Abstract
[Purpose] The purpose of this study was to find evidence for the effectiveness of rehabilitation for pain relief in patients with rheumatoid arthritis. [Subjects and Methods] A systematic review was conducted of MEDLINE, The Cochrane Central Register of Controlled Trials (CENTRAL), and OVID, for studies published from July 2005 to July 2015. We extracted data regarding patients, intervention, comparison, and outcomes, and assessed the methodological quality of the data. [Results] Nine randomized controlled trials comparing the effects of pain relief in patients with rheumatoid arthritis were found. [Conclusion] Physical therapy and occupational therapy can reduce pain in rheumatoid arthritis.
Key words: Pain, Rehabilitation, Rheumatoid arthritis
INTRODUCTION
Rheumatoid arthritis (RA) is a leading cause of disability in adults in the U.S.1). RA is a systemic, inflammatory condition causing pain, joint destruction and disability2). Pain is a common symptom in patients with rheumatoid arthritis and it is hard for them to cope with it3). There are some non-pharmacological treatments4,5,6,7) in rheumatologic care and noticeable advances over the past decade are changing the clinical course of RA8). Physical therapists and occupational therapists are multi-skilled professionals who treat patients with RA, and perform the role of case managers9).
A few studies suggest some evidence in which findings can benefit both therapists and clients in rheumatology care. However until now, no study has reviewed the effectiveness of pain intervention in patients with RA. Therefore, this is the first systematic review about pain relief for patient with RA. The aim of this study was to seek evidence for the effectiveness of rehabilitation for pain relief in patients with RA, and to suggest the guidelines of roles for physical therapists and occupational therapists.
SUBJECTS AND METHODS
For this study, we searched electronic databases using a strategy Mesh-term and free-text term. Then we performed a search of MEDLINE, The Cochrane Central Register of Controlled Trials (CENTRAL), and OVID, for studies published from July 2005 to July 2015, using the keywords: occupational therapy (OT), pain, physical therapy (PT), and rheumatoid arthritis. Studies identified were evaluated based on following the inclusion criteria: (1) subjects had RA, (2) study design: randomized controlled trials (RCTs), (3) had outcomes of pain relief, and (4) full text was available. Exclusion criteria were: (1) study was not an experimental study, (2) subjects had diseases other than RA, (3) study was about the development of evaluation tools, or (4) study design was review. Hand searching of journals and reference lists of relevant articles was also conducted without regard to languages.
Two reviewers independently evaluated the titles and abstracts for selecting articles to be included or excluded from our study. Then, we read the full text of the studies in detail. Multiple studies were considered as one trial if they described a single trial. The methodological quality of the trials was also independently assessed using the Physiotherapy Evidence-Based Database (PEDro) scale10, 11), a 10-point scale that has 11 items for the assessment of internal validity and statistical information in RCTs. Trials with a PEDro score greater than 5 are considered to be of moderate to high quality12). A total score was determined through discussion, if there were disagreements between the two reviewers. Intervention outcomes were reported using the patient, intervention, comparison and outcome (PICO) method.
RESULTS
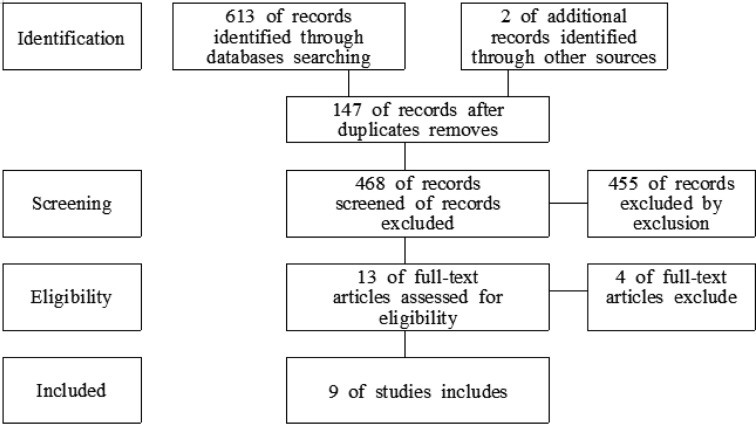
A total of 613 potentially relevant articles were identified based on the initial search, but 604 of them did not meet the inclusion criteria. Therefore, 9 studies13,14,15,16,17,18,19,20,21) were identified for this analysis (Fig. 1). All the studies were RCTs and clinical trials. Four articles had a score < 6 on the PEDro scale while the others had a score ≥ 6 (Table 1).
Fig. 1.
