Abstract
Objectives
The purpose of this descriptive study was to investigate the current situation of clinical alarms in intensive care unit (ICU), nurses' recognition of and fatigue in relation to clinical alarms, and obstacles in alarm management.
Methods
Subjects were ICU nurses and devices from 48 critically ill patient cases. Data were collected through direct observation of alarm occurrence and questionnaires that were completed by the ICU nurses. The observation time unit was one hour block. One bed out of 56 ICU beds was randomly assigned to each observation time unit.
Results
Overall 2,184 clinical alarms were counted for 48 hours of observation, and 45.5 clinical alarms occurred per hour per subject. Of these, 1,394 alarms (63.8%) were categorized as false alarms. The alarm fatigue score was 24.3 ± 4.0 out of 35. The highest scoring item was "always get bothered due to clinical alarms". The highest scoring item in obstacles was "frequent false alarms, which lead to reduced attention or response to alarms".
Conclusions
Nurses reported that they felt some fatigue due to clinical alarms, and false alarms were also obstacles to proper management. An appropriate hospital policy should be developed to reduce false alarms and nurses' alarm fatigue.
Keywords: Critical Care, Nurse, Clinical Alarms, Fatigue, Recognition
I. Introduction
With the development of medical technology, clinical alarms from diverse medical devices, which are explosively increasing, are becoming a new issue in intensive care units (ICUs). Medical device (clinical) alarms, which were designed to draw medical staff's attention when a patient's conditions goes beyond the proper range, are causing a new alarm hazard problem [1]. According to previous studies, there were no more than 6 types of alarms from one critically ill patient in 1983; however, there were at least 40 types of clinical alarms in 2011 [1].
Excessive clinical alarms may cause an alarm hazard, which includes inappropriate application of alarms, alarm fatigue, and the application of a uniform alarm range to every patient [2]. While defects of devices threatened patient safety in the past, alarms indiscriminately generated by the explosive increase in the number of medical devices now threaten their safety. Reports on safety accidents related to the diversity of medical device alarms have raised awareness of the clinical alarm hazard. In 2002, 65% of 23 sentinel events were related to dysfunction and disuse of alarm devices and inappropriate alarm setting [3]. Five-hundred sixty-six deaths related to the monitoring of device alarms [4], severe burns due to neglect of alarms from hyperthermic machines [5], and hypoxic brain damage [6] were also reported. In 2012, alarm hazard was ranked first among ten types of medical technology hazards in the United States [2].
Ambient noises, including clinical alarms in ICUs were estimated to be more than 80 dB, which is close to the noise level generated by a pneumatic drill in an operating room [7]. In addition to the noise problem caused by alarms, ICU nurses may have difficulty in distinguishing alarms for urgent intervention from others since different device manufacturers use different types of alarms. For example, they need to differentiate alarms for replacing the syringe of an infusion pump from those for a life-threatening emergency when they hear both types of alarms [8]. ICU nurses were found to have difficulty in differentiating more than 6 different alarms [1,9] and could differentiate no more than 9–14 out of 23 alarms on average [10].
In one study, medical staff members were repeatedly exposed to an average of 771 patient monitor alarms per patient per day [11]. Medical staff overexposed to alarms may experience a decrease in concentration, become careless, and commit mistakes. Moreover, overexposure may make medical staff less sensitive to alarms and may cause them to cope improperly with significant alarms that can affect patients' safety [12]. The literature suggests that excessive medical device alarms may cause nurses to feel alarm fatigue [7,13,14].
Alarm fatigue occurs when medical staff are overwhelmed by excessive clinical alarms [2]; in particular, false (positive) alarms, inappropriate alarms-setting ranges, and the overuse of patient monitors act as principal factors that cause alarm fatigue [7,14]. Of these, the most problematic factor is false alarms: frequent false alarms may produce the 'cry wolf' effect and may cause nurses to regard significant alarms as false and thus fail to respond properly. It may also make an alarm system less reliable and may cause nurses not to use alarm devices [14,15]. It is therefore essential to effectively manage medical device alarms and develop good interventions that can reduce false alarms. Since 2010, standardized prevention has been suggested on the basis of various studies on how to conceptualize and reduce alarm fatigue [16,17,18,19] and basic research on nurses' recognition of clinical alarms and on the obstacles to their alarm management [16,17] in the United States. On the contrary, in Korea, little research has been conducted on medical device alarms. Medical device alarm hazard and alarm fatigue are novel concepts, and the Korean Society for Patient Safety established in 2013 has just posted a foreign article introducing the concept of clinical alarms [20].
