Abstract
Background
This post-hoc sub-analysis investigated whether age (<65 years vs ≥65 years) affects glycemic control or hypoglycemic risk in patients with type 2 diabetes mellitus (T2DM) treated with once-daily insulin detemir.
Methods
This was a 26-week, randomized, open-label, phase IV trial involving 2812 patients at 1083 predominantly primary care sites throughout the United States, of which 541 were designated for investigator-led insulin titration. The main efficacy measure was change in HbA1c (A1C) from baseline to Week 26. Patients were stratified by age in the sites designated for the investigator-led titration of insulin detemir. Safety measures included adverse events and change in hypoglycemic event rates from baseline to Week 26.
Results
At Week 26, mean A1C and fasting plasma glucose decreased in both groups, but mean differences in change from baseline were not significant between groups. Within the group ≥65 years, significant reductions occurred for all daytime hypoglycemia, but there was no significant change from baseline in the other categories. In the group <65 years, reductions from baseline were significant for all hypoglycemic event categories. Changes in hypoglycemia rates from baseline were not significantly different between the age groups and there was no weight increase in either age group.
Conclusions
This analysis demonstrates that insulin detemir has similar efficacy and safety profiles for patients with T2DM ≥65 years compared with <65 years when treated via an investigator-led algorithm.
Key Points
| This post-hoc analysis presents an exploratory sub-analysis of efficacy and safety in patients with type 2 diabetes mellitus who were either under or over the age of 65 years and were treated with the basal insulin analog, insulin detemir. |
| Efficacy and safety profiles were found to be similar with both age groups and the results of this analysis support the use of a once-daily basal insulin in lowering HbA1c (A1C) and fasting plasma glucose while demonstrating a low rate of hypoglycemia and no weight gain. |
| This analysis showed that basal insulin may be a viable option for those aged ≥65 years and should be considered earlier in the course of diabetes rather than reserved for the latter stages of the disease. |
Introduction
The elderly represent a heterogeneous group with polypharmacy, comorbidity, and metabolic considerations associated with advanced age. Therefore, effective diabetes mellitus management in this group requires a comprehensive, multidisciplinary, and individualized approach. In addition, the lack of large, well controlled trials makes it difficult to determine which treatment options would benefit the majority of patients; thus, most recommendations were extrapolated from data in the non-elderly [1–5]. Two more recent published guidelines [6, 7] are evidence-based.
The population of older adults with diabetes is expected to increase due to the rise in obesity, changing lifestyle, and the increase in the overall life expectancy of the United States (US) population [8]. It is estimated that 33 % of nursing home residents have diabetes and 40 % of the population is presumed to be prediabetic [9, 10]. This growing disease burden represents a large public health concern since diabetes complications are more common and costly in older individuals who have lived with diabetes longer and are more vulnerable to hypoglycemia than younger patients [1, 11]. Nonetheless, recommendations for glycemic targets in the elderly are not exclusively driven by immediate clinical benefits but are also intended to prevent the untoward effects of pharmacotherapy, particularly hypoglycemia.
Currently, there are limited published data regarding basal insulin analog use in older adults, although basal insulin is the most common and effective recommended first step in initiating insulin therapy [12, 13]. Some studies suggest that insulin therapy in the elderly is underutilized despite available data showing that insulin therapy, particularly insulin analog therapy, is both safe and effective in this patient population [14, 15].
This publication presents an exploratory sub-analysis of efficacy and safety, particularly as it relates to the incidence of hypoglycemia and adverse events (AEs), in patients aged ≥65 years and <65 years who were treated with the basal insulin analog, insulin detemir (Novo Nordisk A/S, Bagsvaerd, Denmark), in the investigator-led arm of the PREDICTIVE™ 303 trial [16, 17]. This arm was chosen for analysis because it more closely reflects the typical practice, where most patients have their basal insulin levels adjusted by their physicians rather than adjusting it themselves. The goal of this analysis was to gain insight into the outcomes for glycemic control in patients aged ≥65 years compared with patients younger than 65 and whose insulin dosing was not self-managed, somewhat similar to what might occur in long-term institutional settings.