Diagram on process about searching process
Table 1. Summary of characteristics of included studies.
| Evidence | PEDro score | Patient (IG/CG) | Intervention | Comparison | Outcome | |
|---|---|---|---|---|---|---|
| Assessment | Result | |||||
| Rahnama et al., 201513) | 5 | RA N=48 Age=58.6 ± 7.8 F:M=all M DD=no mention |
aerobic exercise and strengthening exercise 30 to 45 min. 3 days per wk. for 8 wks. | no intervention | VAS (pain) WOMAC (functional ability) |
Pain relief and functional ability improved in exercise group. |
| Jahanbin et al., 201414) | 6 | RA 65 (32/32) 48.6/ 48.8y all F no mention |
conditioning, isotonic, isometric and aerobic exercise 45 min. 2 times per wk. for 8 wks. | received a booklet | VAS (pain) AIMS-2 (health status) |
Pain relief and health status improved in exercise group. |
| Hewlett et al., 201115) | 5 | RA 127 (62/62) 59.2y 44:18/ 49:13 14.6/ 14.2y |
cognitive behavioral therapy (CBT) group: fatigue self-management 6×2 h sessions for 6 wks. Consolidation: 1 h sessions for 14 wks. | fatigue self-management: 1 h sessions | MAF (fatigue impact) VAS (pain) |
Fatigue and pain relief improved in CBT group. |
| Breedland et al., 201116) | 5 | RA 34 (19/ 15) 45.0/ 51.8y 12:7/ 12:3 9.7/ 5.9y |
group based exercise and educational program 60 min. for 8 wks. | no intervention | AIMS-2 (health status) ASES (pain) |
No significant differences between groups. |
| Macedo et al., 200917) | 7 | employed RA 32 (16/16) 48.6/ 52.6y 15:1/ 15;1 11.6/ 8.4y |
comprehensive occupational therapy (COT) group: education, compliance and management 30 min. –2 h of each 6–8 session for 6 mon. | usual care group: medical management and rheumatology clinic visit | COPM (function) RA WIS (work productivity) DAS 28 (disease activity) VAS (pain) |
Function, work productivity, disease pain relief improved in COT group. |
| Adams et al., 200818) | 8 | RA 112 (56/60) 59.6/ 55.2y 42:14/ 42:18 8.6/ 12.4 mon. |
static resting splints group: splints+ standardized occupational therapy for 12 mon. (nightwear) | standardized OT group: JP education, hand exercises | hand deviation (deformity) MHQ (hand function) VAS (pain) grip strength |
No significant differences between groups. |
| Hammond et al., 200819) | 6 | RA 167 (86/81) 55.6/ 55.3y 57:29/ 51:30 7.2/ 7.6y |
modular behavioral (MB) group: 2.5 h meeting, 4 sessions per wk. 2 h review, 1session Module 1: behavioral JP program Module 2: initial discussion for 18 mon. | standard education program group: 2 h meeting, 5 session per wk. (information, exercise, JP, healthy diet) | RASE (psychological status) VAS (pain) HAQ (functional status) |
Psychological status, pain relief and functional status improved in MB group. |
| Veehof et al., 200820) | 7 | RA 53 (17/16) 66.3/ 55.1y 71:29/ 69:31(%) 8.2/ 5.0y |
prefabricated wrist working splint (splinting) group: 4 wks. | usual care group 4 wks. | VAS, DASH (pain) grip strength DASH, SODA-S (functional ability) |
Pain relief, grip strength and functional ability improved in splinting group. |
| Li et al., 200621) | 4 | RA 111 (63/48) 54.2/ 56.8y 55:8/ 38:10 10.6/ 13.2y |
primary therapist model (PTM) group: education splints/ foot orthosis psychosocial support for 6 wks. | traditional treatment model (TTM) group: assistive devices advice for modality aids | HAQ (physical function) VAS (pain) |
Physical function and pain relief improved in PTM group. |
AIMS-2: Arthritis Impact Measurement Scale-2. ASES: Arthritis Self-Efficacy Scale. CG: Control Group. COPM: Canadian Occupational Performance Measure. DAS 28: Clinical evaluation consisted of disease activity score. DASH: Disabilities of the Arm Shoulder Hand questionnaire. DD: Disease Duration. F: females. HAQ: Health Assessment Questionnaire. IG: Intervention Group. JP: Joint Protection. M: Males. MAF: Multi-Dimensional Assessment of Fatigue Scale. MHQ: Michigan Hand Outcomes Questionnaire. N: Number of subjects. RA: Rheumatoid Arthritis. RA WIS: RA Work Instability Scale. RASE: RA self-efficacy. SODA-S: Sequential Occupational Dexterity Assessment short version. VAS: Visual Analog Scales. WOMAC: Western Ontario and McMaster Osteoarthritis Index
Table 1 presents the summary of characteristics of the included studies according to the PICO method. There was a greater proportion of women than men in 8 of the studies. The kinds of OT and PT interventions used were various: exercise, cognitive behavioral therapy, education, or particular splint. In comparison, a control group was given: usual rheumatology care and conventional program, information about diagnosis or no intervention. For two studies, intervention was conducted by physical therapists and occupational therapists. Various assessment tools were used for assessing the outcomes, according to the purpose of the respective study. With the exception of two studies, there was significant improvement in the experimental group16, 18). PT including various exercises, education and assistive devices and OT including cognitive behavioral therapy, education, management and splints were effective methods for pain relief in patients with RA.