This study aimed to investigate the current status of medical device alarms in ICUs, where medical devices equipped with an alarm function are most frequently used, to determine nurses' recognition of and fatigue in relation to alarms, and to identify obstacles to alarm management. This information will provide basic data that could help create a safe hospital environment.
II. Methods
This is descriptive research on medical device alarms status in ICUs, on nurses' alarm fatigue and recognition of alarms, and on the obstacles to alarm management.
1. Investigation Tool for Clinical Alarms Status
The tool adapted from Baillargeon [21] instrument was used to investigate the number of alarms from medical devices applied to the patients, alarm-generating devices, and the alarm-setting status of patient monitors and mechanical ventilators. A manual counter was used to count alarm sounds, and both the medical devices generating alarms and the causes of the alarms were recorded whenever they rang. Alarms were divided into valid and false ones on the basis of Baillargeon's study [21], and false alarms were then examined in terms of technical and non-technical problems based on a literature review [19,22].
2. Nurses' Recognition of Clinical Alarms and Obstacles to Clinical Alarm Management
To investigate ICU nurses' recognition of medical device alarms, 23 items appropriate for the Korean ICU situation were selected among 31 items developed by the Healthcare Technology Foundation (HTF) [23] and validated through translation and reverse translation. The first part of the selected questionnaire consisted of 14 items concerning recognition of medical device alarms on a 5-point scale: from 1, meaning 'strongly disagree', to 5, meaning 'strongly agree'. The second part consisted of 9 items concerning obstacles to effective alarm management. Nurses were asked to rank obstacles from 1 to 9.
3. Alarm Fatigue
Eight relevant items were selected from the table of subjective symptoms of fatigue revised by the Japanese Occupational Hygiene Association [24] in 2002 and from the instrument applied by Kim and Sung [25]. Except one item with a content validity index lower than 0.8, seven items were finally adopted. Each item was rated using a 5-point scale with a higher score meaning greater fatigue. For reliability, Cronbach's α coefficient was estimated to be 0.79 in the present study.
4. Data Collection Period and Procedure
Approval of the Institutional Review Board of Inha University in Incheon, South Korea was obtained for the research plan (No. 140829-2A) before the research began. Data were collected from October 18 to December 1, 2014 for 9 days. Alarms status in 5 ICUs (2 medical ICUs, 2 surgical ICUs, 1 coronary care unit) was investigated, and then, a survey was conducted on nurses' alarm fatigue, their recognition of alarms, and the obstacles to alarm management.
Data were collected through personal observation of each patient in ICUs by a nurse researcher. Twenty-four hours were evenly divided into observation units of one hour to exclude any impact of observation time, and each unit involved two sessions of observation. One out of 56 beds in the 5 ICUs was assigned by lots to each unit of observation time. That is, beds were randomly assigned to each unit of time, and random assignment was repeated 48 times. A session of observation lasted one hour, and no patient was repeatedly observed. The observation unit of an hour was determined based on the authors' personal experience. The survey was carried out with the participation of 77 out of 80 nurses who worked in the ICUs, understood the purpose of this study, and agreed to participate in the research.
5. Data Analysis
The collected data were analyzed using SPSS ver. 18.0 for Windows (SPSS Inc., Chicago, IL, USA). The frequency and percentage were used to analyze the types of medical device alarms in ICUs, the alarm-setting status for patient monitors, the frequency of alarms, the rate of false alarms, and the causes of alarms. Mean and standard deviation were used to analyze ICU nurses' alarm fatigue and recognition of alarms. Lastly, t-test and ANOVA were used to analyze alarm fatigue based on ICU nurses' general characteristics.
III. Results
1. Frequency of Alarms, Rate of False Positive Alarms, and Alarm-Setting Status of Patient Monitors
There were 9 types of devices generating auditory clinical alarms: patient monitors, infusion pumps, mechanical ventilators, continuous renal replacement therapy machines (CRRT), defibrillators, heating/cooling systems, intermittent pneumatic compression devices, ultrasound humidifiers, and blood refrigerators. There were a total of 32 devices of these 9 types, which could possibly generate 45 types of alarms.