Materials and Methods
This exploratory post hoc sub-analysis of the PREDICTIVE 303 trial [16, 17] examines the efficacy and safety of insulin detemir in patients with type 2 diabetes who were stratified by age into two groups, aged <65 years (n = 1915) and ≥65 years (n = 897), and designated for investigator-led titration regimens during the 26-week trial period. Patients with type 2 diabetes, aged ≥18 years, HbA1c (A1C) ≤12 %, and mean body mass index (BMI) ≤45 kg/m2 were eligible for enrollment regardless of their diabetes treatment regimens. Data included in this post hoc sub-analysis were for patients who received only one dose of insulin detemir per day. The trial was approved by institutional review boards, and all participants enrolled in the trial provided written informed consent.
Trial Design and Treatment
Patients were encouraged to maintain contact with their physician throughout the trial. All subjects participated in a screening/baseline visit and follow-up visits at Weeks 12 and 26 and received a glucose meter (OneTouch® UltraSmart® Milpitas, CA, USA: LifeScan Inc) and test strips, with appropriate instructions for use. All glucose measurements performed with capillary blood were automatically calibrated by the meter to plasma-equivalent glucose values. Insulin detemir was supplied in the FlexPen® (3 mL, 100 U/mL, Bagsvaerd, Denmark: Novo Nordisk A/S) [16, 17].
Insulin detemir was the only basal insulin used throughout the trial. The protocol recommended insulin detemir to be injected once daily in the evening at approximately the same time each day. Throughout the trial, patients performed self-measured fasting plasma glucose (SMFPG) before breakfast on the last 6 days prior to each scheduled visit. Physicians determined the initial dose of insulin detemir based on the manufacturer’s instructions [17] and adjusted the dose during the trial according to their standard-of-care practice. During the first 12 weeks, only the dose of insulin detemir was to be titrated; in the final 14 weeks, investigators were encouraged to adjust all medications taken to treat diabetes, including prandial insulin doses, where appropriate.
Assessments
The main outcomes for efficacy were A1C and the change in A1C from baseline to the end of the 26-week treatment period. Change in A1C was analyzed only for patients with A1C values measured at baseline and at 26 weeks. Additional outcome variables included FPG, body weight, and final insulin detemir dose (Table 2). The safety analysis set (SAS) included all patients who took at least one injection of insulin detemir after the baseline visit and reported any safety information.
Table 2.
Changes from baseline for A1C, FPG, insulin detemir dose, and body weight in patients aged <65 and ≥65 years
| Parameter | <65 yearsa | ≥65 yearsa | Mean estimated differences in changes from baseline between groupsb | ||||
|---|---|---|---|---|---|---|---|
| n | Mean change | SD (SE) | n | Mean change | SD (SE) | ||
| A1C (%) | 1219 | −0.56 | 1.5 (0.04) | 584 | −0.47 | 1.3 (0.05) | 0.094, p = 0.17 |
| Fasting plasma glucose (mg/dL) | 1221 | −21.8 | 83.7 (2.4) | 582 | −25.5 | 70.2 (2.9) | −3.70, p = 0.33 |
| Insulin detemir dose (U/kg) | 1268 | 0.19 | 0.3 (0.008) | 603 | 0.11 | 0.2 (0.008) | −0.078, p < 0.0001 |
| Body weight (kg) | 1500 | −0.13 | 5.5c (0.14) | 719 | −0.49 | 5.1c (0.19) | −0.356, p = 0.13 |
Data for A1C, FPG, and insulin detemir dose were from the efficacy analysis set; body weight came from the safety set
FPG fasting plasma glucose, SD standard deviation, SE standard error
aData shown are for observed mean changes within each age group
bData shown are for differences between age groups for changes from baseline (Day 1) to the end of Week 26 (≥65 − <65)
cSD values for body weight changes are large because the gap between the minimum and maximum values was wide
Statistical Analyses
A 2-sided t test with Welch’s correction was used for comparisons between age groups with respect to changes from baseline for A1C, FPG, body weight, and insulin dose. The safety data collected included adverse events and hypoglycemic events.