DISCUSSION
This study compared the effects of rehabilitation and rheumatology care for pain relief in patients with RA. The results indicated that PT and OT interventions are effective for pain relief in people with RA. In this review, most studies indicate that OT and PT interventions are more benefits than usual rheumatology care. These results are consistent with those of previous systematic reviews22, 23). Many intervention methods and assessment tool were used in this study. Categorization of RA intervention and assessment in this study is similar to the four categorizations noted by de Almeida24): patient guidance and education, joint protection and energy conservation, modifying activities and environments, and assistive technologies. In a remarkable intervention, one study was carried out to determine whether comprehensive intervention promotes function in employed people17). There is limited provision of vocational rehabilitation (VR) in the rheumatology area. It is suggested that VR is effective in increasing both knowledge and confidence in rheumatology25), so therapists try to involve and study this area. Another intervention, the therapy glove, decreases pain, stiffness, and swelling26). It is an effective method in rehabilitation in RA. However, we exclude that intervention in our study, because it was composed of a case study and published before 2000.
Currently, people with arthritis are diagnosed early and treated aggressively, so joint deformities and activity limitations are less common27). Therefore, therapists will need to focus on preventive as well as compensatory strategies for public health8).
Limitations of this systematic review are that we did not conduct a meta-analysis. Nevertheless, this is the first study that systematically reviewed PT and OT interventions for pain relief in patients with RA. Systematic reviews an important study design for informing practice and, can provide suggestions for OT and PT researchers who define future research agendas, and can assist administrators and decision-makers who develop evidence based policies and guidelines28). An important finding in our study, PT and OT intervention have some strong evidence of improvement for population with RA. We recommend that in the future, studies involving various and better intervention methods for patients with RA should be conducted.
REFERENCES
- 1.McNeil J, Binette J, Centers for Disease Control and Prevention (CDC): Prevalence of disabilities and associated health conditions among adults—United States, 1999. MMWR Morb Mortal Wkly Rep, 2001, 50: 120–125. [PubMed] [Google Scholar]
- 2.Scott DL, Steer S: The course of established rheumatoid arthritis. Best Pract Res Clin Rheumatol, 2007, 21: 943–967. [DOI] [PubMed] [Google Scholar]
- 3.Suurmeijer TP, Waltz M, Moum T, et al. : Quality of life profiles in the first years of rheumatoid arthritis: results from the EURIDISS longitudinal study. Arthritis Rheum, 2001, 45: 111–121. [DOI] [PubMed] [Google Scholar]
- 4.Peungsuwan P, Sermcheep P, Harnmontree P, et al. : The effectiveness of thai exercise with traditional massage on the pain, walking ability and QOL of older people with knee osteoarthritis: a randomized controlled trial in the community. J Phys Ther Sci, 2014, 26: 139–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lim KO, Lee DY, Shin WS: The effects of a warm whirlpool bath on pain and stiffness of patients with chronic stroke induced knee osteoarthritis. J Phys Ther Sci, 2013, 25: 873–875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nakata K, Kougo M, Huo M, et al. : The immediate effect of neuromuscular joint facilitation (NJF) treatment for knee osteoarthritis. J Phys Ther Sci, 2012, 24: 69–71. [Google Scholar]
- 7.Aoki O, Tsumura N, Kimura A, et al. : Home stretching exercise is effective for improving knee range of motion and gait in patients with knee osteoarthritis. J Phys Ther Sci, 2009, 21: 113–119. [Google Scholar]
- 8.Mallinson T, Fischer H, Rogers JC, et al. : Human occupation for public health promotion: new directions for occupational therapy practice with persons with arthritis. Am J Occup Ther, 2009, 63: 220–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hurst K: Multi-skilled health carers: nature, purpose and implications. Health Manpow Manage, 1997, 23: 197–211. [DOI] [PubMed] [Google Scholar]