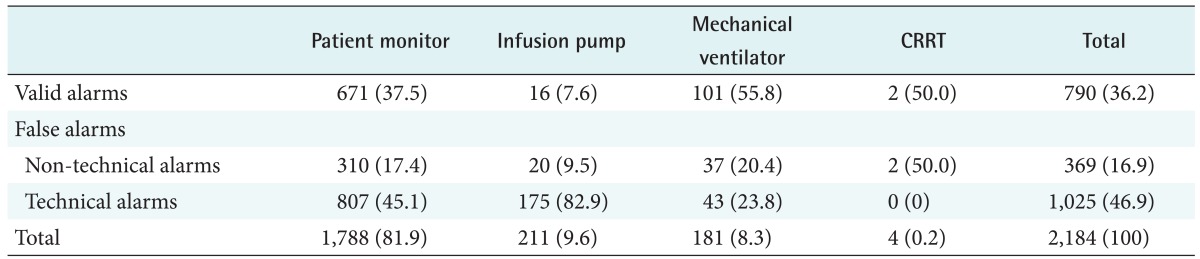
Four of the 9 types of devices actually generated alarms: patient monitors, mechanical ventilators, continuous renal replacement therapy machines, and infusion pumps. A total of 2,184 alarms rang for the 48 patients for 48 hours in total; thus, an average of 45.5 alarms rang per patient per hour. Of these, 37.3 were generated from patient monitors. They included 790 valid alarms (36.2%) and 1,394 false ones (63.8%): 369 non-technical alarms and 1,025 technical ones (Table 1).
Table 1. Frequency of clinical alarms and false alarms (n = 2,184).
Values are presented as number (%).
CRRT: continuous renal replacement therapy.
As for the alarm-setting status of patient monitors, nurses personally set an alarm range that reflected the patient's conditions in no more than 9 cases (18.8%); the default system alarm values already set continued to be applied in 17 cases (35.4%); and the range set by the nurses from the previous shifts continued to be applied in 22 cases (45.8%).
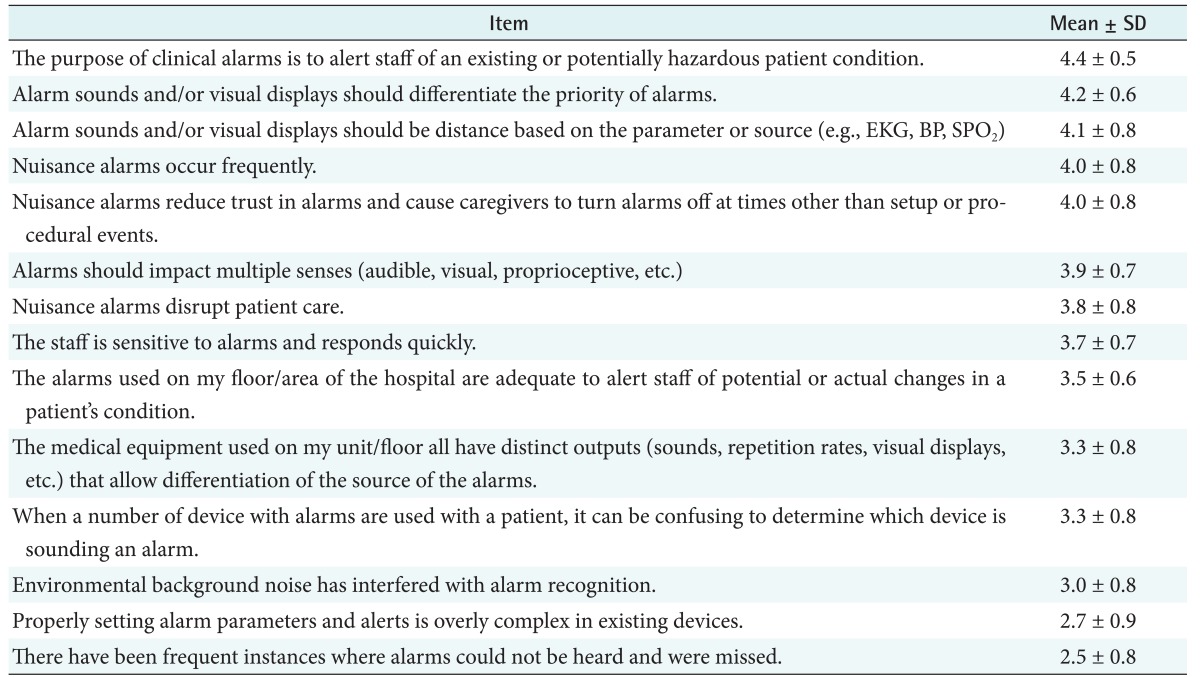
2. ICU Nurses' Recognition of Alarms
Possible score range for each item was from 1 to 5. Of 14 items in total, they scored lowest for "there have been frequent instances where alarms could not be heard and were missed" and highest for "the purpose of clinical alarms is to alert staff of an existing or potentially hazardous patient condition" (Table 2).
Table 2. Recognition of nurses on clinical alarms (n = 77).