In the main PREDICTIVE® 303 trial [16], hypoglycemic events were defined as (a) symptoms of hypoglycemia that resolved with oral carbohydrate intake, glucagon, or intravenous glucose, and (b) any symptomatic or asymptomatic blood glucose <56 mg/dL (<3.1 mmol/L). Nocturnal hypoglycemic events were defined as those occurring between 2300 and 0600 hours. Severe hypoglycemia was defined as an episode of hypoglycemia during which the patient was unable to self-treat.
Differences in hypoglycemia rates between groups were analyzed using a Poisson regression model with a log-link function and the logarithm of the time period in which a hypoglycemic episode was considered treatment emergent as offset. All relative risk ratios were adjusted for the reported total number of years the patient was exposed to the drug in order to correct for exposure. SAS for Unix (SAS Institute, Cary, NC, USA), and GraphPad Prism, version 6 (GraphPad Software, La Jolla, CA, USA), were used for data analyses.
Results
Demographics
Table 1 lists the baseline demographic characteristics of patients in the post hoc analysis trial. There were fewer patients in the group aged ≥65 years (n = 897) than in the group aged <65 years (n = 1915). Additionally, patients in the older group had a longer duration of diabetes [mean ± standard deviation (SD), 14.3 ± 9.1 years vs 9.8 ± 7.3 years] and lower body weight (92.0 ± 18.5 kg vs 101.2 ± 21.8 kg) than those aged <65 years. Similar proportions of patients in both age groups were insulin-naïve (36.4 and 30.1 % in the <65- and ≥65-years age groups, respectively) or had prior treatment with insulin glargine (35.7 and 37.0 % in the <65- and ≥65-years age groups, respectively) or neutral protamine Hagedorn (NPH) (5.1 and 8.6 % in the <65- and ≥65-years age groups, respectively).
Table 1.
Baseline demographic characteristics—safety population
| Parameter | <65 years (n = 1915) | ≥65 years (n = 897) |
|---|---|---|
| Age (years) | ||
| Mean (SD) | 52.3 (8.5) | 71.9 (5.4) |
| Sex, n (%) | ||
| Female | 921 (48.1) | 434 (48.4) |
| Male | 994 (51.9) | 462 (51.5) |
| Missing | 0 | 1 (0.1) |
| Race, n (%) | ||
| White American | 1423 (74.3) | 732 (81.6) |
| Black or African American | 361 (18.9) | 130 (14.5) |
| Asian | 40 (2.1) | 9 (1.0) |
| American Indian or Alaska Native | 17 (0.9) | 10 (1.1) |
| Native Hawaiian or other Pacific Islander | 3 (0.2) | 1 (0.1) |
| Other | 50 (2.6) | 12 (1.3) |
| BMI (kg/m2), n (%) | 34.6 (6.3) | 32.4 (5.7) |
| Pre-trial insulin therapy, n (%) | ||
