Highlights
-
•
We report the first case of duodenal atresia and choledochocele requiring surgical treatment in the neonatal period.
-
•
The patient received a classical duodeno-duodenostomy on day 2 of life.
-
•
The choledochocele was treated with transduodenal marsupialization at the age of three months.
-
•
A life-long observation seems mandatory to examine the potential risk of metaplasia in the cystic remnant.
Keywords: Duodenal atresia, Choledochal cyst, Choledochocele, Newborn surgery, Marsupialization
Abstract
Introduction
The congenital combination of duodenal atresia and choledochal cyst has only been reported in a few children. None of these patients had an intrapancreatic choledochocele causing persistent hyperbilirubinemia in the newborn period.
Presentation of case
A female newborn presented with duodenal atresia and received a duodeno–duodenostomy on day two of life. The postoperative course was uneventful except for progressive hyperbilirubinemia and elevation of liver enzymes. No evidence for surgical obstruction, malformations of the hepatobiliary system, or infectious diseases were found. At three months of age and persistent hyperbilirubinemia an intrapancreatic choledochocele type III according to Todani was confirmed by ultrasound and MRI. Upon laparotomy no lesion was visible or palpable within the pancreas. Even after duodenotomy distally of the duodeno–duodenostomy only a normal papilla Vateri could be identified. Transduodenal ultrasound allowed for localization and saline distension to outline the borders of the choledochocele. A transduodenal marsupialization provided immediate biliary drainage and postoperatively bilirubin levels returned to normal limits.
Discussion
We present a case of duodenal atresia and choledochocele requiring surgical treatment in the neonatal period. Transduodenal marsupialization prompted adequate biliary drainage without inflicting the potential complications of biliary and pancreatic diversion at this early age. A life-long endoscopic observation seems mandatory to examine the potential risk of metaplasia of the cystic remnant.
Conclusion
Early transduodenal marsupialization of an intrapancreatic choledochocele in a case of duodenal atresia is safe and feasible to prevent secondary liver cirrhosis.
1. Introduction
The association of duodenal atresia (DA) with other congenital anomalies like annular pancreas, intestinal atresia, malrotation or cardiac defects is well known. However, the combination of DA with biliary malformations has been reported in only a few cases. The management of such cases deserves special attention, especially when the biliary malformation causes problems in the newborn period.
This case report describes a patient with the rare association of duodenal atresia and an intrapancreatic choledochocele. The surgical treatment is described and the outcome presented. The local ethical committee approved the study (27-498 ex 14/15). The case report has been reported in line with the CARE criteria [1].
2. Presentation of case
The female patient was born at 38 weeks of gestational age with a birth weight of 2342 g (small for gestational age). On prenatal ultrasound polyhydramnion and a double-bubble sign had been detected. After confirmation of the DA postnatally the child received a classical duodeno-duodenostomy on day 2 of life. No annular pancreas was noted.
The immediate postoperative course was uneventful. However, elevated bilirubin levels (5.99 mg/dl) were recorded and phototherapy was initiated for two days. Nevertheless, hyperbilirubinemia (6.1 mg/dl) and elevated liver parameters (AP 966 U/l; GGT 414 U/l; CHE 8624 U/l; AST 161 U/l; ALT 71 U/l) persisted. The stool was never pale. An extensive work-up revealed no evidence for iatrogenic injury or malformation of the biliary system. At the age of 3 months a cystic formation was noted located in the pancreatic head on abdominal ultrasound measuring 1.2 × 1.5 cm. (Fig. 1). Dilations of the common bile duct or intrahepatic bile ducts were not present. MCRP confirmed a choledochocele type III according to Todani et al. [2] inside the pancreatic head and just distally to the duodenal anastomosis (Fig. 2).
Fig. 1.
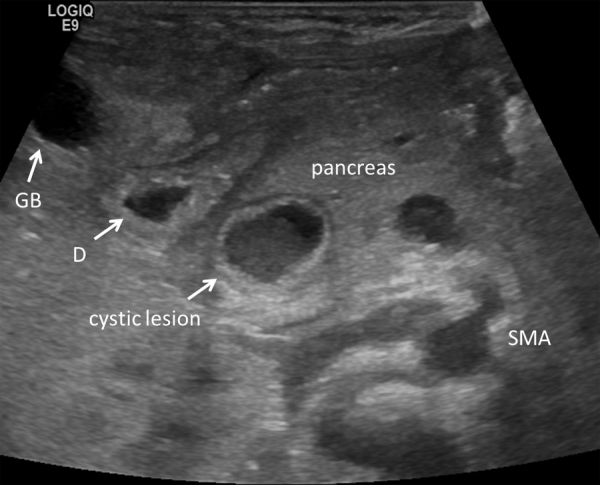
Ultrasound performed at three months of age revealed the cystic lesion in close relation to the duodenum (D). To the left of the duodenum the Gallbladder (GB) can be seen, as well as the superior mesenteric artery (SMA) to the right.