Recognition was measured using a 5-point scale with a higher score meaning greater agreement.
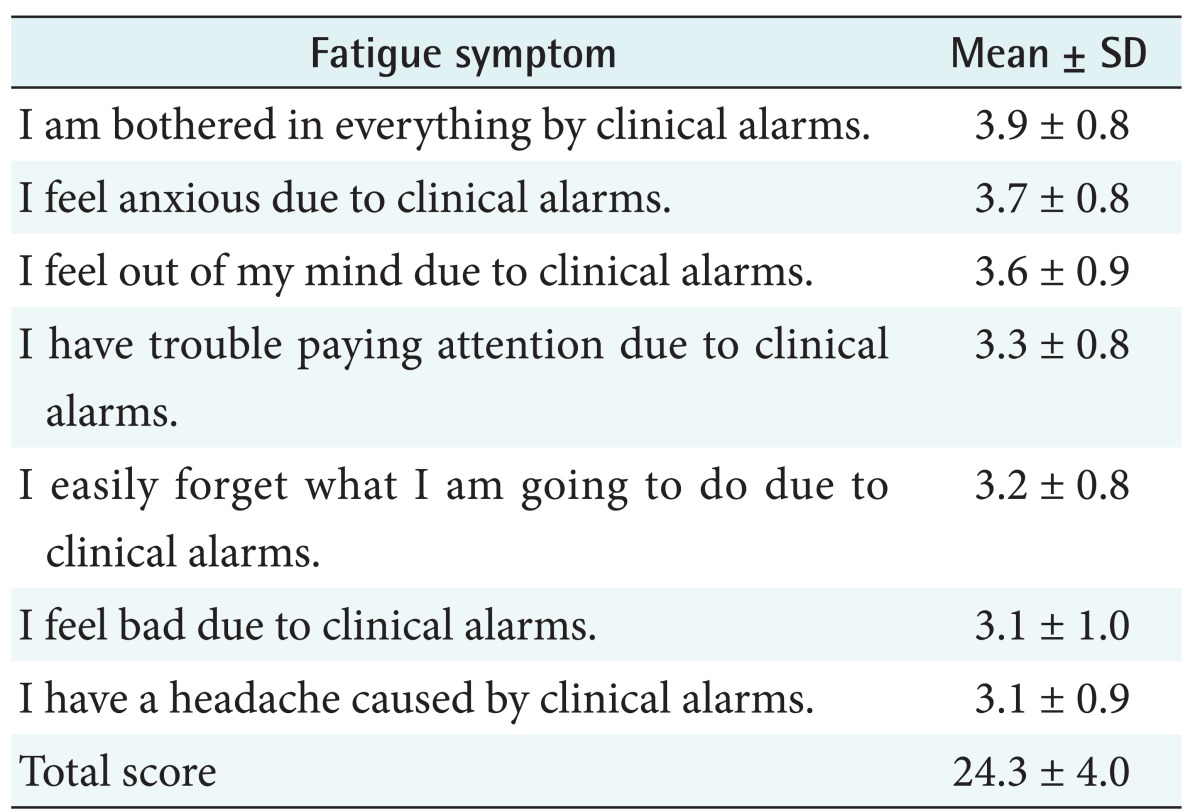
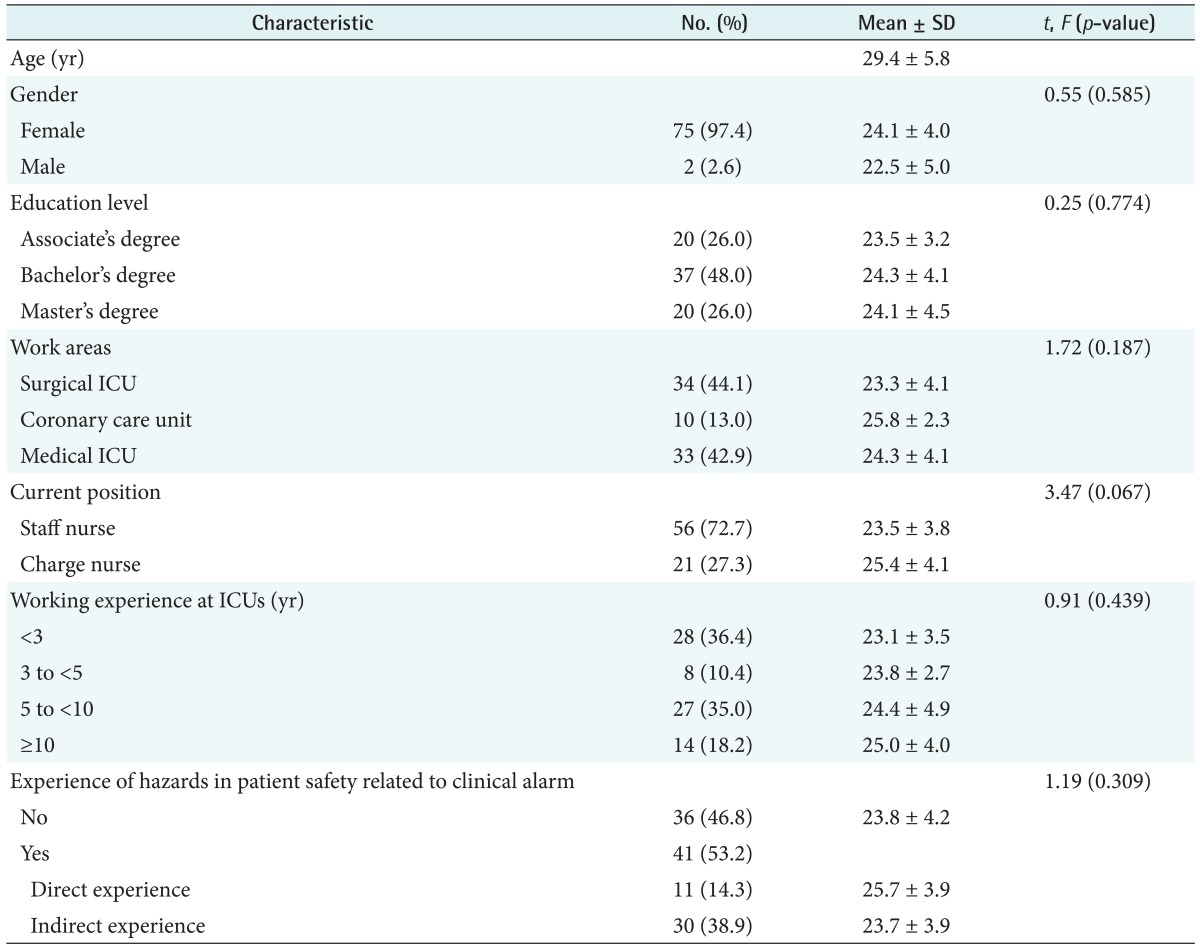
3. Alarm Fatigue of ICU Nurses and Differences in Alarm Fatigue by Nurses' General Characteristics
Nurses scored highest for "I am bothered in everything by medical device alarms" and lowest for "I have a headache caused by medical device alarms" (Table 3). For the nurses in this study, the mean age was 29.4 (±5.8) years, and the mean career in ICUs was 6.1 (±4.8) years. Thirty-six of them (46.8%) had no experience of alarm-related patient safety accidents; 11 (14.3%) personally had such experience; and 30 (38.9%) indirectly had such experience. The ICU nurses scored 24.3 (±4.0) out of 35 for alarm fatigue (Table 4).