| Glargine | 684 (35.7) | 332 (37.0) |
| NPH | 98 (5.1) | 77 (8.6) |
| Insulin-naïvea | 697 (36.4) | 270 (30.1) |
| Others | 436 (22.8) | 218 (24.3) |
| A1C (%) | 8.65 | 8.22 |
| Fasting plasma glucose (mg/dL) | 180.5 | 160.2 |
| Body weight (kg) | 101.2 | 91.8 |
| Duration of type 2 diabetes | ||
| n | 1909 | 897 |
| y, SD | 9.8 (7.3) | 14.3 (9.1) |
BMI body mass index, NPH neutral protamine Hagedorn, SD standard deviation
aInsulin-naïve is defined as patients who took oral anti-diabetes drugs only or did not have therapy as pretreatment
Efficacy
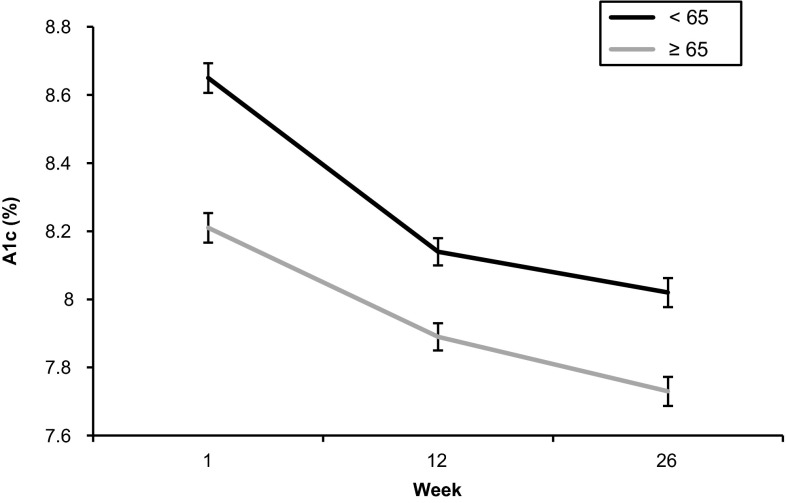
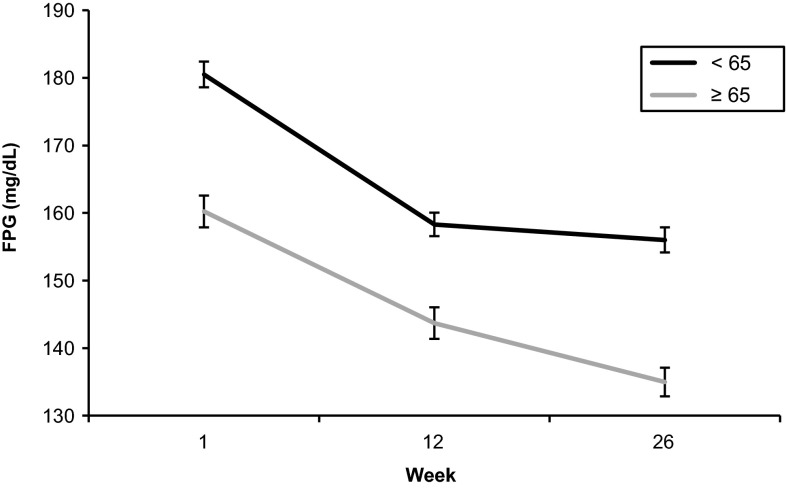
Mean baseline values of A1C and FPG were numerically lower in the group aged ≥65 years than in the group aged <65 years (Table 1). Mean differences between groups in changes from baseline for A1C, FPG, and body weight were not significantly different (Figs. 1, 2; Table 2). Starting and ending A1C for patients <65 years were 8.65 and 8.0 %, respectively, compared with 8.2 and 7.7 % for patients ≥65 years. Mean estimated A1C difference in change from baseline between age groups (≥65 − <65) was 0.09 % (p = 0.17). Starting and ending FPG for patients <65 years were 180.5 mg/dL and 156 mg/dL, respectively, compared with 160.2 mg/dL and 135 mg/dL for patients ≥65 years. Mean estimated FPG difference in change from baseline between age groups was −3.7 mg/dL (p = 0.33). Estimated mean differences in body weight changes from baseline between age groups were not statistically significant (Table 2). The change in insulin dose from baseline increased a small amount for both age groups, with mean estimated differences in change in insulin dose between age groups of −0.08 units/kg (p < 0.0001). Despite the lower A1C achieved in both the <65- and ≥65-years age groups, there was no weight gain, an especially important observation for the ≥65-years group who can be unduly burdened by additional weight.
Fig. 1.
HbA1c (A1C) (mean ± SE) in patients aged <65 and ≥65 years
Fig. 2.
Fasting plasma glucose (FPG) (mean ± SE) in patients aged <65 and ≥65 years
Safety
Overall, baseline hypoglycemia rates (events/patient/year) were similar in both groups at treatment initiation (Table 3). For severe hypoglycemia, the rates were low overall and remained low throughout the trial (between 5 and 28 events per 100 patients treated for 1 year). Changes in hypoglycemia rates from baseline to end of treatment (Week 26) were not significantly different between the two age groups.