Fig. 2.
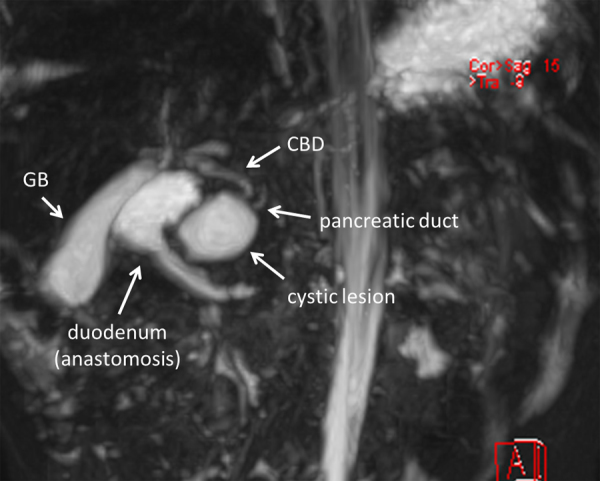
3D-reconstruction of MRCP showing the cystic lesion in close proximity to the duodenal anastomosis, the pancreatic duct and the common bile duct (CBD). GB…gallbladder.
Due to persistent hyperbilirubinemia the patient received another laparotomy. Intraoperatively the duodenum was kocherized, but the lesion could not be identified within the pancreas. Therefore a duodenotomy was performed revealing a normal papilla Vateri, but still no cystic lesion. Finally, transduodenal ultrasound was performed intraoperatively allowing the localization and saline distension of the cyst. The decision was made not to resect the pancreatic head, but to perform a transduodenal marsupialization, taking great care not to damage the papilla of Vater. Marsupialization of the cystic wall to the dorsal duodenal mucosa allowed for free bile flow (Fig. 3).
Fig. 3.
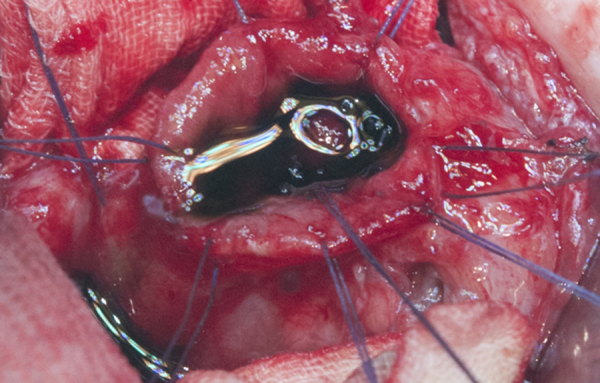
Intraoperative photograph showing marsupialization of the cyst providing successful drainage.
Postoperatively, bilirubin levels and liver parameters normalized (Bili 2.91 mg/dl, AP 552 U/l, GGT 625 U/l, CHE 734 U/l). At latest follow-up at a patient́s age of two years the child was free of symptoms without signs of jaundice and a bilirubin level of 0.28 mg/dl.
3. Discussion
How do you treat a neonate with DA and an intrapancreatic choledochocele that shows persistent hyperbilirubinemia? Unfortunately, the present literature reveals only scarce information or recommendations, because the incidence of this combination of congenital malformations is very low [3].
One embryological explanation for this unlikely combination may be the difference in the development of each malformation [4]. DA usually occurs between the 8th and 10th week of gestation due to a failure of recanalization of the primitive midgut. An association with pancreatic malformations is well-known. Basically the development of CC seems to be attributed to an abnormal primary proliferation of the embryological ductal system causing congenital obstruction and subsequent dilatation. Whether the congenital combination of DA and annular pancreas may additionally contribute to the development of CC is open for discussion. Interestingly enough, the few patients with DA and CC described before all suffered from a concomitant annular pancreas [3], whereas our patient had a normal pancreas.
Other major differences between previous patients with DA and CC versus our case concern the onset of symptoms, type of CC and surgical strategy. None of the nine yet reported patients required surgery within the first year of life. Instead the correction of the CC was performed with a mean age of 4.9 years (range: 13 months–12 years). Secondly, the vast majority of these patients suffered from an extrahepatic and extrapancreatic CC, which could be treated “classically” by complete resection and biliary diversion. Such a strategy is recommended due to the potential risk of malignant transformation of the remaining cyst [5], [6]. Instead our patient became symptomatic immediately after birth and required surgery once the diagnosis had been established at an age of three months. Due to the intrapancreatic localization of this choledochocele a complete resection would have required a biliary as well as pancreatic diversion. Despite the considerable intraoperative risk factors in this age group, the long-term sequelae of such an extensive reconstruction were appreciated. Thus, the decision was taken to perform a “simple” transduodenal marsupialization, which provided immediate biliary drainage.