Table 3. Nurses' fatigue in relation to clinical alarms (n = 77).
Fatigue was measured using a 5-point scale with a higher score meaning greater fatigue.
Table 4. General characteristics of nurses and difference in fatigue by characteristics (n = 77).
ICU: intensive care unit.
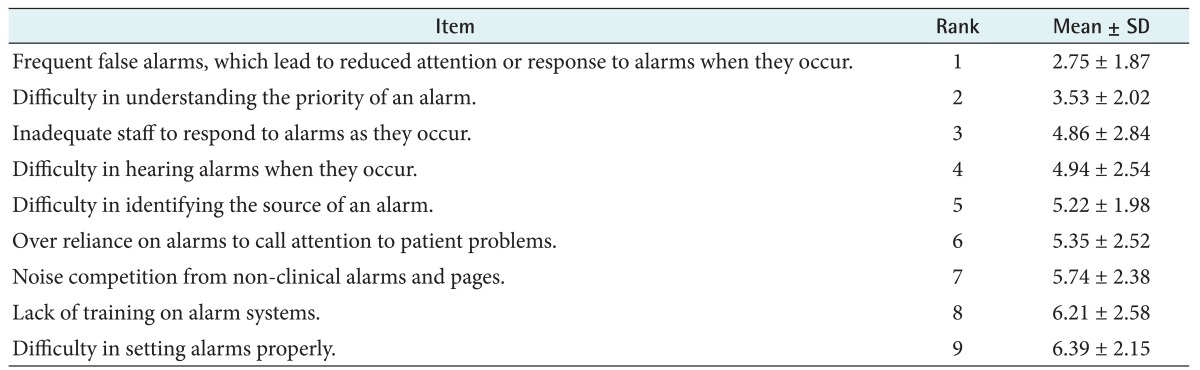
4. Obstacles to Clinical Alarm Management
Of the nine obstacles to effective management of medical device alarms, "frequent false alarms lead to reduced attention or response to alarms when they occur" was ranked 1st and "difficulty in setting alarms properly" was ranked 9th (Table 5).