Table 3.
Hypoglycemic events in patients aged <65 and ≥65 years
| Age (years) | Type of hypoglycemia | Exposure time | All | Severe | ||
|---|---|---|---|---|---|---|
| % | R | % | R | |||
| <65 | Daytime (n = 1531) | Baseline | 17.2 | 6.20 | 2.2 | 0.57 |
| Week 26 | 11.0 | 3.32a | 0.3 | 0.05a | ||
| ≥65 | Daytime (n = 736) | Baseline | 19.4 | 6.17 | 1.9 | 0.35 |
| Week 26 | 12.5 | 4.04a | 0.5 | 0.14 (NS) | ||
| <65 | Nocturnal (n = 1531) | Baseline | 7.1 | 2.25 | 1.5 | 0.27 |
| Week 26 | 4.4 | 1.25a | 0.3 | 0.07a | ||
| ≥65 | Nocturnal (n = 736) | Baseline | 6.5 | 1.92 | 1.0 | 0.24 |
| Week 26 | 5.3 | 2.52 (NS) | 0.4 | 0.28 (NS) | ||
There were no significant differences in changes of hypoglycemia rate when comparisons between age groups were performed
Significance was based on a generalized linear model with a Poisson distribution and a logarithmic link function
% represents the proportion of patients reporting at least one hypoglycemic event, where % = n/N × 100 and n is the number of patients reporting at least one hypoglycemic event
n number of patients who have data on both visits, NS not significant
aStatistically significant difference in rate from baseline, for patients within the indicated age group
Rates for all daytime hypoglycemic events were significantly decreased within both age groups, and reductions in severe daytime hypoglycemia were statistically significant within the group aged <65 years. Nocturnal hypoglycemia rates changed between one and two events/patient/year within each age group, and were statistically significant (all and severe) for the group aged <65 years.
The proportions of patients with reported AEs are shown in Table 4. The observed percentage of subjects experiencing at least one serious AE (SAE) was lower in patients aged <65 years than in those aged ≥65 years (5.2 vs 7.7 %, respectively), but the proportion of AEs possibly or probably related to insulin detemir treatment were similar. Cardiac disorders were the most common SAE in both age groups, and occurred in similar proportions of patients in each age group [18/897 (2.0 %) patients aged ≥65 years and 23/1915 (1.2 %) patients aged <65 years]. In patients aged ≥65 years, one of the five deaths was due to cardiac disorders compared with two out of four patients aged <65 years. Two out of five patients aged ≥65 years died of neoplasms (one case of metastatic breast cancer and one case of abdominal malignancy), with no neoplasms in patients aged <65 years. No relationship to treatment was ascribed to the abdominal malignancy, and all other deaths were characterized by the investigators as unlikely to be related to insulin detemir.
Table 4.
Adverse events distribution in patients aged <65 and ≥65 years
| <65 years (n = 1915) | ≥65 years (n = 897) | |||||
|---|---|---|---|---|---|---|
| n | % | E | n | % | E | |
| Adverse events (AEs) | 321 | 16.8 | 578 | 163 | 33.1 | 281 |
| Serious adverse events (SAEs) | 99 | 5.2 | 137 | 69 | 7.7 | 93 |
| Insulin detemir-related AEs (probably/possibly related) | 86 | 4.5 | 140 | 32 | 3.6 | 58 |
E number of events
Discussion
In this post hoc analysis of the PREDICTIVE 303 trial data, mean differences in change from baseline in A1C and FPG were not significantly different between the groups aged <65 and ≥65 years. Baseline hypoglycemia rates were low for both age groups. Hypoglycemia rates decreased significantly within each age group, but there were no significant differences in changes in hypoglycemia rates from baseline between the groups. This is a clinically meaningful finding and should encourage the use of basal insulin in the elderly patient population.
The low hypoglycemia rates for the group aged ≥65 years were maintained despite improvements in A1C. Body weight changes amounted to small, but non-significant decreases between the two age groups. This lack of weight gain while achieving improved A1C values is important, especially in light of the more typical weight gain observed with insulin use. Final insulin dose was only slightly higher in the group aged <65 years compared with the group aged ≥65 years. The difference in mean change in dose between the two age groups was statistically significant, but not clinically relevant. Adverse events related to treatment occurred at similar rates in both age groups.