- 10.Maher CG, Sherrington C, Herbert RD, et al. : Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther, 2003, 83: 713–721. [PubMed] [Google Scholar]
- 11.Macedo LG, Elkins MR, Maher CG, et al. : There was evidence of convergent and construct validity of Physiotherapy Evidence Database quality scale for physiotherapy trials. J Clin Epidemiol, 2010, 63: 920–925. [DOI] [PubMed] [Google Scholar]
- 12.Moseley AM, Herbert RD, Sherrington C, et al. : Evidence for physiotherapy practice: a survey of the Physiotherapy Evidence Database (PEDro). Aust J Physiother, 2002, 48: 43–49. [DOI] [PubMed] [Google Scholar]
- 13.Rahnama N, Mazloum V: Effects of strengthening and aerobic exercises on pain severity and function in patients with knee rheumatoid arthritis. Int J Prev Med, 2012, 3: 493–498. [PMC free article] [PubMed] [Google Scholar]
- 14.Jahanbin I, Hoseini Moghadam M, Nazarinia MA, et al. : The effect of conditioning exercise on the health status and pain in patients with rheumatoid arthritis: a randomized controlled clinical trial. Int J Community Based Nurs Midwifery, 2014, 2: 169–176. [PMC free article] [PubMed] [Google Scholar]
- 15.Hewlett S, Ambler N, Almeida C, et al. : Self-management of fatigue in rheumatoid arthritis: a randomised controlled trial of group cognitive-behavioural therapy. Ann Rheum Dis, 2011, 70: 1060–1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Breedland I, van Scheppingen C, Leijsma M, et al. : Effects of a group-based exercise and educational program on physical performance and disease self-management in rheumatoid arthritis: a randomized controlled study. Phys Ther, 2011, 91: 879–893. [DOI] [PubMed] [Google Scholar]
- 17.Macedo AM, Oakley SP, Panayi GS, et al. : Functional and work outcomes improve in patients with rheumatoid arthritis who receive targeted, comprehensive occupational therapy. Arthritis Rheum, 2009, 61: 1522–1530. [DOI] [PubMed] [Google Scholar]
- 18.Adams J, Burridge J, Mullee M, et al. : The clinical effectiveness of static resting splints in early rheumatoid arthritis: a randomized controlled trial. Rheumatology (Oxford), 2008, 47: 1548–1553. [DOI] [PubMed] [Google Scholar]
- 19.Hammond A, Bryan J, Hardy A: Effects of a modular behavioural arthritis education programme: a pragmatic parallel-group randomized controlled trial. Rheumatology (Oxford), 2008, 47: 1712–1718. [DOI] [PubMed] [Google Scholar]
- 20.Veehof MM, Taal E, Heijnsdijk-Rouwenhorst LM, et al. : Efficacy of wrist working splints in patients with rheumatoid arthritis: a randomized controlled study. Arthritis Rheum, 2008, 59: 1698–1704. [DOI] [PubMed] [Google Scholar]
- 21.Li LC, Davis AM, Lineker SC, et al. : Effectiveness of the primary therapist model for rheumatoid arthritis rehabilitation: a randomized controlled trial. Arthritis Rheum, 2006, 55: 42–52. [DOI] [PubMed] [Google Scholar]
- 22.Ye L, Kalichman L, Spittle A, et al. : Effects of rehabilitative interventions on pain, function and physical impairments in people with hand osteoarthritis: a systematic review. Arthritis Res Ther, 2011, 13: R28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vliet Vlieland TP, van den Ende CH: Nonpharmacological treatment of rheumatoid arthritis. Curr Opin Rheumatol, 2011, 23: 259–264. [DOI] [PubMed] [Google Scholar]
- 24.de Almeida PH, Pontes TB, Matheus JP, et al. : [Occupational therapy in rheumatoid arthritis: what rheumatologists need to know?]. Rev Bras Reumatol, 2015, 55: 272–280. [DOI] [PubMed] [Google Scholar]
- 25.O’Brien R, Woodbridge S, Hammond A, et al. : The development and evaluation of a vocational rehabilitation training programme for rheumatology occupational therapists. Musculoskelet Care, 2013, 11: 99–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nasir SH, Troynikov O, Massy-Westropp N: Therapy gloves for patients with rheumatoid arthritis: a review. Ther Adv Musculoskelet Dis, 2014, 6: 226–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vital EM, Emery P: Advances in the treatment of early rheumatoid arthritis. Am Fam Physician, 2005, 72: 1002–1004, 1004. [PubMed] [Google Scholar]
- 28.Pasqui F, Mastrodonato L, Ceccarelli F, et al. : [Occupational therapy in rheumatoid arthritis: short term prospective study in patients treated with anti-TNF-alpha drugs]. Reumatismo, 2006, 58: 191–198. [DOI] [PubMed] [Google Scholar]