Table 5. Obstacles to proper management of clinical alarms (n = 77).
Nurses were asked to determine the ranking of obstacles from 1st to 9th.
Ranking was measured according to the percentage of 1st rank.
IV. Discussion
In the present study, 32 devices generated 45 different alarms to warn nurses of abnormality in a patient or in device operation. Similarly, Borowski et al. [1] found about 40 different alarms in ICUs in 2011. Thus, it can be inferred that there is no significant difference in the types of alarm-generating medical devices in ICUs in Korea and abroad. Based on the finding from previous studies [1,9,10] that a nurse can distinguish 6–14 different alarms, it can be inferred that nurses may distinguish a device for up to 31% of 45 different alarms. It is therefore necessary to reduce the number of alarms that medical staff should differentiate by standardizing the alarms for each device, as suggested by Cvach [13].
As a single medical device, a patient bedside monitor generated the largest number of alarms, probably because it is an essential device for every ICU patient, and it monitors diverse variables of biorhythm. Previous studies [11,21,22] have found that patient monitors generated 28.8–39.2 alarms per hour. Such a gap between previous research and this study may partly result from differences in the number and type of variables monitored by patient monitors. The variation in the research period ranging from 6 hours to 18 days and the differences in the method of counting alarms—manual counting and automatic counting based on a system— also could account for this gap. It may be necessary to take these differences in counting and observation period into account in interpreting results.
In the present study, false alarms represented 63.8% of all the alarms. Patient monitors accounted for 62.5% of all the alarms. This rate of false alarms from patient monitors was higher than 52.3% that the false alarms were only generated for electrocardiograms [21]. In contrast, another research [26] reported that the rate of false alarms was 86%, and the largest number of false alarms was generated by a device measuring oxygen saturation. Such differences between the present study and previous studies may occur because the prior research had alarms counted automatically via a system and set a wider range of upper and lower limits than this study.
In this study, 72.2% of 1,117 false alarms from patient monitors were due to technical problems, such as separation of a sensor. This rate is higher than 13.7% for false alarms resulting from technical problems, as found by Baillargeon [21]. Such a gap is due to the differences in categorization of alarms. Baillargeon [21] classified cases in which the same alarm rang repeatedly more than five times as annoying alarms, and this occurred mainly when a sensor was separated. Annoying alarms were 32% in Baillargeon's study [21]. For such a great gap, nevertheless, the result that there were lots of false alarms with technical problems implies the possibility of reducing alarms most easily, for example, by replacing sensors. Alarms could be reduced by up to 46% by replacing skin electrodes for electrocardiogram monitors regularly and removing foreign materials from the skin before sensors are attached, as suggested by Cvach [13]. This method can be applied immediately to reduce the frequency of alarms in clinical practice.
Many researchers have indicated that occurrence of false alarms results from the application of a uniform alarm range to every patient [2]. This study also determined that false alarms could be reduced if nurses actually took patients' present conditions into account and set individualized alarms ranges. It was found that nurses set an alarm range that reflected the patient's conditions in only 9 (18.8%) out of 48 cases. Of the obstacles to clinical alarm management, however, most of the nurses regarded "difficulty in setting alarms properly" as the least important. This result implies that many of nurses in practice failed to set individualized alarms ranges for patients although setting alarms properly is not a difficult task.
Previous research simply regarded alarm fatigue as overexposure to alarms and reported that clinical alarms caused nurses to feel alarm fatigue [14]. While it is impossible to make a direct comparison because no researcher has tried to quantify alarm fatigue, we have developed an alarm fatigue scale to estimate fatigue in this study. It is presumed that the nurses felt alarm fatigue at moderate or higher levels: they scored 24.3 (±4.0) out of 35—69.4 out of 100—for alarm fatigue. Similarly, Chung and Kang [27] found that operating room nurses scored 69.2 for fatigue in general. Thus, the nurses in this study felt alarm fatigue at similar levels to those in general. Since no researcher has quantified alarm fatigue either in Korea or abroad, it is necessary to conduct further research on this issue to reconfirm the results.