Several drawbacks of marsupialization of a choledochal cyst have been described. Malignant transformation has been described in 2.5% [7] to 26% [8] of all choledochal cysts. The risk of developing malignancy seems to be higher in patients with inadequate cyst excision [9]. Liu et al. even reported a 33.3% malignancy rate after incomplete removal of the cyst [5]. The question remains whether or not choledochoceles carry the same risk for malignant transformation as “classical” choledochal cysts. Moreover, the development of bile stones within the residual cyst may also be possible due to stasis. Therefore, a life-long endoscopic observation seems mandatory to examine the potential risk of metaplasia in the cystic remnant. In any case of histological doubt a complete resection and biliary drainage procedure could be performed in a more favorable age of our patient.
4. Conclusion
In summary, we present a case with the congenital combination of DA and intrapancreatic choledochocele requiring surgical treatment in the neonatal period. We were able to demonstrate that in cases of intraoperative invisible and non-palpable intrapancreatic choledochoceles, the duodenum can be opened and ultrasound can be applied allowing localization and saline distension of the cyst. Subsequent marsupialization can be performed prompting adequate biliary drainage without the risk and long-term morbidity of a biliary and pancreatic diversion at an early age.
Conflict of interest
None.
Funding
No funding has been received for this study.
Ethical Approval
Approval of the local ethics committee has been given (Ethics Committee of the Medical University of Graz, Reference number: 27-498 ex 14/15).
Consent
Consent has been obtained from the patient’s guardian.
Authors contribution
SZ collected the data. GS writing of the paper. ES collected the data, data analysis. AWF writing of the paper. HT writing of the paper, study concept.
Guarantor
The Guarantor is Dr. Georg Singer.
References
- 1.Gagnier J.J., Kienle G., Altman D.G., Moher D., Sox H., Riley D. The CARE guidelines: consensus-based clinical case report guideline development. J. Clin. Epidemiol. 2014;67:46–51. doi: 10.1016/j.jclinepi.2013.08.003. [DOI] [PubMed] [Google Scholar]
- 2.Todani T., Watanabe Y., Narusue M., Tabuchi K., Okajima K. Congenital bile duct cysts: classification, operative procedures, and review of thirty-seven cases including cancer arising from choledochal cyst. Am. J. Surg. 1977;134:263–269. doi: 10.1016/0002-9610(77)90359-2. [DOI] [PubMed] [Google Scholar]
- 3.Iwai A., Hamada Y., Takada K., Inagaki N., Nakatake R., Yanai H. Choledochal cyst associated with duodenal atresia: case report and review of the literature. Pediatr. Surg. Int. 2009;25:995–998. doi: 10.1007/s00383-009-2462-3. [DOI] [PubMed] [Google Scholar]
- 4.Sugimoto T., Yamagiwa I., Obata K., Ouchi T., Takahashi R., Suzuki R. Choledochal cyst and duodenal atresia: a rare combination of malformations. Pediatr. Surg. Int. 2004;20:724–726. doi: 10.1007/s00383-002-0783-6. [DOI] [PubMed] [Google Scholar]
- 5.Liu Y.B., Wang J.W., Devkota K.R., Ji Z.L., Li J.T., Wang X.A. Congenital choledochal cysts in adults: twenty-five-year experience. Chin. Med. J. (Engl.) 2007;120:1404–1407. [PubMed] [Google Scholar]
- 6.Wang D.C., Liu Z.P., Li Z.H., Li D.J., Chen J., Zheng S.G. Surgical treatment of congenital biliary duct cyst. BMC Gastroenterol. 2012;12:29. doi: 10.1186/1471-230X-12-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Naga M.I., Suleiman D.N. Endoscopic management of choledochal cyst. Gastrointest. Endosc. 2004;59:427–432. doi: 10.1016/s0016-5107(03)02367-8. [DOI] [PubMed] [Google Scholar]
- 8.Flanigan D.P. Biliary carcinoma associated with biliary cysts. Cancer. 1977;40:880–883. doi: 10.1002/1097-0142(197708)40:2<880::aid-cncr2820400242>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 9.Watanabe Y., Toki A., Todani T. Bile duct cancer developed after cyst excision for choledochal cyst. J. Hepatobiliary Pancreat. Surg. 1999;6:207–212. doi: 10.1007/s005340050108. [DOI] [PubMed] [Google Scholar]