This post hoc analysis included some limitations. First, the trial was not evenly randomized in terms of each group having equal numbers of patients. Second, there was no randomization for comorbidities and baseline glucose parameters. Lastly, investigators were encouraged to adjust any medication taken to treat diabetes during the last 14 weeks of the trial, including prandial insulin doses. This could have confounded the results since the number of patients requiring this intervention may have been different between age groups. Nevertheless, the results of this sub-analysis support the use of insulin detemir in the elderly population with type 2 diabetes. Physicians successfully titrated insulin detemir to patients aged ≥65 years with similar safety and improvements in efficacy seen in patients aged <65 years.
The results of this current sub-analysis are similar to other published analyses. A post-hoc analysis [14] conducted on data pooled from three phase III trials comparing insulin detemir and NPH insulin [18–20] suggested that insulin detemir can reduce A1C levels with less hypoglycemia and less weight gain in both older and younger persons with type 2 diabetes. A post-hoc analysis of the original INITIATEplus trial [21] demonstrated that biphasic insulin aspart 70/30 was well tolerated and effective in patients with type 2 diabetes aged <65 years and ≥65 years [22]. The addition of insulin glargine to current oral anti-diabetic (OAD) therapy for patients ≥65 years with poor glycemic control was as effective as increasing the dose of the OAD and demonstrated lower hypoglycemia risk in this patient population [15]. These studies support the use of insulin analogs in older patients with type 2 diabetes.
There are few evidence-based studies from which treatment guidelines for elderly patients can be derived. The current recommendations are intended to individualize treatment plans [4, 5, 23, 24]. The risk of hypoglycemia among patients with type 2 diabetes aged ≥65 years is possibly more serious than in a younger population [22]. Therefore, glycemic control in patients aged ≥65 years must be carefully balanced with safety, especially hypoglycemic risk [22].
The results of this subanalysis support the use of once-daily basal insulin in lowering A1C and FPG while demonstrating a low rate of hypoglycemia and no weight gain. In addition to meeting the needs of patients with type 2 diabetes who are aged <65 years as demonstrated in earlier trials, this analysis showed that basal insulin may be a viable option for those aged ≥65 years and should be considered earlier in the course of diabetes rather than being reserved for the latter stages of the disease.
Conclusion
Patients with type 2 diabetes treated with insulin detemir according to physician-led dose titration showed no differences in efficacy or hypoglycemia rate changes as a function of age.
Acknowledgments
The authors wish to thank Heba Costandy, MD/MS, and Aric Fader, PhD, of MedVal Scientific Information Services, LLC, for providing medical writing and editorial assistance, and Pei-Ling Chu, PhD and Wayne Weng, PhD, Novo Nordisk Inc., for assistance with statistical analyses. This manuscript was prepared according to the International Society for Medical Publication Professionals’ “Good Publication Practice for Communicating Company-Sponsored Medical Research: the GPP2 Guidelines.”
Compliance with Ethical Standards
Conflicts of interest and funding
Anuj Bhargava conducts or has conducted research studies in the interest of diabetes for Novo Nordisk, Eli Lilly and Company, AbbVie, MannKind Corporation, Intarcia, Orexigen Therapeutics, Inc., Sanofi-Aventis, Jaeb, Merck, University of Oxford, Boehringer, Ingelheim Pharmaceuticals, Inc., Duke University Medical Center, Medtronic, AstraZeneca, and Halozyme. He serves on advisory boards for Abbott and Janssen. He also is a speaker for Janssen, Takeda, Sanofi, and Daiichi Sankyo. Vicky Chan and Edward S. Kimball are employees of Novo Nordisk Inc. David Oyer serves on the advisory boards/speakers bureaus for AstraZeneca, Boehringer Ingelheim Pharmaceuticals, Inc., Eli Lilly and Company, Janssen Pharmaceuticals, Inc., and Novo Nordisk Inc. Funding to support the preparation of this manuscript was provided by Novo Nordisk Inc.
