |
Data are presented as mean±SD. CG: control group; EG: experimental group; cm: centimeter. #Significantly different from corresponding control group (p<0.05). *Significantly different from corresponding before period (p<0.05)
DISCUSSION
In this study, an 8-week resistance exercise program was shown to improve cardiopulmonary functions in young healthy adults with a sedentary lifestyle. The exercise program was performed regularly for 45 minutes, 3 times/week.
The 6MWT scores, which represented cardiorespiratory endurance, were significantly higher after the regular performance of resistance exercise. At week 8, the average 6MWT was 637.9 m in the experimental group and 594.1 m in the control group. Previous studies also showed similar results5, 7, 8). A 6-week Thai dance exercise program was shown to improve 6MWT in the elderly5). The other 2 study populations that had better 6MWT scores following intervention were patients with ankylosing spondylitis and chronic obstructive airway disease. These exercises were aerobic exercises or exercises based on the Global Posture Reeducation7, 8).
Similar to other aerobic exercises, resistance exercise improved all pulmonary function outcomes in the experimental group compared to the control group (Tables 2, 3, and 4), including the PEF, FVC, FEV1, and MVV. Increased PEF, FVC, and FEV1 in the resistance exercise group indicated improvement in total lung capacity and airway flow. A better MVV value in the experimental group implied improvement in the respiratory muscle strength. These results are compatible with those of previous studies by Spruit et al. and Abrahin et al.9, 10). The studies showed that resistance exercise improved lung function in patients with COPD after 12 weeks and in elderly women.
A previous study by Durmus et al. showed that resistance exercise also improved chest expansion at the fourth intercostal space7). This study provided additional information regarding all levels of chest expansion, showing significant improvement after the 8-week resistance exercise program in the experimental group compared to the control group and the baseline values. The chest expansion is one of the factors that indicate the strength of striated respiratory muscles. Resistance exercise can be performed either as a single set or as multiple sets to improve respiratory muscle strength10).
This study showed that young adults with a sedentary lifestyle were compliance to the 8-week resistance exercise program. However, further studies are needed to study the long-term effects of resistance exercise on cardiovascular outcomes and its effects in other patient settings11,12,13,14,15,16,17). The other advantage of this study is that it was a randomized control trial.
In conclusion, the 8-week resistance exercise program improved cardiopulmonary functions in young sedentary subjects.
REFERENCES
- 1.Fiatarone MA, Marks EC, Ryan ND, et al. : High-intensity strength training in nonagenarians. Effects on skeletal muscle. JAMA, 1990, 263: 3029–3034. [PubMed] [Google Scholar]
- 2.Cabrera de León A, Rodríguez-Pérez MC, Rodríguez-Benjumeda LM, et al. : [Sedentary lifestyle: physical activity duration versus percentage of energy expenditure ] Rev Esp Cardiol, 2007, 60: 244–250(in Spanish). [PubMed] [Google Scholar]
- 3.Billinger SA, Arena R, Bernhardt J, et al. American Heart Association Stroke CouncilCouncil on Cardiovascular and Stroke NursingCouncil on Lifestyle and Cardiometabolic HealthCouncil on Epidemiology and PreventionCouncil on Clinical Cardiology: Physical activity and exercise recommendations for stroke survivors: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke, 2014, 45: 2532–2553. [DOI] [PubMed] [Google Scholar]
- 4.Fish DE, Krabak BJ, Johnson-Greene D, et al. : Optimal resistance training: comparison of DeLorme with Oxford techniques. Am J Phys Med Rehabil, 2003, 82: 903–909. [DOI] [PubMed] [Google Scholar]
- 5.Janyacharoen T, Laophosri M, Kanpittaya J, et al. : Physical performance in recently aged adults after 6 weeks traditional Thai dance: a randomized controlled trial. Clin Interv Aging, 2013, 8: 855–859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Swisher A, Goldfarb A: Use of the Six-Minute Walk/Run Test to predict peak oxygen consumption in older adults. Cardiopulm Phys Ther J, 1998, 9: 3–5. [Google Scholar]
- 7.Durmuş D, Alayli G, Uzun O, et al. : Effects of two exercise interventions on pulmonary functions in the patients with ankylosing spondylitis. Joint Bone Spine, 2009, 76: 150–155. [DOI] [PubMed] [Google Scholar]
- 8.Borghi-Silva A, Arena R, Castello V, et al. : Aerobic exercise training improves autonomic nervous control in patients with COPD. Respir Med, 2009, 103: 1503–1510. [DOI] [PubMed] [Google Scholar]
- 9.Spruit MA, Gosselink R, Troosters T, et al. : Resistance versus endurance training in patients with COPD and peripheral muscle weakness. Eur Respir J, 2002, 19: 1072–1078. [DOI] [PubMed] [Google Scholar]
- 10.Abrahin O, Rodrigues RP, Nascimento VC, et al. : Single- and multiple-set resistance training improves skeletal and respiratory muscle strength in elderly women. Clin Interv Aging, 2014, 9: 1775–1782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cho YS, Park SJ, Jang SH, et al. : Effects of the combined treatment of extracorporeal shock wave therapy (ESWT) and stabilization exercises on pain and functions of patients with myofascial pain syndrome. J Phys Ther Sci, 2012, 24: 1319–1323. [Google Scholar]
- 12.Lee Y: Effect of exercise therapy on the body composition and blood components of obese men. J Phys Ther Sci, 2011, 23: 595–598. [Google Scholar]
- 13.Endo Y, Oyunchimeg C, Nakagawa K, et al. : Evaluation of an exercise program for diabetic patients in Mongolia. J Phys Ther Sci, 2013, 25: 245–248. [Google Scholar]
- 14.Lee KH: The role of compensatory movements patterns in spontaneous recovery after stroke. J Phys Ther Sci, 2015, 27: 2671–2673. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 15.Prachanai R, Bouphan P:The participation in health promotion of health personnel in community hospitals Roi Et province, Thailand. KKU Res J, 2015, 20: 91–104. [Google Scholar]
- 16.Sea-jern N, Pochana K, Sunglhapong A: The prevalence and personal factors related to musculoskeletal disorders in occupational van drivers: a case study of public transport center in Hatyai, Songkhla. KKU Res J, 2014, 19: 107–118. [Google Scholar]
- 17.Chaiyawat P, Sophonratanapokin B: Health needs assessment of physical therapy for the elderly in suburban of Bangkok after flooding in 2011. KKU Res J, 2013, 19: 180–191. [Google Scholar]