Previous research on ICU nurses' recognition of clinical alarms [23] found that over 90% of the respondents agreed or strongly agreed with two items: "alarms sound and/or visual displays should differentiate the priority of alarms" and "alarms sound and/or visual displays should be distinct based on the parameter or source". These results were similar with the present results: 94.8% of the respondents agreed or strongly agreed that "alarm sounds and/or visual displays should differentiate the priority of alarms" and 87.0% agreed or strongly agreed that "alarm sounds and/or visual displays should be distance based on the parameter or source (e.g., EKG, BP, SPO2)". Similarly, the majority of respondents recognized the problem of false alarms. Their agreement with such items as "nuisance alarms occur frequently" (76.6%), "nuisance alarms disrupt patient care" (66.3%), and "nuisance alarms reduce trust in alarms and cause caregivers to turn alarms off at times other than setup or procedural events" (79.2%) was also at similar levels to those in prior research [17,23].
The issue of "frequent false alarms, which lead to reduced attention or response to alarms when they occur" was regarded as most important among the nine obstacles, and it was ranked first by 42% of the respondents in HTF [23]. In 2011, six years after the research by HTF [23], Funk et al. [17] also found that it was ranked first and remained an important issue, still unsolved. Similarly, Christensen et al. [7] found that 81% of the 48 ICU nurses indicated false alarms and inappropriate alarm setting as main causes of alarm fatigue. To make ICU nurses less likely to feel fatigue associated with alarms, therefore, it is necessary to make efforts to reduce false alarms.
Borycki [28] warned that new healthcare technologies could introduce technology-induced errors, while we have not paid much attention, in terms of patient safety, to medical device alarms. There is no Korean study that can be compared with this study; however, the results of this study were differed insignificantly from those of previous studies. The nurses recognized false alarms as an important issue in alarm management, set individualized alarms ranges in very few cases although they felt a moderate level of fatigue from medical device alarms, and used an alarm systems inefficiently. Since medical device alarms in ICUs and alarm fatigue are directly linked to the issue of patient safety, effort to manage medical device alarms effectively and reduce alarm fatigue can also prevent potential hazardous events.
Footnotes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Borowski M, Gorges M, Fried R, Such O, Wrede C, Imhoff M. Medical device alarms. Biomed Tech (Berl) 2011;56(2):73–83. doi: 10.1515/BMT.2011.005. [DOI] [PubMed] [Google Scholar]
- 2.ERCI Institute. Top 10 technology hazards for 2012: the risks that should be at the top of your prevention list. Health Devices. 2011;40(11):358–373. [PubMed] [Google Scholar]
- 3.The Joint Commission. Sentinel event alert [Internet] Washington (DC): The Joint Commission; 2002. [cited at 2015 Dec 17]. Available from: http://www.jointcommission.org/assets/1/18/SEA_25.pdf. [Google Scholar]
- 4.US Food and Drug Administration. FDA patient safety news: alarms monitoring problems [Internet] Silver Spring (MD): Food and Drug Administration; 2011. [cited at 2015 Dec 17]. Available from: http://www.fda.gov/downloads/Safety/FDAPatientSafetyNews/UCM417915.pdf. [Google Scholar]
- 5.ERCI Institute. Hazard: Gorman-Rupp hypothermia machine. Health Devices. 1972;1(8):190–191. [PubMed] [Google Scholar]
- 6.Bell L. Alarm fatigue linked to patient's death: interview by Laura Wallis. Am J Nurs. 2010;110(7):16. doi: 10.1097/01.NAJ.0000383917.98063.bd. [DOI] [PubMed] [Google Scholar]
- 7.Christensen M, Dodds A, Sauer J, Watts N. Alarm setting for the critically ill patient: a descriptive pilot survey of nurses' perceptions of current practice in an Australian Regional Critical Care Unit. Intensive Crit Care Nurs. 2014;30(4):204–210. doi: 10.1016/j.iccn.2014.02.003. [DOI] [PubMed] [Google Scholar]