References
- 1.California Healthcare Foundation/American Geriatrics Society Guidelines for improving the care of the older person with diabetes mellitus. J Am Geriatr Soc. 2003;51(5 suppl):S265–S280. doi: 10.1046/j.1532-5415.51.5s.1.x. [DOI] [PubMed] [Google Scholar]
- 2.Sinclair A, Morley JE. How to manage diabetes mellitus in older persons in the 21st century: applying these principles to long term diabetes care. J Am Med Dir Assoc. 2013;14(11):777–780. doi: 10.1016/j.jamda.2013.09.001. [DOI] [PubMed] [Google Scholar]
- 3.Neumiller JJ, Setter SM. Pharmacologic management of the older patient with type 2 diabetes mellitus. Am J Geriatr Pharmacother. 2009;7(6):324–342. doi: 10.1016/j.amjopharm.2009.12.002. [DOI] [PubMed] [Google Scholar]
- 4.Sue KM, Briscoe VJ, Clark N, et al. Diabetes in older adults: a consensus report. J Am Geriatr Soc. 2012;60(12):2342–2356. doi: 10.1111/jgs.12035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kirkman MS, Briscoe VJ, Clark N, et al. Diabetes in older adults: a consensus report. Diabetes Care. 2012;35(12):2650–2664. doi: 10.2337/dc12-1801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mallery LH, Ransom T, Steeves B, Cook B, Dunbar P, Moorhouse P. Evidence-informed guidelines for treating frail older adults with type 2 diabetes: from the Diabetes Care Program of Nova Scotia (DCPNS) and the Palliative and Therapeutic Harmonization (PATH) Program. J Am Med Dir Assoc. 2013 [Epub ahead of print]. [DOI] [PubMed]
- 7.Sinclair A, Morley JE, Rodriguez-Manas L, et al. Diabetes mellitus in older people: position statement on behalf of the International Association of Gerontology and Geriatrics (IAGG), the European Diabetes Working Party for Older People (EDWPOP), and the International Task Force of Experts in Diabetes. J Am Med Dir Assoc. 2012;13(6):497–502. doi: 10.1016/j.jamda.2012.04.012. [DOI] [PubMed] [Google Scholar]
- 8.Boyle JP, Honeycutt AA, Narayan KM, et al. Projection of diabetes burden through 2050: impact of changing demography and disease prevalence in the US. Diabetes Care. 2001;24(11):1936–1940. doi: 10.2337/diacare.24.11.1936. [DOI] [PubMed] [Google Scholar]
- 9.Centers for Medicare and Medicaid Services. MDS active resident information report: Third Quarter 2010. CMS.gov.
- 10.Cowie CC, Rust KF, Ford ES, et al. Full accounting of diabetes and pre-diabetes in the US population in 1988–1994 and 2005–2006. Diabetes Care. 2009;32(2):287–294. doi: 10.2337/dc08-1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sloan FA, Bethel MA, Ruiz D, Jr, Shea AH, Feinglos MN. The growing burden of diabetes mellitus in the US elderly population. Arch Intern Med. 2008;168(2):192–199. doi: 10.1001/archinternmed.2007.35. [DOI] [PubMed] [Google Scholar]
- 12.Davis KL, Wei W, Meyers JL, Kilpatrick BS, Pandya N. Use of basal insulin and the associated clinical outcomes among elderly nursing home residents with type 2 diabetes mellitus: a retrospective chart review study. Clin Interv Aging. 2014;9:1815–1822. doi: 10.2147/CIA.S65411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Munshi MN, Pandya N, Umpierrez GE, Digenio A, Zhou R, Riddle MC. Contributions of basal and prandial hyperglycemia to total hyperglycemia in older and younger adults with type 2 diabetes mellitus. J Am Geriatr Soc. 2013;61(4):535–541. doi: 10.1111/jgs.12167. [DOI] [PubMed] [Google Scholar]
- 14.Garber AJ, Clauson P, Pedersen CB, Kolendorf K. Lower risk of hypoglycemia with insulin detemir than with neutral protamine hagedorn insulin in older persons with type 2 diabetes: a pooled analysis of phase III trials. J Am Geriatr Soc. 2007;55(11):1735–1740. doi: 10.1111/j.1532-5415.2007.01414.x. [DOI] [PubMed] [Google Scholar]
- 15.Papa G, Fedele V, Chiavetta A, et al. Therapeutic options for elderly diabetic subjects: open label, randomized clinical trial of insulin glargine added to oral antidiabetic drugs versus increased dosage of oral antidiabetic drugs. Acta Diabetol. 2008;45(1):53–59. doi: 10.1007/s00592-007-0023-6. [DOI] [PubMed] [Google Scholar]
- 16.Meneghini L, Koenen C, Weng W, Selam JL. The usage of a simplified self-titration dosing guideline (303 Algorithm) for insulin detemir in patients with type 2 diabetes—results of the randomized, controlled PREDICTIVE™ 303 study. Diabetes Obes Metab. 2007;9(6):902–913. doi: 10.1111/j.1463-1326.2007.00804.x. [DOI] [PubMed] [Google Scholar]
- 17.Selam JL, Meneghini LF. Basal-bolus therapy with insulin detemir using the 303 algorithm in the US PREDICTIVE 303 trial. Adv Ther. 2009;26(2):194–207. doi: 10.1007/s12325-009-0007-8. [DOI] [PubMed] [Google Scholar]
- 18.Haak T, Tiengo A, Draeger E, Suntum M, Waldhausl W. Lower within-subject variability of fasting blood glucose and reduced weight gain with insulin detemir compared to NPH insulin in patients with type 2 diabetes. Diabetes Obes Metab. 2005;7(1):56–64. doi: 10.1111/j.1463-1326.2004.00373.x. [DOI] [PubMed] [Google Scholar]
- 19.Hermansen K, Davies M, Derezinski T, Ravn GM, Clauson P, Home P. A 26-week, randomized, parallel, treat-to-target trial comparing insulin detemir with NPH insulin as add-on therapy to oral glucose-lowering drugs in insulin-naive people with type 2 diabetes. Diabetes Care. 2006;29(6):1269–1274. doi: 10.2337/dc05-1365. [DOI] [PubMed] [Google Scholar]
- 20.Raslova K, Bogoev M, Raz I, Leth G, Gall MA, Hancu N. Insulin detemir and insulin aspart: a promising basal-bolus regimen for type 2 diabetes. [Correction appears in Raslova K, et al. Diabetes Res Clin Pract. 2006;72:112] Diabetes Res Clin Pract. 2004;66(2):193–201. doi: 10.1016/j.diabres.2004.03.003. [DOI] [PubMed] [Google Scholar]
- 21.Oyer DS, Shepherd MD, Coulter FC, et al. A1c control in a primary care setting: self-titrating an insulin analog pre-mix (INITIATEplus trial) Am J Med. 2009;122(11):1043–1049. doi: 10.1016/j.amjmed.2008.12.026. [DOI] [PubMed] [Google Scholar]
- 22.Oyer DS, Shepherd MD, Coulter FC, et al. Efficacy and tolerability of self-titrated biphasic insulin aspart 70/30 in patients aged >65 years with type 2 diabetes: an exploratory post hoc subanalysis of the INITIATEplus trial. Clin Ther. 2011;33(7):874–883. doi: 10.1016/j.clinthera.2011.05.093. [DOI] [PubMed] [Google Scholar]
- 23.Garber AJ, Abrahamson MJ, Barzilay JI, et al. AACE comprehensive diabetes management algorithm 2013. Endocr Pract. 2013;19(2):327–336. doi: 10.4158/endp.19.2.a38267720403k242. [DOI] [PubMed] [Google Scholar]
- 24.Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycemia in type 2 diabetes: a patient-centered approach. Position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) Diabetes Care. 2012;35(6):1364–1379. doi: 10.2337/dc12-0413. [DOI] [PMC free article] [PubMed] [Google Scholar]