- 8.Edworthy J, Hellier E. Alarms and human behaviour: implications for medical alarms. Br J Anaesth. 2006;97(1):12–17. doi: 10.1093/bja/ael114. [DOI] [PubMed] [Google Scholar]
- 9.AACE Health Technology Foundation, Clinical Alarm Task Force. Impact of clinical alarms on patient safety: a report from the American College of Clinical Engineering Healthcare Technology Foundation. J Clin Eng. 2007;32(1):22–33. [Google Scholar]
- 10.Momtahan K, Hetu R, Tansley B. Audibility and identification of auditory alarms in the operating room and intensive care unit. Ergonomics. 1993;36(10):1159–1176. doi: 10.1080/00140139308967986. [DOI] [PubMed] [Google Scholar]
- 11.Association for the Advancement of Medical Instrumentation. Clinical Alarms 2011 Summit [Internet] Arlington (VA): Association for the Advancement of Medical Instrumentation; 2011. [cited at 2015 Dec 17]. Available from: http://s3.amazonaws.com/rdcms-aami/files/production/public/FileDownloads/Summits/2011_Alarms_Summit_publication.pdf. [Google Scholar]
- 12.Bell L. Monitor alarm fatigue. Am J Crit Care. 2010;19(1):38. doi: 10.4037/ajcc2010641. [DOI] [PubMed] [Google Scholar]
- 13.Cvach M. Monitor alarm fatigue: an integrative review. Biomed Instrum Technol. 2012;46(4):268–277. doi: 10.2345/0899-8205-46.4.268. [DOI] [PubMed] [Google Scholar]
- 14.Sendelbach S. Alarm fatigue. Nurs Clin North Am. 2012;47(3):375–382. doi: 10.1016/j.cnur.2012.05.009. [DOI] [PubMed] [Google Scholar]
- 15.ERCI Institute. The hazards of alarm overload. Keeping excessive physiologic monitoring alarms from impeding care. Health Devices. 2007;36(3):73–83. [PubMed] [Google Scholar]
- 16.Cvach MM, Biggs M, Rothwell KJ, Charles-Hudson C. Daily electrode change and effect on cardiac monitor alarms: an evidence-based practice approach. J Nurs Care Qual. 2013;28(3):265–271. doi: 10.1097/NCQ.0b013e31827993bc. [DOI] [PubMed] [Google Scholar]
- 17.Funk M, Clark JT, Bauld TJ, Ott JC, Coss P. Attitudes and practices related to clinical alarms. Am J Crit Care. 2014;23(3):e9–e18. doi: 10.4037/ajcc2014315. [DOI] [PubMed] [Google Scholar]
- 18.Purbaugh T. Alarm fatigue: a roadmap for mitigating the cacophony of beeps. Dimens Crit Care Nurs. 2014;33(1):4–7. doi: 10.1097/DCC.0000000000000014. [DOI] [PubMed] [Google Scholar]
- 19.Gazarian PK. Nurses' response to frequency and types of electrocardiography alarms in a non-critical care setting: a descriptive study. Int J Nurs Stud. 2014;51(2):190–197. doi: 10.1016/j.ijnurstu.2013.05.014. [DOI] [PubMed] [Google Scholar]
- 20.Inokuchi R, Sato H, Nanjo Y, Echigo M, Tanaka A, Ishii T, et al. The proportion of clinically relevant alarms decreases as patient clinical severity decreases in intensive care units: a pilot study. BMJ Open. 2013;3(9):e003354. doi: 10.1136/bmjopen-2013-003354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Baillargeon E. Alarm fatigue: a risk assessment [master's theses] Providence (RI): Rhode Island College; 2013. [Google Scholar]
- 22.Graham KC, Cvach M. Monitor alarm fatigue: standardizing use of physiological monitors and decreasing nuisance alarms. Am J Crit Care. 2010;19(1):28–34. doi: 10.4037/ajcc2010651. [DOI] [PubMed] [Google Scholar]
- 23.ACCE Healthcare Technology Foundation. Impact of clinical alarms on patient safety. Plymouth Meeting (PA): ACCE Healthcare Technology Foundation; 2006. [Google Scholar]
- 24.Japanese Society for Occupational Health, Working Group for Occupational Fatigue. Subjective symptoms survey (Jikaku-sho Shirabe) Labor Sci. 2002;57(5):295–298. [Google Scholar]
- 25.Kim SJ, Sung MS. Subjective symptoms on fatigue in hospital nurses. J Korean Acad Nurs. 1998 Dec;28(4):908–919. [Google Scholar]
- 26.Tsien CL, Fackler JC. Poor prognosis for existing monitors in the intensive care unit. Crit Care Med. 1997;25(4):614–619. doi: 10.1097/00003246-199704000-00010. [DOI] [PubMed] [Google Scholar]
- 27.Chung CH, Kang HY. Job stress and fatigue of the nurses in the operating room. J Korea Contents Assoc. 2013;13(12):291–298. [Google Scholar]
- 28.Borycki E. Trends in health information technology safety: from technology-induced errors to current approaches for ensuring technology safety. Healthc Inform Res. 2013;19(2):69–78. doi: 10.4258/hir.2013.19.2.69. [DOI] [PMC free article] [PubMed] [Google Scholar]